Back to Journals » Advances in Medical Education and Practice » Volume 14
A Pilot Study of Symptoms of Major Depressive Disorder in Medical Students at an Osteopathic Medical School Before and After High-Stakes Examinations
Authors Arabatzis TJ, Doroshenko J, Ashraf MA, Smith RM
Received 15 June 2023
Accepted for publication 26 October 2023
Published 9 November 2023 Volume 2023:14 Pages 1259—1271
DOI https://doi.org/10.2147/AMEP.S426015
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Taxiarhia J Arabatzis,1 Justin Doroshenko,2 Muhammad A Ashraf,3 Ryan M Smith4
1Department of Internal Medicine-Pediatrics Residency Program, Geisinger Medical Center, Danville, PA, USA; 2Department of Emergency Medicine Residency Program, University of Texas Health San Antonio, San Antonio, TX, USA; 3Diagnostic Radiology Residency Program, Hartford Hospital, Hartford, CT, USA; 4Department of Psychiatry, University of New England College of Osteopathic Medicine, Biddeford, ME, USA
Correspondence: Ryan M Smith, Email [email protected]
Background: Given the high prevalence of symptoms of major depressive disorder (MDD) in medical students, identifying factors that impact the development of such symptoms is important. Previous data suggest that medical students can experience symptoms of MDD after medical school exams. It is not known if medical students experience more symptoms of MDD directly before or after exams. The aim of the current study is to determine the prevalence of symptoms of MDD in first- and second-year medical students directly before and after high-stakes medical school examinations.
Methods: Two anonymous surveys were sent via REDCap to first- and second-year medical students at the University of New England College of Osteopathic Medicine. A pre-exam survey on the day of the exam asking about the past three days’ MDD symptoms, and a post-exam survey sent three days after the exam asking about MDD symptoms experienced after the exam was sent out to a total of 391 students with a response rate of 23%.
Results: First- and second-year medical students regardless of gender experienced symptoms of MDD at higher rates before exams than afterwards. Female students experienced symptoms of MDD (as defined by the DSM-5) including sadness, sleep disturbances, and feelings of guilt or worthlessness at a greater rate compared to males before exams. After exams, females were more likely to experience sleep disturbances and decreased energy. Second-year male students were the least likely to experience symptoms of MDD.
Conclusion: First- and second-year medical students can experience symptoms of MDD surrounding exams. This study highlights the emotional burden that students may carry near exams. It underscores the importance of further research on this topic to evaluate the effect exams have on the mental health of medical students during their training.
Keywords: depression, medical school, examinations, gender, MDD
A Letter to the Editor has been published for this article.
Introduction
Throughout the world, greater than one-quarter of medical students experience symptoms of major depressive disorder (MDD) at some point during their medical school training.1–5 Research has consistently shown that medical students experience higher rates of symptoms of MDD and anxiety compared to the general population.2–9 According to the National Institutes of Health, in 2020, the prevalence of MDD in the United States (US) was 8.4%, with females (10.5%) having a greater prevalence than males (6.2%).10 MDD has been shown to occur in medical students at a prevalence as high as 25%, whereas the general population has a rate closer to 10%.10 The finding that a greater proportion of female medical students experience symptoms of MDD compared to males has also been described multiple times.11–18 However, other studies show that there is no difference,19,20 suggesting that the true effect of gender on the development of the symptoms of MDD in medical students is still not fully elucidated. However, it does appear more research points towards a female predominance in the development of symptoms of MDD in medical students, again consistent with the general population.10 Given the high prevalence of symptoms of MDD in medical students, identifying factors that affect the development of these symptoms is both timely and important to the mental health of our future health care providers.
Much of the current research on the development of the symptoms of MDD in medical students is from countries outside of the United States (US), leaving this area of research largely unexplored in the US. Additionally, during the COVID-19 pandemic, a survey of medical students at forty medical schools in the US found increased rates of both symptoms of MDD and anxiety compared to pre-pandemic rates, revealing a possible exacerbation of an already largely unaddressed problem in the medical education system.21 Interestingly, data from other countries shows that while both anxiety and stress were increased in medical students during the COVID-19 pandemic, rates of the development of MDD did not change.22,23 Of note, the study noted that was conducted in the US looking at medical students during the pandemic was published in 2021, while the other studies were published in 2020; perhaps the progression of the pandemic may later show the same trend in medical students in other countries. These differences could also reflect cultural differences, as prior research has shown that attitudes towards mental illness can differ among medical students based on their country of origin.24
Prior research that looked at the prevalence of the development of MDD and burnout in matriculating medical students compared to non-medical students who had finished a four-year degree found that matriculating medical students experienced lower rates of MDD and burnout compared to other students who just finished a four-year degree.25 Other studies have shown that the prevalence of MDD among medical students upon entry into medical school resembles the general population, but increases during their medical education and training.26–28 Additionally, third-year medical students are at greater risk of developing symptoms of MDD compared to first-year medical students.29 This suggests that many students do not come into medical education with symptoms of MDD, but rather the medical education process may be contributing to the development of the symptoms of MDD.25 Finally, another recent study looking at matriculating medical students in Australia found that students entering medical school had significant baseline rates of depression, anxiety, and stress;27 this further complicates elucidating whether students entering medical school are generally more inclined to develop symptoms of MDD, or if they come in already having either higher rates of MDD or a greater predilection to develop MDD.
According to the NIH, 66% of adults aged 18 and older who experienced an episode of MDD received treatment for their illness.10 This is in stark contrast to medical students who receive professional help for depression—with studies showing that only 15–22% of students with diagnosed MDD sought help for their diagnosis.1,30 One particular cross-sectional study found that 81% of medical students surveyed who met the criteria for MDD were undiagnosed at the time.31 Across multiple studies, barriers exist to medical students seeking professional help, included stigma, confidentiality concerns, and fear of unwanted intervention.30,32 The fact that medical students may have high rates of MDD but are undiagnosed—and less likely to seek help for depression—is startling, and only emphasizes that uncovering the factors that contributed to the development of MDD in this population may help prevent serious consequences in medical student’s mental health and the mental health of our future physicians.
Factors that contribute to the development of symptoms of MDD in medical students include “dysfunctional coping strategies and low resilience”.33 Other research has shown that approaching high-stakes examinations increases the manifestation of symptoms of MDD and anxiety in medical students,34 and the rates of MDD are highest in medical students right after medical school exams.15 Yet, the presence of symptoms of MDD and anxiety in medical students are likely multifactorial in nature, due both to the multiple stressors and the heterogeneity of the population that makes up medical students. Developing a better understanding of the triggers of depressive symptoms in medical students may lead to better interventions to curb symptoms in this population.
The present researchers’ prior work investigated the development of symptoms of MDD in medical students immediately following high-stakes medical school examinations. That research found that female medical students experienced greater development of symptoms of MDD compared to their male counterparts.15 However, in the previous work, students were surveyed only after high-stakes examinations. The aim of the current study is to determine the prevalence of symptoms of MDD in first- and second-year medical students both directly before and directly after high-stakes medical school examinations to better characterize how, and if, these examinations may be contributing to the development of symptoms of MDD in medical students. The study hypotheses were: (1) female medical students will develop more symptoms of MDD both before and after high-stakes medical school examinations, and (2) medical students will experience symptoms of MDD both directly before and after high-stakes medical school examinations, with significantly more symptoms after examinations.
Methods
Two secure surveys were sent via university e-mail to first- and second-year medical students at the University of New England College of Osteopathic Medicine (UNECOM) in Biddeford, Maine, using the REDcap program. The survey was sent to a total of 391 students. The first survey was sent on the day of the examinations (pre-examination survey) and students were asked to record symptoms of MDD, if any, they had experienced in the three days leading up to the exam. The second survey was sent out three days after the examination (post-examination survey). The survey was sent after multiple exams to get a large enough sample size, but participants were asked to only fill out the survey once. The authors were in contact with school administrators to ensure dates of exams for the student body surveyed to ensure the surveys were sent out truly before and after exam periods. The surveys sent to students can be found in Figure 1a (pre-exam survey) and Figure 1b (post-exam survey). A consent form was attached to each survey. The survey was created by the authors and asked similar symptom questions as prior research by the authors.15 The survey asked about the symptoms of major depressive disorder (MDD) as described in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). Both the survey and research project were approved by the University of New England (UNE) IRB. All data were collected anonymously via REDcap. Data was stratified by gender and chronological year of medical education. Data was compiled and statistics were run using IBM SPSS software. Participants who completed the survey in full were included in the data analysis. Only one participant reported their gender as non-binary, and thus was removed from analysis for statistical comparison reasons. Two-sided chi-square tests were used to determine differences between categorical groups. P < 0.05 was the threshold used for considered statistical significance.
 |
Figure 1 (a) Pre-exam Survey Questions. (b) Post-exam Survey Questions. |
Results
Survey Participants
A total of 91 students responded to the pre-exam survey out of 391 for a response rate of 23.3%. A total of 41 (21.5%) first-year students participated in the pre-exam survey. A total of 50 (25.0%) second-year medical students participated in the pre-exam survey. A total of 115 students responded to the post-exam survey out of 391 for a response rate of 29.4%. A total of 65 (34.0%) first-year students and 50 (25.0%) second-year medical students participated in the post-exam survey. Overall, more female medical students participated in the study compared to males (Table 1).
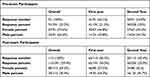 |
Table 1 Study Participants |
Symptoms of MDD Before and After Medical School Exams
When all medical students in the sample were combined (male and female first- and second-year medical students) and rates of development of symptoms of MDD were compared both before and after exams, we found that a higher percentage of medical students experienced symptoms of MDD before medical school exams compared to after medical school exams (Figure 2). This was statistically significant for all DSM-5 symptoms of MDD except for psychomotor agitation (p = 0.06) and suicidal ideation (p = 0.458) (Figure 2) which, although not statistically significant, still followed the trend of a greater percentage of students experiencing these symptoms before exams compared to after exams. For the following symptoms of MDD, a greater percentage of students experienced them before exams compared to after, and this was statistically significant for the following symptoms: sadness (p < 0.001), anhedonia (p = 0.004), sleep disturbances (p = 0.015), guilt or worthlessness (p < 0.001), decreased energy (p = 0.001), decreased concentration (p = 0.006), and changes in appetite (p = 0.001) (Figure 2).
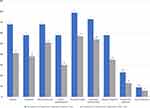 |
Figure 2 Prevalence of depression symptoms before and after test. * p < 0.05 horizontal axis is symptoms of depression, vertical axis is percentage of students who experiences symptoms. |
Gender Differences in Symptoms of MDD Experienced Before and After Medical School Exams
In the current study, female medical students were more likely to experience symptoms of MDD both before and after medical school exams compared to male peers (Figures 3 and 4). In the 3 days leading up to medical school exams, a statistically significant percentage of female medical students, compared to male medical students, experienced the following symptoms of MDD: sadness (p = 0.001), sleep disturbances (p = 0.006), and feelings of guilt or worthlessness (p = 0.001) (Figure 3. The same trend followed for anhedonia (p = 0.151), decreased energy (p = 0.080), decreased concentration (p = 0.200), changes in appetite (p = 0.151), psychomotor agitation or retardation (p = 0.385), and suicidal ideation (p = 0.926) (Figure 3).
When surveyed 3 days after exams, the trend of a greater percentage of female medical students experiencing the symptom of MDD compared to males was seen for all symptoms, except for suicidal ideation (p = 0.461) (Figure 4). This was statistically significant for the symptoms of sleep disturbances (p = 0.001) and decreased energy (p = 0.013) (Figure 4). The same trend followed for the symptoms of sadness (p = 0.342), anhedonia (p = 0.157), guilt or worthlessness (p = 0.297), decreased concentration (p = 0.724), changes in appetite (p = 0.355), and psychomotor agitation (p = 0.346), though the differences were not statistically significant (Figure 4). Of note, regardless of gender, a large percentage of students experienced at least some symptoms of MDD both before and after medical school exams.
Symptoms of MDD in Female Medical Students Before and After Exams
When we looked at both first- and second-year female medical students, we found similar trends to that described above, with females experiencing more symptoms of MDD before exams as compared to after, which was statistically significant for sadness (p < 0.000), anhedonia (p = 0.015), feelings of guilt or worthlessness (p < 0.000), decreased energy (p = 0.011), decreased concentration (p = 0.008) and changes in appetite (p = 0.002) (Figure 5a). The same trend was seen for sleep disturbance (p = 0.054), psychomotor agitation or retardation (p = 0.115), and suicidal ideation (p = 0.343), but this was not statistically significant (Figure 5a). Overall, both first- and second-year female medical students exhibited similar trends, with both first- and second-year female students experiencing more symptoms of MDD before exams as compared to afterward. For first-year female medical students, this was significant for sadness (p < 0.001), feelings of guilt or worthlessness (p = 0.004), decreased energy (p = 0.009), and decreased concentration (p = 0.002) (Figure 5b). For second-year female medical students, this was significant for sadness (p = 0.045), feelings of guilt or worthlessness (p = 0.001), and changes in appetite (p = 0.012) (Figure 5c). Figure 5 Continued.
Symptoms of MDD in Male Medical Students Before and After Exams
When we looked at first- and second-year male medical students, we found a similar trend to that of females, where male medical students experienced higher rates of symptoms of MDD before exams compared to after for all symptoms, except for suicidal ideation (Figure 6a). These findings were less pronounced than the differences seen in females, with the only statistically significant difference seen for decreased energy (p = 0.044). Interestingly, for the symptom of anhedonia, second-year male medical students experienced this symptom more than first-year medical students, but this was not statistically significant (p = 0.145). When we looked at first-year male medical students and compared symptoms of MDD both before and after exams, we again uncovered a similar pattern as with first-year female medical students, where first-year male medical students experienced more symptoms of MDD before exams compared to after; however, the difference was less pronounced in males, with the only statistically significant difference seen for decreased energy (p = 0.017) (Figure 6b). Second-year medical students experienced similar rates of development of symptoms of MDD before and after exams, and no statistical difference was found looking at the development of symptoms of MDD before exams and after (Figure 6c). Figure 6 Continued.
Discussion
In this pilot study it was found that, overall, medical students experience symptoms of MDD as defined by the DSM-5, both directly before and after medical school exams. This was not surprising, as prior research has shown that medical students experience high rates of development of symptoms of MDD around exams.15,34 This, along with a large body of research supporting that up to more than a quarter of medical students’ experience depression,1–5 made this conclusion not surprising, yet still alarming. It was also not surprising that female medical students in this study developed more symptoms of MDD compared to their male counterparts (Figures 3 and 4). This was also consistent with prior research,11–18,35 and once again highlights that gender disparities exist in medical students who are most likely to experience symptoms of MDD. This is important to recognize, as female medical students in recent years make up greater than 50% of all medical students matriculated at the US allopathic and osteopathic medical schools.36 In the current study, gender was looked at specifically, but understanding how symptoms of MDD affect minority populations and other underserved populations is an important next step.
We were surprised to discover that students experienced more symptoms of MDD before exams, which was statistically significant for all symptoms except for psychomotor agitation and suicidal ideation (Figure 2). We had hypothesized that medical students would experience more symptoms of MDD after exams as compared to before based on our previous study that showed that medical students experience high rates of depression directly after exams.15 In the prior study, comparisons of students’ symptoms of MDD before exams to those after was not addressed. Given that research has shown that symptoms of stress and anxiety in medical students are indeed related to academic pressures,37 it makes sense that the impending exam would increase these symptoms of MDD and distress before exams, and then perhaps the fatigue of preparing for and then taking the exam could contribute to symptom development after the exam.
In this pilot study, first- and second-year medical students, overall, experienced similar rates of development of symptoms of MDD around exams. Prior research is mixed, with some studies showing first-year students as more likely to develop symptoms of MDD, and that MDD symptoms decrease as students advance through the course of their medical education training.3 Other studies show that second-year medical students experience higher rates of development of symptoms of MDD compared to first-year students.38 These prior studies may suggest that when students experience more symptoms of MDD varies depending not only on gender but also on cultural context. This study was conducted in the US, and many other studies have been conducted outside the US.24,38 It was noteworthy that there were very few overall differences in symptoms of MDD between first- and second-year medical students possibly indicating that stress and academic pressure do not abate over the course of the first two years of medical school.
Overall, it is worth noting the alarming rate at which the medical students surveyed in this study experienced symptoms of MDD. As noted previously, both prior research and this study point to a substantial, and perhaps underreported, rate of development of symptoms of MDD among medical students. Additionally, there was a noteworthy number of medical students that experienced suicidal ideation both before and after exams, despite this number not reaching statistical significance (Figure 2). Given the statistically significant rates of MMD symptoms among first- and second-year medical students and the simple raw numbers of students experiencing suicidal ideation, it seems reasonable to suggest that not only is more in-depth research into the root causes of these problems needed but so too are systemic changes in how we operationalize medical education, ensuring that the mental health and wellbeing of medical students during the early years of medical education is emphasized.
Limitation
One limitation of this study was that it was done at one medical school in the US, limiting the sample size. Additionally, more female medical students responded to this study than male medical students. And overall response rates were often less than 30%. This was perhaps due to students’ unwillingness to participate in the survey, due to the sensitive nature of the questions. By making the survey anonymous this hopefully allowed students to answer the survey more honestly. Although, there were some low response rate we still feel that this pilot study is an important first step in looking at symptoms of depression around high stakes medical school exams, and warrants further investigation into this topic, to see if the above results are reproducible. Because we did see high rates of symptoms of MDD in the students who did participate in the survey, we are less inclined to think that students under-reported symptoms, but whether male medical students truly experience fewer symptoms of MDD compared to females, or if they are less likely to admit to such symptoms, even in an anonymous survey, is still unknown. This study only differentiated between self-identified male and female medical students and does not specifically address symptoms or differences among students who identify as non-binary or gender nonconforming. Given the well-documented rates of MDD among this population in general,39,40 it is worth exploring the specific effect of medical school exams on their mental health in future research. Additionally, we only surveyed students within a three-day period before and after exams, so we do not know what the lasting consequences of these symptoms are, or how long these symptoms truly exist both before and after exams. This was why symptoms of MDD was reported and not MDD itself because the 2-week requirement of symptoms to meet full criteria of MDD as the DSM-5 was not met in this study. We did not ask about other circumstances in the students’ lives, as other stressful situations outside of medical school exams could have contributed to the development of symptoms of MDD in these medical students. However, we do believe that enough students experienced symptoms of MDD for the effects alone to not be due to random chance.
Conclusion
Overall, first- and second-year medical students experience high rates of development of symptoms of MDD surrounding medical school exams. Medical students in this study were more likely to experience symptoms of MDD before exams as compared to after. Female medical students experienced symptoms of MDD at greater rates compared to their male counterparts. Second-year male medical students were the least likely to experience symptoms of MDD around exams in this study, however this finding may be limited by small sample size and other limitations as noted previously. This study demonstrates that high-stakes medical school exams can result in a significant emotional burden for students and underscores the importance of further research on this topic to elucidate how high-stakes examinations may contribute to the overall mental health of medical students as they progress through their training and enter the physician workforce.
Compliance with Ethical Standards
Two secure surveys were sent via university e-mail to first- and second-year medical students at the University of New England College of Osteopathic Medicine (UNECOM) in Biddeford, Maine, using the REDcap program. No minors were involved in the survey, so all participants were able to consent for themselves. A consent form was attached to each survey (please see additional document with submission labeled consent form). After reading the consent, the first question of the survey was: “Please read the attached Informed Consent Statement and choose if you would like to participate in the survey”. Participants were then asked to select yes or no (as noted in Figure 1a and 1b, and if they selected no, they were asked to not finish the survey. The survey remained anonymous. The survey was created by the authors and asked about the symptoms of major depressive disorder (MDD) as described in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). The consent form, survey, and research project were approved by the University of New England (UNE) IRB and is in compliance with the Declaration of Helsinki. All data were collected anonymously via REDcap.
Acknowledgment
An abstract of this paper was presented at the American Association of Colleges of Osteopathic Medicine Educating Leaders Conference 2022 as a virtual poster presentation in April 2022. The poster was published online: https://www.aacom.org/docs/default-source/aacom-awards/s2-2022_poster.pdf?sfvrsn=a6a0cacf_6
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors received no financial support for the research, writing of the manuscript, or publication of this work.
Disclosure
The authors declare no conflicts of interest in the research, authorship, or publication of this manuscript.
References
1. Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. J Am Med Assoc. 2016;316(21):2214–2236. doi:10.1001/jama.2016.17324
2. Mizra AA, Baig M, Beyari GM, Halawani MA, Mizra AA. Depression and Anxiety Among Medical Students: a Brief Overview. Adv Med Educ Practice. 2021;12:393–398. doi:10.2147/AMEP.S302897
3. Puthran R, Zhang MWB, Tam WW, Ho RC. Prevalence of depression amongst medical students a meta-analysis. Med Educ. 2016;50(4):456–468. doi:10.1111/medu.12962
4. Pokhrel NB, Khadayat R, Tulachan P. Depression, anxiety, and burnout among medical students and residents of a medical school in Nepal: a cross-sectional study. BMC Psychiatry. 2020;20:298. doi:10.1186/s12888-020-02645-6
5. Mao Y, Zhang N, Liu J, Zhu B, He R, Wang X. A systematic review of depression and anxiety in medical students in China. BMC Med Educ. 2019;19:327. doi:10.1186/s12909-019-1744-2
6. Dyrbe LN, West CP, Satele D, et al. Burnout among U.S medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–451. doi:10.1097/ACM.0000000000000134
7. Mousa OY, Dhamoon MS, Lander S, Dhamoon AS. The MD Blues: under-recognized depression and anxiety in medical trainees. PLoS One. 2016;11(6):e0156554. doi:10.1371/journal.pone.0156554
8. Quek TT, Tam WW, Tran BX, et al. The Global Prevalence of Anxiety Among Medical Students: a Meta-Analysis. Int J Environ Res Public Health. 2019;16(15):2735. doi:10.3390/ijerph16152735
9. Suarez DE, Cardozo AC, Ellmer D, Trujillo EM. Short report: cross sectional comparison of anxiety and depression symptoms in medical students and the general population in Colombia. Psychol Health Med. 2021;26(3):375–380. doi:10.1080/13548506.2020.1757130
10. National Institute of Mental Health. Prevalence of major depressive episode among adults. 2020. Available from: https://www.nimh.nih.gov/health/statistics/major-depression#:~:text=An%20estimated%2021.0%20million%20adults,compared%20to%20males%20(6.2%25).
11. Hardeman RR, Przedworski JM, Burke SE, et al. Mental well-being in first year medical students: a comparison by race and gender. J Racial Ethnic Health Disparities. 2015;2:403–413. doi:10.1007/s40615-015-0087-x
12. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S and Canadian medical students. Acad Med. 2006;81(4):354–373. doi:10.1097/00001888-200604000-00009
13. Basnet B, Jaiswal M, Adhikari B. Depression among undergraduate medical students. Kathmandu Univ Med J. 2012;10(39):56–59. doi:10.3126/kumj.v10i3.8021
14. Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross-sectional study. Med Educ. 2005;39(6):594–604. doi:10.1111/j.1365-2929.2005.02176.x
15. Arabatzis TJ, Marsidi J, Ashraf M, Supino C, Smith R. Gender disparities in symptoms of depression after medical school exams and student coping strategies for postexam depression symptoms. J Med Educ Curricular Dev. 2022;9:1–12. doi:10.1177/23821205211055391
16. Brenneisen Mayer F, Souza Santos I, Silveira PS, et al. Factors associated to depression and anxiety in medical students: a multicenter study. BMC Med Educ. 2016;16(1):282. doi:10.1186/s12909-016-0791-1
17. Azad N, Shahid A, Abbas N, Shaheen A, Munir N. Anxiety And Depression In Medical Students Of A Private Medical College. J Ayub Med Coll. 2017;29(1):123–127.
18. Jadoon NA, Yaqoob R, Raza A, Shehzad MA, Zeshan SC. Anxiety and depression among medical students: a cross-sectional study. J Pak Med Assoc. 2010;60(8):699–702.
19. Silva V, Costa P, Pereira I, et al. Depression in medical students: insights from a longitudinal study. BMC Med Educ. 2017;17(1):184. doi:10.1186/s12909-017-1006-0
20. Ahmadi J, Ahmadi N, Soltani F, Bayat F. Gender differences in depression scores of Iranian and German medical students. Iran J Psychiatry Behav Sci. 2014;8(4):70–73.
21. Halperin SJ, Henderson MN, Prenner S, Grauer JN. Prevalence of anxiety and depression among medical students during the COVID-19 pandemic: a Cross Sectional Study. J Med Educ Curricular Dev. 2021. doi:10.1177/2382120521991150
22. Nakhostin-Ansari A, Sherafati A, Aghajani F, Khonji MS, Aghajani R, Shahmansouri N. Depression and Anxiety among Iranian Medical Students during COVID-19 Pandemic. Iran J Psychiatry. 2020;15(3):228–235. doi:10.18502/ijps.v15i3.3815
23. Saraswathi I, Saikarthik J, Senthil Kumar K, Madhan Srinivasan K, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020;8:e10164. doi:10.7717/peerj.10164
24. Stefanovics EA, Rosenheck RA, He H, Ofori-Atta A, Cavalcanti M, Chiles C. Medical Student Beliefs and Attitudes Toward Mental Illness Across Five Nations. J Nerv Ment Dis. 2016;204(12):909–915. doi:10.1097/NMD.0000000000000610
25. Brazeau CMLR, Shanafelt T, Durning SJ, et al. Distress among matriculating medical students relative to the general population. Acad Med. 2014;89(11):1520–1525. doi:10.1097/ACM.0000000000000482
26. Rosal MC, Ockene IS, Ockene JK, Barrett SV, Ma Y, Hebert JR. A longitudinal study of students’ depression at one medical school. Acad Med. 1997;72(6):542–546.
27. Yusoff MS, Abdul Rahim AF, Baba AA, Ismail SB, Pa MN M, Esa AR. The impact of medical education on psychological health of students: a cohort study. Psychol Health Med. 2013;18(4):420–430. doi:10.1080/13548506.2012.740162
28. Levine RE, Litwins SD, Frye AW. An evaluation of depressed mood in two classes of medical students. Acad Psychiatry. 2006;30(3):235–237. doi:10.1176/appi.ap.30.3.235
29. Ludwig AB, Burton W, Weingarten J, Milan F, Myers DC, Kligler B. Depression and stress amongst undergraduate medical students. BMC Med Educ. 2015;15:141. doi:10.1186/s12909-015-0425-z
30. Givens JL, Tjia J. Depressed medical students’ use of mental health services and barriers to use. Acad Med. 2002;77(9):918–921. doi:10.1097/00001888-200209000-00024
31. Thompson G, McBride RB, Hosford CC, Halaas G. Resilience among medical students: the role of coping style and social support. Teach Learn Med. 2016;28(2):174–182. doi:10.1080/10401334.2016.1146611
32. Menon V, Sarkar S, Kumar S. Barriers to healthcare seeking among medical students: a cross sectional study from South India. Postgrad Med J. 2015;91(1079):477–482. doi:10.1136/postgradmedj-2015-133233
33. Ramadianto AS, Kusumadewi I, Agiananda F, Raharjanti NW. Symptoms of depression and anxiety in Indonesian medical students: association with coping strategy and resilience. BMC Psychiatry. 2022;22:92. doi:10.1186/s12888-022-03745-1
34. Thiemann P, Brimicombe J, Benson J, Quince T. When investigating depression and anxiety in undergraduate medical students timing of assessment is an important factor- a multicenter cross-sectional study. BMC Med Educ. 2020;20:125. doi:10.1186/s12909-020-02029-0
35. Pacheco JPG, Silveira JB, Ferreira RPC, et al. Gender inequality and depression among medical students: a global meta-regression analysis. J Psychiatr Res. 2019;111:36–43. doi:10.1016/j.jpsychires.2019.01.013
36. Morris DB, Gruppuso PA, McGee HA, Murillo AL, Grover A, Adashi EY. Diversity of the National Medical Student Body - Four Decades of Inequities. N Engl J Med. 2021;384(17):1661–1668. doi:10.1056/NEJMsr2028487
37. Azim SR, Baig M. Frequency and perceived causes of depression, anxiety and stress among medical students of a private medical institute in Karachi: a mixed method study. J Pak Med Assoc. 2019;69(6):840–845.
38. Ahmed I, Banu H, Al-Fageer R, Al-Suwaidi R. Cognitive emotions: depression and anxiety in medical students and staff. J Crit Care. 2009;24(3):e1–7. doi:10.1016/j.jcrc.2009.06.003
39. Gonzales G, Loret de Mola E, Gavulic KA, McKay T, Purcell C. Mental Health Needs Among Lesbian, Gay, Bisexual, and Transgender College Students During the COVID-19 Pandemic. J Adolesc Health. 2020;67(5):645–648. doi:10.1016/j.jadohealth.2020.08.006
40. Hershner S, Jansen EC, Gavidia R, Matlen L, Hoban M, Dunietz GL. Associations Between Transgender Identity, Sleep, Mental Health and Suicidality Among a North American Cohort of College Students. Nat Sci Sleep. 2021;13:383–398. doi:10.2147/NSS.S286131
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.