Back to Journals » Pragmatic and Observational Research » Volume 14
Adult Severe Asthma Registries: A Global and Growing Inventory
Authors Cushen B, Koh MS, Tran TN, Martin N, Murray R , Uthaman T, Goh CYY , Vella R , Eleangovan N, Bulathsinhala L, Maspero JF, Peters MJ, Schleich F , Pitrez P, Christoff G , Sadatsafavi M , Torres-Duque CA , Porsbjerg C, Altraja A, Lehtimäki L , Bourdin A , Taube C, Papadopoulos NG , Zsuzsanna C, Björnsdóttir U, Salvi S, Heffler E, Iwanaga T , al-Ahmad M , Larenas-Linnemann D , van Boven JF , Aarli BB, Kuna P, Loureiro CC, Al-lehebi R , Lee JH , Marina N, Bjermer L , Sheu CC , Mahboub B , Busby J, Menzies-Gow A, Wang E, Price DB
Received 6 February 2023
Accepted for publication 11 September 2023
Published 20 October 2023 Volume 2023:14 Pages 127—147
DOI https://doi.org/10.2147/POR.S399879
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Amrita Dosanjh
Breda Cushen,1,* Mariko Siyue Koh,2,* Trung N Tran,3 Neil Martin,3,4 Ruth Murray,5 Thendral Uthaman,6 Celine Yun Yi Goh,5,6 Rebecca Vella,7 Neva Eleangovan,5,6 Lakmini Bulathsinhala,5,6 Jorge F Maspero,8,9 Matthew J Peters,10 Florence Schleich,11 Paulo Pitrez,12 George Christoff,13 Mohsen Sadatsafavi,14 Carlos A Torres-Duque,15,16 Celeste Porsbjerg,17 Alan Altraja,18 Lauri Lehtimäki,19 Arnaud Bourdin,20 Christian Taube,21 Nikolaos G Papadopoulos,22,23 Csoma Zsuzsanna,24 Unnur Björnsdóttir,25 Sundeep Salvi,26 Enrico Heffler,27 Takashi Iwanaga,28 Mona al-Ahmad,29 Désirée Larenas-Linnemann,30 Job FM van Boven,31 Bernt Bøgvald Aarli,32,33 Piotr Kuna,34 Cláudia Chaves Loureiro,35,36 Riyad Al-lehebi,37 Jae Ha Lee,38 Nuria Marina,39 Leif Bjermer,40 Chau-Chyun Sheu,41,42 Bassam Mahboub,43 John Busby,44 Andrew Menzies-Gow,45 Eileen Wang,46 David B Price5,6,47 On behalf of ISAR Inventory Study Group
1Department of Respiratory Medicine, Beaumont Hospital, Dublin, Ireland; 2Department of Respiratory and Critical Care Medicine, Singapore General Hospital, Singapore, Singapore; 3AstraZeneca, Gaithersburg, MD, USA; 4Department of Respiratory Medicine, University of Leicester, Leicester, UK; 5Optimum Patient Care Global, Cambridge, UK; 6Observational Pragmatic Research Institute, Singapore, Singapore; 7Optimum Patient Care, Brisbane, Queensland, Australia; 8Clinical Research for Allergy and Respiratory Medicine, CIDEA Foundation, Buenos Aires, Argentina; 9University Career of Specialists in Allergy and Clinical Immunology at the Buenos Aires University School of Medicine, Buenos Aires, Argentina; 10Department of Thoracic Medicine, Concord Hospital, Sydney, Australia; 11CHU Sart-Tilman, GIGA I3, University of Liege, Liège, Wallonia, Belgium; 12Pulmonology Division, Hospital Santa Casa de Porto Alegre, Porto Alegre, Brazil; 13Faculty of Public Health, Medical University, Sofia, Bulgaria; 14Respiratory Evaluation Sciences Program, Faculty of Pharmaceutical Sciences, The University of British Columbia, Vancouver, Canada; 15CINEUMO, Respiratory Research Center, Fundación Neumológica Colombiana, Bogotá, Colombia; 16Universidad de La Sabana, Chia, Colombia; 17Department of Respiratory Medicine and Infectious Diseases, Research Unit, Bispebjerg Hospital, Copenhagen, Denmark; 18Department of Pulmonology, University of Tartu and Lung Clinic, Tartu University Hospital, Tartu, Estonia; 19Allergy Centre, Tampere University Hospital, Faculty of Medicine and Health Technology, Tampere University, Tampere, Finland; 20PhyMedExp, Univ Montpellier, CNRS, INSERM, CHU Montpellier, Montpellier, France; 21Department of Pulmonary Medicine, University Medical Center Essen-Ruhrlandklinik, Essen, Germany; 22Division of Infection, Immunity & Respiratory Medicine, University of Manchester, Manchester, UK; 23Allergy Department, 2nd Pediatric Clinic, University of Athens, Athens, Greece; 24Asthma Outpatient Clinic, National Koranyi Institute for Pulmonology, Budapest, Hungary; 25Department of Allergy and Respiratory Medicine, University Hospital, Reykjavik, Iceland; 26Pulmocare Research and Education Foundation, Pune, India; 27Personalized Medicine, Asthma and Allergy, IRCCS Humanitas Research Hospital, Rozzano, Milan, Italy; 28Kindai University Hospital, Osakasayama, Japan; 29Microbiology Department, College of Medicine, Kuwait University, Kuwait, Al-Rashed Allergy Center, Ministry of Health, Kuwait City, Kuwait; 30Centro de Excelencia en Asma y Alergia, Hospital Médica Sur, Ciudad de México, Mexico; 31University of Groningen, University Medical Center Groningen, Groningen Research Institute for Asthma and COPD (GRIAC), Department of Clinical Pharmacy & Pharmacology, Groningen, the Netherlands; 32Department of Thoracic Medicine, Haukeland University Hospital, Bergen, Norway; 33Department of Clinical Science, University of Bergen, Bergen, Norway; 34Division of Internal Medicine Asthma and Allergy, Medical University of Lodz, Lodz, Poland; 35Pneumology Unit, Hospitais da Universidade de Coimbra, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; 36Centre of Pneumology, Faculty of Medicine, University of Coimbra, Coimbra, Portugal; 37Department of Pulmonology, King Fahad Medical City, Riyadh, Saudi Arabia, Alfaisal University, Riyadh, Saudi Arabia; 38Division of Pulmonology and Critical Care Medicine, Department of Internal Medicine, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Republic of Korea; 39Pneumology Service, Biocruces, Cruces University Hospital, Barakaldo, Spain; 40Respiratory Medicine and Allergology, Department of Clinical Sciences, Skåne University Hospital, Lund University, Lund, Sweden; 41Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan; 42Department of Internal Medicine, School of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan; 43Rashid Hospital, Dubai Health Authority (DHA), Dubai, United Arab Emirates; 44Centre for Public Health, School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, Belfast, Northern Ireland, UK; 45Lung Division, Royal Brompton & Harefield Hospital, London, UK; 46Division of Allergy and Clinical Immunology, Department of Medicine, National Jewish Health and University of Colorado School of Medicine, Denver and Aurora, CO, USA; 47Centre of Academic Primary Care, Division of Applied Health Sciences, University of Aberdeen, Aberdeen, Scotland, UK
*These authors contributed equally to this work
Correspondence: David B Price, Observational and Pragmatic Research Institute (OPRI) Pte Ltd, 22 Sin Ming Lane, #06-76, Midview City, 573969, Singapore, Tel +65 3105 1489, Email [email protected]
Aim: The International Severe Asthma Registry (ISAR; http://isaregistries.org/) uses standardised variables to enable multi-country and adequately powered research in severe asthma. This study aims to look at the data countries within ISAR and non-ISAR countries reported collecting that enable global research that support individual country interests.
Methods: Registries were identified by online searches and approaching severe asthma experts. Participating registries provided data collection specifications or confirmed variables collected. Core variables (results from ISAR’s Delphi study), steroid-related comorbidity variables, biologic safety variables (serious infection, anaphylaxis, and cancer), COVID-19 variables and additional variables (not belonging to the aforementioned categories) that registries reported collecting were summarised.
Results: Of the 37 registries identified, 26 were ISAR affiliates and 11 non-ISAR affiliates. Twenty-five ISAR-registries and 4 non-ISAR registries reported collecting > 90% of the 65 core variables. Twenty-three registries reported collecting all optional steroid-related comorbidity variables. Twenty-nine registries reported collecting all optional safety variables. Ten registries reported collecting COVID-19 variables. Twenty-four registries reported collecting additional variables including data from asthma questionnaires (10 Asthma Control Questionnaire, 20 Asthma Control Test, 11 Asthma Quality of Life Questionnaire, and 4 EuroQol 5-dimension 5-level Questionnaire). Eight registries are linked to databases such as electronic medical records and national claims or disease databases.
Conclusion: Standardised data collection has enabled individual severe asthma registries to collect unified data and increase statistical power for severe asthma research irrespective of ISAR affiliations.
Keywords: Asia-Pacific, biologics, COVID-19, Europe, ISAR, International Severe Asthma Registry, oral corticosteroids, Registry, Middle East, Severe Asthma, Latin America, USA
Introduction
Severe asthma is defined as uncontrolled asthma despite adherence to optimised controller therapy and treatment of contributory factors, or that worsens when high-dose treatment is decreased.1 Although severe asthma is relatively rare, it deserves particular attention because it accounts for a substantial proportion of total asthma morbidity, mortality, and cost. For example, patients with severe asthma experience high exacerbation and hospitalisation rates, limitation of health-related quality of life, and high oral corticosteroid (OCS) burden.2–5 The increased cumulative incidence in all-cause adverse outcomes from OCS initiation has shown associations with greater healthcare resource utilisation and costs.6 A 2021 study in Spain estimated an individual cost of €758.70/exacerbation7 per patient, whereas a 2018 study in France estimated a mean annual asthma-related cost of €8222/year per patient.8 Moreover, a 2019 study from the US reported costs of patients receiving steps 4 and 5 of the GINA therapy of USD15,244/ year per patient on asthma-related healthcare.9 In fact, severe asthma accounts for over 50% of the costs attributed to asthma of all severities.2 Severe asthma is also clinically challenging to manage due to the extensive diagnostic and therapeutic interventions required for control and the need for personalised treatments.
To facilitate research and address the clinical challenges associated with managing severe asthma, several countries around the world such as Australia and New Zealand (Australasia),10 Germany,11 Italy,12–16 Netherlands, South Korea,17 Spain, United Kingdom,18–20 and the United States began to establish national or local severe asthma registries. In response to calls from both the World Health Organization21 and the Global Asthma Report22 for better surveillance of chronic respiratory diseases including severe asthma, the International Severe Asthma Registry (ISAR; http://isaregistries.org/) was established in 2017.23,24 ISAR is a global initiative and the largest adult severe asthma registry, currently including prospective data on 13,169 patients from 26 countries (as of October 2022). It was founded in partnership with national and regional severe asthma registries to act as a data custodian, storing standardised severe asthma data that can be shared for clinical and research purposes.23,25,26 At the outset of ISAR, variables that pre-existing registries report collecting were studied and compared; the observed variations in data quality and definitions of severe asthma globally highlighted the need for standardisation. The set of core variables to be collected by severe asthma registries, including those planning to contribute to ISAR was identified using a modified Delphi method (Table 1).25
 |
Table 1 List of ISAR’s Core and Optional Variables |
Once the core variables were standardised and collected by countries, ISAR-affiliated registries next started to collect optional steroid-related comorbidities and safety variables. Steroid-related comorbidity variables were collected in recognition of the increasing impact of systemic steroids in severe asthma and potential benefit of biologics in reducing steroid burden (Table 2). The safety variables are serious infections (eg, tuberculosis, pneumonia, meningitis, sepsis urinary tract infections), anaphylaxis, and cancer; these adverse events have been possibly associated with biologic initiation. Anti-immunoglobulin E (anti-IgE) and anti-interleukin 5/5 receptor (anti–IL-5/5R) therapies have been reported to show associations with anaphylaxis, indicating the need to monitor patients after administration of biologic treatment.27 Biologic therapy may also impair the body’s immune system and ability to respond to antigens, leading to increased risk of parasitic, bacterial, and viral infections.28,29 Additionally, as eosinophils are involved in immune responses against certain cancers, and as anti–interleukin (IL)-5/5R and anti–IL-4/13 treatments inhibit eosinophil maturation and activity, there is value in tracking the potential long-term cancer risk of biologic treatment in severe asthma.28
 |
Table 2 List of Identified Severe Asthma Registries Worldwide |
Severe asthma registries are collecting COVID-19 variables (eg, biomarker tests, respiratory symptoms, asthma outcomes, and COVID-19-related healthcare resource utilisation) as a result of the associated pandemic (Table 1). Although higher frequencies of COVID-19 in patients with asthma have not been identified,39 severe COVID-19 in patients with severe asthma is possible.40 Reports suggest hospitalised patients with severe asthma and COVID-19 infection have poorer outcomes, and biologics for severe asthma did not significantly impact COVID-19 outcomes.40
Many individual registries also reported collecting additional variables outside the scope of ISAR’s core and optional categories in accordance with their individual research interests. This shows the diversity and complexity of the management of patients with severe asthma globally.
Establishing standardised variables and classifying them according to appropriate themes provides greater consistency and depth of data on patients with severe asthma globally. Likewise, encouraging individual registries to collect additional variables increases the breadth of data being collected. Currently, the inter-registry variability in data being collected is unknown. Our paper aims to describe the current global severe asthma registry landscape by summarising the variables collected by each registry and how they align with those of ISAR, as well as the variables that are collected in addition. It is anticipated that surveying the consistency, depth, and breadth of variables collected by severe asthma registries worldwide will highlight the existing resources for managing and studying severe asthma.
Methods
Identification of Registries
Severe asthma registries contributing data to the ISAR initiative (ISAR-affiliated) and those collecting data independent of ISAR (non–ISAR-affiliated) were included in the present analysis. Individual local (those of local sites or hospitals), national (those of countries), and regional registries (the regional registry included in this study is that of Australia and New Zealand [Australasia]) were identified by a systematic online search (up to August 2022), and by approaching 36 severe asthma experts globally to identify active, though not yet published registries. PubMed, MEDLINE, EMBASE, Google Scholar, and Web of Science databases were queried using the following keywords and combinations thereof: “severe asthma”, “difficult asthma”, “therapy-resistant asthma”, “severe refractory asthma”, “uncontrolled asthma”, “registry”, “repository”, “database”, “clinical trial records” and “clinical health records”. Registries that qualified for inclusion were those that collected data on adult patients with asthma and required patients to have a confirmed diagnosis of severe asthma. A confirmed diagnosis of severe asthma was defined as receiving GINA 2018 step 5 therapy, or uncontrolled asthma receiving GINA 2018 step 4 therapy (Table 1).41 Registries that either collected data on children only, contained information only on specific asthma drugs, were general asthma registries, or were non-contactable were excluded. No registries that were invited refused participation.
Identification and Categorisation of Variables
Eligible registries opting to participate in the present study provided a list of variables they reported collecting in their case report forms or data collection specifications. In this manuscript, “reported” indicates past, current and/or planned data collection. Individual variables were then identified and assigned into one of three main categories: core variables (those identified in the ISAR-led Delphi study),25 steroid-related comorbidities / safety variables (“optional” as established by ISAR), and additional variables (any other variable collected by a registry, which does not meet the criteria for inclusion into the core or optional categories) (Table 1). In line with current events, some countries also reported collecting COVID-19 variables to determine COVID-19’s potential association with severe asthma (Table 1).
Assessment of Variables That Participating Registries Reported Collecting
Once categorised, the proportion of core variables that each registry reported collection of was calculated. The steroid-related comorbidities / safety variables, additional variables and COVID-19 variables that registries reported collecting were also summarised. In this manuscript, counts and percentages are presented to summarise data in tables and the Figure. In due course, ISAR will use any suitable statistics to analyse and report observational data according to STROBE guidance.42 Similarly, to conduct and report prediction models, whether for diagnostic or prognostic purposes, we will endorse TRIPOD guidance.43
Results
Identification of Registries
Thirty-seven individual registries from 35 different countries were identified. All 37 registries opted to participate in this study. Of the identified registries, 26 were ISAR affiliates and the remaining 11 were independent at the time of publication (Table 2). ISAR-affiliated registries were from Argentina, Australia and New Zealand (Australasia), Belgium, Bulgaria, Canada, Colombia, Denmark, Estonia, Greece, India, Ireland, Italy, Japan, Kuwait, Mexico, Poland, Portugal, Saudi Arabia, Singapore, South Korea, Spain, Sweden, Taiwan, United Arab Emirates, the United Kingdom, and the United States (National Jewish Health). Non–ISAR-affiliated registries as of September 2022 were from Belgium, Brazil, Finland, France, Germany (2 registries), Hungary, Iceland, Netherlands, Norway, and the United States (CHRONICLE). Characteristics of these registries, such as the numbers of centres and patients in each registry, have been outlined in Table 2.
Assessment of Core Variables That Registries Reported Collecting
Sixty-five Delphi-derived core variables were analysed25 (Table 1 and Supplementary Tables 1.1 and 1.2). The 95 variables in the ISAR Delphi publication were categorized and represented as 65 core variables in the tick table of this study. For example, the serum allergy test “positivity”, “result” and “date” were 3 separate variables in the ISAR Delphi publication, but were categorized as 1 core variable “serum allergy test” in the tick table of this study. The following 5 variables “exacerbation date, rescue steroid used (including dose and frequency), OCS dose and prescription dates, ICS dose and prescription dates, ICS+LABA dose and prescription dates” have been presented as core variables in the inventory manuscript (as per our CRF and data collection methods) but are considered effectiveness bolt-on variables in ISAR for contractual purposes.25 These 5 variables are not part of the core variable list from the Delphi study. Twenty-five ISAR-affiliated registries reported collection of all core variables (Figure 1). Five non–ISAR-affiliated registries reported collection of >90% of core variables, with the Brazil Severe Asthma Group (BraSA) and the United States (CHRONICLE) reporting collection of all core variables. Core variables that non–ISAR-affiliated registries were less likely to report collecting compared to ISAR-affiliated registries include rescue steroid (ie, OCS) information (55% [n = 6/11] of non–ISAR-affiliated registries, 92% [n = 24/26] of ISAR-affiliated registries), details of highest blood eosinophil count (BEC) not during an exacerbation (55% [n = 6/11] of non–ISAR-affiliated registries, 92% [n = 24/26] of ISAR-affiliated registries), exacerbation date (27% [n = 3/11] of non–ISAR-affiliated registries, 92% [n = 24/26] of ISAR-affiliated registries), bronchial provocation test (64% [n = 7/11] of non–ISAR-affiliated registries, 100% of ISAR-affiliated registries).
 |
Figure 1 Proportion of ISAR core variables that severe asthma registries worldwide report collecting. |
Assessment of Steroid-Related Comorbidities / Safety Variables That Registries Reported Collecting
Twenty-three of the 37 registries (19 ISAR-affiliated and 4 non–ISAR-affiliated) reported collecting all optional steroid-related comorbidity variables. 78% of registries (n = 29/37; 23 ISAR-affiliated and 6 non–ISAR-affiliated) reported collecting all optional safety variables (Table 3).
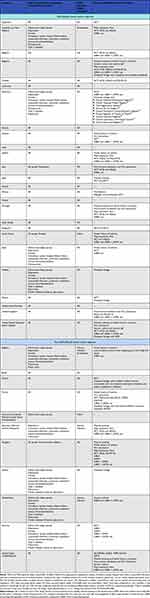 |
Table 3 Summary of ISAR Optional Variables and Key Non-ISAR Additional Variables That Severe Asthma Registries Worldwide Report Collecting |
Assessment of Additional Variables That Registries Reported Collecting
Key additional non-ISAR variables that registries reported collecting include information on family history of asthma, intensive care unit admissions, use of acute non-invasive ventilation, sputum culture, peak expiratory flow, patient-reported outcome measures (such as Asthma Control Test [ACT],53 Asthma Control Questionnaire [ACQ],54 Asthma Quality of Life Questionnaire [AQLQ],55 and EuroQol 5-dimension 5-level Questionnaire [EQ-5D-5L]),56 and database linkage (Table 3). In particular, 25 registries (18 ISAR affiliated and seven non–ISAR-affiliated) reported collecting data from patient-reported outcome measures (12 report collecting ACQ, 22 report collecting ACT, 12 report collecting AQLQ,55 and 4 report collecting EQ-5D-5L). Eight registries (five ISAR affiliated and three non–ISAR-affiliated) are linked or plan to be linked to databases such as hospital or clinic electronic medical records (EMRs), prescription databases, national disease databases, or national insurance databases (Table 3).
Assessment of COVID-19 Variables That Registries Reported Collecting
Since the beginning of the COVID-19 pandemic, ten registries (seven ISAR-affiliated and three non–ISAR-affiliated) reported collection of COVID-19 variables to determine COVID-19’s potential association with severe asthma outcomes. Variables that countries reported collecting include confirmation of COVID-19 infection, COVID-19 diagnostic tests, biomarker tests and results, respiratory symptoms, and changes in respiratory symptoms (if any) during a COVID-19 infection. All ISAR-affiliated registries also reported collecting data on key events such as exacerbations, hospitalisations, and emergency department visits during a COVID-19 infection, as well as data on COVID-19 treatments.
Discussion
The majority of severe asthma registries, regardless of ISAR affiliation, reported collection of >90% of ISAR’s core variables (Table 1). Most, if not all registries reported collecting safety variables and OCS comorbidity data (Table 3 and Supplementary Tables 1.1 and 1.2), reflecting a common goal of documenting OCS burden and safety events in patients. The registries’ use of patient-reported outcome measures demonstrates a shared goal of monitoring and quantifying patient outcomes, whereas the reported collection of COVID-19 variables reflects an aim of optimising severe asthma care and research. The collation of variables in a single tick table (Supplementary Tables 1.1 and 1.2) helps promote collaboration and communication across registries and the wider severe asthma community. Additionally, the practice of database linkage by Bulgaria, Denmark, Finland, France, Iceland, Sweden, Taiwan, and the United States (NJH) is beneficial as the access to data from EMRs and national databases (national claim databases, national prescription databases, etc) can improve the robustness of research involving people who have severe asthma (Table 3).
ISAR is the first global, collaborative effort to standardise and consolidate data collection across national and regional registries. The ability to collect a standardised set of variables while maintaining individuality enables registries to develop locally relevant research priorities and clinical interests.23 The extent of data collected also allows for ISAR to adapt to variations in definitions of disease and treatments, and consequently, flexibility in research. Further, ISAR’s data interoperability allows for pooling of data across 26 countries, contributing prospectively collected data for 13,169 patients (as of October 2022). Thus, ISAR is able to answer important research questions on severe asthma with sufficient statistical power.24 The collation of data into ISAR’s centralised repertoire enables the ENLIGHTEN research program with projects on the characterisation and care of patients with severe asthma, and the effectiveness of biologic therapy.57 ISAR’s first global publication describes the demographic and clinical features of patients with severe asthma, including variations in exacerbation rates and healthcare resource utilisation.3 Documenting such international variations can indicate gaps in care or differences in exposures and risk factors for asthma. Similarly, five distinct patient clusters with unique clinical characteristics were identified through biomarker expression in the BRISAR project, providing insights into the delivery of personalised medicine.58
ISAR creates opportunities to identify and improve the clinical management of patients with severe asthma. For example, the ISAR eosinophil gradient algorithm, which was built using ISAR data and expert consensus, identified 83.8% of patients to be likely eosinophilic (grade 3).59 However, there is possible bias towards eosinophilic phenotypes as some ISAR registries only recruit patients who are prescribed biologic therapies. ISAR’s research has also brought awareness to the effectiveness of biologics. For example, although both anti-IgE and anti–IL-5/5R therapies reduced exacerbations rates and long-term OCS daily dose in the FIRE study, anti–IL-5/5R therapy appeared to be more effective.60 The BEAM study will inform future work on response and predictors of response.61,62 Additionally, patients prescribed biologic therapies showed greater improvements in severe asthma outcomes than patients who continued high OCS exposure (HOCS) in the GLITTER study.63,64 These findings may influence guidelines to recommend biologics, even in patients showing improvement on OCS. The global variations in access to biologics illustrated by the BACS study should also be acknowledged.65 The PRISM study showed that comorbidities were associated with increased exacerbation rates in patients with severe asthma.66 Further research on the impact of biologics in patients with severe asthma and comorbidities is needed to inform the development of clinical guidelines.
Research from individual registries has also expanded the current understanding of severe asthma. Several population-based registries, including the Korean Severe Asthma Registry (KoSAR), the German Asthma Network (GAN) and the UK Severe Asthma Registry (UKSAR) have described the prevalence and characteristics of severe asthma in their respective countries.11,17,18 National registry data from countries including Belgium, Italy, and the UK have been used to quantify biologic use, exacerbations, BEC, OCS exposure, comorbidity prevalence, and investigate associations between biologics and asthma outcomes (eg, exacerbations and lung function decline).12,18,19,35
ISAR’s collaboration with other severe asthma registries has also influenced the development of current research agendas. The SUNNIE study used data from ISAR and CHRONICLE (USA) to describe biologic utilisation worldwide.67 CHRONICLE is a real-world, prospective, non-interventional cohort study of US specialist-treated patients with severe asthma.38 The SUNNIE study identified that three-quarters of patients remain on their first biologic treatment, and the most common switch is from anti-IgE to anti–IL-5/5R therapy.67
The key strength of the current study is that the named registries were collaborators, and freely shared their data collection specifications. Furthermore, the inventory of variables provided by this study could be a starting point for new severe asthma registries while enabling existing registries to identify potential gaps in their data collection. An additional strength of ISAR is flexibility to adapt to new variations in asthma definitions and treatments, such as treatable traits and the asthma-COPD overlap,68 and else.
The main limitation of this study is the difficulty in ascertaining the actual collection of variables (ie, the extent of missing data and whether they were systematic or random) and should be a feature of future research. Secondly, it is possible local severe asthma registries were not identified by the online search or severe asthma experts. Thirdly, the interpretation of data field names may differ slightly across countries, potentially affecting the study’s findings. Finally, the current study only analysed local, national or regional severe asthma registries; analyses of continental registries such as the pan-European Severe Heterogeneous Asthma Research Collaboration, Patient-centred (SHARP),69 were not included as per the ISAR protocol. Even though SHARP’s four primary aims “1) end dependency on systemic corticosteroids for asthma control, 2) enable access to severe asthma specialists for all people with severe asthma, 3) improve understanding of the heterogeneity of severe asthma mechanisms, and 4) seek to prevent the development of severe forms of asthma69 overlaps with ISAR’s vision for the future, analyses of continental registries were beyond the current study’s scope.
As a growing inventory, ISAR looks to welcome additional registries from the US that are based at the University of North Carolina and the University of Texas, San Antonio as well as registries from Malaysia and Ecuador in the near future. Meanwhile, to ensure future sustainability, severe asthma registries should continue to evolve through quality improvement initiatives. For example, ISAR’s interactive asthma reports that will be used by registries and patients will track the status of patients over time, enhancing their care. The ISAR tools are flexible and interactive, with a potential to produce asthma reports at the individual patient level or pooled by site, or by country for international comparisons. Individual countries have also employed quality improvement initiatives. In Canada, an algorithm to identify severe asthma in primary care EMRs based on Pan-Canadian Respiratory Standards Initiative for Electronic Health Record (PRESTINE) and core asthma elements were developed by experts using a modified Delphi process.70,71 Subsequently, PRESTINE developed severe asthma elements for specialists’ EMRs, and an algorithm to identify severe asthma using the core elements in primary care EMRs.70,71 In Denmark, the data collection platform for its severe asthma registry is a research database and medical record form.30 The Portuguese registry is linked to a mobile app that collects self-reported data (eg, sociodemographics, history of asthma, exacerbations, comorbidities, etc.) that are verified and validated by a physician before being saved to the registry’s database. Such knowledge translation and quality improvement initiatives also eliminate the need for dual data entry and enable evidence-based asthma management.
Conclusion
The ISAR initiative has fostered data standardisation across countries, improving the external validity and accuracy of severe asthma research. Irrespective of registries’ affiliations with ISAR, ISAR and individual registries complement each other. Allowing registries to retain ownership over their data enables an informed data collection process that serves local, regional, or national clinical needs and research interests. Importantly, knowledge gained from research outputs from severe asthma registries worldwide can inform local health policy, be incorporated into clinical guidelines, and be translated into quality improvement programs that enhance the care of asthma patients globally.
Ethics Statement
Registration of the ISAR database with the European Union Electronic Register of Post-Authorization studies was also undertaken (ENCEPP/DSPP/23720). ISAR has ethical approval from the Anonymised Data Ethics Protocols and Transparency (ADEPT) committee (ADEPT0218). All data collection sites in the International Severe Asthma Registry (ISAR) have obtained regulatory agreement in compliance with specific data transfer laws, country-specific legislation, and relevant ethical boards and organizations.
The ethics application process differs among participating registries/countries in ISAR. Within some registries, ethics approval is required at each individual satellite site, whereas for other collaborators, a central ethics committee can process applications on behalf of all satellite sites. Informed consent was obtained from patients where required to allow anonymised data sharing for approved research projects in ISAR.
The guidelines outlined in the Declaration of Helsinki were followed.
Acknowledgment
The authors would like to thank Mr Joash Tan (BSc, Hons) and Ms Andrea Lim (BSc, Hons) of the Observational Pragmatic Research Institute (OPRI) for their editorial and formatting assistance that supported the development of this publication. The ISAR Inventory Study Group listing can be found in Supplementary Table 2.
The author would also like to acknowledge the collaborators from the following countries, for their valuable contribution to the publication.
Australia and New Zealand
Ceri Banks, Phil Bardin, John Blakey, Chung Li Ping, Belinda Cochrane, Eve Jessica Denton, James Fingleton, Peter G. Gibson, Graham Hall, Nicole Hatten, Ezinne Igwe, Christine Jenkins, Gregory Katsoulotos, David Langton, Peter Middleton, Laura Mitchell, Paul Reynolds, Hayley See, Rachel Tan, John Upham.
Belgium
Guy G. Brusselle.
Bulgaria
Diana Hristova, Eleonora Stamenova, Violina Vasileva.
Canada
Shawn Aaron, Marie-Eve Boulay, Louis-Philippe Boulet, Kayla Cardoso, Andréanne Côté, Simon Couillard, Khushi Dabla, Jessie Dhillon, Jane Duke, Martine Duval, Cathy Fugere, Kylie Haydey, Angie Johnson, Amy May, Carrie McPhee, Lyle Melenka, Alison Morra, Ron Olivenstein, Shoshana Parker, Leeanne Parris, Kathy Vandemheen, Hélène Villeneuve, Laura Zunino.
Colombia
Patricia Parada, Benjamin Sarta-Moran, Briyith Ruiz, Abraham Ali-Munive, Mauricio González-García, Silvia Ramírez, Carolina Figueroa-Troncoso, Bellanid Rodríguez, Lucy Yaquelin Sánchez Durán, Diana Rey-Sanchez, Audrey Piotrostanalzki.
Denmark
Karin Dahl Assing, Anne-Sofie Bjerrum, Anna von Bulow, Ole Hilberg, Claus Rikard Johnsen, Niels Steen Krogh, Linda M Rasmussen, Johannes Schmid, Alexandra Wimmer-Aune.
France
Karima Bourayou, Lisa Gauquelin, Diakhou Ndao, Linda Thieulon, Yannick Vacher.
Germany
Stephanie Korn, Ina Haasler.
Greece
Christina Agapi Aggelopoulou, Petros Bakakos, Kostis Exarchos, Mina Gaga, Lampros Kalogiros, Maria Ntakoula, Giannis Paraskevopoulos, Fotis E Psarros, Agni Sioutkou, Lefteris Zervas.
India
Priyanka Dhumal, Swapnil Gadhave, Jyoti Narwadkar.
Ireland
Elaine MacHale, Patrick Mitchell.
Japan
Niimi Akio, Kana Hamada, Kubota Hironi, Fukuda Hironobu, Yoko Kajino, Mayumi Matsunaga, Yumi Matsuoka, Murakami MegumiRika, Hiroshi Mizutani, Kimiko Mori, Hiroshi Ohnishi, Kumiko Ota, Iwasaki Yoshikazu, Nakamura Youichi, Fujita Yuuji.
The Netherlands
Elisabeth Bel.
Norway
Sverre Lehmann.
Poland
Dorota Szydlowska.
Portugal
Inês Belchior, Carlos Lopes, Luís Amaral, Frederico Soares Regateiro, Wanda Videira.
Saudi Arabia
Walaa Abuzahra, Yahya Habis, Siraj Wali.
Singapore
The authors would like to acknowledge the support of The Academic Respiratory Initiative for Pulmonary Health (TARIPH). John Arputhan Abisheganaden, Eileen Chew, Tavleen Kaur Jaggi, Augustine Tee.
South Korea
Kwang Ha Yoo.
Spain
Borja G. Cosio, Luis Perez-de-Llano.
Sweden
Benita Björk, Alf Tunsäter, Casper Winsnes.
Taiwan
Ling-Yi Chang, Kuan-Yuan Chen, Joanna Chen, Shih-Lung Cheng, Kuo-Chin Chiu, Chu-Kuang Chou, Linkou Chang Gung, Liang-Wen Hang, Meng-Jer-Hsieh, Jeng-Yuan Hsu, Erick Wan-Chun Huang, Xu Cheng Hui, Shi Yi Jun, Ou Pei Jun, Hsin-Kuo Ko, Kang-Yun Lee, Ming-Shian Lin, Sheng-Hao Lin, Ching-Hsiung Lin, Shih-Feng Liu, Zheng Yu Qiao, Du Yi Rou, Diahn-Warng Perng, Lim Rong Ru, Wong Wan Ru, Fu Yun Rui, Sheng-Yeh Shen, Lee Xiao Ting, Hao-Chien Wang, Lee Shu Wen, Ng Jia Yi, Hong Yuan Zhen.
USA
Jennifer Brandorff, Amanda Grippen Goddard, Flavia Hoyte, Christena Kolakowski, Kanao Otsu, Pearlanne Zelarney, Joy Zimmer.
Funding
This study was conducted by the Observational and Pragmatic Research Institute (OPRI) Pte Ltd and was funded by Optimum Patient Care Global. No funding was received by the Observational & Pragmatic Research Institute Pte Ltd (OPRI) for its contribution.
Disclosure
Breda Cushen has received honoraria for lectures from AstraZeneca, Novartis and Boehringer Ingelheim. Mariko Siyue Koh reports grant support from AstraZeneca, and honoraria for lectures and advisory board meetings paid to her hospital (Singapore General Hospital) from GlaxoSmithKline, AstraZeneca, Novartis, Sanofi and Boehringer Ingelheim, outside the submitted work. Trung N. Tran is an employee of AstraZeneca, a co-funder of the International Severe Asthma Registry. Neil Martin is an employee of AstraZeneca, a co-funder of the International Severe Asthma Registry. Ruth Murray declares no relevant conflicts of interest in this work. Thendral Uthaman is an employee of the Observational and Pragmatic Research Institute (OPRI). OPRI conducted this study in collaboration with Optimum Patient Care and AstraZeneca. Celine Yun Yi Goh is an employee of Optimum Patient Care Global (OPCG), a co-funder of the International Severe Asthma Registry. Rebecca Vella is an employee of Optimum Patient Care, a co-funder of the International Severe Asthma Registry. Neva Eleangovan was an employee of the Observational and Pragmatic Research Institute (OPRI). OPRI conducted this study in collaboration with Optimum Patient Care and AstraZeneca. Lakmini Bulathsinhala is an employee of the Observational and Pragmatic Research Institute (OPRI). OPRI conducted this study in collaboration with Optimum Patient Care and AstraZeneca. Jorge F Maspero reports speaker fees, grants or advisory boards for AstraZeneca, Sanofi, GSK, Novartis, Inmunotek, Menarini, Noucor. Matthew J Peters declares personal fees and non-financial support from AstraZeneca and GlaxoSmithKline. Florence Schleich reports consultancy work for GSK, AstraZeneca, Sanofi - Advisory board, received speaker fees from GSK, AstraZeneca, Chiesi, Amgen, TEVA and research grants from GSK, AstraZeneca, Chiesi. Paulo Pitrez received fees as speaker or for consultations from GSK, AstraZeneca, Novartis, Sanofi, and Boehringer Ingelheim. George Christoff declares no relevant conflicts of interest in this work. Mohsen Sadatsafavi has received honoraria from AZ, BI, TEVA, and GSK for purposes unrelated to the content of this manuscript and has received research funding from AZ and BI directly into his research account from AZ for unrelated projects. Carlos A. Torres-Duque has received fees as advisory board participant and/or speaker from AstraZeneca, Boehringer-Ingelheim, GlaxoSmithKline, Novartis and Sanofi-Aventis; has taken part in clinical trials from AstraZeneca, Novartis and Sanofi-Aventis; has received unrestricted grants for investigator-initiated studies at Fundacion Neumologica Colombiana from AstraZeneca, Boehringer-Ingelheim, GlaxoSmithKline, Grifols and Novartis. Celeste Porsbjerg has attended advisory boards for AstraZeneca, Novartis, TEVA, and Sanofi-Genzyme; has given lectures at meetings supported by AstraZeneca, Novartis, TEVA, Sanofi-Genzyme, and GlaxoSmithKline; has taken part in clinical trials sponsored by AstraZeneca, Novartis, MSD, Sanofi-Genzyme, GlaxoSmithKline, and Novartis; and has received educational and research grants from AstraZeneca, Novartis, TEVA, GlaxoSmithKline, ALK, and Sanofi-Genzyme. Alan Altraja has received lecture fees from AstraZeneca, Berlin-Chemie Menarini, Boehringer Ingelheim, GlaxoSmithKline, MSD, Norameda, Novartis, Orion, Sanofi, and Zentiva; sponsorships from AstraZeneca, Berlin-Chemie Menarini, Boehringer Ingelheim, GlaxoSmithKline, MSD, Norameda, Novartis, and Sanofi; and has participated in advisory boards for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, Sanofi, and Teva. Lauri Lehtimäki has received personal fees from ALK, AstraZeneca, Boehringer Ingelheim, Chiesi, GSK, Menarini, Novartis, Orion Pharma and Sanofi. Arnaud Bourdin has received industry-sponsored grants from AstraZeneca-MedImmune, Boehringer-Ingelheim, Cephalon/Teva, GlaxoSmithKline, Novartis, Sanofi-Regeneron and consultancies with AstraZeneca-MedImmune, Boehringer-Ingelheim, GlaxoSmithKline, Novartis, Regeneron-Sanofi, Med-in-Cell, Actelion, Merck, Roche, and Chiesi. Christian Taube declares no relevant conflicts of interest in this work. Nikolaos G. Papadopoulos has been a speaker and/or advisory board member for Abbott, Abbvie, ALK, Asit Biotech, AstraZeneca, Biomay, Boehringer Ingelheim, GSK, HAL, Faes Farma, Medscape, Menarini, MSD, Mylan, Novartis, Nutricia, OM Pharma, Regeneron, Sanofi, Takeda, Viatris. He also reports research support from Capricare, Nestle, Numil, Vianex, and REG, outside the submitted work. Zsuzsanna Csoma declares no relevant conflicts of interest in this work. Unnur Bjornsdottir receives gratuities for lectures/presentations from AstraZeneca, Sanofi and Novartis. Sundeep Salvi declares research support and speaker fees from Cipla, Glenmark, GSK. Enrico Heffler declares personal fees from: Sanofi, Regeneron, GSK, Novartis, Astrazeneca, Stallergenes, Circassia. Takashi Iwanaga received lecture fees from Kyorin, GlaxoSmithKline, Novartis, Boehringer Ingelheim and AstraZeneca. Mona Al-Ahmad has received advisory board and speaker fees from AstraZeneca, Sanofi, Novartis, and GlaxoSmithKline. Received a grant from Kuwait Foundation for the Advancement of Sciences (KFAS). Désirée Larenas Linnemann reports personal fees from Allakos, Amstrong, AstraZeneca, Bayer, Chiesi, DBV Technologies, Grunenthal, GSK, Mylan/Viatris, Menarini, MSD, Novartis, Sanofi, Siegfried, UCB, Carnot, grants from Sanofi, Lilly, Pfizer, Abbvie, AstraZeneca, Novartis, Circassia, UCB, GSK, Purina institute, outside the submitted work. She also reports speaker’s bureau, safety board, Advisory board for ALK, Allakos, Amstrong, Astrazeneca national and global, Bayer, Chiesi, Grunenthal, Grin, GSK national and global, Viatris, Menarini, MSD, Novartis, Pfizer, Sanofi, Siegfried, UCB, Carnot; support with congresses from Abbvie, Lilly, Sanofi, Astrazeneca, Pfizer, Novartis, GSK, Purina institute. Job F.M. Van Boven received grants and/or consultancy fees from AstraZeneca, Chiesi, European Commission COST (COST Action 19132), GSK, Lung Alliance Netherlands, Novartis, Teva, and Trudell Medical, outside the submitted work and all paid to his institution. Bernt Bøgvald Aarli reports grants from Boehringer Ingelheim during the conduct of the study and personal fees from Boehringer Ingelheim, AstraZeneca, GSK, Sanofi-Aventis Norway, Chiesi, Boehringer Ingelheim, and Novartis Norway, outside the submitted work. Piotr Kuna reports personal fees from Adamed, AstraZeneca, Berlin Chemie Menarini, Celon Pharma, Chiesi, FAES, Glenmark, GSK, Novartis, Polpharma, Boehringer Ingelheim, Sandoz, Teva, Zentiva, outside the submitted work. Cláudia Chaves Loureiro declares research Grant (P.I., collaborator or consultant: AstraZeneca, GSK; Speakers Bureau / Honoraria: AstraZeneca, GSK, Novartis, Teva, Sanofi; Consultant / advisory board: AstraZeneca, Bial, GSK, Jaba Recordatti, Novartis, Teva, Sanofi. Riyad Al-Lehebi has given lectures at meetings supported by AstraZeneca, Boehringer Ingelheim, Novartis, GlaxoSmithKline, and Sanofi, and participated in advisory board fees from GlaxoSmithKline, AstraZeneca, Novartis, Abbott. Jae Ha Lee declares no conflicts of interest in this work. Nuria Marina Malanda reports grants, personal fees and non-financial support from AstraZeneca, GSK, Teva, Novartis, Sanofi, and Pfizer, outside the submitted work. Leif Bjermer has (in the last three years) received lecture or advisory board fees from Alk-Abello, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Mundipharma, Novartis, Sanofi, Genzyme/Regeneron, and Teva. Chau-Chyun Sheu has received speaker fees from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis and Pfizer, and has acted as an investigator for trials sponsored by AstraZeneca, Novartis, Roche, Sanofi-Regeneron, Galapagos, Shionogi, Aridis, Bristol Myers Squibb, Insmed and Horizon Therapeutics. Bassam Mahboub reports no conflicts of interest in this work. John Busby has received personnel from NurvAir. Andrew N. Menzies-Gow has attended advisory boards for AstraZeneca, GlaxoSmithKline, Novartis, Regeneron, Sanofi and Teva, and has received speaker fees from AstraZeneca, Novartis, Teva and Sanofi. He has participated in research with AstraZeneca for which his institution has been remunerated and has attended international conferences with Teva. He has had consultancy agreements with AstraZeneca and Sanofi. Eileen Wang has received honoraria from AstraZeneca, GlaxoSmithKline, Wefight, and Clinical Care Options. She has been an investigator on studies sponsored by AstraZeneca, GlaxoSmithKline, Genentech, Sanofi and Sema4, Novartis, and Teva, for which her institution has received funding. David B Price has advisory board membership with AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Viatris, Teva Pharmaceuticals; consultancy agreements with AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, Viatris, Teva Pharmaceuticals; grants and unrestricted funding for investigator-initiated studies (conducted through Observational and Pragmatic Research Institute Pte Ltd) from AstraZeneca, Chiesi, Viatris, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, UK National Health Service; payment for lectures/speaking engagements from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Commute Digital, Medscape, Viatris, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, Teva Pharmaceuticals; payment for the development of educational materials from Mundipharma, Novartis; payment for travel/accommodation/meeting expenses from AstraZeneca, Boehringer Ingelheim, Novartis, Medscape, Viatris, Teva Pharmaceuticals; stock/stock options from AKL Research and Development Ltd which produces phytopharmaceuticals; owns 74% of the social enterprise Optimum Patient Care Ltd (Australia and UK) and 92.61% of Observational and Pragmatic Research Institute Pte Ltd (Singapore); 5% shareholding in Timestamp which develops adherence monitoring technology; is peer reviewer for grant committees of the UK Efficacy and Mechanism Evaluation programme, and Health Technology Assessment; and was an expert witness for GlaxoSmithKline.
References
1. Reddel HK, Bacharier LB, Bateman ED, et al. Global Initiative for Asthma (GINA) Strategy 2021 - executive summary and rationale for key changes. Eur Respir J. 2021;205. doi:10.1183/13993003.02730-2021
2. Godard P, Chanez P, Siraudin L, Nicoloyannis N, Duru G. Costs of asthma are correlated with severity: a 1-yr prospective study. Eur Respir J. 2002;19:61–67. doi:10.1183/09031936.02.00232001
3. Wang E, Wechsler ME, Tran TN, et al. Characterization of severe asthma worldwide: data from the International Severe Asthma Registry. Chest. 2020;157:790–804. doi:10.1016/j.chest.2019.10.053
4. Bourdin A, Fabry-Vendrand C, Ostinelli J, et al. The burden of severe asthma in France: a case-control study using a medical claims database. J Allergy Clin Immunol Pract. 2019;7:1477–1487. doi:10.1016/j.jaip.2018.12.029
5. McDonald VM, Hiles SA, Jones KA, Clark VL, Yorke J. Health-related quality of life burden in severe asthma. Med J Aust. 2018;209:S28–S33. doi:10.5694/mja18.00207
6. Voorham J, Xu X, Price DB, et al. Healthcare resource utilization and costs associated with incremental systemic corticosteroid exposure in asthma. Allergy. 2019;74:273–283. doi:10.1111/all.13556
7. Quirce S, Melero C, Huerta A, Uría E, Cuesta M. Economic impact of severe asthma exacerbations in Spain: multicentre observational study. J Asthma. 2021;58:207–212. doi:10.1080/02770903.2019.1674330
8. Nordon C, Grimaldi-Bensouda L, Pribil C, et al. Clinical and economic burden of severe asthma: a French cohort study. Respir Med. 2018;144:42–49. doi:10.1016/j.rmed.2018.10.002
9. Settipane RA, Kreindler JL, Chung Y, Tkacz J. Evaluating direct costs and productivity losses of patients with asthma receiving GINA 4/5 therapy in the United States. Ann Allergy Asthma Immunol. 2019;123:564–572.e3. doi:10.1016/j.anai.2019.08.462
10. McDonald VM, Hiles SA, Godbout K, et al. Treatable traits can be identified in a severe asthma registry and predict future exacerbations. Respirology. 2019;24:37–47. doi:10.1111/resp.13389
11. Korn S, Milger K, Skowasch D, et al. The German severe asthma patient: baseline characteristics of patients in the German Severe Asthma Registry, and relationship with exacerbations and control. Respir Med. 2022;195:106793. doi:10.1016/j.rmed.2022.106793
12. Malipiero G, Paoletti G, Blasi F, et al. Clinical features associated with a doctor-diagnosis of bronchiectasis in the Severe Asthma Network in Italy (SANI) registry. Expert Rev Respir Med. 2021;15:419–424. doi:10.1080/17476348.2021.1840983
13. Heffler E, Blasi F, Latorre M, et al. The severe asthma network in Italy: findings and perspectives. J Allergy Clin Immunol. 2019;7:1462–1468. doi:10.1016/j.jaip.2018.10.016
14. Canonica GW, Blasi F, Paggiaro P, et al. Oral CorticoSteroid sparing with biologics in severe asthma: a remark of the Severe Asthma Network in Italy (SANI). World Allergy Organ J. 2020;13:100464. doi:10.1016/j.waojou.2020.100464
15. Canonica GW, Malvezzi L, Blasi F, et al. Chronic rhinosinusitis with nasal polyps impact in severe asthma patients: evidences from the Severe Asthma Network Italy (SANI) registry. Respir Med. 2020;166:105947. doi:10.1016/j.rmed.2020.105947
16. Puggioni F, Brussino L, Canonica GW, et al. Frequency of tiotropium bromide use and clinical features of patients with severe asthma in a real-life setting: data from the Severe Asthma Network in Italy (SANI) Registry. JAA. 2020;13:599–604. doi:10.2147/JAA.S274245
17. Kim S-H, Lee H, Park S-Y, et al. The Korean Severe Asthma Registry (KoSAR): real world research in severe asthma. Korean J Intern Med. 2022;37:249–260. doi:10.3904/kjim.2021.403
18. Jackson DJ, Busby J, Pfeffer PE, et al. Characterisation of patients with severe asthma in the UK Severe Asthma Registry in the biologic era. Thorax. 2021;76:220–227. doi:10.1136/thoraxjnl-2020-215168
19. Yang F, Busby J, Heaney LG, et al. Factors Associated with Frequent Exacerbations in the UK Severe Asthma Registry. J Allergy Clin Immunol Pract. 2021;9:2691–2701.e1. doi:10.1016/j.jaip.2020.12.062
20. Newby C, Heaney LG, Menzies-Gow A, et al. Statistical cluster analysis of the British Thoracic Society Severe refractory Asthma Registry: clinical outcomes and phenotype stability. PLoS One. 2014;9:e102987. doi:10.1371/journal.pone.0102987
21. World Health Organization. Asthma: WHO’s role and activities. Available from: https://www.who.int/respiratory/asthma/activities/en/.
22. Global Asthma Network. The global asthma report; 2018. Available from: http://www.globalasthmareport.org/Global%20Asthma%20Report%202018%20EMBARGOED.pdf.
23. FitzGerald JM, Tran TN, Alacqua M, et al. International severe asthma registry (ISAR): protocol for a global registry. BMC Med Res Methodol. 2020;20:212. doi:10.1186/s12874-020-01065-0
24. Canonica GW, Alacqua M, Altraja A, et al. International Severe Asthma Registry. Chest. 2020;157:805–814. doi:10.1016/j.chest.2019.10.051
25. Bulathsinhala L, Eleangovan N, Heaney LG, et al. Development of the International Severe Asthma Registry (ISAR): a Modified Delphi Study. J Allergy Clin Immunol Pract. 2019;7:578–588.e2. doi:10.1016/j.jaip.2018.08.016
26. Dharmage SC, Bui DS, Perret J, Lowe A, Lodge C. A step in the right direction: harmonizing measures for use in asthma patient registries. J Allergy Clin Immunol. 2019;144(3):663–664. doi:10.1016/j.jaci.2019.07.005
27. Li L, Wang Z, Cui L, et al. Anaphylactic risk related to omalizumab, benralizumab, reslizumab, mepolizumab, and dupilumab. Clin Transl Allergy. 2021;11(4):e12038. doi:10.1002/clt2.12038
28. Wechsler ME, Munitz A, Ackerman SJ, et al. Eosinophils in health and disease: a State-of-the-Art review. Mayo Clin Proce. 2021;96:2694–2707.
29. Tan LD, Schaeffer B, Alismail A. Parasitic (Helminthic) Infection While on Asthma Biologic Treatment: not Everything Is What It Seems. J Asthma Allergy. 2019;12:415–420. doi:10.2147/JAA.S223402
30. Hansen S, Hilberg O, Ulrik CS, et al. The Danish severe asthma register: an electronic platform for severe asthma management and research. Eur Clin Respir J. 2021;8:1842117. doi:10.1080/20018525.2020.1842117
31. Iwanaga T, Tohda Y. Importance of clinical epidemiology research in studies on respiratory diseases. Respir Investig. 2013;51(4):217–223. doi:10.1016/j.resinv.2013.04.003
32. Sunadome H, Matsumoto H, Petrova G, et al. IL4Rα and ADAM33 as genetic markers in asthma exacerbations and type-2 inflammatory endotype. Clin Exp Allergy. 2017;47(8):998–1006. doi:10.1111/cea.12927
33. Matsumoto H, Kanemitsu Y, Nagasaki T, et al. Staphylococcus aureus enterotoxin sensitization involvement and its association with the CysLTR1 variant in different asthma phenotypes. Ann Allergy Asthma Immunol. 2017;118:197–203.
34. Sá-Sousa A, Fonseca JA, Pereira AM, et al. The Portuguese Severe Asthma Registry: development, features, and data sharing policies. Biomed Res Int. 2018;2018:1–12. doi:10.1155/2018/1495039
35. Graff S, Brusselle G, Hanon S, et al. Anti–Interleukin-5 therapy is associated with attenuated lung function decline in severe eosinophilic asthma patients from the Belgian Severe Asthma Registry. J Allergy Clin Immunol. 2022;10(2):467–477. doi:10.1016/j.jaip.2021.09.023
36. Schleich F, Brusselle G, Louis R, et al. Heterogeneity of phenotypes in severe asthmatics. The Belgian Severe Asthma Registry (BSAR). Respir Med. 2014;108(12):1723–1732. doi:10.1016/j.rmed.2014.10.007
37. Hanon S, Brusselle G, Deschampheleire M, et al. COVID-19 and biologics in severe asthma: data from the Belgian Severe Asthma Registry. Eur Respir J. 2020;56(6):2002857. doi:10.1183/13993003.02857-2020
38. Ambrose CS, Chipps BE, Moore WC, et al. The CHRONICLE Study of US adults with subspecialist-treated severe asthma: objectives, design, and initial results. POR. 2020;11:77–90. doi:10.2147/POR.S251120
39. Hansen ESH, Moeller AL, Backer V, et al. Severe outcomes of COVID-19 among patients with COPD and asthma. ERJ Open Res. 2021;7:00594–02020. doi:10.1183/23120541.00594-2020
40. Lombardi C, Gani F, Berti A, et al. Asthma and COVID-19: a dangerous liaison? Asthma Res Pract. 2021;7(9). doi:10.1186/s40733-021-00075-z
41. Global Initiative for Asthma (GINA). GINA Difficult-to-treat and severe asthma in adolescent and adult patients - Diagnosis and management; 2018. Available from: https://ginasthma.org/wp-content/uploads/2018/11/GINA-SA-FINAL-wms.pdf.
42. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi:10.1016/j.jclinepi.2007.11.008
43. Moons KGM, Altman DG, Reitsma JB, et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med. 2015;162:W1–W73. doi:10.7326/M14-0698
44. Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, et al. Data Resource Profile: the Danish National Prescription Registry. Int J Epidemiol. 2016:dyw213. doi:10.1093/ije/dyw213
45. Schmidt M, Schmidt SA, Sandegaard JL, et al. The Danish National Patient Registry: a review of content, data quality, and research potential. CLEP. 2015;449–490. doi:10.2147/CLEP.S91125
46. Schmidt M, Pedersen L, Sørensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
47. Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health. 2011;39(7_suppl):42–45. doi:10.1177/1403494810393562
48. Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(7_suppl):54–57. doi:10.1177/1403494810395825
49. Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health. 2011;39(7_suppl):26–29. doi:10.1177/1403494811399958
50. Baadsgaard M, Quitzau J. Danish registers on personal income and transfer payments. Scand J Public Health. 2011;39(7_suppl):103–105. doi:10.1177/1403494811405098
51. Grann AF, Erichsen R, Nielsen AG, Frøslev T, Thomsen R. Existing data sources for clinical epidemiology: the clinical laboratory information system (LABKA) research database at Aarhus University, Denmark. CLEP. 2011;133. doi:10.2147/CLEP.S17901
52. Jensen VM, Rasmussen AW. Danish education registers. Scand J Public Health. 2011;39(7_suppl):91–94. doi:10.1177/1403494810394715
53. Schatz M, Sorkness CA, Li JT, et al. Asthma control test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117:549–556. doi:10.1016/j.jaci.2006.01.011
54. Juniper EF, O′byrne PM, Guyatt GH, Ferrie PJ, King D. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14(4):902. doi:10.1034/j.1399-3003.1999.14d29.x
55. QolTech. Measurement of health-related quality of life and asthma control. Available from: https://www.qoltech.co.uk/aqlq.html.
56. EuroQol Research Foundation. EQ-5D-5L. Available from: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/.
57. Paoletti G, Pepys J, Casini M, et al. Biologics in severe asthma: the role of real-world evidence from registries. Eur Respir Rev. 2022;31:210278. doi:10.1183/16000617.0278-2021
58. Denton E, Price DB, Tran TN, et al. Cluster analysis of inflammatory biomarker expression in the International Severe Asthma Registry. J Allergy Clin Immunol. 2021;9:2680–2688.e7. doi:10.1016/j.jaip.2021.02.059
59. Heaney LG, Perez de Llano L, Al-Ahmad M, et al. Eosinophilic and Noneosinophilic Asthma. Chest. 2021;160:814–830. doi:10.1016/j.chest.2021.04.013
60. Ali N, Lyu J, Newell A, et al. Comparative effectiveness of anti-IL5/5R versus Anti-IgE in patients eligible for both (FIRE). In:
61. Pérez De Llano L, Cepelis A, Tran T, et al. Baseline characteristics of severe asthma patients initiating biologic treatment worldwide. In: Monitoring Airway Disease. European Respiratory Society; 2021:PA1106. doi:10.1183/13993003.congress-2021.PA1106
62. ISAR. Data on file for BEAM project (Understanding response and non-response to biologics); 2022.
63. Chen W, Sadatsafavi M, Bulathsinhala L, et al. Characterisation of severe, steroid-dependent asthma patients who initiate biologics versus those who do not. In: Monitoring Airway Disease. European Respiratory Society; 2021:PA1105. doi:10.1183/13993003.congress-2021.PA1105
64. Chen WJ, Sadatsafavi M, Bulathsinhala L, et al. Characterisation of severe, steroid-dependent asthma patients who initiate biologics versus those who do not. In:
65. Porsbjerg CM, Menzies-Gow AN, Tran TN, et al. Global variability in administrative approval prescription criteria for biologic therapy in severe asthma. J Allergy Clin Immunol. 2022;10(5):1202–1126. doi:10.1016/j.jaip.2021.12.027
66. Scelo G, Porsbjerg CM, Carter V, et al. Prevalence of comorbidities in adults with severe asthma: results from the International Severe Asthma Registry (ISAR). In:
67. Menzies-Gow AN, McBrien C, Unni B, et al. Real world biologic use and switch patterns in severe asthma: data from the International Severe Asthma Registry and the US CHRONICLE Study. JAA. 2022;15:63–78. doi:10.2147/JAA.S328653
68. Barnes PJ. Asthma-COPD Overlap. Chest. 2016;149(1):7–8. PMID: 26757281. doi:10.1016/j.chest.2015.08.017
69. Djukanovic R, Adcock IM, Anderson G, et al. The Severe Heterogeneous Asthma Research Collaboration, Patient-centred (SHARP) ERS Clinical Research Collaboration: a new Dawn in asthma research. Eur Respir J. 2018;52(5):1801671. doi:10.1183/13993003.01671-2018
70. Lougheed MD, Taite A, ten Hove J, et al. Pan-Canadian asthma and COPD standards for electronic health records: a Canadian Thoracic Society Expert Working Group Report. Can J Respir Crit Care Sleep Med. 2018;2:244–250. doi:10.1080/24745332.2018.1517623
71. Lougheed MD, Morra A, Bullock E, et al. Pan-Canadian standards for severe asthma in electronic medical records. Can J Respir Crit Care Sleep Med. 2021;5:391–399. doi:10.1080/24745332.2021.1947758
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
