Back to Journals » Advances in Medical Education and Practice » Volume 14
Anterior Cruciate Ligament Stability in Soft-Embalmed Cadaver vs In vivo Knee: Alternative Approaches to Medical Education
Authors Millar WA , Armstrong LR , Becker RM, Musick AN, Ryan DB, Kwasigroch TE
Received 13 August 2023
Accepted for publication 1 November 2023
Published 10 November 2023 Volume 2023:14 Pages 1279—1284
DOI https://doi.org/10.2147/AMEP.S435207
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
William A Millar, Landon R Armstrong, Robert M Becker, Adam N Musick, David B Ryan, Thomas E Kwasigroch
Department of Medical Education, James H. Quillen College of Medicine, East Tennessee State University, Johnson City, TN, USA
Correspondence: Thomas E Kwasigroch, Department of Medical Education, James H. Quillen College of Medicine, PO Box 70582, Johnson City, TN, 37614, USA, Tel +1 (423) 239-2006, Email [email protected]
Introduction: Soft-embalmed cadavers have been used in medical education with a variety of success in different curriculum objectives. In the United States, the ACL is the most commonly injured ligament. Yet, there has been little focus on the stability of the knee in the sagittal plane provided by the anterior cruciate ligament within the soft-embalmed cadaver model. If the soft-embalmed cadaver ligaments contain similar elastic properties as an in-vivo knees, this will offer yet another means for further advancements in medical education to detect and assess musculoskeletal injuries.
Purpose: Evaluate how similarly the anterior tibial translation of soft-embalmed cadaver anterior cruciate ligaments compares to in-vivo tissue.
Methods: The KT-1000 arthrometer was used to assess the laxity of the anterior cruciate ligament of thirteen soft-embalmed cadavers consisting of five females and eight males with a mean age of 79.3 years and duration of time since embalming ranging from 250 to 1156 days. Anterior displacement of the tibia in relation to the femur was registered at 67N and 89N. The soft-embalmed cadaver measurements were compared against twenty-one healthy uninjured individuals whose anterior tibial translation was measured using the same process. Data sets were analyzed using a welch two-sample t-test to determine the similarity between the means of the data sets.
Results: The t-tests proved a significant difference between live and soft-embalmed cadaver knees. The anterior tibial translation in the set of healthy live knees directly compared to the soft-embalmed cadaver group for 67N depicts an average difference of 1.76mm. The same comparison at 89N depicts an average difference of 2.12mm.
Conclusion: While soft-embalmed cadavers may not directly replicate ATT to an exact number to that of in vivo tissue, they still allow the perception of the tibial translation against a stationary femur. The difference is less than 2.5 mm in both data sets when compared to an in-vivo knee, equivalent to one-tenth of an inch. Suggesting the viability of soft-embalmed cadavers ATT and should not exclude their use in medical education.
Keywords: medical education, anatomy, anterior cruciate ligament, soft-embalmed cadaver
Introduction
The Thiel embalming method, originally developed and honed by Professor Walter Thiel in Austria, has been an increasingly popular training technique in the fields of science and medicine. This system has been fine-tuned since its inception and pivotal publication in 1992.1,2 The embalming solution used in our cadaver model is Surgical Reality Fluid (Trinity Fluids, Harsens Island, MI, United States). This method involves a soft cure anatomical, non-formaldehyde embalming chemical designed to keep a cadaver soft with true organ colors and full body malleability. Surgical reality fluid is similar in composition to the original Thiel formula using an ethanol-based solution. However, it’s an injection solution rather than a submersion process. This method logistically benefits universities and medical research center by eliminating the necessity of on-site tank submersion equipment. This is accomplished without compromising the many benefits associated with the soft-embalming process that have emerged over the past three decades. Fresh frozen cadavers and soft-embalmed cadavers are both used for biomechanical anatomical research. Yet, soft-embalmed cadavers present a much longer duration of anatomical stability as well as a decreased chance of cadaver infection.3
Soft-embalmed cadavers have been used in medical education and have had a variety of successes with different curriculum objectives. These avenues consist of ultrasound-guided anesthetics, laparoscopic surgery, thyroidectomy, and orthopedic surgery. More recently, medical equipment such as laryngoscopes and joint replacements have been tested on soft-embalmed cadavers.4
Soft-embalmed cadavers are proving to have lifelike qualities amongst many experts. The World Journal of Surgery collected opinions of 27 surgeons in an array of specialties, demonstrating surgeons deem these cadavers comparable to live tissue excluding the brain and eyes.5 Soft-embalmed cadaver’s were also proven to display similar stiffness of the medial and laterally collateral ligaments in both tissue and ligament stability.6
While previous research has shown success in demonstrating the stability of the knee in the coronal plane within soft-embalmed cadavers, there has been little focus on the stability of the knee in the sagittal plane provided by the anterior cruciate ligament (ACL). The ACL is still the most commonly injured ligament in the United States with a recent study demonstrating an incidence of 68.6 people per 100,000.7,8 If the soft-embalmed cadaver ligaments contain similar elastic properties as an in vivo knees, this will offer yet another means for further advancements in medical education training to detect and assess musculoskeletal injuries.
The KT-1000 is one of the most consistently used arthrometers and is the “gold standard” for the measurement of anterior tibial translation (ATT).9 This experiment aims to evaluate how similarly the ATT of soft-embalmed cadaver ACLs compare to in-vivo tissue.
Materials and Methods
Cohort
The study cohort consisted of 13 soft-embalmed cadavers, five being female and eight being male. The average age of the donor at the time of embalming was 79.3 years. Days embalmed ranged from 250 to 1156 days. The donors were thoroughly examined and inspected to ensure no surgical lacerations or scars were apparent distal to the iliac crest bilaterally. Those who did not meet these criteria were disqualified from the selection process. The soft-embalmed cadavers were removed from refrigeration set at a temperature of 46 degrees Fahrenheit and placed on an adjustable surgical table two hours prior to assessing anterior tibial translation using the KT-1000 arthrometer.
Method of Measurement
The instrumented KT-1000 examination (MEDmetricÒ Corp., San Diego, CA, United States) was performed with the soft-embalmed cadaver in the supine position. Both legs were placed on a thigh support with the knees in 30° of flexion. A footrest and a strap around the thighs kept the legs in a neutral position.10,11 The arms were placed alongside the body in a relaxed and anatomical position. The sensor mechanism known as the superior pad is placed on the patella, while the inferior pad rests on the anterior tibial tuberosity (Figure 1). The superior pad is the only moving part of the KT-1000 which measures the value of the anterior tibial translation for various force vectors.
 |
Figure 1 KT-1000 Arthrometer measurements performed on a soft-embalmed cadaver. |
The instrument was calibrated to zero before each displacement test. The anterior displacement of the tibia in relation to the femur was measured at 67N and 89N bilaterally in each cadaver 3 times. The readings of the needle position were only accepted if the needle returned to 0 ± 0.5 mm when the tension in the handle was released. The three values were then averaged for a single value to represent 67N and 89N for each cadaver. All measurements were performed by a Doctor of Physical Therapy specifically trained in the use of the KT-1000 arthrometer.
The soft-embalmed ATT measurements were then compared to the ATT of twenty-one healthy uninjured individuals consisting of 13 women and 8 men using the identical KT-1000 measurement technique. This cohort consisted of participants aged 18–45 year old, any participant with history of knee trauma, lower limb injury, or self-reported leg disorders were excluded from the study.12
Statistical Analysis
All data sets were analyzed using a welch two-sample t-test to determine the similarity between the means of the data sets. All statistical analysis was performed in the R project for statistical computing (Vienna, Austria; R Core Team). Effects were considered statistically significant at p ≤ 0.05.
Results
Investigating the potential difference in laxity between the right and left knees of the same cadaver constituted the initial variable studied. The comparative analysis between the right and left knees, conducted under 67N and 89N conditions, revealed an average difference of 1.36 mm, a finding deemed statistically insignificant (CI: −1.64 to 1.34). These results demonstrate the absence of any discernible variation between the laxity of the right and left knees.
Two sets of data were collected to assess if age and sex were significant contributors when measuring laxity. The first test included all thirteen cadavers. The generalized linear mixed model (GLMM) regression for both 67N and 89N originally indicated the age and sex of the donor have significant effects on anterior movement. However, the analysis also exposed two outliers within this data. The outliers were the two cadavers who had the most time elapse since their original date of embalming, 1156 days and 1152 days respectively.
A second welch two sample t-test was conducted with the outliers removed. Including eleven cadavers, ranging in days embalmed from 250 to 949 days. Establishing a new longest length in days embalmed to approximately two years and seven months. Astonishingly, the regressions accounting for other contributions to ACL laxity proved to have no significant effects. This suggests the initial results were mainly driven by outliers. Removing two observations made the sample size fifteen percent smaller. Importantly, this outcome suggests other factors are unlikely to significantly contribute to the increased anterior movement of the soft-embalmed cadaver knees over live knees.
The t-tests show a significant difference between live and soft-embalmed cadaver knees. The cadaver knees were proven to show greater laxity. The anterior tibial translation in the set of healthy live knees directly compared to the soft-embalmed cadaver group for 67N (Figure 2) depicts an average difference of 1.76mm (CI: 0.97–2.54). The same comparison at 89N (Figure 3) depicts an average difference of 2.12mm (CI: 1.16–3.09).
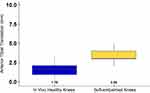 |
Figure 2 Anterior tibial translation of in vivo health knees versus soft-embalmed cadaver knees at 67N. |
 |
Figure 3 Anterior tibial translation of in vivo health knees versus soft-embalmed cadaver knees at 89N. |
Discussion
The soft-embalmed cadaver model is becoming an increasingly popular training tool amongst physicians across many specialties, as well as, post-graduate and medical students. For reasons including the high level of visual and tactile realism, easy maintenance, versatility, and acceptable odor.5,11 In an attempt to determine the breadth applicability of the soft-embalmed cadaver model, it is equivalently important to establish limitations. The study determined a significant difference between soft-embalmed cadaver ACL translation versus our healthy in-vivo control group.
There are several accepted embalming techniques, each consisting of different chemical compounds that are further differentiated into hard and soft fixation. Hard fixation, an embalming approach that primarily relies on the use of aldehydes as the main chemical compound, results in drastically reduced tissue mobility.13 Also, in 2016 formaldehyde was found to be a class 1B carcinogen, which is one of the main appeals to the Thiel and surgical reality fluid techniques due to the main product being ethylene glycol with a drastically decreased formaldehyde content of 0.8%.14
In contrast, soft embalming methods employ compounds such as ethylene glycol that maintain or even improve tissue flexibility. Of the soft-embalming methods, Surgical Reality Fluid scores the highest on McMaster Embalming Scale. A scale developed to evaluate preservation techniques based on five domains: color, visual appearance, texture, physical force required to perform surgical techniques, and suitability for surgical training. When compared to the six other soft-embalming techniques, surgical reality fluid outperformed in all domains. Contributing to the improvement of surgical education with functional task alignment.13
The hypotonic chemical nature of the embalming process and the inability of the cadaver to actively utilize the stabilizing muscles around the knee leads to an increase in anterior tibial translation. The average increase at 67N and 89N was only 1.76mm and 2.12mm respectively. This increase in translation when used for the purpose of medical training is not necessarily a negative consequence. Memory and accurate replication of a skilled movement, within the context of medical techniques, is best learned through visual and kinesthetic feedback loops either separately or combined. Long-term potentiation is shown to be enhanced further when both visual and kinesthetic sensory systems are combined.15 While soft-embalmed cadavers exhibit increased joint laxity, this approach offers a low-risk learning environment for medical professionals, enabling them to establish vital sensorimotor connections in joint manipulation, all without the necessity of involving patients.
Some of the most common knee injuries in sports are that of knee stabilizers, particularly the ACL. This is due to its load-bearing nature which creates susceptibility to both contact and non-contact injury. Improper assessment of an ACL tear can leave a patient with overwhelmingly diminished future activity levels and quality of life.16 This can potentially be alleviated by improving the training model used to teach and assess ACL testing techniques such as Lachman’s, anterior drawers, lever sign test, and pivot shift test. Previous studies have demonstrated that the tissue stability of the medial and lateral knee in total knee arthroplasty is comparable between Thiel cadaver and in vivo knees. When contrasted at 90 degrees of flexion both the medial and lateral compartments showed no significant difference in stiffness.6 Compared to other cadaver models, the hyper-realism, multifunctionality, and laxity of the soft-embalmed cadavers offer an alternative model to traditional teaching methods currently available.
While the joints of soft-embalmed cadavers will continue to display a full range of motion, the durability and properties of the tissue has been shown to change overtime. This is thought to be due to the nature of the embalming process and the gradual loss of fluid. Additionally, there is limited research in cadavers embalmed greater than 3 years due to the Anatomy Act of 1984 and Human Tissue Act of 2004 that requires cremation of cadavers after 3 years of acceptance.17 This was demonstrated by the two outliers in our data above. The soft-embalmed cadavers embalmed greater than three years had significantly increased laxity when compared to those embalmed for less than three years. While our data revealed a noteworthy increase in laxity among cadavers embalmed for over three years, it is essential to acknowledge the limitation of our small sample size (n = 13). As such, drawing a definitive conclusion about a concrete three-year cut-off requires caution. Nevertheless, researchers should prudently consider this possibility when utilizing soft-embalmed cadavers for biomechanical training.
Conclusions
The anterior tibial translation is significantly different between soft-embalmed and in vivo knees with forces of 67N and 89N using the KT-1000. While soft-embalmed cadavers may not directly replicate ATT to an exact number to that of in vivo tissue, they still allow the perception of the tibial translation against a stationary femur. The difference is less than 2.5 mm in both data sets when compared to an in-vivo knee, equivalent to one-tenth of an inch. Suggesting the viability of soft-embalmed cadavers ATT and should not exclude their use in medical education. Future studies should compare the ATT of soft-embalmed cadavers not only to live tissue but the ability to detect and exclude pathology in the knee.
Ethical Approval
This study was submitted to the East Tennessee State University Human research and protections department. It was determined that this proposed activity does not meet the definition of research involving human subjects. Therefore, it does not fall under the purview of the IRB. East Tennessee State University IRB review and approval is not required.
Acknowledgment
The authors thank the ETSU anatomical gift program whose generous gifts made this anatomical research possible. As well as, the body donors for making a noteworthy contribution to medical education.
Funding
This research did not receive any specific funding from any authority or body.
Disclosure
The authors report no conflicts of interest in relation to this work and declare that there is no conflict of interest regarding the publication of this article.
References
1. Thiel W. An arterial substance for subsequent injection during the preservation of the whole corpse. Ann Anat. 1992;174(3):197–200. doi:10.1016/S0940-9602(11)80347-X
2. Thiel W. The preservation of the whole corpse with natural color. Ann Anat. 1992;174(3):185–195. doi:10.1016/S0940-9602(11)80346-8
3. Hunter A, Eisma R, Lamb C. Thiel embalming fluid--a new way to revive formalin-fixed cadaveric specimens. Clin Anat. 2014;27(6):853–855. doi:10.1002/ca.22392
4. Eisma R, Lamb C, Soames RW. From formalin to Thiel embalming: what changes? One anatomy department’s experiences. Clin Anat. 2013;26(5):564–571. doi:10.1002/ca.22222
5. Yiasemidou M, Roberts D, Glassman D, Tomlinson J, Biyani CS, Miskovic D. A multispecialty evaluation of Thiel cadavers for surgical training: reply. World J Surg. 2017;41(12):3230–3231. doi:10.1007/s00268-017-4251-9
6. Vollner F, Pilsl U, Craiovan B, et al. Stability of knee ligament complex of Thiel-embalmed cadaver compared to in vivo knee. J Mech Behav Biomed Mater. 2017;71:392–396. doi:10.1016/j.jmbbm.2017.04.009
7. Siegel L, Vandenakker-Albanese C, Siegel D. Anterior cruciate ligament injuries: anatomy, physiology, biomechanics, and management. Clin J Sport Med. 2012;22(4):349–355. doi:10.1097/JSM.0b013e3182580cd0
8. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med. 2016;44(6):1502–1507. doi:10.1177/0363546516629944
9. Klasan A, Putnis SE, Kandhari V, Oshima T, Fritsch BA, Parker DA. Healthy knee KT1000 measurements of anterior tibial translation have significant variation. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2177–2183. doi:10.1007/s00167-019-05768-w
10. Sernert N, Helmers J, Kartus C, Ejerhed L, Kartus J. Knee-laxity measurements examined by a left hand and a right-hand-dominant physiotherapist, in patients with anterior cruciate ligament injuries and healthy controls. Knee Surg Sports Traumatol Arthrosc. 2007;15(10):1181–1186. doi:10.1007/s00167-007-0347-3
11. Soler-Silva A, Sanchis-Lopez A, Sanchez-Guillen L, et al. The Thiel cadaveric model for pelvic floor surgery: best rated in transferable simulation-based training for postgraduate studies. Eur J Obstet Gynecol Reprod Biol. 2021;256:165–171.
12. Keizer MNJ, Hijmans JM, Gokeler A, et al. Healthy subjects with lax knees use less knee flexion rather than muscle control to limit anterior tibia translation during landing. J Exp Orthop. 2020;7(1):32. doi:10.1186/s40634-020-00246-6
13. Wang A, de SA D, Darie S, et al. Development of the McMaster Embalming Scale (MES) to assess embalming solutions for surgical skills training. Clin Anat. 2023;36(5):754–763. doi:10.1002/ca.24037
14. Kaliappan A, Motwani R, Gupta T, et al. Innovative cadaver preservation techniques: a systematic review. Maedica. 2023;18(1):127–135. doi:10.26574/maedica.2023.18.1.127
15. Pinzon D, Vega R, Sanchez YP, Zheng B. Skill learning from kinesthetic feedback. Am J Surg. 2017;214(4):721–725. doi:10.1016/j.amjsurg.2016.10.018
16. Yu B, Garrett WE. Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007;41 Suppl 1:i47–51. doi:10.1136/bjsm.2007.037192
17. Liao X, Kemp S, Corner G, et al. Elastic properties of Thiel-embalmed human ankle tendon and ligament. Clin Anat. 2015;28(7):917–924. doi:10.1002/ca.22512
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
