Back to Journals » Advances in Medical Education and Practice » Volume 14
Application of Team-Based Flipped Classroom and Traditional Learning on the Antenatal Education Center Course
Authors Lin Y , Xiu X, Lin J, Chen Z , Zheng CX, Pan X, Lin L, Yan J
Received 17 August 2023
Accepted for publication 28 November 2023
Published 12 December 2023 Volume 2023:14 Pages 1379—1390
DOI https://doi.org/10.2147/AMEP.S429806
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Yingying Lin,1,* Xiaoyan Xiu,2,* Juan Lin,3 Zhiwei Chen,3 Cui Xian Zheng,3 Xuehong Pan,2 Lihua Lin,1 Jianying Yan3
1Department of Healthcare, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, People’s Republic of China; 2Department of Health Education, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, People’s Republic of China; 3Department of Obstetrics, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianying Yan, Department of Obstetrics, Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics & Gynecology and Pediatrics, Fujian Medical University, Fuzhou, People’s Republic of China, Tel +86591-86329270, Email [email protected]
Background: The goal is to evaluate the effects of a flipped class strategy on knowledge, self-directed learning ability, learning satisfaction and pregnancy outcomes in primiparas undergoing antenatal education.
Methods: A random sampling method was adopted. A total of 600 primiparas who were diagnosed with early pregnancy in a first-class hospital in southeast China and received continuous prenatal health education from May to July 2020 were selected as the research subjects. In order to make the baseline of the two groups of primipara comparable, we divided the two groups in the antenatal education centre according to the odd-even number of the lesson card number. The odd-numbered group was the experimental group, who used the prenatal health education model based on blended learning; the even-numbered group was the control group, who used the traditional mode of prenatal health education. The two groups were compared on the following outcomes: knowledge, self-directed learning ability, learning satisfaction and pregnancy outcomes.
Results: Compared with traditional learning, the blended learning approach can effectively controlled the gestational weight gain (GWG), alleviated the anxiety and depression during pregnancy, improved the natural delivery rate of the primipara, shortened the delivery process and reduced the risk of gestational diabetes mellitus (GDM), the difference was statistically significant (all P< 0.05).
Conclusion: Blended learning may be an effective strategy because of its validity and practicality in antenatal education.
Keywords: health education, flipped classroom, team-based learning, primipara, pregnancy outcomes, blended learning
Background
Maternal health education in China is based on antenatal education centres supported by health care institutions at all levels. The “Regulations for Pregnancy and Childbirth Health Care” issued by the former Ministry of Health of the People’s Republic of China clearly stipulates that
Maternal and child health institutions at all levels are responsible for guiding and carrying out pregnancy and childbirth health education in their respective jurisdictions, formulating a health education plan and developing suitable health education materials.1
As an important component of perinatal health care work, antenatal education centres play a vital role in publicizing and promoting perinatal health care knowledge.
However, with the advent of social media, the new generation of prospective parents for pregnancy-related social networking and support about pregnancy on the Internet during early gestation. And that it has a significant impact on the prenatal and postpartum decision-making process.2 Therefore, the traditional lecture (TL) model obviously can no longer meet the needs of contemporary pregnant women.
More interactive prenatal education models are being developed and utilized, for example, the application of learner-centred education and active participation of learners in the classroom.3,4 The American Board of Obstetrics and Gynaecology advocates the group prenatal care (GPC) model.5 Based on this model, several pregnant women with similar gestational weeks form a team and acquire antenatal care together and regularly organize activities for discussion and the publicizing of knowledge. On the team, pregnant women can grow up to each other and enhances the quality of prenatal care.6 Such educational backgrounds have stimulated the development of various teaching patterns and learning strategies, such as the flipped classroom (FC) method and team-based learning (TBL).
The FC method covers pre-, in-, and post-class learning methods. The instructor provides various learning materials through an electronic network. Learners acquire foundational knowledge by means of various digital media, at any time and in any location, and apply it in the classroom.7,8 The FC may encourage learners to think independently and imaginatively, but it appears that learners perform only limited pre-learning before class.9 TBL is a teaching strategy of small teams that are transformed into active learning teams by specific procedures.10 It can not only improve learners’ collaboration ability, disciplinary knowledge and application ability11 but also has the potential to increase learners’ satisfaction and achievement.12 Therefore, a blended learning model (ie, a combination of FC and TBL) is the use of TBL within FC by learners. It can promote learners’ active learning, increase the opportunity for active instructor–learner and learner–learner interactions, thereby improving learners’ learning ability, enable them to learn individually and iteratively, facilitate the sharing of learning materials in groups, and help them acquire high knowledge scores.13–15 Several pedagogical theories, such as Piaget’s active learning theory, have proven that a learner’s interest in collaborative interaction for TBL motivates self-directed learning in the FC.8 Active participation in the learning process also helps improve learners’ learning satisfaction.16
At present, studies have just started to investigate the effect of the blended learning approach in antenatal education courses. The objective of this study is to evaluate the effect of the blended learning model in an antenatal education course in regard to learning outcomes and to the maternal and neonatal outcomes of primiparas undergoing antenatal education.
Methods
Design and Participants
In this study, 621 pregnant women receiving antenatal education in the hospital from May to July 2020 were selected as the research subjects. Inclusion criteria: they were willing to participate in this study, able to attend regular antenatal examinations, planned to deliver in the target hospital, signed the informed consent form and had a smartphone. Exclusion criteria were refusal to participate in the study, language barriers, history of major disease or mental illness, employment as medical staff, high-risk pregnancy factors, or a psychological assessment of severe anxiety or depression. We assessed the respondents’ psychiatric symptoms using the Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS). At the end of the study, 11 patients in the control group were lost to follow-up, for a loss rate of 3.54%. The data showed that 6 were withdrawals, 3 were miscarriages and 2 prematurely delivered. In the experimental group, 10 patients were lost to follow-up, with a loss rate of 3.33%. The reasons for the loss to follow-up were 6 cases of withdrawal, 2 cases of miscarriage and 2 cases of premature delivery. By Fisher’s exact test, the results showed that there was no difference in the distribution of the causes of loss of follow-up in both groups (P>0.05). Ultimately, 300 patients in each group completed this study, and the data were complete and effective.
Instruments
The general information questionnaire was designed by the researchers for the study and included the age, height, weight, educational background, and per capita monthly income of each family.
To test the knowledge of participants, we developed a 35-item multiple-choice questionnaire addressing nutrition during pregnancy, body quality control, exercise during pregnancy, delivery mode, breastfeeding, neonatal health care, infant health care and other related information. The questionnaire’s total scores ranged from 0 to 35. The Cronbach’s α value of the scale was 0.90.
The self-directed learning ability scale17 developed by the Teaching and Learning Center of Fujian Medical University was used, which comprises 28 items to be answered on a 5-point Likert scale (ranging from 1 = strongly disagree to 5 = strongly agree). The scale includes three dimensions (information ability, learning cooperation ability and self-management ability), and the total score was 28–140. The average value was calculated, and a higher score means better self-directed learning ability. The Cronbach’s α value of the scale was 0.96.
A standardized scale of the hospital’s Teaching and Learning Center was used to measure learning satisfaction. Furthermore, the scale was regularly reviewed by a special academic advisory committee of the hospital. This scale comprises 13 items to be answered on a 5-point Likert scale (ranging from 1 = strongly disagree to 5 = strongly agree). The average value was calculated, and the higher the values were, the better the learning satisfaction. In this study, the Cronbach’s α value of the scale was 0.93.
Childbirth self-efficacy was measured using the short form of the Chinese Childbirth Self-Efficacy Inventory (CBSEI-C32), which was translated and developed by Wan-Yim IP in 2008. The scale has 32 items, including two subscales of outcome expectation (OE-16) and self-efficacy expectation (EE-16), each with 16 items, and uses a Likert scale of 10, where 1 is not helpful/not sure at all and 10 is very helpful/very sure. This scale was used to evaluate childbirth self-efficacy, with a total score of 32–320. The higher the score, the better childbirth self-efficacy. This scale has good reliability and validity, with a Cronbach’s α coefficient of 0.96.18
The self-efficacy of breastfeeding was measured using the Breastfeeding Self-efficacy Scale (BSES), which was introduced into China in 2002 by Xiaona Dai19 and forms two dimensions of feeding skills (15 items) and personal inner feelings (15 items), for a total of 30 items. The scale was used to evaluate the level of self-efficacy of breastfeeding. A Likert scale of 5 was adopted, with the numbers 1–5 representing “not confident at all” to “always confident”, and the total score was 30–150. The higher the score was, the better the self-efficacy of breastfeeding. Overall, the scale has good structural validity, with a Cronbach’s α coefficient of 0.93.
The SAS developed by Professor Zung in 1965 was used to assess anxiety status according to the actual feeling of the respondents during the recent week. The scale contains 20 items. It adopts a Likert scale of 4: there are 15 SAS sentences with negative words, scoring in order from 1 to 4, the remaining five positive word statements are reverse scored from 4 to 1. The total score is equal to the sum of the scores of each item multiplied by 1.25, and the integer is the standard score. Anxiety status was determined by a SAS standard score above 50, which indicates anxiety.20
The SDS developed by Professor Zung in 1971 was adopted for depression status. The scale contains 20 items, with a total score of 20–80. The actual feelings of the respondents were used to evaluate their depression status in the last week. A Likert scale of 4 was used to calculate the total score according to the options. A score of 1–4 means rarely, sometimes, most of the time, and most or all of the time. The score ≤53 is classified as normal mood. Depression status was determined by an SDS standard score greater than 53, which indicates depression, and the higher the score, the worse the depression.21
Data Collection and Procedures
This study was approved by the Ethics Committee of Fujian Maternity and Children’s Health Hospital, Affiliated Hospital of Fujian Medical University. All individuals participating in this study provided written informed consent. According to the protocol approved by the Research Ethics Committee, participation (or lack of participation) would not influence their clinical care. The research team earnestly protected the rights and interests of the research subjects, such as privacy, respect and knowledge, strictly kept all data confidential, and carried out anonymous numbering for the included samples. The researchers used neutral language and a non-judgmental attitude throughout the study.
Blended Learning Design
Figure 1 depicts the process of FC combined with TBL education reform. The process included reviewing previous research and on the blended learning design, the application of blended learning and effect evaluation. The teaching process was divided into three stages: pre-class preparation, in-class learning and post-class reflection. The information was delivered once every two weeks in a one-hour class for a total of 12 classes.
 |
Figure 1 Blended learning design including the FC with TBL approach used in this study. |
One week before class, the instructor provided the learners with the relevant learning materials using the WeChat platform. The learners’ WeChat group was set up by dividing the learners into 10 groups and selecting a leader for each group. Learners in small groups previewed the learning materials before class and conducted independent learning to familiarize themselves with the relevant teachings and consider the key points and difficulties of the lesson. Before class, the instructor organized a discussion within the group to exchange knowledge or ask questions to improve the quality of the preview. After the discussion, the group leader summarized the questions and key difficult points in the class. During the class stage, the instructor first evaluated the preview effect, then gave a 20-minute lecture, and finally played a demonstration video. Taking groups as units, learners carried out the practical operation of exercises under the guidance of group instructors. Two learners from each group were randomly selected to demonstrate the operation and one of them gave a presentation. The other learners observed and commented, and finally, the instructor summarized the key points and difficulties of the lesson. During the after-class reflection stage, the learners took test questions, and according to the test results and their performance in class, the instructor formulated personalized learning modes and team activity suggestions. The instructor adjusted and reflected upon the teaching content, improved the teaching method, optimized the teaching design, enhanced the teaching effect and enhanced the interest of the learners.
Traditional Lecture
The control group adopted traditional prenatal health education, which comprises fixed courses compiled according to knowledge of prenatal health education and organized according to the first trimesters (T1), second trimesters (T2) and third trimesters (T3). It is run in an antenatal education centre using a lecture based approach to prenatal health education. The information was again delivered once every two weeks in a one-hour class for a total of 12 classes.
Before starting the education intervention, participants in both groups completed questionnaires assessing their antenatal education-related knowledge, self-directed learning abilities, and learning satisfaction regarding the course that they had previously attended at 11 weeks of pregnancy in the antenatal education centre. Participants in both groups completed the same questionnaires during pregnancy.
Statistical Analysis
SPSS 25.0 statistical software was used for data analysis, and P<0.05 was considered statistically significant. The measurement data are described by the mean±SD, and the counting data are expressed by the frequency and composition ratio. A chi-square test and independent sample t-test were used for comparisons between the two groups. The differences between the two groups in self-directed learning ability, knowledge, learning satisfaction, gestational weight gain (GWG), SAS score and SDS score in accordance with the intervention were analysed by one-way repeated measure ANOVA.
Results
General Characteristics of Participants Between the Two Groups
A total of 600 primiparas were included. Table 1 shows the general characteristics. The average ages of the experimental group and control group were 28.83 and 28.66, respectively. There was no difference in age, weight, height, educational background or family per capita monthly income between the two groups (P>0.05). They are comparable.
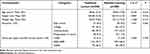 |
Table 1 Baseline Characteristics of Participants Between the Two Groups |
Differences in Learning Outcomes and Psychological Tests Between the Two Groups
There was no difference in statistics between the two groups for psychological tests or the T1 learning outcome variables. The experimental group significantly improved all learning outcome scores and saw an alleviated degree of anxiety and depression in patients. By repeated ANOVA, the self-directed learning ability score showed statistically significant differences in the interactions between the groups (F=552.54, P<0.001), between the gestational week groups (F=6416.57, P<0.001), and between the groups and the gestational week groups (F=769.17, P<0.001). The knowledge score showed statistically significant differences in the interactions between the groups (F=122.96, P<0.001), between the gestational week groups (F=1873.40, P<0.001), and between the groups and the gestational week groups (F=275.71, P<0.001). The learning satisfaction score showed statistically significant differences in the interactions between the groups (F=24.55, P<0.001), between the gestational week groups (F=864.30, P<0.001), and between the groups and the gestational week groups (F=206.66, P<0.001). The SAS score showed statistically significant differences in the interactions between the groups (F =233.42, P<0.001), between the gestational week groups (F=2281.41, P<0.001), and between the groups and the gestational week groups (F=155.79, P<0.001). The SDS score showed statistically significant differences in the interactions between the groups (F=26.32, P<0.001), between the gestational week groups (F=100.25, P<0.001), and between the groups and the gestational week groups (F=23.90, P< 0.001) (Table 2).
 |
Table 2 Differences in Learning Outcome and Psychological Tests in Both Groups |
Differences in GWG and Childbirth Between the Two Groups
GWG, delivery mode and newborn birth weight were significantly different between the two groups. The proportions of underweight gain during pregnancy and overweight gain during pregnancy in the experimental group were 18.00% and 22.00%, respectively, which were lower than the 24.00% and 30.67% in the control group (χ2=12.98, P=0.002). Using repeated ANOVA, the interaction effect of GWG in both groups was not statistically significant (P>0.05). GWGs are different during different periods. Additionally, the GWG between the two groups was different, and the differences were statistically significant (Ftime=3026.145, Ptime<0.001; Fgroups=9.463, Pgroups=0.002). A multivariate ANOVA was used, and the results showed that there was no significant difference in the T1 of GWG in either group (P>0.05), but the T2, T3 and total GWG in the study group were all lower than those of the control group (F values were 4.43, 14.08 and 9.46, P values were all<0.05). Compared to the control group, the incidence of natural childbirth increased, while the incidence of caesarean section decreased. There were obvious differences in both groups (χ2=6.51, P=0.039). The incidence of low birth weight and macrosomia in the experimental group was 3.30% and 1.70%, respectively, which were significantly lower than the 6.70% and 4.70% in the control group (χ2= 8.25, P<0.05). However, the gestational age was not significantly different between the two groups (P>0.05) (Table 3 and Table 4).
 |
Table 3 Comparison of GWG and Childbirth Between the Two Groups |
 |
Table 4 Comparison of GWG Between the Two Groups in Different Periods |
Differences in Delivery Time in Both Groups
The delivery times of the first, second, and the total stage of labour in the experimental group were significantly less than those of the control group (P values were all < 0.001), but there was no significant difference in the delivery time of the third stage of labour between the two groups (P>0.05) (Table 5).
 |
Table 5 Comparison of Labour Duration Between Two Groups of Vaginal Delivery (h) |
Differences in the Self-Efficacy of Both Groups
The test scores for the CSE and BSE of primiparas in the experimental group were 269.66 and 136.17, respectively, which were higher than the 203.10 and 102.03 in the control group, and the difference were statistically significant (tCSE=80.88, P<0.001; tBSE=70.62, P<0.001) (Table 6).
 |
Table 6 Comparison of the Test Scores of CSE and BSE Between the Two Groups |
Differences in Complications During Childbirth Between the Two Groups
The rate of GDM was 16.3% in the study group, which was significantly lower than the control group’s 23.0%, and there was a significant difference (χ2=4.220, P=0.040). Other factors, such as PH, HDCP and intrauterine distress, were not significantly different between the groups (P >0.05) (Table 7).
 |
Table 7 Comparison of Complications During Childbirth Between the Two Groups |
Discussion
With the decline in traditional methods of information sharing, structured antenatal classes have been developed worldwide, driven by the expectations of those who are preparing for childbirth and parenthood.22,23 The dissemination of antenatal information is constantly changing to meet the needs and expectations of parents. At present, studies have just started to investigate the effect of the blended learning approach in antenatal education courses. This study aims to evaluate the effect of the blended learning model in an antenatal education course in regard to learning outcomes and to the maternal and neonatal outcomes of primiparas undergoing antenatal education. Our study suggests that blended learning can enhance outcomes in antenatal education and improve autonomous learning ability, knowledge level, learning satisfaction and even the conditions of the mother and the baby. The effect of blended learning model in antenatal education is remarkable.
Our results show that blended learning can significantly improve the actual effect of antenatal education for primiparas, including improving their knowledge level, learning satisfaction and self-learning ability, compared with traditional antenatal education. Which is similar with the previous studies.24,25 According to the results, the knowledge score of the experimental group was significantly higher than that of the control group, which indicated that the flipped classroom has advantages over the traditional classroom in deepening the primiparas’ comprehensive understanding and analysis of knowledge. There are some reasons in following: firstly, traditional antenatal education is teacher-centred. So primiparas are more passive in learning knowledge, ignoring the process of active exploration and constructive learning. However, the flipped classroom treats primiparas as the centre, and its unique three-process model is more helpful for expanding primiparas’ knowledge of pregnancy than the TL model. Secondly, flipped classrooms can significantly improve pregnant women’s satisfaction. Learner-centred discussions and learner facilitating behaviours expressed through learning activities help participants feel valued in a learning environment.26,27 Interactive discussion is carried out in a flipped classroom. On the one hand, the instructors sort out the knowledge and show their thought process by answering questions in a guiding manner; on the other hand, the primiparas actively participate and think throughout the process. Moreover, flipped classrooms can meet the learning needs of pregnant women in a timely manner. Team education makes enjoyable learning possible. Through group interactive learning, primiparas gain in-depth knowledge and experience exchanges. Petersson et al found that participants had a positive understanding of knowledge exchange and experience sharing within a group.28 Another study shows that women think informal support from their peers and professional support are important.29 Peer support is considered to be an important and enjoyable component of antenatal education. Because of this, the flipped teaching mode obtains higher satisfaction. Finally, in the blended learning model, learners are not limited by time or space before class, easily obtain various learning materials related to topics through smart devices, and realize self-learning. In the process of developing planning, learning and consulting materials, primiparas improved their self-management and self-control ability, and their self-learning awareness and thinking ability were improved.
Interestingly, the results demonstrated that the natural delivery rate of the flipped teaching group was higher than that of the control group, while the caesarean section rate was lower than that of the control group. This finding is consistent with the relevant research results.30 Moreover, the delivery self-efficacy score of the experimental group was higher than that of the control group, indicating that antenatal education based on flipped classrooms is related to the natural childbirth rate and childbirth self-efficacy. CSE plays an important role in the success of natural childbirth, as it strengthens a woman’s confidence in her ability to cope with childbirth. Higher levels of CSE are associated with lower levels of anxiety, pain, and obstetric intervention. Through innovative teaching methods, flipped classrooms strengthen primiparas’ absorption and mastery of delivery knowledge and skills so that they can better understand the benefits of natural childbirth and the indications and sequelae of caesarean section. Antenatal education in a small team may increase women’s trust in their ability to cope with early childbirth, thus reducing the possibility of early admission and the experience of anxiety and childbirth pain.31–34 In addition, we found that antenatal education based on flipped classrooms is related to the labour process of primiparas. The time stage of labour in the experimental group were lower than those in the control group. The flipped classroom model presents important free position, labour pain reduction methods, delivery auxiliary facilities and free position in the form of courseware and video, which can help primiparas master delivery skills effectively and eliminate stress. At the same time, the guidance of midwives is helpful for enhancing the self-confidence of primiparas and ensuring a smooth delivery process. BSE is a mother’s expectation of her ability to breastfeed, and thus it is the determinant of her breastfeeding behaviour. Antenatal education for primiparas was based on the flipped classroom concept, and it sets a breastfeeding task list and regularly publicizes breastfeeding teaching resources. Primiparas can use available chunks of time to obtain breastfeeding knowledge, which is conducive to strengthening the internalization of breastfeeding knowledge. The TBL provides knowledge, emotion and skill support, such that primiparas shift from the passive acceptance of antenatal education knowledge to active participation in obtaining such knowledge. This is helpful in mastering the knowledge of breastfeeding and effectively improving the BSE of primiparas. Our study confirmed the above conclusion.
Furthermore, our results the antenatal education for primiparas based on flipped classrooms is associated with weight gain during pregnancy, birth weight of newborns and GDM. The GWG in the experimental group was lower than that in the control group regardless of the T2, T3 or pregnancy period. With reference to the guidelines for GWG revised by the Institute of Medicine (IOM),35 the proportions of overweight and underweight women in the experimental group were lower than those in the control group. The incidence of normal birth weight in the experimental group was higher than that in the control group, while the incidence of macrosomia and low birth weight was significantly lower than that in the control group. A number of studies have pointed out that nutrition and health education for pregnant women can improve their nutritional awareness and change their unhealthy nutritional behaviours.36 Nutritional intake and physical activity during pregnancy are the main factors affecting the occurrence of macrosomia. The blended learning model lists tasks related to individualized pregnancy nutrition, pregnancy activity and BMI management; it also offers individualized guidance to help primiparas establish a reasonable intake of energy and appropriate aerobic activities for primiparas during pregnancy to maintain their weight in a reasonable range. The results in Table 7 show that blended learning may be associated with the occurrence of GDM. Nutritional imbalance at various stages of pregnancy may significantly increase the risk of pregnancy complications such as anaemia, hypertension syndrome, and GDM. A number of studies have found that GWG is closely related to GDM.37 Excessive GWG will increase the mother’s metabolic burden and lead to glucose and lipid metabolism disorders. The blended learning model actively guides pregnant women with reasonable nutrition, scientifically adjusts their diet and exercise, strengthens communication, solves nutritional problems in a timely manner, maintains blood sugar stability, and reasonably controls pregnant women’s weight and GWG within an appropriate range, thereby reducing the risk of gestational diabetes.
This study has some limitations. First, the study is limited to one region, with a small sample size and a lack of representativeness. Second, the current research only focuses on primiparas, but in reality, the proportion of multiparas can be as high as 44.4%. Third, the current research period was less than one year, which limits understanding of long-term effects and other objective indicators, such as exclusive breastfeeding rate, child rearing and long-term health of mother and child. Future research should expand the research field and increase the sample size, carry out multi-center research, and promote it to the grassroots. At the same time, not just focusing on primiparas, the research will be extended to all pregnant women to expect better pregnancy outcomes.
Conclusions
In short, the blended FC with TBL learning model enhanced primiparas’ knowledge, self-directed learning ability, learning satisfaction, and effective GWG control and reduced depression in pregnant women during pregnancy, which improved the self-efficacy and natural delivery rate of the primipara, shortened the delivery process, and reduced the risk of GDM. In addition, this educational strategy was found to be effective both outside and inside the classroom in obtaining positive learning outcomes. The blended learning model presented in this research is remarkably effective and worth promoting.
Abbreviations
FC, Flipped classroom; TBL, Team-based learning; TL, Traditional lecture; SAS: Self-Rating Anxiety Scale; SDS, Self-Rating Depression Scale; CBSEI-C32, The short form of the Chinese Childbirth Self-Efficacy Inventory; BSES, Breastfeeding self-efficacy Scale; CSE, Childbirth self-efficacy; BSE, Breastfeeding self-efficacy; GWG, gestational weight gain; T1, First trimester; T2, Second trimester; T3, Third trimester; HDCP, hypertensive disorder complicating pregnancy; PH, Postpartum hemorrhage; GDM, gestational diabetes mellitus.
Data Sharing Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The Hospital Ethics Committee of Fujian Provincial Maternity and Children’s Hospital, an affiliated hospital of Fujian Medical University, approved the study (2022KYLLR03050) and complied with the Declaration of Helsinki. All individuals participating in this study provided written informed consent.
Acknowledgments
We would like to thank all the women who kindly agreed to participate in this study. We are also grateful to all the staff at the hospitals and health facilities of the Fujian Maternity and Child Health Hospital and their support with this research.
This article has been released preprint in the research square (https://assets.researchsquare.com/files/rs-640411/v1_covered.pdf?c=1631871876). Preprints are the authors’ early version of their research, it is not considered plagiarism or self-plagiarism. Each preprint also has a disclaimer stating that the paper has not been published. Beyond that, I declare that this article has not been published elsewhere.
Funding
Joint Funds for the innovation of science and Technology, Fujian province (Grant number: 2020Y9165).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Department of Maternal and Child Health and Community Health, Ministry of Health, PRC. “Regulations for Pregnancy and Childbirth Health Care” ([2011] No. 56). Available from: http://www.nhc.gov.cn/zwgkzt/wsbysj/201107/52320.shtml.
2. Moretti FA, Oliveira VE, Silva EM. Access to health information on the Internet: a public health issue? Revista Assoc Med Brasileira. 2012;58(6):650–658.
3. O’Flaherty J, Phillips C. The use of flipped classrooms in higher education: a scoping review. Internet High Educ. 2015;5:85–95. doi:10.1016/j.iheduc.2015.02.002
4. Mehta NB, Hull AL, Young JB, Stoller JK. Just imagine: new paradigms for medical education. Acad Med. 2013;88(10):1418–1423. doi:10.1097/ACM.0b013e3182a36a07
5. McCue BK, Borders AE. ACOG committee opinion No. 731: group prenatal care. Obstet Gynecol. 2018;131(3):e104–e108. doi:10.1097/AOG.0000000000002529
6. De Cesare JZ, Jackson JR. Centering pregnancy: practical tips for your practice. Arch Gynecol Obstet. 2015;291(3):499–507. doi:10.1007/s00404-014-3467-2
7. Bergmann J, Sams A. Flipped Learning: Gateway to Student Engagement.
8. Erbil DG. A review of flipped classroom and cooperative learning method within the context of Vygotsky theory. Front Psychol. 2020;11:1157. doi:10.3389/fpsyg.2020.01157
9. Mortensen CJ, Nicholson AM. The flipped classroom stimulates greater learning and is a modern 21st century approach to teaching today’s undergraduates. J Anim Sci. 2015;93(7):3722–3731. doi:10.2527/jas.2015-9087
10. James S, Cogan P, McCollum M. Team-based learning for immunology courses in allied health programs. Front Immunol. 2019;10:2477. doi:10.3389/fimmu.2019.02477
11. Hamada S, Haruta J, Maeno T, et al. Effectiveness of an interprofessional education program using team-based learning for medical students: a randomized controlled trial. J Gen Fam Med. 2019;21(1):2–9. doi:10.1002/jgf2.284
12. Dearnley C, Rhodes C, Roberts P, Williams P, Prenton S. Team based learning in nursing and midwifery higher education: a systematic review of the evidence for change. Nurse Educ Today. 2018;60:75–83. doi:10.1016/j.nedt.2017.09.012
13. Han E, Klein KC. Pre-class learning methods for flipped classrooms. Am J Pharm Educ. 2019;83(1):6922. doi:10.5688/ajpe6922
14. Persky AM, Hogg A. Influence of reading material characteristics on study time for pre-class quizzes in a flipped classroom. Am J Pharm Educ. 2017;81(6):103. doi:10.5688/ajpe816103
15. Francis N, Morgan A, Holm S, Davey R, Bodger O, Dudley E. Adopting a flipped classroom approach for teaching molar calculations to biochemistry and genetics students. Biochem Mol Biol Educ. 2019;48(3):220–226. doi:10.1002/bmb.21328
16. Davies RS, Dean DL, Ball N. Flipping the classroom and instructional technology integration in a college-level information systems spreadsheet course. Educ Technol Res Dev. 2013;61(4):563–580. doi:10.1007/s11423-013-9305-6
17. Lin Y, Jiang AL. Developing a measure scale of autonomous learning competencies of nursing undergraduates. Nurs J Chin PLA. 2004;21(6):1–4.
18. W-yiprr RTN, Chung TK, Tang CS. The Chinese Childbirth Self‐Efficacy Inventory: the development of a short form. J Clin Nurs. 2008;17(3):333–340. doi:10.1111/j.1365-2702.2006.01919.x
19. Dai X, Chen X, Ling XU. The application of breastfeeding confidence scale in nursing practice. Chin J Nurs. 2004;39(6):407–409.
20. Zung WW. A rating instrument for anxiety disorders. Psychosom. 1971;12(6):371–379. doi:10.1016/S0033-3182(71)71479-0
21. Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12(1):63–70. doi:10.1001/archpsyc.1965.01720310065008
22. Gagnon AJ, Sandall J, Individual or group antenatal education for childbirth or parenthood, or both. Cochrane Database Syst Rev. 2007;(3):CD002869. doi:10.1002/14651858.CD002869.pub2
23. Ahldén I, Ahlehagen S, Dahlgren LO, Josefsson A. Parents’ expectations about participating in antenatal parenthood education classes. J Perinat Educ. 2012;21(1):11–17. doi:10.1891/1058-1243.21.1.11
24. Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017;51(6):585–597. doi:10.1111/medu.13272
25. Haley CM, Brown B, Koerber A, Nicholas CL, Belcher A. Comparing case-based with team-based learning: dental students’ satisfaction, level of learning, and resources needed. J Dent Educ. 2020;84(4):486–494. doi:10.21815/JDE.019.190
26. Canoso JJ, Saavedra MÁ, Pascual-Ramos V, Sánchez-Valencia MA, Kalish RA. Musculoskeletal anatomy by self-examination: a learner-centered method for students and practitioners of musculoskeletal medicine. Ann Anat. 2020;228:151457. doi:10.1016/j.aanat.2019.151457
27. Matsuyama Y, Nakaya M, Okazaki H, Lebowitz AJ, Leppink J, van der Vleuten C. Does changing from a teacher-centered to a learner-centered context promote self-regulated learning: a qualitative study in a Japanese undergraduate setting. BMC Med Educ. 2019;19(1):152. doi:10.1186/s12909-019-1550-x
28. Petersson K, Petersson C, Hakansson A. What is good parental education? Nordic Coll Caring Sci. 2004;18:82–89.
29. Pålsson P, Kvist LJ, Ekelin M, Hallström IK, Persson EK. “I didn’t know what to ask about”: first-time mothers’ conceptions of prenatal preparation for the early parenthood period. Perinatal Educ. 2018;27:
30. Xin-li ZHU, Chun-yi GU, Hua TAO, et al. Survey on normal primiparae’s expected mode of delivery and its influencing factors under two-child policy. Chin J Nurs. 2016;51:1044–1048.
31. Maimburg RD, Vaeth M, Durr J, et al. Randomised trial of structured antenatal training sessions to improve the birth process. BJOG. 2010;117(8):921–928. doi:10.1111/j.1471-0528.2010.02584.x
32. Taheri Z, Mazaheri MA, Khorsandi M, et al. Effect of educational intervention on self-efficacy for choosing delivery method among pregnant women in 2013. Int J Prev Med. 2014;5(10):1247–1254.
33. Ip WY, Tang CS, Goggins WB. An educational intervention to improve women’s ability to cope with childbirth. J Clin Nurs. 2009;18(15):2125–2135. doi:10.1111/j.1365-2702.2008.02720.x
34. Piro SS, Ahmed HM. Impacts of antenatal nursing interventions on mothers’breastfeeding self-efficacy: an experimental study. BMC Pregnancy Childbirth. 2020;20(1):19. doi:10.1186/s12884-019-2701-0
35. Institute of Medicine (US) and National Research Council. (US) Committee to reexamine IOM pregnancy weight guidelines. In: Rasmussen KM, Yaktine AL, editors. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academies Press (US); 2009.
36. Tzoulaki I, Sovio U, Pillas D, et al. Relation of immediate postnatal growth with obesity and related metabolic risk factors in adulthood: the northern Finland birth cohort 1966 study. Am J Epidemiol. 2010;171(9):989–998. doi:10.1093/aje/kwq027
37. Yong HY, Mohd Shariff Z, Mohd Yusof BN. Higher parity, pre-pregnancy BMI and rate of gestational weight gain are associated with gestational diabetes mellitus in food insecure women. Int J Environ Res Public Health. 2021;18(5):2694. doi:10.3390/ijerph18052694
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
