Back to Journals » Vascular Health and Risk Management » Volume 19
Appropriate Use of Primary Statin Preventive Therapy Among Patients with High Atherosclerosis-Related Cardiovascular Disease Risks: Cross-Sectional Study, Northeast Ethiopia
Authors Melaku EE , Ayele ET , Urgie BM , Ayidagnuhim GB , Hassen EM , Tefera AS
Received 11 August 2023
Accepted for publication 31 October 2023
Published 7 November 2023 Volume 2023:19 Pages 707—718
DOI https://doi.org/10.2147/VHRM.S435036
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Ermiyas Endewunet Melaku,1 Esubalew Tesfahun Ayele,2 Besufekad Mulugeta Urgie,1 Getachew Bizuneh Ayidagnuhim,1 Erzik Mohammed Hassen,1 Aklile Semu Tefera2
1Department of Internal Medicine, school of Medicine, Debre Berhan University, Debre Berhan, Ethiopia; 2Department of Epidemiology, School of Public Health, Debre Berhan University, Debre Berhan, Ethiopia
Correspondence: Ermiyas Endewunet Melaku, Debre Berhan University, Debre Berhan, Ethiopia, Tel +251912980319, Email [email protected]
Background: Atherosclerosis-related cardiovascular diseases (coronary heart diseases, ischemic stroke, and peripheral vascular diseases) account for the majority of deaths in diabetic and other high-risk patients. Statin therapy reduces major vascular events, coronary death or nonfatal myocardial infarction, coronary revascularization, and ischemic stroke. However, a gap exists between guideline recommendations and the clinical practice of primary statin preventive therapy. This was a cross-sectional study that aimed to determine the prevalence and some associated risk factors of.
Purpose: This study was intended to assess the magnitude of primary statin preventive therapy and associated factors among patients with high atherosclerosis-related cardiovascular disease risks.
Patients and Methods: An institutional-based cross-sectional study design was conducted by a consecutive sampling technique from February 1, 2023, to May 30, 2023. Face-to-face interviews using a structured questionnaire, document review, and laboratory measurements were implemented to collect data. Data entered into Epi Data were analysed by STATA version 14 and summarized by using frequency tables and graphs. Binary and multivariate logistic regression analyses were performed and checked for association at a p value of < 0.05.
Results: A total of 389 patients were included in this study. Diabetes mellitus (43.75%), hypertension (47.3%), and chronic kidney disease (9.25%) were commonly identified diseases. One hundred sixty-seven (42.93%, CI: 38.07– 47.92) patients with high atherosclerosis-related cardiovascular disease (ASCVD) risks were on primary statin preventive therapy. Duration of diabetes mellitus (AOR=1.33, CI: 1.1569– 1.528), treating physician (AOR=3.875, CI: 1.368– 10.969), follow-up regularity (AOR=3.113, CI: 1.029– 9.417) and ten-year atherosclerosis-related cardiovascular disease risk score (AOR=1.126, CI: 1.021– 1.243) were found to be significantly associated with the use of primary statin preventive therapy.
Conclusion and Recommendations: The magnitude of patients who were on primary statin preventive therapy was relatively low (42.93%). Improving the regular follow-up and making senior physicians (internists) attend patients at medical follow-up clinics would likely improve the number of patients who are on primary statin preventive therapy.
Keywords: atherosclerosis, cardiovascular disease, primary statin preventive therapy
Introduction
Atherosclerosis-related cardiovascular disease (ASCVD) is a plaque buildup in arterial walls that results in arterial wall narrowing manifested by ischemic heart disease, ischemic stroke, peripheral arterial disease, aneurysm, or dissection. It remains the leading cause of morbidity and mortality in both developed and developing nations, and its incidence continues to rise with a consequent increase in the rates of coronary and cerebrovascular events.1–3
The use of statins in ASCVD risk reduction for primary and secondary prevention has been well established in landmark trials.4 Statins reduce the risk of all-cause mortality, cardiovascular mortality, stroke, and myocardial infarction for patients who are at high risk of ASCVD.5 The 2019 American College of Cardiology/American Heart Association (ACC/AHA) guideline recommends the use of primary statin preventive therapy for individuals with a high risk of ASCVD.6
Despite their well-established benefits and corresponding recommendations from expert bodies and guidelines, several studies have shown suboptimal use of primary statin preventive therapy in “real world” clinical practice. The large gap in statin treatment has serious health and economic consequences for patients and the health care system in general.5,7–9
Predictors for the use of primary statin preventive therapy include but are not limited to the age of participants, male sex, urban residence, better income, hypertension, duration of diabetes mellitus, baseline cholesterol level, blood glucose control, chronic kidney disease, ten-year ASCVD risk score, follow-up regularity, specialty of the physician, and other comorbidities.9–20
Even if some studies were conducted on diabetic patients in Ethiopia, the overall magnitude of primary statin preventive therapy involving all at-risk patients has not been studied thus far. Therefore, this study aimed to assess the magnitude of patients who are on primary statin preventive therapy and associated factors in the North Shoa zone, Debre Berhan Comprehensive Specialized Hospital, medical follow-up clinic. The findings might serve as an initial triggering factor for large-scale studies so that emphasis might be given to this vital and cost-effective but neglected therapy.
Materials and Methods
Study Settings
A cross-sectional study was conducted between February 1, 2023, and May 30, 2023, at the medical follow-up clinic of Debre Berhan Comprehensive Specialized Hospital. The hospital is located in Northeast Ethiopia, which is 130 km away from the capital city, Addis Ababa. The hospital has a catchment population of 3.5 million.
Study Subjects and Variables
Study Subjects
Patients with high atherosclerosis-related cardiovascular disease (ASCVD) risk who had follow-up at the medical follow-up clinic, Debre Berhan Comprehensive Specialized Hospital, during the study period were considered the study population. History of hypertension, diabetes mellitus, smoking, and anti-hypertensive medication was taken. Blood pressure and other physical examinations were done and documented. Laboratory measurements including fasting blood sugar and lipid profile were determined for all patients for whom screening is recommended. Then, high-risk patients for ASCVD were selected based on the 2019 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for whom the use of primary statin preventive therapy is recommended. Accordingly, individuals aged 20–75 years and low-density lipoprotein cholesterol (LDL-C) ≥ 190 mg/dl, 40–75 years of age with diabetes mellitus (DM) and LDL-C 70–189 mg/dl and 40–75 years of age with LDL 70–189 mg/dl and a 10-year ASCVD risk of 7.5% or higher were included in this study. Patients who had established ASCVD were excluded from the study.
Study Variables
Dependent variable: Appropriate use of primary statin preventive therapy in patients with high ASCVD risks.
Independent Variables:
- Sociodemographic characteristics: age, sex, marital status, educational status, and place of residence.
- Socioeconomic and behavioral factors: health insurance, income, smoking, and patient refusal to take statins.
- Disease-related factors: hypertension, diabetes mellitus, cholesterol level, fasting blood glucose level, duration of diabetes mellitus, type of diabetes mellitus, chronic kidney disease, diabetes-associated complications, other comorbidities, history of hospitalization, frequency of follow-up, presence of contraindications, medication side effects and use of other drugs, side effects of statins, contraindication to statins, and patients affording to buy statins.
- Physician-related factors: Specialty of the prescriber and physician reluctance (failure to prescribe).
Sample Size and Sampling Procedures
The sample size was calculated using a formula for the estimation of single population proportion with the assumption of 95% confidence interval, 5% margin of error and prevalence of 55%. Consecutive sampling method was used to recruit 389 study participants.21
Data Collection Instruments and Procedure
Data were collected through trained data collectors using a predesigned questionnaire. Patients were interviewed to obtain sociodemographic and socioeconomic data. Relevant medical history and laboratory parameters were obtained from patient records. Laboratory investigations of fasting blood sugar lipid profiles and creatinine were determined. High-risk patients for ASCVD were identified based on the LDL level, ten-year ASCVD score and diabetes mellitus status of patients.
Data Analysis
Data were coded, recoded, cleaned, and explored to identify missing values and inconsistencies. Data were entered into EpiData V.3.1 and analysed by STATA 14.0. In the descriptive analysis, the mean with SD frequency and percentages were calculated. Basic assumptions of logistic regression were checked. Both bivariate and multivariate logistic regression analyses were used to identify factors independently associated with the appropriate use of primary statin preventive therapy in patients with high ASCVD risks. Those variables with p values of less than 0.2 in bivariate analysis were exported to multivariate analysis to control the possible effect of confounders. Adjusted odds ratio (AOR) with 95% confidence interval (CI) and p value <0.05 were used to select independently associated factors with appropriate use of primary statin preventive therapy in patients with high ASCVD risks.
Definition of Terms
- Appropriate use of statin: patients are considered as appropriately treated with primary statin preventive therapy when they are started appropriate dose of statin in the presence of indications according to the 2019 American College of Cardiology/American Heart Association (ACC/AHA) guideline recommendation.
- Atherosclerosis-related cardiovascular disease (ASCVD) is a plaque buildup in arterial walls that results in arterial wall narrowing and is manifested by ischemic heart disease, ischemic stroke, peripheral arterial disease, aneurysm, or dissection.3
- Hypertension: persistently elevated systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg in patients aged 18 years and above, history of hypertension, or the use of anti-hypertensive drugs.22
- Diabetes mellitus: fasting serum glucose ≥126 mg/dl, history of diabetes mellitus or use of antidiabetic medications.3
- Chronic kidney disease: Abnormalities of kidney structure or function persisted for more than 3 months. Diagnosis was performed by clinical, biochemical (increased creatinine) and/or imaging (ultrasound-proven reduced/increased kidney size).23
- Good glycaemic control: Fasting blood sugar ranges from 80 to 130 mg/dl.3
- Lipoproteins are complexes of lipids and proteins in the blood and can be classified as low-density lipoproteins (LDL), high-density lipoproteins (HDL), and very low-density lipoproteins (VLDL) and their abnormality results in premature atherosclerotic cardiovascular disease (ASCVD).3
- Ten-year ASCVD risk score: This is a calculated value from a risk estimator model using multiple variables of age, sex, race, total cholesterol, blood pressure, hypertension medication, diabetes mellitus, and smoking status. It is used to predict the next 10-year risk for a first atherosclerotic cardiovascular disease event for patients without ASCVD. Patients with a score of 7.5% and above are considered to be intermediate- to high-risk patients for developing ASCVD and are indicated to start primary statin preventive therapy to prevent the patient from developing ASCVD.9
- Statins: are lipid-lowering agents that are given for patients with established ASCVD for secondary prevention or for patients who are at high risk of developing ASCVD events for primary prevention.3
- Regular follow-up: Patients who attended their follow-up regularly according to their schedule.20
- Irregular follow-up: Patients who do not attend their follow-up regularly and not according to their schedule.
Results
Sociodemographic Characteristics of the Study Participants
A total of 389 patients who were at high risk of atherosclerosis-related cardiovascular disease and had follow-up at the Debre Berhan Comprehensive Specialized Hospital Medical Follow-up Clinic were included in this study. The total response rate was 93%. Two hundred twenty-one (56.8%) of the participants were females. The mean age of the study participants was 55.4± 1.09. Most of the participants were married (68.12%) (Table 1).
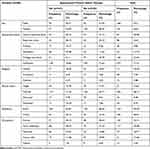 |
Table 1 Sociodemographic Characteristics of Patients with High ASCVD Risk at Debre Berhan Comprehensive Specialized Hospital Medical Follow-Up Clinic, from February 01 to May 30/2023 (n=389) |
Socioeconomic and Behavioural Factors
Twenty-one (5.4%) of the study participants were found to have a past/current smoking history. Most of the participants (74.1%) had community-based health insurance (Table 2).
 |
Table 2 Socioeconomic and Behavioural Factors of Patients with High ASCVD Risk at Debre Berhan Comprehensive Specialized Hospital Medical Follow-Up Clinic, from February 01 to May 30/2023 (n=389) |
Clinical Characteristics of the Study Participants
One hundred twenty-eight (32.9%) of the participants had diabetes mellitus (DM), of which fifty-six (43.75%) had DM-associated complications. One hundred eighty-four (47.3%) and thirty-six (9.25%) of the study participants were found to have hypertension and chronic kidney disease, respectively. One hundred thirty-three (34.19%) of the study participants had comorbidities other than hypertension and diabetes mellitus.
Most of the study participants (58.4%) had irregular follow-up, and 141 (36.25%) of them were treated (followed) by internists. One hundred sixty-nine (43.44%) of the study participants had at least one history of hospitalization. The mean of the ten-year ASCVD is 12.37 ± 0.2690, and the mean duration of DM was 8.05 ±0.42 (Table 3).
 |
Table 3 Clinical Characteristics of Patients with High ASCVD Risk at Debre Berhan Comprehensive Specialized Hospital Follow-Up Clinic, from February 01 to May 30/2023 (n=389) |
Primary Statin Preventive Therapy of Study Participants
Out of 389 study participants who were at risk of atherosclerosis-related cardiovascular diseases, 167 (42.93%) were on primary statin preventive therapy. Atorvastatin was the most common (94%) prescribed statin, followed by simvastatin (5%) (Figure 1).
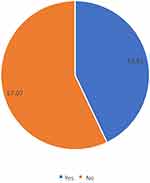 |
Figure 1 Primary statin preventive therapy status of patients with ASCVD risk at the Debre Berhan Comprehensive Specialized Hospital follow-up clinic from February 01 to May 30/2023 (n=389). |
Approximately 50% of patients who had regular follow-up were on primary statin preventive therapy. On the other hand, only 31.5% of patients with irregular follow-up were on primary statin preventive therapy. Approximately 58% and 34% of patients who were treated by internists and general practitioners were on primary statin therapy, respectively. (Table 3).
Out of 121 DM patients aged 40–75, 64 (52.9%) were on primary statin preventive therapy, whereas 28 (31.5%) of 89 high-risk patients with LDL greater than or equal to 190 mg/dl were found to be on primary statin preventive therapy. On the other hand, 75 (41.9%) of the high-risk patients with a 10-year ASCVD risk score of ≥7.5% were on primary statin preventive therapy (Figure 2).
Factors Associated with Appropriate Use of Primary Statin Preventive Therapy
The potential risk variables were entered into the bivariate analysis (binary logistic regression) to check for possible association with the dependent variable (primary statin preventive therapy). Accordingly, age of the participants, fasting blood sugar control level, duration of diabetes mellitus, DM complications, chronic kidney disease, other comorbidities, treating physician at follow-up clinic, history of hospital admission, other medications used, regularity of follow-up and ten-year risk of ASCVD were found to have p values of less than 0.2. Variables with p values less than 0.2 in the binary logistic regression were entered into the multivariate logistic regression.
After computing the multiple logistic regression, duration of diabetes mellitus, ten-year risk of ASCVD score, follow-up regularity and treating physician were found to have a statistically significant association with primary statin preventive therapy at P value <0.05 (Table 4).
As the duration of diabetes mellitus increases by one year, the proportion of patients with high risk of ASCVD who were prescribed primary statin preventive therapy increases by 33% (AOR=1.33, 95% CI: 1.1569–1.528).
A unit increment of ten-year risk of ASCVD risk score increases the status of primary statin preventive therapy for patients with high risk of ASCVD by about 13% (AOR=1.126, 95% CI:1.021–1.243).
Patients with a high risk of ASCVD and having regular follow-up are about 3 times more likely to be on primary statin preventive therapy compared to patients having irregular follow-up (AOR=3.11, 95% CI:1.029–9.417).
Patients with a high risk of ASCVD who are followed (treated) by internists are near to 3.9 times more likely to be on primary statin preventive therapy compared to high-risk patients who are followed by general practitioners (AOR=3.875, 95% CI:1.368 −10.969).
Discussion
A total of 389 high-risk patients for ASCVD were included in this study. Only 167 (42.93%) patients with a high risk of ASCVD who had follow-up at the medical follow-up clinic were found to be on primary statin preventive therapy. The rest of the patients who were at high risk of ASCVD were not on primary statin preventive therapy despite their eligibility.
The number of patients who were at high risk of ASCVD and who started on primary statin preventive therapy (42.93%, CI: 0.380–0.479) was lower than that in studies conducted in the United Kingdom (62%) and India (55.2%). The discrepancy between the findings could be the result of the difference in study participants in which only diabetic patients were included in the Indian studies, setup difference and the treating physician in which subspecialists were the treating physicians in the Indian study.24,25
On the other hand, compared to the studies conducted in the USA (31.1% and 32.5%), which were conducted about 10 years ago, this study showed a higher proportion of high ASCVD risk patients on primary statin preventive therapy (42.93%, CI: 0.380757–0.4792542). The discrepancy of the result could be the difference in the study design, the relatively low sample size used in this study, and the time gap between studies (10 years), as it allows for increased knowledge and improved practices, which may account for the differences observed.4,8
The magnitude of high ASCVD risk patients who were on primary statin preventive therapy (42.93%, CI: 0.380757–0.4792542) was found to be similar to the studies conducted 3 years back in Tanzania, Dareselam (47.3%), and 6 years back in Botswana, Gaborone (45.5%).10,13 When compared to the cross-sectional study of nationally representative, individual-level data from 2013 to 2019 conducted in 41 low- and middle-income countries (8.0%) and a study conducted from July 2015 to June 2018 in Ghana (16.8%), this study showed a higher proportion of high ASCVD risk patients were on primary statin preventive therapy.12,26 The discrepancy in the results could be the difference in the setup where the study was conducted (the study in Ghana included primary and secondary-level hospitals, which could lower the proportion of statin prescriptions and the relatively small sample size used in this study.
When compared to the study conducted in Bonga, Ethiopia, the proportion of high ASCVD risk patients who were on primary statin preventive therapy (42.93%, CI: 0.380757–0.4792542) was found to be similar (40. %).27 On the other hand, compared to the study conducted in Jimma Medical Centre, Ethiopia (36.6%), this study showed a higher proportion of high ASCVD risk patients were on primary statin preventive therapy (42.93%, CI: 0.380757–0.4792542).28 The relative higher proportion of patients being on primary statin preventive therapy despite having a relatively similar setup could be due to the time gap between the two studies were conducted as it allows for increased knowledge and improved practices, which may account for the differences observed.
The proportion of patients who were at high risk of ASCVD and who were on primary statin preventive therapy (42.93%, CI: 0.380757–0.4792542) was lower than that in a study conducted in Aksum, Ethiopia (55.7%).21 The discrepancy between the findings could be the result of the difference in study participants in which only diabetic patients were included in the Aksum Study. Patients with high ten-year ASCVD and high LDL values were also included in this study, which could lower the proportion of primary statin preventive therapy since ten-year ASCVD risk calculation and LDL-level determination need access to laboratory investigations and understanding of the calculation.
This study showed that the duration of diabetes mellitus had a significant association with primary statin preventive therapy, which could be explained by the fact that as the duration of diabetes mellitus increases, the likelihood of being treated with different professionals with different levels of understanding of primary statin preventive therapy is highly likely. The other possible explanation could be that as the duration of DM increases, the likelihood of having DM-associated complications and other metabolic diseases, including dyslipidemia and hypertension, increases, which in turn increases the likelihood of prescribing statin preventive therapy. Similar studies conducted in Iraq, Botswana, and Ethiopia showed that an increase in the duration of DM had a similar association with a higher proportion of primary statin preventive therapy.13,15,28
In this study, the ten-year risk score of ASCVD was also found to have a significant association with primary statin preventive therapy. This significant association could be due to the fact that the higher the ten-year ASCVD risk score, the higher the probability of having metabolic diseases since the ten-year ASCVD risk score uses the values of diabetes mellitus, hypertension, different cholesterol values, and history of smoking for its calculation. Other studies conducted in the USA and India also showed a similar association of ten-year risk with the use of primary statin preventive therapy.8,25
This study also showed that follow-up regularity had a significant association with primary statin preventive therapy, in which a higher percentage of patients with regular follow-up were found to be on statin preventive therapy compared to patients having irregular follow-up. The possible explanation for this significant association could be that patients with regular follow-up could have frequent exposure to health professionals so that the possibility of being on statin preventive therapy increases as well.
In this study, there was also a significant association between primary statin preventive therapy and treating physicians in which high-risk patients who were followed (treated) by internists were more likely to be on primary statin preventive therapy than high-risk patients who were followed by general practitioners. The explanation could be that internists had a better understanding of the importance of primary statin preventive therapy and knowledge of the indications to start primary statin preventive therapy. Similar studies in India, Ghana, and Ethiopia also showed that the specialty of the prescriber, knowledge of the newer clinical practice guidelines, and underestimation of patient risk by physicians affected the prescription and use of statins as recommended by guidelines.9,25,27
Limitations of the Study
The study was performed in a comprehensive specialized hospital in which relatively senior physicians attend patients with relatively better access to laboratory investigations so that the actual figure of primary statin preventive therapy might be overestimated. This is a single centre study with relatively small sample size that might be difficult for generalization of the findings.
Conclusion
The magnitude of patients who were on primary statin preventive therapy was low (approximately 43%). Improving the regular follow-up of high-risk patients for ASCVD and making senior physicians (internists) attend patients at follow-up clinics would significantly improve the number of patients with primary statin preventive therapy. Duration of diabetes mellitus and ten-year ASCVD risk score are strongly associated with a better proportion of patients to be on primary statin preventive therapy.
Recommendations
Physicians should counsel their patients about the importance of regular follow-up. Every patient with a high risk of ASCVD should be assessed for indications to start primary statin preventive therapy. The number of patients who are on primary statin preventive therapy could be increased by making senior (internists) physicians attend patients at the follow-up clinic. Large-scale studies to improve the understanding of primary statin preventive therapy should be conducted.
Abbreviations
ACC, American College of Cardiology; AHA, American Heart Association; ASCVD, Atherosclerosis-Related Cardio Vascular Disease; CKD, Chronic Kidney Disease; CI, Confidence Interval; CVD, Cardiovascular Disease; DBCSH, Debre Berhan Comprehensive Specialized Hospital; DBU, Debre Berhan University; DM, Diabetes mellitus; FBS, Fasting Blood Sugar; IDF, International Diabetic Federation; LDL-C, Low-density lipoprotein-cholesterol; OR, Odds Ratio; RBS, Random Blood Sugar; WHO, World Health Organization.
Data Sharing Statement
The data used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
All the methods of this research were done in accordance with the declaration of Helsinki. Ethical clearance and approval to conduct the research was obtained from Debre Berhan University, Asrat Woldeyes Health Science Campus, Institutional Review Board (IRB) office with Reference No. of IRB 01/121/2015 and Protocol Number IRB-180. Official letters were written from the IRB office to the Debre Berhan Comprehensive Specialized Hospital. Formal letter of permission was obtained from Debre Berhan Comprehensive Specialized Hospital administrative body. Informed consent was obtained from study participants to confirm their willingness to participate after the objective of the study was explained. Respondents were clearly told that they had the right to refuse or terminate at any point of the interview. Respondents were reassured that they were to be anonymous. During the data collection process, those patients who were found to be at high risk of ASCVD were taken care of as per the guideline recommendation.
Acknowledgments
The authors greatly appreciate the cooperation and support of all participants and are grateful to data collectors and supervisors.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, interpretation, drafting, revising, and critically reviewing the article. All authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript and approved its submission for publication in Dove Medical Press.
Disclosure
The authors declare that they have no competing interests.
References
1. Toth PP, Banach M. Statins: then and now. Methodist Debakey Cardiovasc J. 2019;15(1):23. doi:10.14797/mdcj-15-1-23
2. Celermajer DS, Chow CK, Marijon E, Anstey NM, Woo KS. Cardiovascular disease in the developing world: prevalences, patterns, and the potential of early disease detection. J Am Coll Cardiol. 2012;60(14):1207–1216. doi:10.1016/j.jacc.2012.03.074
3. Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J. Harrison’s Principles of Internal Medicine.
4. Saeed A, Zhu J, Thoma F, et al. Cardiovascular disease risk–based statin utilization and associated outcomes in a primary prevention cohort: insights from a large health care network. Circ Cardiovasc Qual Outcomes. 2021;14(9):e007485. doi:10.1161/CIRCOUTCOMES.120.007485
5. Abukhalil AD, Alyan M, AbuAita W, Al-Shami N, Naseef HA. Adherence to clinical guidelines on STATIN prescribing among diabetic patients aged 40–75 years old in a primary care setting: a cross-sectional study. Patient Prefer Adherence. 2022;16:1855–1863. doi:10.2147/PPA.S376000
6. Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e563–e595. doi:10.1161/CIR.0000000000000677
7. Bates T, Connaughton V, Watts G. Non-adherence to statin therapy: a major challenge for preventive cardiology. Expert Opin Pharmacother. 2009;10(18):2973–2985. doi:10.1517/14656560903376186
8. Chobufo MD, Regner SR, Zeb I, Lacoste JL, Virani SS, Balla S. Burden and predictors of statin use in primary and secondary prevention of atherosclerotic vascular disease in the US: from the National Health and Nutrition Examination Survey 2017–2020. Eur J Prev Cardiol. 2022;29(14):1830–1838. doi:10.1093/eurjpc/zwac103
9. Brobbey FS, Malick MMD, Adjei S. Statin therapy prescribing patterns for primary prevention of cardiovascular disease in patients with type 2 diabetes mellitus receiving primary care at the tamale teaching hospital (TTH) in Northern Ghana. EAS J Pharm Pharmacol. 2020;2:74–82.
10. Bideberi AT, Mutagaywa R. Statin prescription patterns and associated factors among patients with type 2 diabetes mellitus attending diabetic clinic at Muhimbili National Hospital, Dar es Salaam, Tanzania. Diabetes Metabol Syndr Obes. 2022;15:633–646. doi:10.2147/DMSO.S347765
11. Go AS, Fan D, Sung SH, et al. Contemporary rates and correlates of statin use and adherence in nondiabetic adults with cardiovascular risk factors: the KP CHAMP study. Am Heart J. 2017;194:25–38. doi:10.1016/j.ahj.2017.08.013
12. Sarfo FS, Ovbiagele B. Prevalence and predictors of statin utilization among patient populations at high vascular risk in Ghana. J Neurol Sci. 2020;414:116838. doi:10.1016/j.jns.2020.116838
13. Mwita JC, Godman B, Esterhuizen TM. Statin prescription among patients with type 2 diabetes in Botswana: findings and implications. BMC Endocr Disord. 2020;20(1):1–9. doi:10.1186/s12902-020-0516-7
14. Steen DL, Khan I, Becker L, et al. Patterns and predictors of lipid‐lowering therapy in patients with atherosclerotic cardiovascular disease and/or diabetes mellitus in 2014: insights from a large US managed‐care population. Clin Cardiol. 2017;40(3):155–162. doi:10.1002/clc.22641
15. Mohammed WK, Alwash SJ. Rate of prescribing statins for primary prevention of atherosclerotic cardiovascular disease in diabetic patients. Iraqi Postgraduate Med J. 2022;21(2):1–10.
16. Wallach-Kildemoes H, Andersen M, Diderichsen F, Lange T. Adherence to preventive statin therapy according to socioeconomic position. Eur J Clin Pharmacol. 2013;69(8):1553–1563. doi:10.1007/s00228-013-1488-6
17. Bradley CK, Wang TY, Li S, et al. Patient‐reported reasons for declining or discontinuing statin therapy: insights from the PALM registry. J Am Heart Assoc. 2019;8(7):e011765. doi:10.1161/JAHA.118.011765
18. Jones N, Fischbacher C, Guthrie B, et al. Factors associated with statin treatment for the primary prevention of cardiovascular disease in people within 2 years following diagnosis of diabetes in Scotland, 2006–2008. Diabetic Med. 2014;31(6):640–646. doi:10.1111/dme.12409
19. Berthold HK, Gouni-Berthold I, Böhm M, Krone W, Bestehorn KP. Patterns and predictors of statin prescription in patients with type 2 diabetes. Cardiovasc Diabetol. 2009;8(1):1–12. doi:10.1186/1475-2840-8-25
20. Brookhart MA, Patrick AR, Schneeweiss S, et al. Physician follow-up and provider continuity are associated with long-term medication adherence: a study of the dynamics of statin use. Arch Intern Med. 2007;167(8):847–852. doi:10.1001/archinte.167.8.847
21. Demoz GT, Wahdey S, Kasahun GG, et al. Prescribing pattern of statins for primary prevention of cardiovascular diseases in patients with type 2 diabetes: insights from Ethiopia. BMC Res Notes. 2019;12(1):1–7. doi:10.1186/s13104-019-4423-9
22. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127–e248. doi:10.1016/j.jacc.2017.11.006
23. Johnson R, Feehally J. Comprehensive Clinical Nephrology
24. Steen DL, Khan I, Ansell D, Sanchez RJ, Ray KK. Retrospective examination of lipid-lowering treatment patterns in a real-world high-risk cohort in the UK in 2014: comparison with the National Institute for Health and Care Excellence (NICE) 2014 lipid modification guidelines. BMJ open. 2017;7(2):e013255. doi:10.1136/bmjopen-2016-013255
25. Gupta R, Lodha S, Sharma KK, et al. Evaluation of statin prescriptions in type 2 diabetes: India Heart Watch-2. BMJ Open Diabetes Res Care. 2016;4(1):e000275. doi:10.1136/bmjdrc-2016-000275
26. Marcus ME, Manne-Goehler J, Theilmann M, et al. Use of statins for the prevention of cardiovascular disease in 41 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data. Lancet Global Health. 2022;10(3):e369–e379. doi:10.1016/S2214-109X(21)00551-9
27. Feyisa D, Feyisa D. Determinants of statin initiation among adult diabetic patients in Bonga, Ethiopia. Diabetes Metabol Syndr Obes. 2020;13:4839. doi:10.2147/DMSO.S283993
28. Melaku T, Solomon Y, Chelkeba L. Statin utilization patterns among Type 2 diabetes mellitus patients with high cardiovascular disease risks in Ethiopia. J Pharm Care. 2018;6(3–4):44–51.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


