Back to Journals » Veterinary Medicine: Research and Reports » Volume 15
Assessment of Knowledge, Attitude and Practice (KAP) Regarding Antimicrobial Usage and Resistance Among Animal Health Professionals of East Wallaga Zone, Oromiya, Ethiopia
Authors Bulcha B , Motuma B, Tamiru Y , Gurmessa WT
Received 9 November 2023
Accepted for publication 8 February 2024
Published 29 February 2024 Volume 2024:15 Pages 57—70
DOI https://doi.org/10.2147/VMRR.S443043
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Young Lyoo
Begna Bulcha, Bayisa Motuma, Yobsan Tamiru, Waktola Tadesse Gurmessa
Department of Veterinary Medicine, School of Veterinary Medicine, Wallaga University, Nekemte, Oromia, Ethiopia
Correspondence: Begna Bulcha, Email [email protected]
Background: Antimicrobial resistance (AMR) is one of the top global public health and economic threats. The use of antimicrobials (AMs) in animal production is a major contributor to the development of AMR globally. Animal health professionals (AHPs) play a key role in ensuring judicious use of AMs.
Objective: To assess the knowledge, attitude and practice (KAP) of antimicrobial usage (AMU) and AMR among healthcare professionals in Nekemte town, Leka Dulecha and Sibu Sire districts.
Methods: A cross-sectional study was conducted with 120 purposively chosen AHPs residing in the districts and the town. A semi-structured questionnaire consisting of 49 questions was used to ascertain the KAP. The chi-square test (X2) was used to analyze the association between the knowledge score and demographic profile of the study participants.
Results: In the study the overall knowledge of the participants was moderately appreciable, and all participants had positive attitudes toward AMR and appropriate usage. In terms of knowledge of antibiotic use, the majority (93.33%) of the participants correctly answered the statement that antibiotics can kill viruses. About 84.17% of the participants correctly knew that antibiotics killed or stopped the growth of both bad and good bacteria. The majority of the participants (74.17%) always or (25.83%) sometimes rely on usage of antibiotics without a doctor’s prescription. It was shown that comparing respondents from Sibu Sire, Leka Dulecha and Nekemte town, the scores of knowledge of AMU were significantly (X2=14.13, p=0.007) different. Most animal healthcare professionals from the Sibu sire have a good knowledge of AMU, and contribute to AMR development.
Conclusion: The study revealed that there was moderate knowledge and positive attitude toward AMU and resistance. This warrants continuing capacity building programs for the professionals on AM usage and resistance, and development of field-friendly disease diagnosis and management tools is essential in the need to reduce AMR.
Keywords: antimicrobial use, antimicrobial resistance, attitude, East Wallaga zone, knowledge score
Introduction
Globally, antimicrobials are extensively prescribed in the livestock industry for treatment and prevention of disease.1,2 The anticipated growth and expansion of livestock productions to meet the increasing demands for animal products is expected to double the consumption of AMs in the livestock sector in developing countries by 2030.3,4 Antimicrobial resistance occurs when microorganisms (such as bacteria, fungi, viruses, and parasites) change when they are exposed to antimicrobials (such as antibiotics, antifungals, antivirals, antimalarials, and anthelmintics).5 As validated by various studies, AMU in animal production is considered an important driver of AMR.6–8
Overuse and misuse of AMs are big factors that can aggravate the development of AMR. It is indicated that AMR is intimately tied to all forms of AMU, and is favored when its use is suboptimal or widespread. In precise, avoidable practice that is recognized as key contributors to AMR include AMU in animal production for growth promotion, prophylaxis, and metaphylaxis; AMU without professional oversight; and AMU after poor diagnostic techniques.9 The transmission of AMR is facilitated by trade, travel, and human and animal movement. Resistant microbes can be in animals and food products intended for human consumption.5
Due to the demand increment for animal origin protein, AMU as food for animal growth promotion will double the use of AMs in the near future, according to the World Food Organization.5 AHPs are key role players in the prescription and use of antimicrobials, they may respond to clients/patients' inappropriate request or carry out inappropriate practices, which in turn increase the chance of AMR.10 As suggested by American Veterinary Medical Associations,11 the “judicious use of antimicrobials in food-producing animals” targets the use of AMs when compulsory for the treatment, prevention, and control of diseases with confirmed diagnosis. The existed trend has dissimilarity to this recommendation (ie AMs are carelessly used in animal origin food chains in different parts of the developing countries of the world), including Ethiopia.12
Assessment regarding AMU in food animals is of paramount importance for understanding and preventing the potential risk posed by AMR to animal and public health and economy of a country.13,14 It is revealed that detailed understanding of AMU can pave the way for tackling AMR and taking effective action against it.15 To date, in developing countries, little is known about judicious use of and the factors underlying AMR. Inconsistent policy governing AMU in animal production, absence of AMU regulations that restrict access to critically important antimicrobials without prescriptions, and lack of systematic post-marketing quality surveillance of veterinary AMs are the most important challenges in less developed countries.16
As per the information gained from the Central Statistical Agency (CSA),17 Ethiopia has the largest livestock populations in Africa, indicative of abundant usage of AMs for health maximization. On another side, its agroecological zones are suitable for accommodating a plethora of pathogens that can affects the livestock health and hence productivity. To fit the demand for animal origin food as the country population grows at an increasing rate, the livestock sector has started to dramatically increase livestock production,18 and this in turn increases the utilization of antimicrobials.3,4 A few studies conducted in the country revealed the presence of antimicrobial residues in animal origin food, and poor AMU practice among food animal rearing communities.12,19 However, information generated from the western part of the country, Ethiopia, where an extensive farming and abundant livestock exists and numerous AHPs are working is scarce. Obviously, inappropriate use of antimicrobials in animals shares a greater part in the development and persistence of AMR and occurrence of drug residue. It is revealed that detailed understanding of AMU can pave the way for tackling AMR and taking effective action against.20 Monitoring AMU in livestock production provides useful information for policy development to reduce AMR risks, all this information can be accessed from animal health professionals (AHPs), and hence understanding or assessing their KAP is very crucial to develop their capacity in mitigating AMR and residues. Therefore, the goal of the current study was to assess the knowledge, attitude and practice (KAP) toward antimicrobial usage and resistance development among AHPs in Nekemte town, Leka Dulecha and Sibu Sire districts.
Materials and Methods
Descriptions of the Study Areas
The study was conducted from December 2022 to June 2023 in Leka Dulecha, Sibu Sire District, and Nekemte town (Figure 1), Eastern Wallaga Zone, Western Ethiopia. Nekemte town is situated 330 km from Finfinne, Ethiopia’s capital city. Geographically, the town is situated in Guto Gida district which is located between 8° 27N and 10° 13N latitude and 38° 08E and 37° 38E longitude. The climate was divided into three categories: highland (28.6%), midland (50.9%), and lowland (20.5%). The annual temperature of the district falls in the range of 14−26 °C, with the annual rainfall range of 1000–2400 mm.
 |
Figure 1 Map of the study Areas (Created by ArcGIS_WGS_1984). |
Leka Dulecha District is located approximately 358 km west of Finfinne, and 27 km west of Nekemte. The capital of Leka Dulecha is known as Getema. The district is bordered by Nuno Kumba to the south, Guto Gida in the East, Buno Bedelle in West and by Diga in the North and by Jima Arjo to the south (Figure 1). It has three agroecological zones: lowlands (44%), midlands (47%), and highland (9%). The area receives an annual rainfall ranging from 1000–2200 mm, with minimum and maximum temperature 12 °C to 29 °C.
Sibu Sire District is in Ethiopia’s Oromia National Regional State, specifically in the East Wallaga zone. It is roughly 50 km from Nekemte, the zonal town, and 280 km from Finfinne, the capital city. Its geographic coordinates are 8° 16’20N to 10° 16’40N and 36° 47’00E to 37° 0’00E.21 According to the Sibu Sire Agricultural Office/SSAO (2018), the district is bordered by Gobu Seyo in the east, Wayu Tuka in the west, Gudeya Bila and Guto Gida in the north, and Wama Hagalo and Billo Boshe in the south.
Study Participants
The study participants/populations were animal health professional individuals who were working and residing in Leka Dulecha, Sibu Sire District, and Nekemte town. This study included individuals of both sexes, age categories (>18 years), and religious backgrounds.
Study Design
To ascertain the KAP of antibiotic consumption and resistance among the professionals, an observational cross-sectional study was carried out with 120 purposefully selected veterinary care professionals in the study locations. The study included a self-directed questionnaire.
Sampling Methods and Sample Size Determination
The numbers of study participants were determined according to the sample size calculation recommended by Arsham,22 and Whitley and Ball.23 Accordingly, by considering standard error of 5%, precision level of 5% with 95% confidence interval and 17% of proportion of attrition, a total of 120 samples were considered.
Reliability and Validity of the Data
For the reliability and validity of the data used in this study the questionnaire developed by the research team was received by other researchers, and the research committee of Wallaga University School of Veterinary Medicine. The questionnaire was also pre-tested by attempting a pilot study and some refinement and correction were made.
Data Collection and Measurement Tools
A semi-structured questionnaire was developed after reviewing the literature on how to conduct a KAP survey and global antimicrobial studies. The questionnaire consists of closed and open ended questions, with a majority of closed ended. The questionnaire survey was conducted by interviewing individuals about their socio-demographic profiles, followed by specific questions related to the KAP of animal health professionals regarding AMU in animals and AMR of animal disease. The questionnaire was administered to animal health professionals living in Leka Dulecha Sibu Sire and Nekemte Town. They were also briefed about the objective of the survey and asked for their consent before the interview commenced. The KAP tool focuses on knowledge and attitudes of AHPs on and toward AMU and AMR respectively.
Data Management and Analysis
After being gathered, the data were entered into a 2016 Microsoft Excel spreadsheet and error-checked. STATA (version 15.1) was used to import and analyze the data. The findings of the practice, knowledge, attitudes, and demographic questions were presented using summary statistics like proportion and frequency. Using an Excel spreadsheet, knowledge and attitudes were scored. The correlation between KAP scores and the study participants’ demographic profiles and knowledge scores and the respondents’ practices was examined using the chi-square test. With a 95% confidence level and 5% precision level selected as the statistical significance threshold, a p-value of less than 0.05 was deemed significant.
The questionnaire comprised eight questions about practice, twenty questions about attitudes, and 19 questions for knowledge, seven of which were on a Likert scale. The knowledge and attitude questions were scored on a five-point Likert scale, which goes from 1 to 5. The least appropriate response received a score of 1, while the most acceptable response received a score of 5. In the knowledge part, the lowest and greatest possible scores were 7 and 35, respectively. In the attitude part, a score of 20 was the lowest achievable and a score of 100 the greatest. The scores were converted into a scale with 0 being the lowest possible score and 100 being the highest possible score using the scoring formula mentioned (described by the WHO),24,25 after determining the mean for each respondent. To interpret the analysis output from the scoring scheme, a score greater than 80% of the possible maximum score was considered good, between 60–80% moderate, and less than 60% considered poor.26
Results
Socio-Demographic Profiles of the Respondents
From the total 120 study participants, 64.17% were male and 35.83% were female. Approximately 25.83% of the healthcare professionals were from Sibu Sire, whereas 46.67% were from Nekemte Town, and 27.50% from Leka Dulecha. Out of the participants, 21.66% fall into the age group of 18–24 years old, 60.83% into the age group of 25–34 years old, and 15% into the age group of 35–44 years old. The majority (55.00%) of the participants have work years’ experience of 5–10 years (Table 1).
 |
Table 1 Socio-Demographic Profile of the Respondents |
Knowledge of AHPs on Antimicrobial Usage and Antimicrobial Resistance
The respondents’ knowledge was assessed using 12 true or false questions administered via a questionnaire, and the majority of respondents answered each question correctly. However, more than half (56.67%) of the respondents fails to get appropriate answers to the statements stated as
Even if man consumes antibiotics in meat/milk, it will only make him healthier; and Antimicrobial resistant-microbes are found in people, animals, food, and the environment (Table 2).
 |
Table 2 Knowledge of Participants About Antimicrobial Usage and Resistance |
In terms of knowledge of antibiotic use, the majority of respondents (93.33%) correctly answered the statement that antibiotics cannot kill viruses; 6.67% incorrectly that antibiotics kill viruses. Slightly more than half of the respondents were (84.17%) correct and (15.83%) incorrect when asked if “Antibiotics kill or stop the growth of both good and bad bacteria.” When respondents were asked whether the overuse of antibiotics made them become ineffective, 90.83% were correct and 9.17% incorrect in their responses. The majority of the respondents (95.83%) were correct (9.17% incorrect) when asked about over and underuse of antimicrobials can cause antimicrobial-resistant resistance microorganism. More than half of respondents were asked, “Man can consume antibiotics as a result of eating meat/drinking milk” with 90.83% correct and 9.17% however incorrect. The majority of the participants (83.33%) said that a withdrawal period did not have to be observed for milking cows treated with antibiotics such as penicillin before milk can be consumed (Table 2).
From 120 healthcare professionals, agreed was 90.00%, disagree 18.33%, and neutral 30.337% on long duration of antibiotic treatment can lead to AMR. They also showed 50.83% agree, 9.17% neutral, 40.00% disagree with healthy people and animals can carry antibiotic resistant bacteria. Most of healthcare professionals (97.5%) agree, 0.83% neutral, and 1.67% disagree on the under-dosing of antibiotic-resistant bacteria contributing ABR. The majority of healthcare professionals (87.50%) agree, 7.50% neutral, and 5.00% disagree on excessive use of antibiotics in livestock, and food production contributes to ABR. Also about 86.67% agree, 10.83 neutral and 2.50 disagree that less public health awareness of antibiotics can cause antibiotic resistance (Table 3).
 |
Table 3 Knowledge of AHPs Toward AMU and AMR Based on the Likert Scale |
Attitude of AHPs Toward Antimicrobial Usage and Antimicrobial Resistance
In this study the majority of animal healthcare professionals stated (75.00% agree) that prescribing unnecessary antibiotics is a professional unethical problem. Many healthcare professionals (72.50%) agree, 24.17% strongly agree, 2.50% disagree, and 0.83% neutral on inappropriate antimicrobial use can lead to resistance. Drugs can be transferred to humans by consumption meat of animals treated recently (63.33% agree, 3.33% neutral, 5.00% disagree, 28.33% strongly agree). Also 75.00% agree, 21.67% strongly agree, 2.50% neutral and 0.83% strongly disagree on “Application of one health approach is important to control antimicrobial resistance”, and on “Broad spectrum antibiotics should be used in place of narrow spectrum antibiotics to reduce resistance” the majority of healthcare professionals (50.00%) disagree, 36.67% neutral, 5.83% agree, 4.17% strongly disagree and 3.33% strong agree (Table 4).
 |
Table 4 Attitude of Healthcare Professionals Toward Antimicrobial Usage and Antimicrobial Resistance |
Total Knowledge and Attitude Score
The mean±SD of knowledge was 66.88±6.90% (Table 5). The maximum and minimum knowledge scores were 75.00 and 46.43%, respectively. This indicates that most respondents had moderate knowledge of antimicrobial usage and the development of resistance. For attitudes, the mean and standard deviation were 66.17±6.89. This finding revealed that, on average, the respondents had a positive attitude toward antimicrobial usage.
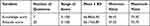 |
Table 5 Number of Questions, Range, Scores, and Level of Knowledge and Attitude of the Participants |
Practice of Animal Health Professionals During Their Antimicrobial Usage
In this study, many participants stated (74.17%) always and (25.83%) sometimes on “Usage of antibiotics without doctor’s prescription.” Out of 120 participants, 76.67% sometimes, 15.00% always and 8.33% never responded to the study on repeated use of same drugs for a disease with similar clinical signs, and more than half (82.50%) never, (16.67%) also sometimes, and (0.83%) always on “How often do you undertake antimicrobial sensitivity testing before starting antibiotic treatment.” A large number of the participants (86.67%) stated their own previous experience, (10.83%) owner preference for a specific antibiotic, and (2.50) advice from colleagues on factors influencing their decision the most important when selecting an antibiotic to use. However, most of them had an incorrect response to questions asked about factors influencing their decision the most important when selecting an antibiotic to use, with 54.17% the cost of antibiotic drugs, 35.83% owner’s ability to pay, 6.67% marketing offers, 2.50% advertisements by drug representatives, and 0.83% profit margins for veterinarians (Table 6).
 |
Table 6 Practice of Professionals Toward Antibiotic Usage, Resistance, and Residue Development |
Association of Knowledge Score with Socio-Demographic Characteristics on AMU
The results of the chi-square analysis showed that comparing participants from Sibu Sire, Leka Dulecha, and Nekemte town, the knowledge of antimicrobials varied significantly (p=0.007). The antimicrobial knowledge scores tended to high (48.39%) in professionals from Sibu sire, followed by those from Nekemte sire. The majority (71.43%) of participants from Nekemte town had moderate knowledge regarding AMU and resistance. High AMR knowledge scores were associated with male sex. Individuals with experience of between 10–50 years of work experience had moderate knowledge scores for antimicrobial usage and means of drug resistance (Table 7).
 |
Table 7 Association of Knowledge and Attitude, and Influencing Factors |
Discussion
Various studies have demonstrated that inappropriate use of antibiotics, especially antibiotics shared between humans and animals, plays an important role in the occurrence of AMR.27,28 Knowing the KAP of professionals and the intervening is very important against AMU and AMR.29 Livestock diseases are a priority issue for livestock farmers across Ethiopia and other low-income countries with large livestock populations and diverse climatic conditions that favor the emergence of pathogens. Antibiotics are widely used to control a variety of diseases.30,31 Farmers’ access to, use of, and satisfaction with veterinary services vary significantly across livestock systems, geographic regions, socioeconomic classes, and service providers.32 Varying levels of resistance to drug-resistant bacteria have also been reported in livestock, in agricultural environments, and in agricultural workers, posing a serious threat to public health and the economy in low-income countries, including Ethiopia.33,34 Therefore, monitoring AMU in livestock production provides useful information for policy development to reduce AMR risks.20 Thus, the main objective of this study was to assess the knowledge, attitude and practice (KAP) on antibiotic use and resistance development among AHPs in Leka Dulecha, Sibu Sire District, and Nekemte town.
The Knowledge of AHPs About Antimicrobial Usage and Antimicrobial Resistance
A better understanding of vaccines, antibiotics, antibiotic residues, drug withdrawal, and AMR is needed to reduce the risk of AMR. Vaccines are used prophylactically to reduce the occurrence of infectious diseases, the use of antibiotics, and the emergence and spread of AMR.35 In this study, the majority (93.33%) of respondents correctly knew that antibiotics are not effective against viral infections. This number is higher than the findings of Sobeck et al,36 which found that 57% of respondents in the United States believe that antibiotics can cure viral infections. There are differences between studies, in Romania, 37.51% of respondents believe that antibiotics can treat viral infections.37 This difference may be due to the fact that the respondents in this study were professionals.
In this study, respondents showed a high level of knowledge about the use of antibiotics. However, only more than half (56.67%) of the respondents fail to get appropriate answers to the statement stated as “Even if man consumes antibiotics in meat/milk, it will only make him healthier.” This may be because most animal healthcare professionals lack knowledge of antimicrobial residues. This warrants transparent communication between livestock experts and stakeholders to create awareness.
According to the results of this study, many participants (85.00%) knew that if bacteria become resistant to antibiotics, treating the infections they cause can be very difficult. This result is slightly higher than research conducted in Bahir Dar (69.7%),38 Jordan (50%),39 and Namibia (72%).40 These variations may be the result of differences in expert understanding of antibiotic-resistant bacteria. Less than half of veterinary professionals (43.33%) knew that drug-resistant bacteria have been found in humans, animals, foods, and the environment. This study is different from the study conducted in Bangladesh (80.5%).41 This variation may have resulted from lack of understanding and exposure.
According to the results of the current study, more than half (50. 83%) of the participants agreed with the view that health people and animals can carry antibiotic resistant bacteria. According to a report by Xian Municipal Human resources and social security Bureau (XMHRSSB, 2018)42 the knowledge of participants in this study was higher than that of a previous Chinese survey conducted in 2015. This higher knowledge might be explained by the fact that respondents in the present study were more concerned about their antibiotic use than the experts. Given that increased UAM frequency is an important factor contributing to AMR, especially when used improperly,43–45 it is reasonable that suggest that these antimicrobial drugs increase the risk.
Attitude of AHPs Toward Antimicrobial Usage and Antimicrobial Resistance
The study participants’ attitude toward the AMU and resistance were the internal perception and feelings that AHPs had toward antibiotic stewardship, which could be positive or negative. In this study, 18.33% strongly agreed that prescribing unnecessary antibiotics was a professional unethical problem. This result is similar to that reported for Jordan.39 However, this is not similar to the study in Harar City where 31% of participants who prescribed unnecessary antibiotics is a professional unethical problem. This difference was a result of respondents’ professional backgrounds. Many animal healthcare professionals (48.33%) agree, 5.83% strongly agree, and 39.17% disagree on inappropriate antimicrobial use can lead to resistance. This difference was a result of respondents’ professional backgrounds.
Most animal healthcare professionals (72.50% agree) on inappropriate antimicrobial use can lead to resistance. There was significant variation between the studies in Oromiya zone; 28.9% of respondents appreciated that irrational AMU can lead to antimicrobial resistance.12 It also differs from a study in Switzerland (63.7%).46 About 45.6% of the subjects agreed that the overuse of antibiotics will lead to antibiotic resistance.47 This discrepancy may be due to the inadequate instruction received at school.
The majority of AHPs (45.00%) responded strongly disagree that more cautious use of antibiotics would reduce antibiotic resistance. Unlike the study conducted at Fitche Hospital, more than half (59%) of the respondents strongly disagreed that more cautious use of antibiotics would reduce antimicrobial resistance.48 In this study, the majority of medical experts (50.00%) disagreed that broad-spectrum antibiotics used should be instead of narrow spectrum to reduce drug resistance. There were many variations; in the Colombian study, 24.6% said it better to prescribe broad spectrum antibiotics to ensure patients are cured of infection than narrow spectrum, and in the study conducted at Fitche Hospital, 35% of experts responded that broad spectrum antibiotics should be used instead of narrow spectrum to reduce drug resistance.48 This discrepancy might be due to the lack of understanding the intended use of broad and narrow spectrum antibiotics.
Practice of Animal Health Professionals on AMU and AMR
A strong association between AMU and AMR in livestock has been observed in observational studies and surveillance data.49 Many causes are attributed to excessive and inappropriate use AM in livestock farming. The lack of national guidelines, the poor quality of veterinary products on markets, the way pets are treated by owners, the lack understanding of danger of overuse, and the lack of access to veterinary drugs over-the-counter by the public are some of these problems.49–51
The observed driver of improper AM prescription is multifactorial. Laboratory diagnostic and AM sensitivity tests are important guides for the selections of AM by veterinarians.52 However, resource-poor countries are still lagging partly because of their limited laboratory capacity.53 Therefore, most veterinary professionals rely primarily on signs and clinical experience to diagnose and treat animals. In the current study, most (82.50%) of the professionals did not undergo antimicrobial sensitivity testing before starting antibiotic treatment. This clinical sign-based diagnosis, and hence, treatment, can only be effective in advanced clinical settings where field diagnostics are used. The development and use of field friendly diseases diagnostics and management tools may be improve AMU and reduce AMR. Examples include the Faffa Malan Chart (FAMACHA) for detecting anemia in sheep in tropics54 and the use of body weight estimation bands for other breeds and cross breeds in Senegal for accurate dosing in veterinary medicine drug used.55
Regarding the factors influencing professional decision in AMR development, most (74.17%) of the respondents used antibiotics without doctor’s prescription for themselves. The veterinary profession in impoverished nations is accustomed to facing challenges in the prescriptions and use of antibiotics. Animal owners throughout Africa frequently purchase AM without a prescription from a veterinarian, utilize leftover AM and refuse to pay for diagnostic testing.56,57 Additionally, many African countries reported other reasons, such as limited access to veterinary professionals and the subsequent involvement of the informal veterinary sector in the distribution of AM.51 To ensure sufficient UAM across the continent, it is important to strengthen the capacity of public and private veterinary services.
In the current study, the owner’s preference for a particular antibiotic (10.83%) and my previous experience (86.67%) with these factors influenced the respondents’ most important decision when choosing to use an antibiotic. It has also been suggested elsewhere that veterinary physicians attempt to meet clients/patients' expectation even when they believe antibiotics are necessary.58,59. Health facilities in most low and middle income countries are characterized by inadequate laboratory facilities and high patient to clinician ratios.60–62
Conclusion and Recommendations
In order to combat AMR in animal and human health, careful research and comprehension of AM consumptions are necessary. Professionals in animal health can play a crucial role in reducing AMR and misuse of AM, its occurrence in animal-derived foods, and the associated risk to human health. The key roles of AHP in combating AMR is usage of AM judiciously with prescription, hence reducing both residue (by insisting the withdrawal period) and resistance (via wise use of right drug at right time for right patient). They are the close friend of livestock owners. The majority of animal healthcare professionals from both the study districts and Nekemte town had moderate knowledge. Regarding sex, the majority of females had low knowledge. There are not enough guidelines or antimicrobial awareness initiatives to encourage the best possible usage of antimicrobials. Multifactorial and integrated awareness building for animal healthcare professionals and producers is required in order to reduce the contribution of animal production to the global health concern posed by antimicrobial resistance (AMR). This approach should be implemented in a variety of nations, each of which has a different level of livestock sector economic development. In conclusion, this study revealed a lack of adequate knowledge however positive attitudes toward antimicrobial use and resistance development. Most professionals focus on drug usage, which exacerbates the occurrence of antimicrobial resistance, but relying on vaccination and herbal medicine can be a good initiative for antimicrobial usage and reduction of AMR. Hence, professionals need to adhere to antimicrobial usage guidelines and apply theoretical concepts in practice through their jobs, and provide training, workshops, appropriate AM use and resistance, and stewardship program for all professionals.
Abbreviations
AMR, Antimicrobial resistance; AMU, Antimicrobial use; CSA, Central Statistics Agency; DA, Disagree; FAO, Food and Agriculture Organization; KAP, Knowledge, attitude practice; SA, Strongly agree; SD, Strongly disagree; SD, Standard deviation; TLU, Tropical domesticated animals units; WHO, World Health Organization.
Data Sharing Statement
The data regarding this study can accessed from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Before startup of the research, Wallaga University School of veterinary Medicine Review committee has seen the proposal of the research and approved by minute reference number VMERC 16/02/01/2022 as the study has no ethical or moral problem on the respondents. Written consent was prepared and shared each and every respondent, and the respondent agreed before giving data.
Acknowledgment
The authors would like to thank Wallaga University for financial support and AHPs of the study areas for their contributions for this study.
Author Contributions
All authors agreed to submit the work to the current journal, agreed to be held accountable for all aspects of the work, and made significant contributions to the conception and design, data acquisition, analysis, and interpretation. They also participated in the article’s drafting or critical revision for important intellectual content.
Disclosure
The authors report no conflicts of interest in this work.
References
1. McEwen SA, Fedorka-Cray PJ. Antimicrobial use and resistance in animals. Clin Infect Dis. 2002;34(Suppl 3):S93–S106. doi:10.1086/340246
2. Economou V, Gousia P. Agriculture and food animals as a source of antimicrobial-resistant bacteria. Infect Drug Resist. 2015;8:49–61. doi:10.2147/IDR.S55778
3. Van Boeckel TP, Pires J, Silvester R, et al. Global trends in antimicrobial resistance in animals in low-and middle-income countries. Science. 2019;365(6459):eaaw1944. doi:10.1126/science.aaw1944
4. Yang H, Paruch L, Chen X, et al. Antibiotic application and resistance in swine production in China: current situation and future perspectives. Front Veter Sci. 2019;6:136. doi:10.3389/fvets.2019.00136
5. World Health Organization (WHO). Antimicrobial resistance global report on surveillance: summary (2020 no. WHO/hse/ped/aip; 2020.
6. Robinson TP, Wertheim HF, Kakkar M, Kariuki S, Bu D, Price LB. Animal production and antimicrobial resistance in the clinic. Lancet. 2016;387(10014):e1–e3. doi:10.1016/S0140-6736(15)00730-8
7. Ekakoro JE, Caldwell M, Strand EB, Okafor CC. Drivers of antimicrobial use practices among Tennessee dairy cattle producers. Vet Med Int. 2018;2018:1836836. doi:10.1155/2018/1836836
8. Muloi D, Ward MJ, Pedersen AB, Fèvre EM, Woolhouse MEJ, van Bunnik BAD. are food animals responsible for transfer of antimicrobial-resistant Escherichia coli or their resistance determinants to human populations? A systematic review. Foodborne Pathog Dis. 2018;15(8):467–474. doi:10.1089/fpd.2017.2411
9. Morar A, Sala C, Imre K. Occurrence and antimicrobial susceptibility of Salmonella isolates recovered from the pig slaughter process in Romania. J Infect Dev Ctries. 2015;9(1):99–104. doi:10.3855/jidc.5236
10. Kumar S, Little P, Britten N. Why do general practitioners prescribe antibiotics for sore throat? Grounded theory interview study. BMJ. 2003;326(7381):
11. AMVA (American Veterinary Medical Association). Judicious therapeutic use of antimicrobials. Available from: https://www.avma.org/KB/Policies/Pages/Judicious-Therapeutic-Use-of-Antimicrobials.aspx.
12. Gebeyehu DT, Bekele D, Mulate B, Gugsa G, Tintagu T. Knowledge, attitude and practice of animal producers towards antimicrobial use and antimicrobial resistance in Oromia zone, north eastern Ethiopia. PLoS One. 2021;16(5):e0251596. doi:10.1371/journal.pone.0251596
13. Landers TF, Cohen B, Wittum TE, Larson EL. A review of antibiotic use in food animals: perspective, policy, and potential. Public Health Rep. 2012;127(1):4–22. doi:10.1177/003335491212700103
14. Cerniglia CE, Pineiro SA, Kotarski SF. An update discussion on the current assessment of the safety of veterinary antimicrobial drug residues in food with regard to their impact on the human intestinal microbiome. Drug Test Anal. 2016;8(5–6):539–548. doi:10.1002/dta.2024
15. Ungemach FR, Müller-Bahrdt D, Abraham G. Guidelines for prudent use of antimicrobials and their implications on antibiotic usage in veterinary medicine. Int J Med Microbiol. 2006;296(Suppl 41):33–38. doi:10.1016/j.ijmm.2006.01.059
16. Schar D, Sommanustweechai A, Laxminarayan R, Tangcharoensathien V. Surveillance of antimicrobial consumption in animal production sectors of low- and middle-income countries: optimizing use and addressing antimicrobial resistance. PLoS. 2018;15(3):e1002521. doi:10.1371/journal.pmed.1002521
17. CSA. Agricultural Sample Survey Volume Ii Report on Livestock and Livestock Characteristics (Private Peasant Holdings). Addis Ababa: Central statistical agency (CSA); 2020.
18. FAO. The future of livestock in Ethiopia: opportunities and Challenges in the face of uncertainty. Available from: http://www.fao.org/3/ca4807en/%20ca4807en.
19. Gemeda BA, Amenu K, Magnusson U. Antimicrobial use in extensive smallholder livestock farming systems in Ethiopia: knowledge, attitudes, and practices of livestock keepers. Front Vet Sci. 2020;7:55. doi:10.3389/fvets.2020.00055
20. World Organization for Animal Health (WOAH). The OIE strategy on antimicrobial resistance and the prudent use of antimicrobials. World Organ Anim Heal; 2016. Available from: https://www.oie.int/fileadmin/Home/eng/Media_Center/docs/pdf/PortailAMR/EN_OIEAMRstrategy.pdf.
21. Arfassa K. Comparative analysis of direct hybrid maize seed marketing and conventional seed distribution system in Eastern Wallaga Zone: The case of Sibu Sire and Gobu SeyoWoredas 2015. [Doctoral dissertation]. Haramaya University; 2015.
22. Arsham H: Descriptive sampling data analysis; 2007. Available from: http://ubmail.ubalt.edu/harsham/Business-stat/opre504.
23. Whitley E, Ball J. Statistics review 4: sample size calculations. Crit Care. 2002;6(4):335–341. doi:10.1186/cc1521
24. World Health Organization. Pharmaceutical policies: medicines use in primary care in developing and transitional countries: fact book summarizing results from studies reported between 1990 and 2006; 2022.
25. Higuita-Gutiérrez LF, Roncancio Villamil GE, Jiménez Quiceno JN. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: a cross-sectional descriptive study. BMC Public Health. 2020;20(1):1861. doi:10.1186/s12889-020-09971-0
26. Sawalha AF. A descriptive study of self-medication practices among Palestinian medical and nonmedical university students. Res Social Adm Pharm. 2008;4(2):164–172. doi:10.1016/j.sapharm.2007.04.004
27. Alnasser AHA, Al-Tawfiq JA, Ahmed HAA, et al. Public knowledge, attitude and practice towards antibiotics use and antimicrobial resistance in Saudi Arabia: a web-based cross-sectional survey. J Public Health Res. 2021;10(4):2276. PMID: 34313091; PMCID: PMC8715265. doi:10.4081/jphr.2021.2276
28. Puvača N, Ljubojević Pelić D, Pelić M, et al. Microbial resistance to antibiotics and biofilm formation of bacterial isolates from different carp species and risk assessment for public health. Antibiotics. 2023;12(1):143. doi:10.3390/antibiotics12010143
29. Wanla W, Katip W, Supakul S, Apiwatnakorn P, Khamsarn S. Effects of an antimicrobial restriction system on appropriate carbapenem use in a hospital without infectious diseases consultation. Int J Gen Med. 2017;10:443–449. doi:10.2147/IJGM.S145133
30. Beyene T, Sultan A, Dinka A, et al. Assessment of rational veterinary drugs use in livestock at adama district veterinary clinic, central Ethiopia. J Vet Sci Technol. 2016;2015:1–7.
31. Etefa M, Beyi AF, Ayana D, Beyene TJ, Tufa TB. Veterinary drug prescribing practices at selected district veterinary clinics of rift valley areas of Ethiopia. Vet Med Int. 2021;2021:6669036. doi:10.1155/2021/6669036
32. Gizaw S, Woldehanna M, Anteneh H, et al. Animal health service delivery in crop-livestock and pastoral systems in Ethiopia. Front Vet Sci. 2021;8:601878. doi:10.3389/fvets.2021.601878
33. Beyene T, Hayishe H, Gizaw F, et al. Prevalence and antimicrobial resistance profile of Staphylococcus in dairy farms, abattoir and humans in Addis Ababa, Ethiopia. BMC Res Notes. 2017;10(1):171. doi:10.1186/s13104-017-2487-y
34. Sarba EJ, Kelbesa KA, Bayu MD, Gebremedhin EZ, Borena BM, Teshale A. Identification and antimicrobial susceptibility profile of Escherichia coli isolated from backyard chicken in and around ambo, central Ethiopia. BMC Vet Res. 2019;15(1):85. doi:10.1186/s12917-019-1830-z
35. Micoli F, Bagnoli F, Rappuoli R, Serruto D. The role of vaccines in combatting antimicrobial resistance. Nat Rev Microbiol. 2021;19(5):287–302. doi:10.1038/s41579-020-00506-3
36. Sobeck J, Smith-Darden J, Gartner D, et al. Antibiotic knowledge, beliefs, and behaviors: testing competing hypotheses using an urban community sample. Health Commun. 2022;37(7):862–871. doi:10.1080/10410236.2021.1875557
37. Filipetto FA, Modi DS, Weiss LB, Ciervo CA. Patient knowledge and perception of upper respiratory infections, antibiotic indications and resistance. Patient Prefer Adherence. 2008;2:35–39.
38. Geta K, Kibret M. Knowledge, attitudes and practices of patients on antibiotic resistance and use in public hospitals of Amhara regional state, northwestern Ethiopia: a cross-sectional study. Infect Drug Resist. 2022;15:193–209. doi:10.2147/IDR.S348765
39. Darwish DA, Abdelmalek S, Abu Dayyih W, Hamadi S. Awareness of antibiotic use and antimicrobial resistance in the Iraqi community in Jordan. J Infect Dev Ctries. 2014;8(5):616–623. doi:10.3855/jidc.4086
40. Pereko DD, Lubbe MS, Essack SY. Public knowledge, attitudes and behaviour towards antibiotic usage in Windhoek, Namibia. S Afr J Infect Dis. 2015;30(4):134–137. doi:10.1080/23120053.2015.1107290
41. Hassan MM, Kalam MA, Alim MA, et al. Knowledge, attitude, and practices on antimicrobial use and antimicrobial resistance among commercial poultry farmers in Bangladesh. Antibiotics. 2021;10(7):784. doi:10.3390/antibiotics10070784
42. Xian Municipal Human resources and social security Bureau (2018). Available from: https://english.beijing.gov.cn/government/departments/202006/t20200627_1932954.html.
43. Chung A, Perera R, Brueggemann AB, et al. Effect of antibiotic prescribing on antibiotic resistance in individual children in primary care: prospective cohort study. BMJ. 2007;335(7617):429. doi:10.1136/bmj.39274.647465.BE
44. Bell BG, Schellevis F, Stobberingh E, Goossens H, Pringle M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. 2014;14(1):13. doi:10.1186/1471-2334-14-13
45. Muhie OA. Antibiotic use and resistance pattern in Ethiopia: systematic review and meta-analysis. Int J Microbiol. 2019;2019:2489063. doi:10.1155/2019/2489063
46. Schwendner AA, Bodmer M, Cousin ME, Schüpbach-Regula G, van den Borne BHP. Knowledge, attitude and practices of Swiss dairy farmers towards intramammary antimicrobial use and antimicrobial resistance: a latent class analysis. Prev Vet Med. 2020;179:105023. doi:10.1016/j.prevetmed.2020.105023
47. Scaioli G, Gualano MR, Gili R, Masucci S, Bert F, Siliquini R. Antibiotic use: a cross-sectional survey assessing the knowledge, attitudes and practices amongst students of a school of medicine in Italy. PLoS One. 2015;10(4):e0122476. doi:10.1371/journal.pone.0122476
48. Tegagn GT, Yadesa TM, Ahmed Y. Knowledge, attitudes and practices of healthcare professionals towards antimicrobial stewardship and their predictors in fitche hospital. Journal of Bioanalysis & Biomedicine. 2017;9(2):91–97. doi:10.4172/1948-593X.1000159
49. Jibril AH, Okeke IN, Dalsgaard A, Olsen JE. Association between antimicrobial usage and resistance in Salmonella from poultry farms in Nigeria. BMC Vet Res. 2021;17(234). doi:10.1186/s12917-021-02938-2
50. Caudell MA, Dorado-Garcia A, Eckford S, et al. Towards a bottom-up understanding of antimicrobial use and resistance on the farm: a knowledge, attitudes, and practices survey across livestock systems in five African countries. PLoS One. 2020;15(1):e0220274. doi:10.1371/journal.pone.0220274
51. Katip W, Oberdorfer P, Kasatpibal N. Effectiveness and nephrotoxicity of loading dose colistin-meropenem versus loading dose colistin-imipenem in the treatment of carbapenem-resistant Acinetobacter baumannii infection. Pharmaceutics. 2022;14(6):1266. doi:10.3390/pharmaceutics14061266
52. Gajic I, Kabic J, Kekic D, et al. Antimicrobial susceptibility testing: a comprehensive review of currently used methods. Antibiotics. 2022;11(4):427. PMID: 35453179; PMCID: PMC9024665. doi:10.3390/antibiotics11040427
53. Gemeda BA, Assefa A, Jaleta MB, Amenu K, Wieland B. Antimicrobial resistance in Ethiopia: a systematic review and meta-analysis of prevalence in foods, food handlers, animals, and the environment. One Health. 2021;13:100286. PMID: 34258373; PMCID: PMC8260865. doi:10.1016/j.onehlt.2021.100286
54. Ferreira JB, Sotomaior CS, Bezerra ACDS, et al. Sensitivity and specificity of the FAMACHA© system in tropical hair sheep. Trop Anim Health Prod. 2019;51(6):1767–1771. doi:10.1007/s11250-019-01861-x
55. Tebug SF, Mouiche MM, Abia WA. Antimicrobial use and practices by animal health professionals in 20 sub-Saharan African countries. Preventive Vet Med. 2020;186. doi:10.1016/j.prevetmed.2020.105212
56. Alhaji NB, Haruna AE, Muhammad B, Lawan MK, Isola TO. Antimicrobials usage assessments in commercial poultry and local birds in North-central Nigeria: associated pathways and factors for resistance emergence and spread. Prev Vet Med. 2018;154:139–147. doi:10.1016/j.prevetmed.2018.04.001
57. Boamah VE, Agyare C, Odoi H, Dalsgaard A. Practices and factors influencing the use of antibiotics in selected poultry farms in Ghana. J Microb Agents. 2016;2. doi:10.4172/Antimicro.1000120
58. Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ. 1998;317(7159):637–642. doi:10.1136/bmj.317.7159.637
59. De Briyne N, Atkinson J, Pokludová L, Borriello SP. Antibiotics used most commonly to treat animals in Europe. Vet Rec. 2014;175(13):325. doi:10.1136/vr.102462
60. Alemnji GA, Zeh C, Yao K, Fonjungo PN. Strengthening national health laboratories in sub-Saharan Africa: a decade of remarkable progress. Trop Med Int Health. 2014;19(4):450–458. doi:10.1111/tmi.12269
61. Mboera LE, Ipuge Y, Kumalija CJ, et al. Midterm review of national health plans: an example from the United Republic of Tanzania. Bull World Health Organ. 2015;93(4):271–278. doi:10.2471/BLT.14.141069
62. Guetiya Wadoum RE, Zambou NF, Anyangwe FF, et al. Abusive use of antibiotics in poultry farming in Cameroon and the public health implications. Br Poult Sci. 2016;57(4):483–493. doi:10.1080/00071668.2016.1180668
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
