Back to Journals » Clinical Interventions in Aging » Volume 19
Association Between Self-Perception of Aging and Long-Term Mortality in Elderly Patients with Hypertension in Rural China: A Possible Beneficial Effect of Nut Intake
Authors Lu A, Yu F, Tan X, Jin X, Wang X, Wu W
Received 18 October 2023
Accepted for publication 13 February 2024
Published 4 March 2024 Volume 2024:19 Pages 357—366
DOI https://doi.org/10.2147/CIA.S445378
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Anping Lu,1,2,* Fangyi Yu,2,* Xiaohan Tan,2 Xiaohong Jin,1 Xiaohua Wang,3 Wenya Wu1
1Nursing Department, The First People’s Hospital of Changshu, Changshu, 215500, People’s Republic of China; 2School of Nursing, Medical College, Soochow University, Suzhou, 215006, People’s Republic of China; 3Division of Cardiology, The First Affiliated Hospital of Soochow University, Suzhou, 215006, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wenya Wu, Nursing Department, The First People’s Hospital of Changshu, Changshu, 215500, People’s Republic of China, Tel +86-1386236425, Fax +86-512-52223921, Email [email protected]
Purpose: Previous research has consistently shown that self-perception of aging (SPA) is an important predictor of health and longevity, while Chinese rural elderly patients with hypertension had poorer SPA. Whether it was associated with their mortality kept unknown. The objective of this study was to investigate the long-term mortality and analyze the association between SPA and this mortality in the specific context of rural elderly patients with hypertension.
Patients and Methods: This study is a longitudinal investigation of the mortality in elderly patients with hypertension in rural Suzhou, China. Sociodemographic and clinical data, SPA, and six-year mortality were investigated. We used binary logistic regression and subgroup analyses to assess the effect of SPA at baseline on six-year mortality.
Results: A total of 280 hypertensive patients aged 60 years and older participated in the study, of whom 21 died, with a six-year mortality rate of 7.5%. After controlling for covariates, the “Emotional representation” dimension (OR=2.824, 95% CI:1.034– 7.712) in SPA remained a risk factor for death. In subgroup analyses of the group aged 75 years and older, high scores on the “Timeline cyclical” (OR=14.125, 95% CI: 1.258– 158.593) and “Emotional representations” (OR=2.567, 95% CI:1.066– 6.182) dimensions were associated with a higher risk of death, while weekly nut intake may have mitigated the negative SPA effect on mortality.
Conclusion: Poorer self-perception of aging was associated with a high risk of mortality in rural elderly patients with hypertension, while the habit of weekly nut intake might help reduce this risk in the group aged 75 years or older.
Keywords: China, hypertension, mortality, rural population, self-perception
Introduction
Self-Perception of Aging (SPA) refers to the subjective perception and emotional responses of elderly people when they are under the threat of physiological, psychological, and social aging, which will affect the behavioral tendencies of the elderly during the aging process and are closely related to health behaviors, health outcomes and happiness in later life.1,2 Previous studies have demonstrated that SPA is an important predictor of health and longevity,3 as well as being linked to individual health promotion and prevention behaviors, including awareness of seeking health care,4 eating behaviors,4 physical activity levels,5 depressive symptoms,6 and even mortality.7 Negative SPA can adversely impact an individual’s physical and psychological well-being,8 with older adults who perceive themselves as useless or have negative attitudes toward aging having a higher risk of death,9 lower rates of recovery from the disease,10 and worse cognitive and psychological functioning.11 In contrast, positive SPA was associated with greater life satisfaction, better functional status, and overall survival.12 Thus, the influence of SPA on expected health outcomes during the aging process should not be ignored.
Chinese elderly patients, especially those living in rural, with chronic diseases have more negative SPA than the normal group.13,14 This negative psychological factor interacts with the etiology of hypertension, causing individual pathological, physiological, and psychological changes, resulting in the deterioration and poor prognosis of hypertension.15 Therefore, the impact of SPA on mortality is worth further exploring in populations suffering from hypertension. However, few studies have explored this association in rural elderly people with hypertension. This study aimed to answer the question of the relationship between SPA and mortality in rural elderly patients with hypertension over a six-year follow-up period.
Materials and Methods
Study Design
This was a longitudinal survey on the mortality of elderly hypertensive patients in rural areas. In the first stage of the survey, we collected the baseline data of participants who met the inclusion-exclusion criteria living in 11 rural village clinics in Suzhou, China, from December 2016 to February 2017. The two trained researchers invited patients with signed informed consent to complete a self-administered questionnaire, which included demographic and clinical data, the Morisky medication adherence scale, and the aging perception questionnaire. Considering that the elderly in rural areas generally have low educational levels, the researchers would read the questionnaire items word by word to the illiterate patients and accurately record their answers. In the second stage of the survey, the researchers conducted a six-year mortality survey in November 2022, a month before the pandemic of Covid-19 in China. This study complied with the Declaration of Helsinki and was approved by the ethics committee of Changshu First People’s Hospital (No.20160929).
Participants
The baseline information of hypertensive patients was collected by convenient sampling, and a total of 280 eligible participants were enrolled. The inclusion criteria were (1) age ≥60 years; (2) patients who have been diagnosed with hypertension according to the Eighth Joint National Committee (JNC8) guideline or were currently taking antihypertensive medication;16 (3) according to the standard of the Chinese administrative division, patients with an agricultural household registration and long-term living in rural areas;17 (4) being able to communicate normally and voluntarily complete all assessments. Subjects with the following conditions will be excluded: (1) combined mental illness and severe cognitive impairment; (2) complicated with tumors or severe cardiopulmonary dysfunction.
We used PASS 15 software to estimate the sample size. The five-year mortality rate for elderly hypertensive patients was reported to be approximately 17.1% in Zhang’s study.18 Based on a 95% confidence interval estimate with a 10% tolerance error, and taking into account a 10% dropout rate a minimum of 263 rural elderly hypertensive patients should be included in this study.
Measures
Mortality
In this study, mortality data were retrieved from the Changshu Regional Health Information Platform. If participants had died, researchers visited/telephoned their family members to confirm their death information. The mortality rate = (the number of deaths/the number of surveyed in total at baseline) ×100%. In previous studies, mortality assessment based on information system retrieval and follow-up has high reliability.7
Self-Perception of Aging (SPA)
The Chinese version of the aging perception questionnaire (APQ) was used to measure the degree of self-perception of aging in the rural hypertensive population. This scale was compiled by Professor Barker in 2007,19 and translated into Chinese by Hu et al in 2012. The Cronbach’s α coefficient of the whole scale was 0.884, which was suitable for the elderly population in China.2 In the first stage of this study, the Cronbach’s α coefficient of 0.776 for the whole scale was indicated. The 32 items contained 7 dimensions examining aging views. (1) “Timeline acute/chronic” measures whether the elderly tend to perceive their aging process quickly or slowly; (2) “Timeline cyclical” reflects the extent to which one experiences variation in the awareness of aging; (3) “Emotional representations” represents the negative emotional reactions produced by aging; (4 and 5) “Control” refers to older adults’ beliefs about managing their own experience of aging and are divided into “Control positive” and “Control negative”; (6) “Consequences positive” measures the positive outcomes and subjective well-being caused by aging, while (7) “Consequences negative” represent the negative consequences and depression caused by aging. All items were scored on a five-point Likert scale, from “completely disagree” to “completely agree” on a scale of 1–5, and the dimension of “control negativity” was scored in the reverse direction. A higher score for each dimension indicates a greater endorsement of a specific perception.
Demographic and Clinical Data
Socio-demographic characteristics included age, sex, marital status, education, living condition, medical insurance (yes/no), smoking (yes/no), exercise (yes/no), high-salt diet (yes/no), daily eating fruits and vegetables (yes/no), weekly nut intake (yes/no), and sleep disturbances (yes/no). Sleep disturbances came from patients’ self-reported “yes” or “no”; The high-salt diet came from daily salt intake recalled by the patients, including the salt content of various condiments, and salt intake of ≥5 grams per person per day was considered to be a high-salt diet.20 Nut intake was based on the recommended standards of the Dietary Guidelines for Chinese Residents (2016),21 participants were classified as eating nuts weekly when they reported nut intake ≥50 grams per week. Clinical data included body mass index (BMI), blood pressure (BP), BP control, duration of hypertension, family history (yes/no), other chronic diseases (yes/no), hospitalization within the past six months (yes/no), frequency of BP measurements (weekly/monthly/irregular), and medication adherence. BMI was equal to body weight (kg)/height (m2), participants were asked to wear light clothing, remove shoes and socks, and measure their height and weight using a corrected rangefinder and weight scale. BP measurements required subjects to rest for at least 5 minutes and were averaged over two consecutive measurements in a sitting position. BP was considered uncontrolled if the participants’ systolic blood pressure was >140 mmHg or diastolic blood pressure was >90 mmHg.16 Medication adherence in this study refers to the adherence to taking antihypertensive medication and is measured using the eight-item Morisky Medication Adherence Scale (MMAS-8), which has a full score of eight, with a score of lower than six indicating poor adherence.22
Statistical Analysis
Statistical analyses were performed using SPSS 26.0 software (SPSS, Inc., Chicago, IL, USA). In sociodemographic characteristics and clinical data, continuous variables conforming to normal distribution were expressed as mean ± standard deviation (SD), otherwise as quartiles M (P25, P75), and categorical variables were represented by frequencies (percentages). Independent samples T-tests, Wilcoxon Mann–Whitney tests, Chi-square tests, and Correction for continuity chi-square test were used to explore the relationships between these variables and mortality rates. To further analyze the relationships between each dimension of SPA and the six-year mortality rate, univariate and multivariate binary logistic regression and subgroup analysis were used, respectively. In multivariate logistic regression, we adjusted for covariates that were statistically significant for mortality (including age and marital status, weekly nut intake, BMI, and frequency of BP measurement; specific categorical variable assignments are shown in Supplement Table 1). In subgroup analyses, we explored the association of each dimension of SPA with mortality in different age groups and in groups with or without weekly nut intake, respectively. All P-values <0.05 were considered significant during statistical analysis.
Results
Status of the Six-Year Death
Baseline data of the participants were collected from December 2016 to February 2017, and a total of 280 rural patients with essential hypertension were enrolled. In November 2022, we conducted follow-up visits to the above participants and 21 of whom died, with a six-year mortality rate of 7.5%.
Socio-Demographic Characteristics and Clinical Data
Socio-demographic characteristics and clinical data of the patients are shown in Table 1. The average age of the participants was 74.55±7.51, of whom 133 were older than 75 years. Fifty-seven percent of the participants were female, and most participants had a low level of education (60% were illiterate). The participants older than 75 years, unmarried or others, without a habit of daily eating nuts, with smaller BMI, and irregular BP measurements had statistically higher mortality rates.
 |
Table 1 Sociodemographic Characteristics and Clinical Data (n=280) |
Associations Between SPA and Six-Year Mortality Rate
Logistic regression of each dimension of SPA for the six-year mortality rate is presented in Table 2. Among the seven dimensions of SPA, the higher scores in the dimensions of “Timeline acute/chronic” and “Emotional representations” were associated with higher risks of a six-year mortality rate. After adjusting for covariates including age, marital status, habit of weekly nut intake, BMI, and frequency of BP measurement, the influence of “Emotional representations” on mortality rate remained statistically significant.
 |
Table 2 Associations Between Self-Perception of Aging and Six-Year Mortality Rate by Logistic Regression (n=280) |
Subgroup Analysis of Different Age
Based on the above findings that age was an important risk factor, we divided the participants into two groups for subgroup analysis (Table 3). There were 147 patients under 75 years of age, of whom 1 died during the follow-up, which resulted in the poor fitting of the Logistic regression model. The group 75 years and above had 133 individuals, of whom 20 died. Multivariate logistic regression equations were constructed after adjusting for the covariates including marital status, a habit of weekly nut intake, BMI, and frequency of BP measurement. The results showed that the effects of “Timeline cyclical” and “Emotional representations” on the six-year mortality rates were statistically significant.
 |
Table 3 Subgroup Analysis of Associations Between Self-Perception of Aging and Six-Year Mortality Rate in the Different Age |
Subgroup Analysis of Whether Weekly Nut Intake
Based on the above finding, the habit of eating nuts or not was a risk factor for death, we divided the population into two groups for subgroup analysis, and the results are shown in Table 4. One hundred and eighty-seven participants had a habit of eating nuts. After adjusting for covariates (including age, marital status, BMI, and frequency of blood pressure measurement), none of the dimensions including “Emotional representations” of SPA had effects on the mortality rate.
 |
Table 4 Subgroup Analysis of Associations Between Self-Perception of Aging and Six-Year Mortality Rate in the Group with or without Weekly Nut Intake |
Subgroup Analysis of Whether Weekly Nut Intake at Age ≥75 Years
In the group of 75 years and older, we divided the participants into two groups for subgroup analysis based on whether they had a habit of weekly nut intake (Table 5). After adjusting for marital status and BMI, the higher scores in the two dimensions of “Timeline cyclical” and “Emotional representations” were associated with greater risks of a six-year mortality rate in the group who did not have a habit of eating nuts. However, in the nut-eating group, the impact of these two dimensions on the mortality rate was not statistically significant.
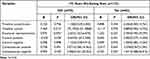 |
Table 5 Subgroup Analysis of the Association Between Self-Perception of Aging and Six-Year Mortality Rate in People Aged ≥75 Years with or without Weekly Nut Intake |
Discussion
In this study, we examined the association between self-perception of aging and mortality in a rural elderly population with hypertension. With the increase of emotional representation dimension scores in SPA, the risk of death increased. At the same time, healthy lifestyle habits and behaviors (including weekly nut intake, BMI management, regular BP monitoring, etc.) were associated with a lower risk of death. In the subgroup analysis of 75 years or older, higher scores of “Timeline cyclical” and “Emotional representation” of SPA were associated with an increased risk of death, while this situation was mitigated by weekly nut intake.
Among socio-demographic characteristics and clinical data, patients who were older, unmarried or others, without a habit of weekly nut intake, with lower BMI, and irregular BP measurements were associated with an increased risk of death. In previous studies, age has been recognized as an important risk factor for mortality.18 With increasing age, hypertensive patients experience mechanical hemodynamic changes, arterial stiffness, neurohormonal and autonomic dysregulation, and declining renal function, which increase the risk of adverse cardiovascular outcomes such as heart failure, stroke, and even death in the elderly.23 In previous studies, good marital status was observed to be a positive health factor, with high mortality rates in each of the non-married categories (including widowed, divorced or separated, and never married) compared to those who were married.24 Weekly consumption of nuts should be considered an essential feature of a health-promoting diet, and the macronutrients, micronutrients, and phytochemicals in nuts have all been shown to contribute to beneficial health outcomes, in particular reducing the risk of cardiovascular disease and associated metabolic alterations,25 which in turn were beneficial for reducing the risk of death from hypertension.
In this study, lower BMI was associated with an increased risk of death. Research has shown that the age-standardized rate of death from any cause was generally lowest in people with a BMI of 22.5 to 24.9, and the hazard ratio above or below this standard was increased.26 In the case of not exceeding the normal criteria, a higher BMI may mean that rural elderly patients with hypertension have better nutritional reserves.27 The frequency of BP measurement was a simple but reliable indicator of access to healthcare and was associated with raising awareness of hypertension, facilitating drug treatment, and achieving BP control.28 Elderly hypertensive patients without regular BP monitoring were unable to find out the problem of uncontrolled BP in time, which can lead to poor disease prognosis.
Previous studies have shown that SPA was an important indicator of physical and mental health as well as the probability of death29 and that there was a positive relationship between negative SPA and mortality in older adults.7 In the present study, we also found a statistically significant difference between the emotional representation dimension of SPA and mortality, and the relationship remained significant after adjusting for covariates. Emotional representation refers to the emotional responses generated by aging, which are characterized by negative emotions such as worry, anxiety, depression, and sadness (eg, “I get depressed when I think about getting older”).19 Negative emotional responses to aging have been associated with negative changes in physical and functional health, as well as with inappropriate coping.7,19 Moreover, in the subgroup analysis of the age group ≥75 years, in addition to the Emotional representation dimension, the Timeline cyclical dimension was a risk factor for death. Timeline cyclical reflects the extent to which one experiences variation in awareness of aging (eg, “I go through phases of feeling old”).19 In Barker et al‘s study, this dimension was associated with more negative emotional responses to aging and more negative aging consequences.19 In stereotypical embodiment theory, negative age stereotypes held by older individuals can have detrimental effects on a variety of cognitive and physical outcomes,30 which was similar to the findings of Klusmann et al that negative SPA leads to lower levels of preventive behaviors, health, and longevity, and this effect was stronger in older and less educated participants.4 It is worth noting that older hypertensive patients in rural areas also face the persistent impact of the disease and poorer health-related quality of life based on higher age and lower education,14 which may cause them to have more negative SPA and thus face cumulative risk of impaired health behaviors and reduced longevity.4 Therefore, it is important to seek interventions for those vulnerable groups to enhance self-efficacy and promote overall health from the SPA perspective.
Nuts (tree nuts and peanuts) are nutritious foods. Over the past few years, many scholars have explored the relationship between nut consumption and health outcomes, with a meta-analysis finding that 28 grams/day increase in nut intake was associated with a reduced risk of all-cause mortality (RR=0.78, 95% CI:0.72–0.84) and cardiovascular disease (RR=0.79, 95% CI:0.70–0.88),31 and Chen et al reported similar results, high nut consumption was significantly associated with lower risk of all-cause mortality (19%, 95% CI: 16–22%) and lower risk of cause-specific mortality (13% to 27%).32 In this study, we first conducted a subgroup analysis of the nut-eating habits of participants of all ages, which showed that SPA did not affect the risk of death regardless of whether the participants ate nuts or not. To explore the reasons, we found that 17 people who died in the group without eating nuts were all older than 75 years old. Therefore, it was more targeted for us to carry out subgroup analyses in the ≥75 years age group.
In the age group 75 years or older, we found that the timeline cyclical dimension and the emotional representation dimension were still risk factors for death in the non-nut-eating group, while the relationship between the two dimensions and death was no longer statistically significant in the nut-eating group. Hu et al reported that Chinese elderly people tend to perceive the aging process as recurrent and unpredictable in terms of periodicity and experience more negative emotional effects brought by aging in terms of emotional representation.2 This may imply that nut consumption may mitigate the effect on mortality rate by reducing the strong perception of recurrent aging and negative emotions in rural hypertensive patients. However, few existing studies have paid attention to the moderating role of nut consumption in the relationship between SPA and mortality. Several studies have demonstrated that nuts are rich in monounsaturated and polyunsaturated fatty acids (PUFA), high-quality protein, fiber, and antioxidant phenolics,25 while oxidative stress and inflammation in the brain are currently believed to contribute to age-related neurodegeneration.33 Nuts are rich in PUFAs and polyphenols, which have good neuronal protective and antioxidant effects, and increasing their consumption is beneficial for improving cognition and overall brain health.25 In a large cross-sectional study of Chinese adults conducted by Su et al, nut consumption was reported to be independently associated with depressive symptoms, and nut consumption may help prevent negative mood symptoms.34 Therefore, we can indirectly infer that nut consumption has beneficial effects on cognition and mood, thereby mitigating the impact of negative SPA on mortality.
At the same time, the impact of chronic illness and the decline in the ability to perform activities of daily living were more significant among very old adults,7 and under the influence of traditional Chinese Confucian culture, most Chinese elderly people attach great importance to family life and intergenerational relations,35 especially in relatively backward rural areas. However, with urbanization and the aging of the population, older individuals have started to perceive themselves as a burden to family and society because they were aware of the reduced degree of contribution to the family, and then have a negative SPA.36 Importantly, Zhang et al’s study found that older adults with more negative SPA tended to engage in less healthy lifestyles, which could lead to a further increased risk of mortality, but that healthy lifestyles could equally mediate the relationship between negative SPA and death.7 Consider that SPA could be malleable and could potentially be modified by different interventions.37 Healthcare professionals should not reinforce ageist stereotypes among older patients in medical and nursing services, but should disseminate positive information and knowledge about aging and encourage healthy eating behaviors such as nut consumption, to improve aging anticipation and control in rural elderly hypertensive patients. Future studies could improve the health outcomes of hypertensive patients in rural areas based on SPA education and the promotion of healthy eating behaviors.
Limitations
There were some limitations in this study. First, this study was carried out in a limited rural area in Suzhou, China, which cannot guarantee the generalization of the research results in other countries. Second, participants were obtained by convenience sampling, which may not adequately represent older hypertensive patients in rural areas. Third, our study population was rural elderly people, who had low levels of education, and some participants were illiterate which may limit understanding of the items of SPA, partly resulting in reduced self-report effectiveness. Fourth, nut consumption was self-reported by patients, and we were unable to accurately distinguish the types and amounts of nuts, which may have reduced validity. Fifth, although we adjusted for covariates in sociodemographic in the multivariate models, residual confounders due to uncollected or poorly collected factors may still exist. Finally, in this study, we used only baseline SPA data to explore the relationship between SPA and six-year mortality, while participants’ SPA may change with age. Future studies should use more measurement points to obtain more SPA information for considering dynamic feedback loops between variables.
Conclusion
Negative self-perception of aging was associated with the risk of mortality in rural elderly patients with hypertension, whereas healthy lifestyles could help reduce mortality risk, and maintaining appropriate nut consumption might be beneficial in improving cognition and mood in people aged 75 years and older. However, the results need to be viewed dialectically due to the limitations of the study. Future research should tend to focus on SPA education and health behavior promotion in elderly patients with chronic diseases.
Abbreviations
SPA, self-perception of aging; BMI, body mass index; BP, blood pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure; PUFA, polyunsaturated fatty acids.
Ethics Approval and Informed Consent
This study complied with the Declaration of Helsinki and was approved by the ethics committee of Changshu First People’s Hospital (No.20160929). All participants signed a detailed consent form including consent for publication.
Acknowledgments
We appreciate all patients and professionals who participated in this study. We would also like to thank the First People’s Hospital of Changshu for its research funding support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the scientific research project of the First People’s Hospital of Changshu (Project No. CS202036).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Turner SG, Hooker K, Geldhof GJ, Meeks S. Self-perceptions of aging: factorial structure and invariance by gender. Meeks S, ed. Gerontologist. 2021;61(3):425–429. doi:10.1093/geront/gnaa059
2. Yunqi H. Research on Self-Perception of Aging of the Elderly and Its Influencing Factors. Shanghai: The Second Military Medical University; 2013.
3. Westerhof GJ, Miche M, Brothers AF, et al. The influence of subjective aging on health and longevity: a meta-analysis of longitudinal data. Psychol Aging. 2014;29(4):793–802. doi:10.1037/a0038016
4. Klusmann V, Sproesser G, Wolff JK, Renner B. Positive self-perceptions of aging promote healthy eating behavior across the life span via social-cognitive processes. J Gerontol B Psychol Sci Soc Sci. 2019;74(5):735–744. doi:10.1093/geronb/gbx139
5. Hooker K, Mejía ST, Phibbs S, Tan EJ, Stevens J. Effects of age discrimination on self-perceptions of aging and cancer risk behaviors. Gerontologist. 2019;59(Suppl 1):S28–S37. doi:10.1093/geront/gny183
6. Gum AM, Ayalon L. Self-perceptions of aging mediate the longitudinal relationship of hopelessness and depressive symptoms. Int J Geriatr Psychiatry. 2018;33(4):591–597. doi:10.1002/gps.4826
7. Zhang X, Kamin ST, Liu S, Fung HH, Lang FR. Negative self-perception of aging and mortality in very old Chinese adults: the mediation role of healthy lifestyle. J Gerontol B Psychol Sci Soc Sci. 2020;75(5):1001–1009. doi:10.1093/geronb/gby136
8. Allen JO. Ageism as a risk factor for chronic disease. Gerontologist. 2016;56(4):610–614. doi:10.1093/geront/gnu158
9. Stewart TL, Chipperfield JG, Perry RP, Weiner B. Attributing illness to “old age”: consequences of a self-directed stereotype for health and mortality. Psychol Health. 2012;27(8):881–897. doi:10.1080/08870446.2011.630735
10. Levy BR, Slade MD, May J, Caracciolo EA. Physical recovery after acute myocardial infarction: positive age self-stereotypes as a resource. Int J Aging Hum Dev. 2006;62(4):285–301. doi:10.2190/EJK1-1Q0D-LHGE-7A35
11. Sargent-Cox KA, Anstey KJ, Luszcz MA. The relationship between change in self-perceptions of aging and physical functioning in older adults. Psychol Aging. 2012;27(3):750–760. doi:10.1037/a0027578
12. Bryant C, Bei B, Gilson K, Komiti A, Jackson H, Judd F. The relationship between attitudes to aging and physical and mental health in older adults. Int Psychogeriatr. 2012;24(10):1674–1683. doi:10.1017/S1041610212000774
13. Hou Y, Zhang D, Gu J, et al. The association between self-perceptions of aging and antihypertensive medication adherence in older Chinese adults. Aging Clin Exp Res. 2016;28(6):1113–1120. doi:10.1007/s40520-015-0516-z
14. Hou Y, Wu Q, Zhang D, Jin X, Wu W, Wang X. The differences in self-perceptions of aging, health-related quality of life and their association between urban and rural Chinese older hypertensive patients. Health Qual Life Outcomes. 2020;18(1):154. doi:10.1186/s12955-020-01411-2
15. Hu B, Liu X, Yin S, Fan H, Feng F, Yuan J. Effects of psychological stress on hypertension in middle-aged Chinese: a cross-sectional study. PLoS One. 2015;10(6):e0129163. doi:10.1371/journal.pone.0129163
16. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. doi:10.1001/jama.2013.284427
17. Cheng H, Gu Y, Ma X, Tang H, Liu X. Urban-rural disparities in hypertension prevalence, awareness, treatment, and control among Chinese middle-aged and older adults from 2011 to 2015: a repeated cross-sectional study. BMC Cardiovasc Disord. 2022;22(1):319. doi:10.1186/s12872-022-02769-5
18. Zhang H, Tian W, Sun Y. Development, validation, and visualization of a web-based nomogram to predict 5-year mortality risk in older adults with hypertension. BMC Geriatr. 2022;22(1):392. doi:10.1186/s12877-022-03087-3
19. Barker M, O’Hanlon A, McGee HM, Hickey A, Conroy RM. Cross-sectional validation of the aging perceptions questionnaire: a multidimensional instrument for assessing self-perceptions of aging. BMC Geriatr. 2007;7:9. doi:10.1186/1471-2318-7-9
20. Samadian F, Dalili N, Jamalian A. Lifestyle modifications to prevent and control hypertension. Iranian J Kidney Dis. 2016;10(5):237–263.
21. Wang SS, Lay S, Yu HN, Shen SR. Dietary guidelines for Chinese residents (2016): comments and comparisons. J Zhejiang Univ Sci B. 2016;17(9):649–656. doi:10.1631/jzus.B1600341
22. Krousel-Wood M, Islam T, Muntner P, et al. Association of depression with antihypertensive medication adherence in older adults: cross-sectional and longitudinal findings from CoSMO. Ann Behav Med. 2010;40(3):248–257. doi:10.1007/s12160-010-9217-1
23. Oliveros E, Patel H, Kyung S, et al. Hypertension in older adults: assessment, management, and challenges. Clin Cardiol. 2020;43(2):99–107. doi:10.1002/clc.23303
24. Johnson NJ, Backlund E, Sorlie PD, Loveless CA. Marital status and mortality: the National Longitudinal Mortality Study. Ann Epidemiol. 2000;10(4):224–238. doi:10.1016/S1047-2797(99)00052-6
25. Ros E, Singh A, O’Keefe JH. Nuts: natural pleiotropic nutraceuticals. Nutrients. 2021;13(9):3269. doi:10.3390/nu13093269
26. Berrington de Gonzalez A, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. New Engl J Med. 2010;363(23). doi:10.1056/NEJMoa1000367
27. Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6(12):944–953. doi:10.1016/S2213-8587(18)30288-2
28. Modesti PA, Perruolo E, Parati G. Need for better blood pressure measurement in developing countries to improve prevention of cardiovascular disease. J Epidemiol. 2015;25(2):91–98. doi:10.2188/jea.JE20140146
29. Gu D, Dupre ME, Qiu L. Self-perception of uselessness and mortality among older adults in China. Arch Gerontol Geriatrics. 2017;68:186–194. doi:10.1016/j.archger.2016.10.015
30. Levy B. Stereotype embodiment: a psychosocial approach to aging. Curr Dir Psychol Sci. 2009;18(6):332–336. doi:10.1111/j.1467-8721.2009.01662.x
31. Aune D, Keum N, Giovannucci E, et al. Nut consumption and risk of cardiovascular disease, total cancer, all-cause and cause-specific mortality: a systematic review and dose-response meta-analysis of prospective studies. BMC Med. 2016;14(1):207. doi:10.1186/s12916-016-0730-3
32. Chen GC, Zhang R, Martínez-González MA, et al. Nut consumption in relation to all-cause and cause-specific mortality: a meta-analysis 18 prospective studies. Food Funct. 2017;8(11):3893–3905. doi:10.1039/c7fo00915a
33. Mecocci P, Boccardi V, Cecchetti R, et al. A long journey into aging, brain aging, and alzheimer’s disease following the oxidative stress tracks. J Alzheimers Dis. 2018;62(3):1319–1335. doi:10.3233/JAD-170732
34. Su Q, Yu B, He H, et al. Nut consumption is associated with depressive symptoms among Chinese adults. Depress Anxiety. 2016;33(11):1065–1072. doi:10.1002/da.22516
35. Gu D, Feng Q, Sautter JM, Yang F, Ma L, Zhen Z. Concordance and discordance of self-rated and researcher-measured successful aging: subtypes and associated factors. J Gerontol B Psychol Sci Soc Sci. 2017;72(2):214–227. doi:10.1093/geronb/gbw143
36. Gu D, Brown BL, Qiu L. Self-perceived uselessness is associated with lower likelihood of successful aging among older adults in China. BMC Geriatr. 2016;16(1):172. doi:10.1186/s12877-016-0348-5
37. Schroyen S, Letenneur L, Missotten P, Jérusalem G, Adam S. Impact of self-perception of aging on mortality of older patients in oncology. Cancer Med. 2020;9(7):2283–2289. doi:10.1002/cam4.2819
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
