Back to Journals » Vascular Health and Risk Management » Volume 20
Association of Body Mass Index with Outcomes in Patients with Atrial Fibrillation: Analysis from the (JoFib) Registry
Authors Ibdah R , Alghzawi AA , Atoum AK, Alenazi LI , Al Omary AY, Hammoudeh A, Laswi B, Rawashdeh S
Received 15 October 2023
Accepted for publication 27 February 2024
Published 5 March 2024 Volume 2024:20 Pages 89—96
DOI https://doi.org/10.2147/VHRM.S444894
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Harry Struijker-Boudier
Rashid Ibdah,1 Ahmad Abdalmajeed Alghzawi,2,3 Amer K Atoum,1 Lina Ib Alenazi,1 Anwar Y Al Omary,1 Ayman Hammoudeh,4 Bushra Laswi,1 Sukaina Rawashdeh1
1Department of Internal Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 2Department of Public Health, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 3Ministry of Health, Amman, Jordan; 4Department of Cardiology, Istishari Hospital, Amman, Jordan
Correspondence: Rashid Ibdah, Department of Internal Medicine, Jordan University of Science and Technology, P.O.Box 3030, Irbid, 22110, Jordan, Tel +962790124465, Email [email protected]
Background: Atrial fibrillation (AF) accounts for the majority of arrhythmias affecting adults. It is associated with an increased mortality and various complications. Obesity being a major risk factor of cardiovascular and metabolic diseases including AF has always been connected to the overall burden of AF, but its role in the development of AF complications remains unclear. Our study aims to evaluate the impact of obesity on the complications of AF in Jordanian patients to establish a proper prognosis since studies regarding this topic in the Middle East are scant.
Methods: This study analyzed data from the Jordanian AF study (JoFib), which enrolled Jordanians with AF. Clinical characteristics were compared among patients who developed complications and those who did not. A binary logistic regression analysis was conducted to identify factors associated with AF complications development.
Results: 1857 patients were enrolled. There was no significant difference in BMI value between patients who developed complications and those who did not. Male sex, old age, hypertension, diabetes mellitus, and higher risk scores were associated with increased odds of developing complications. The oral anticoagulant use was found to be protective. Smoking had no significant effect on odds of complications.
Conclusion: The study concludes that increased BMI is not significantly associated with a reduced risk of developing AF complications. Further research with longer follow-up and larger sample sizes is needed to confirm these results.
Keywords: atrial fibrillation, clinical outcome, complications, Middle East, obesity, paradox
Introduction
Atrial fibrillation is the most commonly encountered chronic cardiac arrhythmia in clinical practice among adults, it is associated with an increased risk of mortality, cerebrovascular accidents and systemic embolism, amassing an estimated global prevalence of up to 33.5 million patients worldwide1 that is expected to double over the next 40 years,2 A clarification of this profane course is the global aging and increase in elderly age group and survival with chronic diseases3 as well as risk factors including obesity, chronic kidney disease, hyperthyroidism, diabetes mellitus, hypertension, alcohol consumption, smoking and other modifiable lifestyle-related risk factors,4 The arrhythmia itself is not feared as much as its complications namely strokes, those of which their incidence have plummeted due to the utilization of oral anticoagulant agents (OACs) and direct OACs (DOACs) in particular,5 but the lack of access to such drugs has created a disparity of results in various regions of the world.6 There is more global focus on the prevention of such complications rather than treatment, by focusing on eliminating or reducing the risk factors to prevent contingency of Atrial fibrillation, and predominantly obesity.7
Obesity has become a pandemic affecting well over 650 million people around the world and continuously rising in prevalence at a shocking rate, which all may be attributed to the sedentary lifestyle and technological advances that made everything a click away.8 Obesity is described as a body mass index (BMI) greater than 30 kg/m2, it is a prime example of modifiable risk factors associated with cardiovascular and metabolic diseases namely atrial fibrillation which all drive the rates of mortality and morbidity in obese patients,8 obesity exerts its effect through a cascade of pathophysiological mechanisms leading to Increased plasma levels of free-fatty acids and cytokines, intracellular non-adipose tissue lipids (eg, liposomes), and ectopic adipose tissue depots (eg, within the visceral compartment) can contribute to systemic inflammation, insulin resistance, and over activity of the sympathetic nervous system. The metabolic and anatomic effects of excess adiposity can lead to the development of type 2 diabetes, non-alcoholic fatty liver disease, obesity-related dyslipidemias, high blood pressure, and osteoarthritis. The cascade and associated diseases mainly metabolic syndromes (insulin-resistance, dyslipidemia, and hypertension) are the main contributors to obesity-related heart failure and cardiovascular diseases (CVD).9 Obesity induces hemodynamic changes that reshape cardiac structure, fostering conditions favorable for atrial fibrillation (AF). Elevated adiposity correlates with increased total blood volume, primarily boosting cardiac output through heightened stroke volume. Unfortunately, this sustained rise leads to left ventricular enlargement and hypertrophy, causing diastolic dysfunction and, over time, potential systolic impairment. Additionally, increased BMI is linked to left atrial enlargement, resulting in elevated pressures and volumes, and subsequent increased pulmonary capillary pressures. Obesity-related sleep-related breathing disorders exacerbate the risk, with cycles of hypoxia, acidosis, and disrupted sleep altering autonomic tone. This increases the likelihood of abnormal cardiac impulse formation and pulmonary arterial pressures, potentially leading to right ventricular hypertrophy and failure. Left unaddressed, these changes can result in biventricular hypertrophy and impairment, creating an ideal substrate for the genesis and persistence of AF.10 Since obesity plays a role in atherosclerosis and plaque development, it leads to structural and functional changes of the heart, which causes heart failure, the altered myocardial structure increases the risk of atrial fibrillation and sudden cardiac death.11
The interrelation between a higher body mass index (BMI) and the risk of AF along with other anthropometric measures namely waist circumference, weight and height has been the mainstay of various research worldwide,12 however, the connection between BMI and AF-related complications is somewhat unclear with studies suggesting an otherwise inverse relationship,12,13 which led to the development of the obesity paradox phenomenon, which refers to the observation that even though obesity is a major risk factor for cardio and cerebrovascular diseases, obese patients that have developed such conditions have a better chance of survival in acute complications of these conditions mainly stroke and peripheral embolization in comparison to non-obese patients with similar conditions. An obese patient with atrial fibrillation appears to have a better long-term outcome than a non-obese patient with the same condition.14,15 Obesity, a cardiovascular risk factor, paradoxically demonstrates improved survival rates in acute cardiovascular decompensation, including congestive heart failure. Clinically, patients diagnosed with chronic cardiovascular diseases who are overweight or class I obese also exhibit enhanced survival rates and outcomes,16,17 nevertheless there are not sufficient data that can prove such claim, especially in the Middle East.
The lack of Middle Eastern studies regarding obesity and complications of AF mainly stroke and systemic embolization has posed a difficult task in allocating a trend in the aforementioned relation, and the available studies are limited to a small number of enrolled patients and cannot be considered as reliable,5 which further insists on the need for finding an answer to that relation. The Jordan AF (JoFib) study enrolled Middle Eastern patients suffering from valvular AF (VAF) or non-valvular NVAF that are highly adherent to their usage of OAC and specifically DOACS and included major risk factors including hypertension, diabetes mellitus, alcohol use, smoking, and obesity.18 The purpose of this study was to determine whether obesity and body mass index affect prognosis in Middle Eastern patients receiving oral anticoagulants for AF that have been enrolled in the JoFib study.
Materials and Methods
The Jordan AF (JoFib) registry is a prospective, multicenter observational registry that enrolled consecutive AF patients aged >18 years in 19 hospitals and 11 outpatient clinics across Jordan between May 2019 through January 2021. Prior to the start of the data collection, a statistician conducted a power analysis and determined the sample size. Data were collected using a standardized clinical data form at the time of enrollment and were followed up at one, 6 and 12 months after the initial assessment. Diagnosis of AF was confirmed by a 12-lead electrocardiogram (EKG) rhythm strip lasting >30 seconds, >1 episode of AF on an ambulatory EKG monitor, or a past diagnosis by a treating cardiologist. Baseline data included clinical and demographic profiles, laboratory data, EKG, transthoracic echocardiographic features, and the use of antiplatelet and OACs including non-vitamin K anticoagulants and vitamin K antagonists, and other pharmacological medications. Standard definitions were used to classify the types of AF, including paroxysmal, persistent, long-standing, and permanent and to calculate the CHA2DS2-VASc and HAS-BLED scores for each patient.
The patients were stratified into four groups: underweight (BMI ≤ 18), normal weight (BMI ≥18 and <25 kg/m2), overweight (BMI ≥ 25 and <30 kg/m2), and obese (BMI ≥ 30 kg/m2). The Patient’s clinical characteristics, comorbidities, risk scores, and AF complications were recorded. Atrial fibrillation complications included; cerebrovascular accidents (CVA), acute coronary syndrome (ACS), Major bleeding, systemic embolization (SSE) and mortality.
The institutional review board of Jordan University of Science and Technology, Prince Hamza Hospital, and Istishari Hospital approved all relevant study documentation and amendments and the study was registered at ClinicalTrials.gov under reference number NCT03917992. The study complies with the declaration of Helsinki and all patients signed a written informed consent. All treatment decisions were left to the discretion of the treating physician.
Statistical analysis
Summary statistics were utilized to describe the continuous variables, employing means and standard deviations (SD), while categorical variables were described using percentages. To compare the means between the two groups, an Independent t-test was performed, while a chi-square test was employed to compare percentages. In order to identify factors associated with the AF complications, a binary logistic regression analysis was conducted. The variables included in the logistic regression model were selected using a stepwise backward method, the BMI variable was used as a continuous variable not as categories in the regression model in order to increase sensitivity. A significance level of p < 0.05 was considered as statistically significant. The analysis was conducted using the IBM SPSS statistical software application (version 28).
Results
The BMI data were available for 1857 out of 2020 enrolled patients (91.9%). Basal demographics are presented in Table 1. The patients were distributed according to the BMI category, underweight (BMI ≤ 18, N = 13), normal weight (BMI ≥18 and <25 kg/m2, N = 423), overweight (BMI ≥25 and <30 kg/m2, N = 655), and obese (BMI ≥ 30 kg/m2, N = 766). BMI categories are shown in Table 1. There was no significant difference in BMI value between patients who developed complications and those who did not.
 |
Table 1 Basal Demographic Characteristics |
In terms of sex, there was no significant difference in the percentage of males and females between the two groups. However, patients who developed complications were significantly older than those who did not. Patients using antiplatelet had a higher percentage of developing complication, but this difference is not statistically significant. There was no significant difference between patients who developed complication and those who did not in regard to OAC use. The percentage of patients who developed complications was significantly higher in those with a prior history of hypertension (HTN), diabetes mellitus (DM), and dyslipidemia. Regarding smoking, the percentage of smokers did not differ significantly between the two groups. The INR value did not differ significantly between the two groups; however, CH2DS2VASC and HASBLED scores were significantly higher in patients who developed complications compared to those who did not.
Table 2 illustrates the percentage of patients who developed complications in each BMI category. Patients with the lowest BMI had a higher percentage of mortality, CVA, and bleeding. On the other hand, patients with the highest BMI had more SE, whereas overweight patients had more ACS. Regarding all complications combined, we can note an increase in complication percentage as the BMI decreases. In addition, underweight patients had higher HA2DS2VASC and HASBLED scores.
 |
Table 2 Risk Scores and the Percentage of Patients with Complications in Each BMI Category |
A binary logistic regression analysis was conducted to evaluate the factors associated with complication development; the results are illustrated in Table 3. Male patients were found to have higher odds of developing complications of AF compared to female patients, there is a positive correlation between age and the chance of developing complications, with an increase in age increasing the likelihood of complications. In addition, patients with DM had higher odds of developing complications as well. The use of OAC drugs in AF patients has shown to be a protective factor that lowers the chances of complications and improves the prognosis in patients with AF, CHA2DS2VASC and HASBLED scores were shown to be important in developing AF complications in Jordanian patients as an increase in these scores shows worse prognosis and more risk of complications. However, there is no significant relationship between a high BMI and a reduced chance of complications from AF. Additionally, smoking was not found to significantly increase the odds of developing complications related to AF.
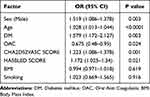 |
Table 3 Binary Logistic Regression Analysis of Factors Associated with AF Complications Development |
Discussion
The present analysis aims to evaluate the hypothesized relation between obesity (BMI) and the development of AF complications as there is a deficient amount of studies regarding this topic. Previous studies suggested that overweight and class I obesity patients who are already diagnosed with AF have better survival chances in the onset of acute AF complications than normal-weight patients. This is known as the obesity paradox.15 Our aim is to investigate whether the obesity paradox applies to AF patients enrolled in the (JoFib) study or not.
According to our findings, increasing BMI and obesity do not appear to decrease the chance of developing AF complications significantly, although the OR is less than 1 which indicates decreasing complication chances as the BMI increases, this relationship is insignificant. In addition, there was no significant difference in the BMI of patients who developed complications from those who did not, and this is conflicting with what other studies show in which increased BMI in AF patients appears to have better long-term outcomes than non-obese patients,14 and that high BMI was independently associated with a lower risk of stroke/SE and better survival.13 Other studies disprove the obesity paradox, as suggested by GARFIELD-AF registry investigators,12 which suggests that both high BMI (BMI ≥ 35.0 kg/m2) and low BMI (BMI < 18.5 kg/m2) are at an increased risk of AF complications mainly (mortality and new/worsening heart failure) and this is inconsistent with the obesity paradox. In addition, Iliodromiti et al reported that there is a direct correlation between high BMI and the risk of CVD. However, the increased risk of CVD reported in underweight subjects (BMI < 18.5 kg/m2) mostly disappeared after statistical adjustment for pre-existing comorbidities,19 and this contradicts the obesity paradox.
The study evaluated other risk factors for AF complications, such as sex. In comparison with females, more male patients developed AF complications, although, the difference was not statistically significant. On the other hand, when applying regression analysis, male patients had higher odds of developing complications of AF than female patients. Several reasons contribute to this, including the fact that men’s hearts and blood vessels are larger, resulting in a greater accumulation of plaque and a greater risk of atherosclerosis, as well as the fact that sex hormones alter the immune response, resulting in different disease phenotypes and complications.20
The average age of patients with complications was higher than that of patients without complications. Furthermore, as the patient’s age increases, the odds of developing complications increase. Aging contributes to multiple chronic diseases, such as diabetes mellitus, hypertension, heart failure, and dyslipidemia. These diseases contribute to the development of AF and its complications. Based on a study done on older patients, it was found that aging AF patients experience a high thromboembolic risk as well as a concomitant high bleeding risk.21
Furthermore, patients with complications had a higher percentage of patients with a history of HTN, DM, and dyslipidemia; all these factors are part of the metabolic syndrome and contribute to atherosclerosis and vascular endothelial injury which drive forward risks of strokes, obesity-related heart failure, and CVDs.9 Patients who have DM have higher odds of developing AF complications. This is supported by the fact that type 2 DM is an independent risk factor for AF development since the undergoing inflammation, oxidative stress and hyperglycemia cause structural, electrical and autonomous remodeling of the heart that accelerates the risk of cardiovascular mortality of stroke, chronic kidney disease (CKD) and heart failure (HF) as well as the risk of death may be 25–66% higher in patients with DM and AF than in non-diabetic.22
The CHA2DS2VASC and HAS-BLED scores have been shown to be important factors in predicting the development of AF complications since increases in these scores indicate a worse prognosis and a higher risk of complications. Since the CHA2DS2VASC score is used as the preferred risk model for anticoagulation decision-making in atrial fibrillation AF patients, recent studies confirmed that high scores were associated with higher mortality and more complications.23 As for the HAS-BLED score, there has been a demonstrated association between high scores and greater bleeding events among AF patients. Therefore, the HAS-BLED score is recommended for assessing anticoagulation‐related major bleeding risk in everyday clinical practice.24
The use of OAC drugs in AF patients has shown to be a protective factor, in which OAC use lowers the odds of developing complications and improves the prognosis. This was previously described by a data from the JoFib study.18 Other studies reported that chronic usage of OAC treatment is the most effective available prophylactic approach in patients with AF at high risk of thromboembolic events.25 In addition, a non-vitamin K oral anticoagulant should be used rather than a vitamin K antagonist in patients with AF undergoing catheterization.26
As for smoking, the percentage of smokers among patients who developed complications was not statistically significant when compared to those who did not. In addition, smoking was not associated with a significant increase in the odds of developing AF complications; our findings can be attributed to the small percentage of non-smoking patients, as the majority of our study samples are smokers. According to the literature, this is contrary to what is known, as smoking is associated with endothelial injury and atherosclerotic plaque development while nicotine in cigarettes contributes to the development of atrial fibrosis and provides an arrhythmogenic substrate increasing the likelihood of atrial arrhythmias namely AF.27 Moreover, smoking cessation after AF diagnosis was associated with reduced CVD, total stroke, and ischemic stroke risk.28 In addition, smoking accounts for 30% of all coronary heart disease (CHD) deaths in the United States yearly and doubles the risk of ischemic strokes with investigations demonstrating benefits of smoking cessation can reach up to 50% reduction in risk of reinfarction, sudden cardiac death, and total mortality in CHD patients if they quit smoking after the initial infarction.29
Limitations
Several limitations affected our results, In general, in non-interventional, observational studies, residual confounding, and data collection are inherent sources of bias. In order to overcome this effect, consecutive patients were recruited from different sectors of the local healthcare system. Short follow-up period for the JoFib patients as they were only followed up for 1 year, a longer follow-up period could have altered the findings, as a longer follow-up period could have provided more variable data and the findings could have been in line with the obesity paradox. The results were affected by the relatively small sample size, which was limited to around 2000 patients. There was a loss of follow-up in 5.7% of patients, which is lower than other investigators have reported.30 Certain analyses may be hampered as a result, as well as the generalizability of the results. However, further investigations and researches are needed to be carried out in the future to prove this hypothesis, with longer duration of patient follow-up and a larger sample size.
Conclusion
The findings suggest that increased BMI was not significantly associated with the decreased likelihood of developing AF complications, thereby disproving the theory of the obesity paradox. However, several other factors were identified as significant predictors.
Data Sharing Statement
In accordance with the data-sharing guidelines outlined by Dove Medical Press, we express our dedication to disseminating individual, de-identified participant data originating from our registry. The specific dataset earmarked for sharing encapsulates the information employed throughout this study. Access to the data will be facilitated exclusively through the corresponding author, reachable at [email protected]. Initiating on February 1, 2024, we anticipate that the data will be accessible for a period of six months.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sagris M, Vardas EP, Theofilis P, et al. Atrial fibrillation: pathogenesis, predisposing factors, and genetics. Int J Mol Sci. 2022;23(1):6. doi:10.3390/ijms23010006
2. Wijesurendra RS, Casadei B. Mechanisms of atrial fibrillation. Heart. 2019;105(24):1860–1867. doi:10.1136/heartjnl-2018-314267
3. Kornej J, Börschel CS, Benjamin EJ, et al. Epidemiology of atrial fibrillation in the 21st century: novel methods and new insights. Circ Res. 2020;127(1):4–20. doi:10.1161/CIRCRESAHA.120.316340
4. Centers for Disease Control and Prevention. Atrial Fibrillation|cdc.gov. CDC; 2022. [Epub ahead of print].
5. Hammoudeh A, Khader Y, Tabbalat R, et al. One-year clinical outcome in middle eastern patients with atrial fibrillation: the Jordan atrial fibrillation (JoFib) study. Int J Vasc Med. 2022;2022. doi:10.1155/2022/4240999
6. Bose A, O’Neal WT, Wu C, et al. Sex differences in risk factors for incident atrial fibrillation (from the Reasons for Geographic and Racial Differences in Stroke [REGARDS] Study). Am J Cardiol. 2019;123(9):1453–1457. doi:10.1016/j.amjcard.2019.01.056
7. O’Keefe EL, Sturgess JE, O’Keefe JH, et al. Prevention and treatment of atrial fibrillation via risk factor modification. Am J Cardiol. 2021;160:46–52. doi:10.1016/j.amjcard.2021.08.042
8. Javed S, Gupta D, Lip GYH. Obesity and atrial fibrillation: making inroads through fat. Eur Heart J Cardiovasc Pharmacother. 2021;7(1):59–67. doi:10.1093/ehjcvp/pvaa013
9. Gadde KM, Martin CK, Berthoud HR, et al. Obesity: pathophysiology and Management. J Am Coll Cardiol. 2018;71(1):69–84. doi:10.1016/j.jacc.2017.11.011
10. Vyas V, Lambiase P. Obesity and atrial fibrillation: epidemiology, pathophysiology and novel therapeutic opportunities. Arrhythmia Electrophysiol Rev. 2019;8(1):28–36. doi:10.15420/aer.2018.76.2
11. Csige I, Ujvárosy D, Szabó Z, et al. The Impact of Obesity on the Cardiovascular System. J Diabetes Res. 2018;2018:1–12. doi:10.1155/2018/3407306
12. Camm CF, Virdone S, Goto S, et al. Association of body mass index with outcomes in patients with newly diagnosed atrial fibrillation: GARFIELD-AF. Open Heart. 2022;9:1–13.
13. Boriani G, Ruff CT, Kuder JF, et al. Relationship between body mass index and outcomes in patients with atrial fibrillation treated with edoxaban or warfarin in the ENGAGE AF-TIMI 48 trial. Eur Heart J. 2019;40(19):1541–1549a. doi:10.1093/eurheartj/ehy861
14. Badheka AO, Rathod A, Kizilbash MA, et al. Influence of obesity on outcomes in atrial fibrillation: yet another obesity paradox. Am J Med. 2010;123(7):646–651. doi:10.1016/j.amjmed.2009.11.026
15. Amundson DE, Djurkovic S, Matwiyoff GN. The obesity paradox. Crit Care Clin. 2010;26(4):583–596. doi:10.1016/j.ccc.2010.06.004
16. Kachur S, Lavie CJ, De Schutter A, et al. Obesity and cardiovascular diseases. Minerva Med. 2017;108(3):212–228. doi:10.23736/S0026-4806.17.05022-4
17. Şaylık F, Çınar T, Hayıroğlu Mİ. Effect of the obesity paradox on mortality in patients with acute coronary syndrome: a comprehensive meta-analysis of the Literature. Balkan Med J. 2023;40(2):93–103. doi:10.4274/balkanmedj.galenos.2022.2022-11-56
18. Hammoudeh AJ, Khader Y, Kadri N, et al. Adherence to the 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline on the use of oral anticoagulant agents in middle eastern patients with atrial fibrillation: the Jordan atrial fibrillation (JoFib) study. Int J Vasc Med. 2021;2021. doi:10.1155/2021/5515089
19. Carbone S, Lavie CJ. Disproving the obesity paradox-not. Eur Heart J. 2018;39(40):3672. doi:10.1093/eurheartj/ehy541
20. Fairweather D. Sex differences in inflammation during atherosclerosis. Clin Med Insights Cardiol. 2014;8(Suppl 3):49–59. doi:10.4137/CMC.S17068
21. Zathar Z, Karunatilleke A, Fawzy AM, et al. Atrial fibrillation in older people: concepts and controversies. Front Med. 2019;6:1.
22. Gherasim L, Pp MD. Association of Atrial fibrillation with diabetes mellitus, high risk comorbidities. Mædica. 2022;17(1):143. doi:10.26574/maedica.2022.17.1.143
23. Harb SC, Wang TKM, Nemer D, et al. CHA2DS2-VASc score stratifies mortality risk in patients with and without atrial fibrillation. Open Heart. 2021;8:1.
24. Zhu W, He W, Guo L, et al. The HAS-BLED score for predicting major bleeding risk in anticoagulated patients with atrial fibrillation: a systematic review and meta-analysis. Clin Cardiol. 2015;38(9):555–561. doi:10.1002/clc.22435
25. Crystal E, Connolly SJ. Role of oral anticoagulation in management of atrial fibrillation. Heart. 2004;90(7):813–817. doi:10.1136/hrt.2003.021642
26. Uziębło-życzkowska B, Krzesiński P, Maciorowska M, et al. Antithrombotic therapy in patients with atrial fibrillation undergoing percutaneous coronary intervention, including compliance with current guidelines—data from the Polish Atrial Fibrillation (POL-AF) Registry. Cardiovasc Diagn Ther. 2021;11(1):14–27. doi:10.21037/cdt-20-839
27. Goette A, Lendeckel U, Kuchenbecker A, et al. Cigarette smoking induces atrial fibrosis in humans via nicotine. Heart. 2007;93(9):1056–1063. doi:10.1136/hrt.2005.087171
28. Choi S, Chang J, Kim K, et al. Association of smoking cessation after atrial fibrillation diagnosis on the risk of cardiovascular disease: a cohort study of South Korean men. BMC Public Health. 2020;20(1):20. doi:10.1186/s12889-019-8142-x
29. Ockene IS, Miller NH. Cigarette smoking, cardiovascular disease, and stroke: a statement for healthcare professionals from the American Heart Association. Circulation. 1997;96(9):3243–3247. doi:10.1161/01.CIR.96.9.3243
30. Boriani G, Proietti M, Laroche C, et al. Association between antithrombotic treatment and outcomes at 1-year follow-up in patients with atrial fibrillation: the EORP-AF general long-term registry. Europace. 2019;21(7):1013–1022. doi:10.1093/europace/euz032
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
