Back to Journals » Clinical Interventions in Aging » Volume 19
Associations Between Patterns of Daily Stepping Behavior, Health-Related Quality of Life, and Pain Symptoms Among Older Adults with Chronic Pain: A Secondary Analysis of Two Randomized Controlled Trials
Authors Fanning J , Brooks AK, Irby MB, N'Dah KW , Rejeski WJ
Received 5 December 2023
Accepted for publication 9 March 2024
Published 14 March 2024 Volume 2024:19 Pages 459—470
DOI https://doi.org/10.2147/CIA.S453336
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Jason Fanning,1 Amber Keller Brooks,2 Megan Bennett Irby,1 Kindia Williams N’Dah,1 W Jack Rejeski1
1Department of Health and Exercise Science, Wake Forest University, Winston-Salem, NC, USA; 2Department of Anesthesiology, Wake Forest University School of Medicine, Winston-Salem, NC, USA
Correspondence: Jason Fanning, Department of Health and Exercise Science, Wake Forest University, 1834 Wake Forest Road, Winston-Salem, NC, 27109, USA, Email [email protected]
Purpose: One’s amount, intensity, and distribution of physical activity may have implications for whether it has positive or negative effects on pain and quality of life for older adults living with chronic pain. Thus, we investigated baseline patterns of stepping related to pain symptoms and health-related quality of life at baseline and over a 12-week follow-up period.
Patients and Methods: Participants were low-active older adults (69.54± 6.74 years) with obesity and chronic pain who enrolled in one of two randomized controlled trials. Participants completed measures of pain intensity, interference, and health-related quality of life and wore an accelerometer for 7 days at baseline and week 12. Functional principal components analysis identified patterns of within-day stepping behavior at baseline, and linear regressions were used to investigate how these component scores related to pain and health-related quality of life at baseline and over 12 weeks.
Results: Two patterns were extracted; one describing more vs less stepping and the second capturing movement later vs earlier in the day. More baseline stepping was associated with better physical functioning (B=0.148, p< 0.001) and energy (B=0.073, p=0.033), while a later start in the day was associated with worse social functioning (B=− 0.193, p=0.031). More stepping at baseline predicted positive changes in physical functioning (B=0.094, p=0.019), emotional role limitations (B=0.132, p=0.049), energy (B=0.112, p< 0.001), social functioning (B=0.086, p=0.043), pain (B=0.086, p=0.009), general health (B=0.081, p=0.003) and pain intensity (B=− 0.039, p=0.003). A later start to the day was associated with worsening physical functioning (B=− 0.229, p< 0.001), physical (B=− 0.282, p=0.047) and emotional role limitations (B=− 0.254, p=0.048), general health (B=− 0.108, p=0.041), and pain interference (B=0.055, p=0.043).
Conclusion: Findings suggest there is value in activity patterns as an indicator for additional behavioral intervention, as those who move little and/or delay daily movement are likely to experience subsequent decrements in quality of life and pain symptoms.
Keywords: pain, patterns, physical activity, accelerometry, quality of life
Introduction
The advent of accelerometry for physical activity (PA) assessment has initiated a cascade of methodological and conceptual advancements that have greatly enhanced our understanding of the relationships between PA and health outcomes across the lifespan. In recent years, the ability for accelerometers to gather objective movement data at high resolution has given rise to an expansion of interest beyond structured exercise both to sedentary behaviors1–5 and to a shift in public health guidelines toward moving more and more often.6,7 Such a recommendation is especially important for individuals living with chronic pain, whose symptoms are negatively affected by too little activity, extended periods of sitting, and overexertion.8–10 This approach to activity promotion was at the core of two recent randomized controlled pilot studies by our group: the Mobile Intervention to Reduce Pain and Improve Health (MORPH)11,12 and MORPH-II.13,14 In both studies, older adults with chronic pain were tasked with achieving daily stepping goals by distributing movement throughout the day. We demonstrated that older adults in this study who increased time spent in light and moderate intensity walking in bouts of at least 5 minutes reported improvements in pain symptoms.15 However, conventional accelerometer processing procedures that focus on discrete summary measures (eg, average steps per day, average daily sedentary breaks) are a poor match for capturing this type of PA prescription. What follows is an application of functional principal component analysis (fPCA) to within-day activity behaviors collected on MORPH and MORPH-II participants. FPCA facilitates analysis on daily patterns of PA, as opposed to summary metrics, and the ways in which these patterns relate to clinical outcomes of interest such as pain and quality of life.16,17
Over the course of approximately three decades, the widespread uptake of accelerometer devices in research and by the public has been the cause and consequence of advances in technology, development of analytic methods, and changing public health messaging related to PA behavior. The primary focus of early research using accelerometry involved capturing overall energy expenditure and volume of PA.18 Subsequently, the focus shifted toward disentangling time spent at various aerobic intensities (most often ≥3 metabolic equivalents [METS]; ie, moderate to vigorous intensity physical activity [MVPA]), calibrated to walking or jogging behaviors.19 Following this work, attention expanded to understanding and contrasting time spent in MVPA and sedentary behaviors, increasing awareness that the effects of MVPA depend upon a host of structural factors such as bout length,4,5 and daily behavioral profiles outside of structured exercise. Unique scientific and methodological challenges have emerged at each stage. For instance, conventional accelerometer data processing methods are simple and typically involve aggregating a measure of total acceleration per minute. Acceleration thresholds are typically derived from devices worn on the hip or wrist during walking or jogging on a treadmill; these thresholds are then used to calculate time spent in sedentary behavior, light-intensity PA (LPA), and MVPA. Important limitations emerging from this approach include an inability to characterize non-ambulatory behaviors and a failure to account for often sizable differences in metabolic output due to age, fitness, resting metabolic rate, and other individual differences that compromise accuracy in characterizing activity as LPA and MVPA. Moreover, wrist worn devices can result in gross overestimation of LPA and MVPA due to low MET activities with a high frequency of arm movement such as basic home chores; to complicate matters further, the frequency of these behaviors varies as a function of age and sex.20,21
As noted above, recent PA guidelines for public health6,7,22 emphasize two activity-based metrics across the day: the amount and patterning or distribution of daily PA, often messaged as “move more, more often”. Yet, until the recent introduction of fPCA to the field of accelerometry, there were no methods permitting examination of patterns of daily movement and how these patterns might affect health outcomes. Like conventional principal components analysis, the aim of fPCA is to reduce the number of functions in a data set to a new, smaller set of orthogonal components that retain as much of the variation present in the original functions as possible.16 Zeitzer et al17 utilized fPCA to examine relationships between patterns of accelerometer-measured PA with sleep, cognition, and mortality in older men. The authors identified four components or patterns: component 1 characterized a high versus low overall activity pattern; component 2 characterized a pattern of earlier vs later risers and bedtimes; component 3 captured biphasic vs monotonic patterns of PA; and component 4 represented a pattern contrasting those with morning vs evening activity peaks. These component scores were then used to predict changes in sleep, cognition, and mortality over a 6.5 to 8-year follow-up period. The researchers found that the low overall activity pattern (component 1) was associated with worse sleep habits, decreases in cognition, and greater all-cause mortality. Those who went to bed earlier and got up earlier (component 2) experienced decline in cognition. Component 4, a bimodal activity pattern, was associated with greater cardiovascular-related mortality and those with a later peak in activity had greater risk for all-cause mortality. These initial data using fPCA underscore the value of these methods for identifying potential patterns inherent in older adults’ daily PA that may have effects on a broad range of health outcomes.
Recognizing the unique behavioral challenge inherent to activity promotion for older adults living with chronic pain, we conducted the MORPH11,12 and MORPH-II13,14 iterative pilot randomized controlled refinement trials. In MORPH, older adults with chronic multisite pain were randomized to a waitlist control or to receive a group-mediated behavioral weight loss and “day-long” PA program. This program was supported by mHealth technology and was designed to promote the achievement of daily stepping goals (an amount goal) by moving often throughout the day (a distribution goal). Participants met in-person once-weekly for 3 weeks and then via videoconference once-weekly for 9 weeks. Relative to control, MORPH participants demonstrated improvements in body weight, pain intensity, and several psychosocial mediators of behavior change. Participants also demonstrated modest improvements in activity behaviors. Key lessons learned included a desire to engage in only one meeting format—and given the onset of COVID-19, a fully remote format was preferable—and the need to better coach moving often in the early stages of the program. MORPH-II deployed a modified protocol based upon these lessons: it was delivered fully remotely, focused on PA behaviors by reducing focus on dietary weight loss, and included a student assistant coaching model wherein frequent calls that focused on feedback review were implemented by pre-health students early in the program. MORPH-II contributed to large magnitude improvements in daily steps and sedentary breaks, and moderate-to-large magnitude improvements in psychosocial mediators of behavior change.14
The present exploratory study leverages data from MORPH and MORPH-II and similar methods to those published my Zeitzer et al17 to investigate the following: (1) at baseline, which components, or patterns, of daily PA explain the greatest variance in daily stepping patterns (the target of the MORPH interventions); (2) how these baseline patterns relate both cross-sectionally and longitudinally over the 12-week interventions to pain symptoms and health-related quality of life (HRQOL), a highly valued outcome for older adults; and (3) whether these baseline patterns account for change in pain and HRQOL above and beyond conventional PA metrics (ie, average daily steps, minutes of MVPA and sedentary time, sedentary breaks). As demonstrated by Zeitzer et al, we expected one key component to capture high versus low stepping levels. Due to lessons learned within these two studies, and in contrast to Zeitzer et al, we expected a second key component to capture early vs delayed daily activity. Next, we expected these patterns to be related to changes in pain and quality of life, with the different patterns of PA each relating to different domains of HRQOL, and that the components would explain greater variance in these outcomes than conventional PA metrics.
Materials and Methods
All study-related procedures were approved by the Wake Forest University Health Sciences (MORPH) and Wake Forest University (MORPH-II) institutional review boards with all individuals providing informed consent prior to participation in accordance with the 1964 Declaration of Helsinki. Both MORPH (NCT03377634) and MORPH-II (NCT04655001) were registered at ClinicalTrials.gov.
Participants
The protocols, primary outcomes, and CONSORT diagrams for MORPH and MORPH-II have been published in detail previously.11–14 As noted above, these 12-week pilot randomized controlled trials focused on iteratively refining a group-mediated behavioral intervention designed to manage pain primarily through achieving movement throughout the day. Each trial also integrated elements of mindfulness-based relapse prevention.23 MORPH had a stronger focus on dietary weight loss combining in-person (3 weeks) and remote (9 weeks) delivery of the intervention. Based on experiences in MORPH, the MORPH-II trial featured increased attention on daylong PA recommendations, was delivered fully remotely via videoconference, and implemented a student coaching model to encourage specific feedback of mHealth app-provided feedback (detailed further below). MORPH recruitment occurred between 2018 and 2019, and MORPH-II recruitment occurred between 2021 and 2022. Participants in both studies were aged 55–85, had a body mass index (BMI) between 30 and 45 kg/m2 (self-reported and corrected using the Shields equation24 in MORPH-II given its remote nature), were self-reported to be low-active and weight stable, and had no contraindications to exercise. Unique eligibility requirements for MORPH included the ability to attend the research center for the in-person sessions, access to a smartphone and willingness to use the device to interact with a study-specific mHealth application, and pain in at least 2 of the following sites on most days in the previous 12 weeks: neck, shoulder, back, hip, or knee. Regarding MORPH-II, participants had to have chronic pain in at least one of the following sites on most days in the previous 12 weeks: back, hip, or knee. Participants in MORPH-II received a technology kit that included a tablet computer and as such were not required to use a personal device to interact with the study app. Additionally, given the remote delivery of the program, they were not required to attend a research center for testing or intervention.
Interventions
Measurement Control
Participants who were randomized to the control condition received a Fitbit Inspire physical activity monitor and a BodyTrace wireless scale to account for any potential short-term effect on behavior associated with provision of these self-monitoring technologies.
The MORPH Intervention
The MORPH behavioral intervention employed a unique combination of features, including a group-mediated design, hybrid (MORPH) or fully remote (MORPH-II) delivery, the extensive use of digital health tools, and a unique approach to activity promotion focusing on increasing daily steps by distributing movement across the day (ie, “daylong movement”). MORPH and MORPH II were conducted as iterative refinement trials to better understand which components were ineffective or underperforming and to implement and refine modifications to address these components. The overarching aim of the MORPH intervention—which has been described in-depth elsewhere11–14 —was to help older adults manage their pain symptoms through a combination of daylong movement; dietary weight management to reduce inflammation and mechanical stress on the body; and mindfulness-based behavioral strategies to assist in managing stress and affect. Central to the design of these interventions is the recognition that health behaviors and pain symptoms are dynamic and must be managed in real time; thus, the interventions were supported by a set of digital health tools comprising a smartphone “Companion App” paired with the BodyTrace wireless weight scale and Fitbit Inspire activity monitor. The Companion App provided participants an opportunity to stay connected via chat with interventionists and fellow group members, engage with real-time visual feedback on progress toward step goals and their distribution of activity across the day, and cues to success by way of “mastery badges” when specific programmatic goals were achieved.
The MORPH group-mediated behavioral intervention was informed by social cognitive25 and self-determination26 theories, along with principles of group dynamics.27,28 Participants met weekly in groups of 4–8 individuals for approximately one hour. The group was leveraged as a behavioral tool, providing opportunities for modeling and demonstration of competence, development of social bonds, formation of activity repertoires, and opportunities to address challenges as they arose. In the first MORPH trial, participants attended 3 in-person meetings to develop initial social bonds and become oriented to the program, and this was followed by 9 videoconference meetings to reduce time and travel burden. Participant feedback indicated that changing from an in-person to remote format was disruptive to the formation of social bonds. As such, the MORPH-II trial was delivered fully remotely, which also assisted in delivery through the COVID-19 pandemic and increased the reach of the program. Another key modification implemented in MORPH-II was the inclusion of brief coaching calls placed by trained pre-health student coaches in a tapered fashion with more frequent calls occurring in the initial weeks of the program. During these calls, the participant and coach reviewed the previous day’s feedback on movement patterns to discuss and troubleshoot periods with extended inactivity as well as periods that were marked by frequent movement. This was designed to help participants better internalize their own patterns of activity and to develop more concrete strategies for addressing causes of extended sitting in participants’ daily lives.
Measures
Demographics
Date of birth, sex, and race were self-reported by participants prior to randomization.
Physical Activity
Participants were asked to wear an ActivPAL 4 triaxial accelerometer (PAL Technologies, Glasgow, Scotland) for 7 consecutive days at baseline and during the final week of the intervention. The ActivPAL is adhered via medical dressing to the upper midline of the thigh on a participant’s non-dominant leg and provides excellent classification of stepping and sedentary behaviors.29,30 Data were processed using PALBatch version 8.11.63 following a 24-hour wear protocol such that at least 20 hours of wear time were required for a valid day. Data were classified via the CREA algorithm version 1.3. To be included in analyses, individuals needed to complete at least one valid day of data to fit a function across a full 1440 minutes. Note that currently there are no data available to guide a minimum number of days required to examine patterns of activity using functional data analyses, though a minimum of 3 valid days are recommended for analyses using conventional accelerometer metrics (eg, minutes of activity or sedentary behavior).31 Therefore, we conducted additional sensitivity analyses removing an individual without at least 3 valid days of accelerometer data. Given the focus of the activity intervention on stepping across the day, the focal outcome utilized in analyses was steps. Steps were extracted at the minute level. Following procedures published by Zeitzer et al32 a “typical day” was constructed by averaging steps during each minute across valid days for a total of 1440 observations per person. Next, a 9-basis Fourier function was fit to each participant’s data to produce a unique function for each participant. Functional PCA was conducted on these functions to identify a set of orthogonal functions that retain as much variability in the original functions as possible. Components were retained based upon inspection of a scree plot. Individual component scores were extracted and leveraged in parametric analyses.
Pain Intensity and Interference
Pain intensity refers to the magnitude of an individual’s experience of their pain, and this was assessed using the 3-item PROMIS pain intensity scale, version 2. This scale asks participants to reflect on the previous 7 days and rate the intensity of their pain at its worst, on average, and at present. Response options range from 1 (“no pain”) to 5 (“severe pain”). Pain interference refers to the extent to which one’s pain interferes with their daily life and was measured using the 8-item PROMIS pain interference scale. This scale tasks participants with reflecting on the previous 7 days, rating the extent to which pain interfered with daily activities. Response options range from 1 (“not at all”) to 5 (“very much”). The PROMIS web-based scoring system was used to score each scale, yielding standardized scores such that 50 represents the national average and 10 represents the standard deviation. Higher scores on each scale represent greater intensity or interference.33
Health-Related Quality of Life
The 36-item Short-Form Survey (SF-36) was used to measure HRQOL. The SF-36 measures eight domains of HRQOL including physical functioning, bodily pain, role limitations due to physical health problems, role limitations due to emotional health problems, emotional well-being, social functioning, energy and fatigue, and perceptions of general health. Scores for each subscale are provided on a 0–100 scale whereby higher scores indicate a more favorable health state.34,35
Analyses
Descriptive statistics, including means ± standard deviation (SD) for continuous variables and counts (%) for categorical variables, were first computed for participant characteristics at baseline. Next, individual component scores were extracted following the fPCA procedures described above. To assist in visualizing differences in component scores, we plotted the overall mean component in blue, plus (orange) or minus (green) component scores multiplied by approximately one pooled standard deviation derived from the four component scores.36 To explore relationships between these component scores and both HRQOL and pain symptoms at baseline, a series of multiple linear regression analyses were conducted with a unique model fit for each component score and each outcome of interest (ie, the SF-36 domain scores, pain intensity, or pain interference). These models included an individual component score, key demographics including age, gender (only the option of either man or woman), and race (white vs non-white), and a code for each study (ie, MORPH or MORPH-II). Dichotomous covariates were dummy coded for inclusion in each model. Similar models were fit to investigate how component scores at baseline predicted longitudinal changes in HRQOL and pain symptoms. Here, change in a given variable was entered as the dependent variable, and predictors included the baseline value for the dependent variable of interest, the individual component score at baseline, key demographics, and study assignment. Finally, group assignment (MORPH intervention vs control) was entered into the model to investigate whether the pattern of one’s movement across the day at baseline predicted change in pain and HRQOL independent of one’s group assignment. To investigate how component scores compared to traditional activity metrics for predicting changes in HRQOL and pain over time, a final series of linear regressions were conducted. For each statistically significant model identified in the prior step, all key covariates (ie, demographics, study, and group assignment, the baseline value for the dependent variable) were entered first. Next, the statistically significant component scores, average daily steps, sedentary breaks, minutes of MVPA, and minutes of sedentary time at baseline were subject to forward selection such that the most statistically significant variable with p < 0.05 was selected, and this process was repeated iteratively until no significant predictors remained. As with prior models, these were fit separately for each component. Statistical significance was established at p < 0.05. All fPCA procedures were conducted in Python 3.9 using the scikit-fda package.37 All parametric analyses were conducted in SPSS version 28 (IBM corp., Armonk, NY).
Results
Participant Characteristics
Participant characteristics can be found in Table 1. In total, 68 randomized participants (69.54±6.74 years) had sufficient data at baseline for inclusion in analyses. Overall, 23.53% of participants were male, 82.35% were White, 88.23% had at least a college education, and 54.41% were randomized to receive the behavioral interventions. Both pain intensity and interference scores were approximately 1 SD higher than the general population (59.82 and 59.90 points respectively). On average, participants engaged in 4875 steps per day, which is substantially lower than step-based translations of the US physical activity guidelines,38 and sat for approximately 11.55 hours per day.
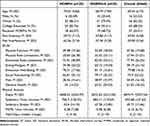 |
Table 1 Participant Characteristics at Baseline |
Functional PCA Results
In line with prior research,17 four components were initially fit to the functional stepping data. Figure 1 depicts these four components. Here, the blue line represents the mean function, orange represents high values for a given component, and green represents low values for a component. Component 1 explained 52.8% of variance, component 2 explained 16.1% of variance; component 3 explained 11.0% of variance, and component 4 explained 6.9% of variance. Based upon inspection of the screen plot, the first two components were retained in further analyses. The first component captures amount of stepping such that those with high scores engage in more movement than those with low scores, exhibiting a similar trend across the day. Component 2 represents early vs late risers. Those with low scores begin moving early and taper activity across the day, whereas high scores capture those who take longer to begin moving, reaching a peak that is lower and later in the day.
Regression Results
Baseline Relationships
Results of cross-sectional models relating component scores to HRQOL and pain symptoms at baseline are reported in Table 2. Component 1 scores were positively associated with physical functioning as assessed via the SF-36 (B=0.148, p<0.001) such that higher scores (ie, those engaging in more stepping) was associated with better functioning. Component 1 scores were also positively associated with energy and fatigue scores at baseline (B=0.073, p=0.033) such that those who moved more reported having more energy. Component 2 scores were negatively associated with social functioning at baseline (B=−0.193, p = 0.031) such that those who tended to take longer to begin their day with a lower overall stepping peak tended to have worse social health compared to those with an earlier and higher peak. One individual had fewer than 3 days of valid data. Removal of this case did not affect interpretation of baseline results.
 |
Table 2 Baseline Relationships Between the First Three Individual Component Scores, Health-Related Quality of Life, and Pain Symptoms |
Baseline Components as Predictors of Change in HRQOL and Pain Symptoms
All results from longitudinal models relating component scores to baseline-adjusted change in HRQOL and pain symptoms over 12 weeks can be found in Table 3. Component 1 scores were positively associated with change in physical function (B=0.094, p = 0.019) and component 2 scores were negatively associated with change in physical function (B=−0.229, p < 0.001). This indicates that those who move more in general demonstrated more favorable changes in physical function over 12 weeks compared with those who moved less. Conversely, those who started their movement later in the day at baseline reported worsening physical function over the 12-week program. Notably, in exploratory variable selection models, components 1 and 2 were selected above any other activity variable. Only component 2 scores were associated with changes in physical role limitations (B=−0.282, p=0.047) such that individuals with a delayed start to their stepping reported worsening role limitations as a result of their physical functioning. Again, this component score was selected over other variables in follow-up analyses. Both component 1 (B=0.132, p=0.049) and component 2 (B=−.254, p = 0.048) were associated with changes in role limitations due to emotional health such that those who engaged in more overall movement or began movement earlier in the day reported more favorable changes. Notably, in variable selection models, overall sedentary time (B=−.102, p = 0.003) was selected over component 1, which was dropped from the model. By contrast, both overall sedentary time (b=−.105 p = 0.002) and component 2 scores (B = −0.269, p = 0.024) were selected as significant predictors of changes in emotional role limitations. In both cases, more time spent sitting at baseline predicted worsening role limitations. Component 1 scores significantly predicted change in energy over the 12-week program (B=0.112, p < 0.001) such that greater stepping at baseline was associated with more positive changes in perceived energy over time. Moreover, this was the only component score to be selected in a follow-up variable selection model. Component 1 scores also exhibited statistically significant, direct associations with both social functioning (B=0.086, p = 0.043) and pain (B=0.086, p = 0.009) such that higher baseline component 1 scores were associated with more favorable changes in both social functioning and pain over 12 weeks. Interestingly, in variable selection models, average daily sedentary time was selected instead of component 1 for both social function (B=−.070, p < 0.001) and pain (B=−.047, p = 0.006) such that more sedentary time at baseline was associated with less favorable changes in scores for each domain. Finally, both component 1 (B=0.081, p = 0.003) and 2 (B-0.108, p = 0.041) scores were associated with changes in general health over 12 weeks. Here again, more movement and movement earlier in the day were each associated with more beneficial changes over time. Component 1 was retained, as were both component 2 (B=−.118, p=0.013) and average daily sedentary time (B=−.029, p=0.032) in follow-up variable selection models. Sensitivity analyses removing the individual with fewer than 3 days of valid wear somewhat attenuated the relationships between component 1 scores and changes in emotional role limitations (p = 0.055) and emotional well-being (p = 0.051), as well as between component 2 scores and changes in physical (p = 0.063) and emotional (p = 0.057) role limitations.
 |
Table 3 Relationships Between the First Three Individual Component Scores at Baseline and 12-Week Change in Health-Related Quality of Life and Pain Symptoms, Adjusted for Baseline Scores |
Regarding pain symptoms, component 1 scores were negatively associated with change in pain intensity scores over 12 weeks (B=−.039, p = 0.003) such that more activity at baseline was associated with a reduction in pain over time. However, a variable selection model identified average daily minutes of MVPA (B=−.422, p < 0.001) as the best variable and did not retain component 1 scores. Component 2 scores were positively associated with changes in pain interference (B=0.055, p = 0.043) such that individuals who began their movement later in the day were more likely to experience worsening pain interference over time. Only this component score was retained in a follow-up variable selection model. Sensitivity analyses removing the individual with fewer than 3 days of wear somewhat attenuated the relationship between component 2 scores and change in pain interference (p = 0.060).
Discussion
In this series of exploratory analyses leveraging data from two randomized controlled pilot studies of behavioral interventions in older adults with chronic multi-site pain, we sought to identify patterns of stepping across the day at baseline, whether these patterns were cross-sectionally and longitudinally associated with HRQOL and pain symptoms, and to explore whether they were uniquely associated with change in HRQOL and pain relative to traditional activity metrics. Using fPCA, we expected to identify components contrasting high vs low amounts of movement as well as early versus delayed start to daily movement. We expected that these components would relate to unique domains of pain and HRQOL and that they would be uniquely related to changes in these outcomes relative to traditional accelerometer metrics used to assess PA. Our findings generally support these hypotheses. First, a pattern capturing the extent to which participants engaged stepping each day explained the greatest proportion of variance in daily stepping patterns. This pattern was followed by a second pattern that differentiated individuals who initiated movement later in the day and reached a lower overall peak from those with an earlier and higher stepping peak. We also identified a third pattern that mirrored a component identified in prior work,17 differentiating biphasic from monotonic patterns of daily movement. However, this pattern was not associated with any of our study outcomes.
In general, our findings support the broader movement toward a “move more, more often” approach to activity promotion,7 which inherently includes a focus on amount of movement and the way in which movement is distributed throughout the day. Healthcare providers may consider beginning with a focus on simply moving more, which was associated with improvements in many aspects of HRQOL and pain intensity. A caveat is that these relationships may act in the reverse direction or even bidirectionally. For instance, changes in HRQOL or pain intensity unrelated to PA may have made it easier for individuals to move more. Nevertheless, given the strength of the data supporting the position that moving more is beneficial for many health outcomes, including well-being,39 we believe a recommendation to engage in more stepping behavior is a generally safe and useful recommendation for those living with chronic pain. One might then build upon this recommendation by adding a focus on moving early and often. Findings from Zhaoyang et al40 suggest that perceptions of pain symptoms when waking may powerfully affect subsequent activity behaviors and, in turn, the experience of pain. These researchers investigated relationships between daily activity behaviors and pain catastrophizing in 143 older adults with knee osteoarthritis. The researchers found that when individuals catastrophized about their pain symptoms in the morning, they were more likely to engage in less PA and more sedentary time on that day, and the effect on sedentary behavior extended to the subsequent day. Moreover, greater sedentary time on a given day was associated with worse pain catastrophizing the next morning. Our findings suggest that those who delay activity and achieve a lower peak in movement are likely to demonstrate worsening physical functioning, role limitations, general perceptions of health, and pain interference. Taken together with Zhaoyang et al's findings, these results suggest there is value in utilizing one’s daily activity patterns in the context of a behavioral activity programming to identify and intervene upon those who may be experiencing pain catastrophizing and subsequent inactivity.
One final finding of interest was that conventional activity metrics such as sedentary time and time spent in MVPA were selected instead of component 1 in variable selection models, and this was not the case for component 2. It is notable that component 1 was strongly correlated with steps (r=0.88), and moderately correlated with sedentary time (r=−.56), sedentary breaks (r=0.43), and MVPA time (r=0.52). By contrast, component 2 was not correlated with any of these variables (each |r| ≤ 0.17). This adds further support to the value of fPCA for studying the relationships between movement and health, as component 2 clearly captures unique information relative to conventional measures of PA.
Strengths and Limitations
There are several notable strengths to the analyses presented herein, including the use of a research-grade accelerometer that accurately classifies stepping behavior, a longitudinal design, and first-of-its kind application of fPCA to activity data in older adults with chronic pain. There are also several important limitations. First, given the novelty of these analyses and the pilot nature of the MORPH and MORPH-II trials, we believe that a type-II error would be at least as impactful as a type-I error.41 Therefore we have not corrected for multiple comparisons and emphasize the exploratory nature of these initial analyses. Second, fPCA is most often applied cross-sectionally and as a result, we were unable to investigate change in activity profiles over time. Similarly, an “average day” was created by averaging each minute across valid days of wear, preventing investigation of variation in movement patterns from day to day. Third, participants in the MORPH trials had chronic pain in varied sites, arising from varied sources, and most participants had back pain. As such, we cannot determine whether the observed activity patterns are associated with a specific cause of pain or pain site. Finally, the sample was relatively small and well-educated. The implications of the sample size are evident in sensitivity analyses that demonstrated mild attenuation of significant effects with removal of a subject with fewer than 3 days of valid wear. This underscores the importance of viewing the results presented herein as an initial exploration of the relationships between patterns of activity, pain, and HRQOL. Future replications of this early-stage work should investigate methods for monitoring patterns of activity longitudinally in larger and more educationally diverse samples.
Conclusion
Chronic pain is a common condition in aging that powerfully affects quality of life. PA is widely recognized as one option for managing chronic pain symptoms, but little is known about how one’s activity patterns relate to pain symptoms and quality of life. This study is the first to apply fPCA to the investigation of activity patterns in older adults with chronic pain. Amount of movement and the tendency to delay one’s activity explained the most variance in daily movement patterns, and these patterns uniquely predicted changes in subdomains of HRQOL, pain intensity, and pain interference. These preliminary findings set the stage for future research on interrelationships between activity patterns, HRQOL, and pain symptoms in larger and more diverse samples. In the near term, these findings also suggest there is value in leveraging one’s pattern of daily movement as an indicator for additional behavioral intervention, as those who move little and/or delay daily movement are likely to experience subsequent decrements in HRQOL and pain symptoms.
Data Sharing Statement
Data collected for this study, including individual deidentified participant data and a data dictionary defining each field in the set, will be made available to others with an academic affiliation upon reasonable request from the corresponding author.
Acknowledgments
This work was supported by the National Institute on Aging [R21 AG058249-01], the Wake Forest University Claude D. Pepper Older Americans Independence Center [P30-AG21332], and the Wells Fargo Faculty Scholarship at Wake Forest University. We would like to thank our participants for the time dedicated to this research. Additionally, we would like to thank Charlotte Crotts for her assistance in the conduct of the trials.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–666. doi:10.2337/dc07-2046
2. Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Diabetes Care. 2008;31(2):369–371. doi:10.2337/dc07-1795
3. Dunstan DW, Dogra S, Carter SE, Owen N. Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat Rev Cardiol. 2021;1–12. doi:10.1038/s41569-021-00547-y
4. Dunstan DW, Healy GN, Sugiyama T, Owen N. Too much sitting: the population health science of sedentary behavior. Eur Endocrinol. 2010;6(1):19–23.
5. Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting: a health hazard. Diabetes Res Clin Pract. 2012;97(3):368–376. doi:10.1016/j.diabres.2012.05.020
6. Ross R, Chaput JP, Giangregorio LM, et al. Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020. doi:10.1139/apnm-2020-0467
7. Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028. doi:10.1001/jama.2018.14854
8. Dzakpasu FQS, Carver A, Brakenridge CJ, et al. Musculoskeletal pain and sedentary behaviour in occupational and non-occupational settings: a systematic review with meta-analysis. Int J Behav Nutr Phys Act. 2021;18(1):1–56. doi:10.1186/S12966-021-01191-Y/FIGURES/6
9. Naugle KM, Ohlman T, Naugle KE, Riley ZA, Keith NCR. Physical activity behavior predicts endogenous pain modulation in older adults. Pain. 2017;158(3):383–390. doi:10.1097/J.PAIN.0000000000000769
10. Heneweer H, Vanhees L, Picavet HSJ. Physical activity and low back pain: a U-shaped relation? Pain. 2009;143(1–2):21–25. doi:10.1016/J.PAIN.2008.12.033
11. Fanning J, Brooks AK, Ip E, Nicklas BJ, Rejeski WJ. A Mobile Health Intervention to Reduce Pain and Improve Health (MORPH) in older adults with obesity: protocol for the MORPH trial. JMIR Res Protoc. 2018;7(5):e128. doi:10.2196/resprot.9712
12. Fanning J, Brooks AK, Ip E, et al. A Mobile Health Behavior Intervention to Reduce Pain and Improve Health in Older Adults With Obesity and Chronic Pain: the MORPH pilot trial. Front Digit Health. 2020;2(598456). doi:10.3389/fdgth.2020.598456
13. Fanning J, Brooks AK, Hsieh KL, et al. Building on lessons learned in a Mobile Intervention to Reduce Pain and Improve Health (MORPH): protocol for the MORPH-II trial. JMIR Res Protoc. 2021;10(7):e29013. doi:10.2196/29013
14. Fanning J, Brooks AK, Ford S, Robison JT, Irby MB, Rejeski WJ. A remote group-mediated daylong physical activity intervention for older adults with chronic pain: results of the MORPH-II randomized pilot trial. Front Digit Health. 2022;4:1040867. doi:10.3389/fdgth.2022.1040867
15. Fanning J, Brooks AK, Robison JT, et al. Associations between patterns of physical activity, pain intensity, and interference among older adults with chronic pain: a secondary analysis of two randomized controlled trials. Front Aging. 2023;4:1216942. doi:10.3389/fragi.2023.1216942
16. Ullah S, Finch CF. Applications of functional data analysis: a systematic review. BMC Med Res Methodol. 2013;13:43. doi:10.1186/1471-2288-13-43
17. Zeitzer JM, Blackwell T, Hoffman AR, et al. Daily Patterns of Accelerometer Activity Predict Changes in Sleep, Cognition, and Mortality in Older Men. J Gerontol a Biol Sci Med Sci. 2018;73(5):682–687. doi:10.1093/gerona/glw250
18. Melanson EL
19. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exercise. 1998;30(5):777–781. doi:10.1097/00005768-199805000-00021
20. Fanning J, Miller ME, Chen S-H, Davids C, Kershner K, Rejeski WJ. Is Wrist Accelerometry Suitable for Threshold Scoring? A Comparison of Hip-Worn and Wrist-Worn ActiGraph Data in Low-Active Older Adults With Obesity. J Gerontol a Biol Sci Med Sci. 2022;77(12):2429–2434. doi:10.1093/GERONA/GLAB347
21. Hall KS, Howe CA, Rana SR, Martin CL, Morey MC. METs and accelerometry of walking in older adults: standard versus measured energy cost. Med Sci Sports Exercise. 2013;45(3):574–582. doi:10.1249/MSS.0b013e318276c73c
22. Medicine E. Rx for Health Series. American College of Sports Medicine; 2023. Available from: https://www.exerciseismedicine.org/eim-in-action/health-care/resources/rx-for-health-series/.
23. Bien T. Mindfulness-Based Relapse Prevention for Addictive Behaviors: a Clinician’s Guide. J Psychiatr Ment Health Nurs. 2011;18(7):e19–e20. doi:10.1111/j.1365-2850.2011.01761.x
24. Shields M, Connor Gorber S, Janssen I, Tremblay MS. Bias in self-reported estimates of obesity in Canadian health surveys: an update on correction equations for adults. Health Rep. 2011;22(3):35–45.
25. Bandura A. Self-Efficacy: The Exercise of Control. W. H. Freeman and Company; 1997.
26. Deci EL, Ryan RM. Self-determination theory: a macrotheory of human motivation, development, and health. Can Psycho. 2008;49:182–185.
27. Brawley LR, Rejeski WJ, Lutes L. A group-mediated cognitive-behavioral intervention for increasing adherence to physical activity in older adults. J Appl Biobehav Res. 2000;5(1):47–65. doi:10.1111/j.1751-9861.2000.tb00063
28. Brawley LR, Rejeski WJ, King AC. Promoting physical activity for older adults: the challenges for changing behavior. Am J Preventive Med. 2003;25(3 SUPPL. 2):172–183. doi:10.1016/S0749-3797(03)00182-X
29. Wu Y, Petterson JL, Bray NW, Kimmerly DS, O’Brien MW. Validity of the activPAL monitor to measure stepping activity and activity intensity: a systematic review. Gait Posture. 2022;97:165–173. doi:10.1016/J.GAITPOST.2022.08.002
30. Rosenberg D, Walker R, Greenwood-Hickman MA, et al. Device-assessed physical activity and sedentary behavior in a community-based cohort of older adults. BMC Public Health. 2020;20(1):1–13. doi:10.1186/S12889-020-09330-Z/TABLES/3
31. Hart TL, Swartz AM, Cashin SE, Strath SJ. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int J Behav Nutr Phys Act. 2011;8:62. doi:10.1186/1479-5868-8-62
32. Zeitzer JM, Blackwell T, Hoffman AR, Cummings S, Ancoli-Israel S, Stone K. Daily Patterns of Accelerometer Activity Predict Changes in Sleep, Cognition, and Mortality in Older Men. J Gerontol Ser A. 2017;73(5):682–687. doi:10.1093/gerona/glw250
33. PROMIS. Intro to PROMIS. HealthMeasures; 2023. Available from: https://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis.
34. RAND Corporation. 36-Item Short Form Survey (SF-36) Scoring Instructions; 2023. Available from: https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/scoring.html.
35. Wyrwich KW, Tierney WM, Babu AN, Kroenke K, Wolinsky FD. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Serv Res. 2005;40(2):577–592. doi:10.1111/j.1475-6773.2005.0l374.x
36. Grupo de Aprendizaje Automatico. FPCAPlot. Available from: https://fda.readthedocs.io/en/stable/modules/exploratory/autosummary/skfda.exploratory.visualization.FPCAPlot.html. Accessed April 12, 2023.
37. Madrid GdAA-UAd. scikit-fda; 2023. Available from: https://fda.readthedocs.io/en/latest/index.html.
38. Tudor-Locke C, Craig CL, Aoyagi Y, et al. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act. 2011;8(1):80. doi:10.1186/1479-5868-8-80
39. Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; 2018.
40. Zhaoyang R, Martire LM, Darnall BD. Daily pain catastrophizing predicts less physical activity and more sedentary behavior in older adults with osteoarthritis. Pain. 2020;161(11):2603–2610. doi:10.1097/j.pain.0000000000001959
41. Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. doi:10.1097/00001648-199001000-00010
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

