Back to Journals » Clinical Epidemiology » Volume 14
Autism Spectrum Disorder Diagnoses: A Comparison of Countries with Different Income Levels
Authors Matos MB, Bara TS, Cordeiro ML
Received 3 May 2022
Accepted for publication 2 August 2022
Published 13 August 2022 Volume 2022:14 Pages 959—969
DOI https://doi.org/10.2147/CLEP.S373186
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Henrik Sørensen
Marilia B Matos,1,2 Tiago S Bara,1,2 Mara L Cordeiro1– 3
1Faculdades Pequeno Príncipe, Curitiba, Brazil; 2Instituto de Pesquisa Pelé Pequeno Príncipe, Curitiba, Brazil; 3Department of Psychiatry and Biobehavioral Sciences, University of California Los Angeles, Los Angeles, CA, USA
Correspondence: Mara L Cordeiro, Instituto de Pesquisa Pelé Pequeno Príncipe, Av. Silva Jardim, 1632, Curitiba, 80250-200, Brazil, Tel +5541-3310-1035, Fax +5531-3322-1446, Email [email protected]; [email protected]
Purpose: This study aimed to assess whether high-income countries have a lower mean age at the time of diagnosis of autism spectrum disorder (ASD) than low- and middle-income countries.
Method: We reviewed studies related to ASD diagnoses and the time of first concerns in low-, middle-, and high-income countries, published in PubMed, SciELO, Lilacs, and ScienceDirect. Thirty articles were included: 13 from low- and middle-income countries and 17 from high-income countries.
Results: The average delay between initial concerns and diagnosis was 32.33 months, with initial concerns averaging 23.64 months and diagnosis at 55.97 months. No statistical differences were found between countries with low-, middle-, and high-income.
Conclusions: This review found a considerable delay in ASD diagnosis despite an early presence of recognized signs and symptoms. It highlights the urgent need for standardized tools for early ASD diagnosis.
Keywords: autism spectrum disorders, low-income countries, diagnosis, first signs
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by differences in social interaction, communication, and unusual repetitive behavior that is self-stimulatory.1,2 ASD is associated with substantial social and economic burdens. ASD diagnosis rates have risen rapidly in recent decades, with 1 in 44 children being diagnosed with ASD as of 2018 in the United States (US).3,4
The heightened awareness of ASD is mainly a feature of high-income countries, where epidemiological data are widely available.5–7 Few studies on the prevalence of ASD have been conducted in low- and middle-income countries, with rates varying from 0.09 to 1.2%; however, no significant epidemiological study has been conducted in Africa.8–13
The relative lack of ASD awareness in low- and middle-income countries may be due to insufficient knowledge about the disorder, lack of trained health professionals, poor awareness of diagnostic tools, and low government and private resources.10 The cultures, education systems, and economies of low- and middle-income countries vary greatly, with incomes ranging from low to lower-middle, middle, and upper-middle levels,14 which frequently results in a pronounced disparity in healthcare access across different populations.13
Healthcare research and discourse in developing countries have focused primarily on infectious diseases, with relatively little attention to mental and behavioral health issues. The recognition of ASD may also be constrained due to stigma against mental health problems and behavioral disorders, particularly in children.13
Currently, ASD diagnosis is based exclusively on clinical observations, and ASD treatment involves intensive and individualized early therapeutic interventions.15 The lack of recognition of the early signs of ASD, typically occurring within the first two years of life when intervention is recommended to start, leads to delayed diagnosis and treatment.15 As early diagnosis is associated with a better prognosis,5 studies examining the prevalence and early signs of ASD are essential for the development and evaluation of screening tools. Additionally, there is a need to identify the reasons for delayed diagnosis and develop new strategies for pediatric primary care to promote timely diagnoses and intervention.
The objectives of this study were to conduct a systematic review of published research related to ASD diagnosis delays in low- and middle-income countries and compare the findings with those from high-income countries. We hypothesized that high-income countries have a lower mean age of diagnosis than low- and middle-income countries. To verify this hypothesis, we focused our analysis on the following: age at the time of assessment related to first concerns, early signs, and the time interval from concerns to a final diagnosis. We also explored the reasons for delayed diagnosis and discussed the importance of early ASD screening.
Materials and Methods
Data Sources and Search Strategies
This systematic review was conducted and written according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.16 The study was registered with the International Prospective Register of Systematic Reviews (PROSPERO identifier CRD42020158996) before data extraction and analyses. We searched the PubMed, SciELO, LILACS, and ScienceDirect databases for scientific literature related to ASD delayed diagnosis. We searched using the keyword search strategies as follows. In PubMed, we searched for the following: autism[Title] OR autistic[Title] OR autism spectrum[Title] OR autistic spectrum[Title] OR autism spectrum disorders[Title]OR autistic spectrum disorders[Title] OR Asperger[Title] OR Asperger’s[Title] OR Asperger’s syndrome[Title] OR ASD[Title] OR Pervasive developmental disorders[Title] OR Disintegrative disorder[Title] AND Sign[Title] OR Signs[Title] OR Early signs[Title] OR Symptom[Title] OR Early symptoms[Title] OR Concerns[Title] OR First concerns[Title] OR Concern[Title] OR Diagnostic[Title] OR Diagnosis[Title] OR Diagnoses[Title] OR Age[Title] OR Age of first concerns[Title] OR Age of first symptoms[Title] OR Age of first signs[Title] OR Age of diagnosis[Title] OR Age of diagnoses[Title] OR Recognition[Title] OR Delay[Title] OR Delayed diagnosis[Title] OR Delayed diagnoses[Title] OR Identification[Title]. In SciELO we searched for the following: (ab:(*autism)) OR (ab:(asd)) OR (ab:(autistic)) AND (ab:(age)) OR (ab:(time)). In Lilacs, we searched for the following: Autism AND age. Finally, in ScienceDirect we searched for the following: Autism AND age of diagnosis. There were no date limitations on the searches.
Study Selection
First, two of the authors separately reviewed the titles and abstracts for all the studies during the period January to August 2020. Second, full texts were obtained for final selection. When a consensus could not be reached on the eligibility of any article, the third author was involved in the discussion (Figure 1).
 |
Figure 1 Records identified through a database search. |
Inclusion and Exclusion Criteria
The following inclusion criteria were applied for retrieved studies: published in English, Portuguese, or Spanish; case series, cohort, or survey study design; and studies related to the age of initial concerns and age of ASD diagnosis data reported. This study included published articles and excluded reviews. We aimed to determine the prevalence of ASD or validate an instrument, including individuals diagnosed after screening or represented by only a published abstract.
Data Extraction
Data related to the following items were extracted: first author, year of publication, study location, population/sample size, sex distribution, age at first concern, age at the time of ASD diagnosis, and instruments used for diagnosis. If present, the first ASD signs, the first person to suspect (FPS), and factors related to delayed diagnoses were also extracted. Studies were divided by location and income for further statistical analyses.
Bias and Quality Assessment
Quality assessment of the included studies was conducted independently by two reviewers. Any discrepancies were resolved by consensus with a third reviewer. For the bias assessment, we used the Newcastle scale,17 which is a checklist of three types of bias most often associated with observational studies (selection, comparability, and outcome).
Statistical Analysis
The results were synthesized in a narrative format, and summary tables were used to compare the results across the included studies. Due to the limited number of studies published, combined with the heterogeneity of study populations and outcomes, the data were not pooled or subjected to a meta-analysis. A standardized summary of the evidence table was used to assess the overall strength of the evidence. This summary of evidence table included the number and design of included studies, sample size, a summary of findings by outcome, consistency or precision of results, potential reporting bias, study quality summary, body of evidence limitation, and applicability of the findings.
Articles were divided into groups regarding the country where the study was performed and publication age for further comparison. The year 2014 was used as a cut point since there were changes in the ASD diagnosis criteria published in 2013 with the DSM 5.1
The grouped variables “period of time” (studies before 2014 and after) and “level of development of the countries in the studies” (“low- and middle-income” countries and “high-income” developed countries) were analyzed using the Mann–Whitney test. The null hypothesis of the test was that age values differ in terms of their distribution. All analyses were performed using SPSS for Windows® software version 21.0, with a significance level of 0.05.
Results
Articles Retrieved
The database search yielded 4420 records identified in PubMed, ScienceDirect, Lilacs, and SciELO. Based on a review of the titles and abstracts of these records, 199 articles were considered potentially relevant and were further reviewed. After full-text assessments, 169 articles were excluded because they did not meet the inclusion criteria, and 30 were included. The third reviewer’s intervention was required for the decision regarding 50 articles. (Figure 1).
Quality assessment was performed in all articles without high bias in one or more parameters. At this stage, the third reviewer’s intervention was necessary to evaluate five articles. The summary scores of the selected studies are reported in Table 1.
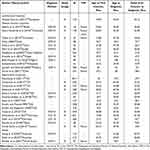 |
Table 1 Summary scores and correspondence level of development of the countries in the included studies |
Figure 2 shows the distribution of means according to the level of development of the different countries. As shown in Figure 2, 13 of the 30 included studies were conducted in upper-, middle-, and lower-income countries.18–29 The other 16 studies were conducted in high-income countries, including six in the US,20,30–34 four in the United Kingdom (UK),35–37 two in Spain,21,22 two in Germany,38,39 two in Australia,23,24 and one in Saudi Arabia.40
 |
Figure 2 Distribution of means according to the level of development of the countries in the studies. Note: Superscript number: Reference number. |
First Person to Suspect
Six studies had information on the FPS that the child’s development was not typical; a family member was reported in most studies.22,23,41–43 One of the studies conducted in Nigeria found that the teacher was the FPS in 51.7% of the cases.26
Time Lag Between Initial Concerns and Diagnosis
For each time variable (i.e, the FPS’s initial concerns [Time 1], diagnosis [Time 2], and the delay between [Time 3]), the data were grouped between “period of time” (studies before 2014 and after) and “level of development of the countries in the studies” (“low- and middle-income” countries and “high-income” developed countries). Thus, it was possible to notice similar values from the boxplots (Figure 3); in general, the median and average age values tended to be higher for studies from 2014 onward, and in the “low- and middle-income” countries. The interquartile range (third quartile minus first quartile) tended to be greater for values obtained in surveys before 2014, but there were more discrepant values for age after 2014.
The Mann–Whitney test indicated that the age distribution (Times 1, 2, and 3) between the “period of time” and “differences by the level of development of the countries in the studies” did not differ at the significance level α = 5%, as shown in Table 2. These results remained stable over time in general, even though some of the studies with retrospective cohorts reflected ASD diagnoses made almost a decade ago.
 |
Table 2 Comparison of p-Values of the Mann–Whitney Test Results |
Delay Between Initial Concerns and Seeking Help
Some studies reported the time interval between the FPS’s initial concerns and parents seeking help. This delay was, on average, 3 months in a Brazilian study,44 32 months in an Indian study,45 and 13.5 months in a study conducted in the Philippines.46
Among high-income countries, there was a 2.4 months delay in a Spanish study,22 8 months in Australia,24 and 6.96 (for ASD) and 12.96 (for Asperger’s syndrome) months in a study from the UK.36 The latter findings were similar to a previous study on the same group that was conducted in the last decade in the UK, where the average delay was 6–7 months.37
Factors Associated with Child’s Age at Initial Concerns and Age of Diagnosis
Clinical Characteristics
Children who were initially diagnosed with Asperger’s syndrome were diagnosed later than children diagnosed with classic autism.21,33,36,39,41,47 In contrast, in the Venezuelan study,48 the ages of concern and diagnosis did not differ significantly between children diagnosed with autism and those diagnosed with pervasive developmental disorder not otherwise specified.
Children with an intellectual disability (ID) tended to have concerns reported earlier than autistic children without ID, along with earlier commencement of services. Impaired cognitive functioning was associated with a younger age at diagnosis.30,32,38,39,48 However, Kishore and Basu42 reported no association between ID and an early diagnosis.
The presence of comorbidities also showed mixed results in the studies. For example, comorbidities were associated with an earlier diagnosis in an Indian study,49 but a later diagnosis in an Australian study.24
Sociodemographic Characteristics
A linear regression analysis indicated that social status did not significantly affect the age of diagnosis in a German study,39 and an American study also reported no differences in sociodemographic factors.33 However, in the Venezuelan study, higher social and economic status and higher parental education levels were associated with earlier diagnosis.48 Whereas, Jayanath and Ozonoff’s18 Malaysian study showed that sociodemographic factors were associated with a later diagnosis. One study found that Hispanic children in the US tended to receive services for ASD later than non-Hispanic White children.32 Another study reported that being Black or multiracial or living in a rural area were risk factors for delayed diagnosis.30
Parental Concerns
Regarding types of parental concerns, concerns regarding verbal communication were strongly represented for children with early parental reports, early commencement of services, and diagnosis. Children with earlier reports of behavioral concerns later had average signs of diagnosis (87.9 months), but later than children whose parents were concerned about a learning disability (69.7 months). Children exhibiting unusual movements and nonverbal communication concerns were diagnosed earlier than those who did not show these signs.32
Diagnostic Trends Over Time
Two of the reviewed studies, one in Germany and one in the US, compared diagnostic data between younger children/more recent diagnoses and older children/less recent diagnoses to examine how ASD diagnosis may have changed over time.32,39 In the German study, the average age of diagnosis for children diagnosed between 2000 and 2007 was not significantly different from that between 1998 and 2002.39 In the US study, younger children with more recent diagnoses (6–11 years) had earlier parental concerns, service initiation, and ASD diagnoses than older children with less recent diagnoses (12–17 years).32
Early Signs and Symptoms
The first signs and symptoms were described in several studies.18,23,28,35–37,42,45,46,50 Speech delay was the most recognized concern between high-income (50.3%) and low/middle-income countries (53.5%), as described in Figure 4.
Discussion
We sought to test the hypothesis that children with ASD in high-income countries would have an earlier diagnosis than children in low- and middle-income countries. Our systematic review showed that the mean age of ASD diagnosis was 55.97 months and the mean age of first concerns was 23.64 months. Although the age of diagnosis in high-income countries was earlier than that in low- and middle-income countries, there was no statistically significant difference between age of diagnosis in high-income (52.60 months) and low/middle-income countries (60.38 months). The mean age of initial concerns in high-income countries was 23.93 months and that in the low/middle-income countries was 23.27 months. There were no differences in the age of initial concerns and diagnoses between articles published before or after 2014.
The great diversity in ASD phenotype presentations, cultural differences, and differences in social status make simple, linear comparisons of the age of initial concerns and diagnosis difficult. Nevertheless, it is important to note that all the analyzed studies showed delays from initial concerns to diagnosis (mean = 37.12 months in “low- and middle-income” countries and mean = 28.67 months in “high-income” developed countries).
Despite efforts to enable earlier recognition of ASD signs, delayed ASD diagnosis remains an issue. Although ASD signs are present within the first two years of life,15 a previous review indicated that the median age of diagnosis ranged from 36 months to 82 months,51 consistent with the present results. A more recent meta-analysis reported that the mean age at ASD diagnosis was 60.48 months, ranging from 30.90 to 234.57 months.52
More disturbingly, when comparing studies over the years, we found no significant improvement in the diagnosis timeline. These results indicate the need for more active clinical approaches despite increased awareness of ASD and the importance of early diagnosis. There were also no differences between the mean age of delay in studies before and after 2014 (p=0.976).
There are two major factors associated with delayed ASD diagnosis: clinical characteristics and socioeconomic factors. Concerning clinical characteristics, children with severe IDs and children who are nonverbal are more easily recognized.53 Regarding socioeconomic factors, it has been suggested that later diagnosis may be related to low income, limited parent education, and being a member of a historically disenfranchised race or ethnic group.30,32,48 In this regard, the Venezuelan study found an effect of socioeconomic status, whereas the German study did not.39,48 An American study showed delayed diagnosis among children of Hispanic ethnicity.32
The finding that FPS were overwhelmingly parents22,23,31,32,42–44,49 suggests that many health professionals who should have been alerted to signs earlier were not properly prepared to do so.
The most frequently reported first concerns were “delayed or absent speech” and “delays in social skills.” In addition, some symptoms that are not only associated with ASD can be indicators for a more accurate evaluation, such as motor delays, general medical conditions, eating problems, excessive crying, delayed toilet training, and sleeping disorders. These signs and symptoms are included in the Modified Checklist for Autism in Toddlers (M-Chat), an easy and free screening tool that can be used in pediatric settings.54 However, this tool should be used with caution as it has low sensitivity, and monitoring for signs of ASD in screen-negative children should be continued.55
Some of the ASD criteria of DSM-51 were not reported as first concerns, such as sensory disorders, inflexible adherence to routines, and highly restricted and fixated interests. Although repetitive/restricted behavior was mentioned, it was not as significant as the other reported concerns. These results highlight the importance of screening tools not only based on the ASD diagnostic criteria but also common first symptoms reported. Screening is a powerful strategy for improving early diagnosis and, consequently, early intervention enrollment. Early intervention is based on the concept of neuroplasticity, that is, the ability of the brain to reorganize in response to experience via changes in neural circuitry.56
In a prospective cohort study, Pierce57 evaluated the stability of ASD diagnosis made between 12 and 36 months old and then compared the results with those of other developmental problems and those of typical development; the overall diagnostic stability of ASD among young children diagnosed with ASD was 0.84, which was higher than that of any of the compared diagnostic groups (eg ASD features without a diagnosis, developmental delays, language delays). Moreover, the results suggested that an ASD diagnosis can be reliable in children as young as 14 months old.58
Although no long-term studies have compared the outcomes of screened versus non-screened children, arguments for screening thus far have been based on the negligible cost of screening relative to the life-long economic costs of ASD.
Furthermore, in low- and middle-income countries, most children identified by screening had not been previously identified as having ASD by parents or physicians.58 At this stage, there is no debate about whether or not to screen for ASD; however, researchers and clinicians should discuss the best approach and how to move from screening to timely diagnosis. In 2016, the US Preventive Service Task Force (USPSTF) concluded that
the current evidence is insufficient to assess the balance of benefits and harms of screening for ASD in young children for whom no concerns of ASD have been raised by their parents or a clinician.
The USPSTF classified this recommendation as grade I, indicating that more research is required in this field.29 The absence of universal ASD screening places the responsibility for early diagnosis on health professionals, teachers, and parents, who in many cases are not well-prepared to recognize the signs of ASD in infants or toddlers. Thus, universal screening programs should expand the opportunity for toddlers to receive early intervention, and thus have a better prognosis. The aforementioned USPSTF statement should not be understood as a contraindication for screening, but rather as a statement of the urgent need for long-term studies of screening outcomes.
The ASD prevalence rates reported in low- and middle-income countries7–9,11,12,48 are likely gross underestimates. A recent review of the global prevalence of ASD showed that 86.5% of cases identified in epidemiological studies were in North America, Europe, and Japan, where only 10% of the world’s children live.59 This discrepancy might be due to the following: difficulties associated with conducting research in developing countries; a lack of ASD awareness among parents, teachers, and health professionals; attribution of behavioral problems to poor parenting skills;59 and limited healthcare access.13
Our study has some notable limitations. First, only 30 studies were eligible for inclusion that were quite varied in design, with their inherent limitations. This limited study inclusion might have occurred, at least in part, because our aim was limited to specifically evaluating the delay of ASD diagnosis. Unfortunately, most of the studies retrieved on the diagnosis did not evaluate the first signs recognized by the parents. However, the limited data available were found to be concordant with the data obtained in other settings. Second, the analysis sample may have been biased as some of the studies were performed at referral centers.20,26,28,32,34,38,41–44,48,49 As referral centers are expected to be better prepared to recognize signs of ASD than non-referral local centers, it is reasonable to conclude that the current situation of ASD delayed diagnosis might be worse than that portrayed in this review. Another limitation is that most of the studies included did not distinguish participants by ASD severity.22,31,41,43,44,48,49 This shortcoming makes it difficult to compare the age of reported concerns and age of diagnosis, given that more severe patients are more easily recognized.
Conclusion
To the best of our knowledge, this is the first systematic review comparing ASD diagnosis and treatment delays in low-, middle-, and high-income countries. Additionally, we have provided an account of the most frequent first concerns of FPS, which is extremely important for early recognition and screening for ASD. On average, there was a 32.33-month delay between initial concerns of the FPS and ASD diagnosis in the reviewed studies. This delay has been stable for many years. In most of the cases, the FPS were parents rather than healthcare professionals. This review highlights the urgent need for standardized tools for early ASD diagnosis, which is challenging because of the high phenotypic variability among people with autism. There is a need for more studies on ASD diagnosis, especially in low- and middle-income countries. Elucidation of the epidemiology and clinical course of ASD is critical for the developing public health programs and medical education strategies for the effective recognition and treatment of ASD effectively.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was also financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nivel Superior -Brazil (CAPES) – Finance Code 001 to MBM and TSB.
Disclosure
The authors declare that they have no competing interests.
References
1. American Psychatric Association. Diagnostic and Statistical Manual of Mental Disorders.
2. Kim YS, Leventhal BL, Koh YJ, et al. Prevalence of autism spectrum disorders in a total population sample. Am J Psychiatry. 2011;168(9):904–912. doi:10.1176/appi.ajp.2011.10101532
3. Graf WD, Miller G, Epstein LG, Rapin I. VIEWS & REVIEWS The autism “epidemic” Ethical, legal, and social issues in a developmental spectrum disorder. Neurology. 2017;88:1371–1380. doi:10.1212/WNL.0000000000003791
4. Maenner MJ, Shaw KA, Baio J, et al. Prevalence of autism spectrum disorder among children aged 8 Years-Autism and developmental disabilities monitoring network, 11 Sites, United States, 2016. MMWR Surveill Summ. 2020;69(4):1–12. doi:10.15585/MMWR.SS6904A1
5. Baron-Cohen S, Scott FJ, Allison C, et al. Prevalence of autism-spectrum conditions: UK school-based population study. Br J Psychiatry. 2009;194(6):500–509. doi:10.1192/bjp.bp.108.059345
6. Hilton CL, Fitzgerald RT, Jackson KM, et al. Brief report: under-representation of african americans in autism genetic research: a rationale for inclusion of subjects representing diverse family structures. J Autism Dev Disord. 2010;40(5):633–639. doi:10.1007/s10803-009-0905-2
7. Paula CS, Ribeiro SH, Fombonne E, Mercadante MT. Brief report: prevalence of pervasive developmental disorder in Brazil: a pilot study. J Autism Dev Disord. 2011;41(12):1738–1742. doi:10.1007/s10803-011-1200-6
8. Bakare M, Munir K. Autism spectrum disorders (ASD) in Africa: a perspective. Afr J Psychiatry. 2011;14(3):208–210. doi:10.4314/ajpsy.v14i3.3
9. Chauhan A, Singh M, Jaiswal N, Agarwal A, Sahu JK, Singh M. Prevalence of cerebral palsy in indian children: a systematic review and meta-analysis. Indian J Pediatr. 2019;86(12):1124–1130. doi:10.1007/s12098-019-03024-0
10. Collins PY, Patel V, Joestl SS, et al. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi:10.1038/475027a
11. Fombonne E, Marcin C, Manero AC, et al. Prevalence of autism spectrum disorders in guanajuato, Mexico: the leon survey. J Autism Dev Disord. 2016;46(5):1669–1685. doi:10.1007/s10803-016-2696-6
12. Lejarraga H, Menendez AM, Menzano E, et al. Screening for developmental problems at primary care level: a field programme in San Isidro, Argentina. Paediatr Perinat Epidemiol. 2008;22(2):180–187. doi:10.1111/j.1365-3016.2007.00897.x
13. Yamin AE, Frisancho A. Human-rights-based approaches to health in Latin America. Lancet. 2015;385(9975):e26–e29. doi:10.1016/S0140-6736(14)61280-0
14. The World Bank. FROM crisis TO green, resilient, and inclusive recovery. J Econ. 2021;4:114.
15. Lappé M, Lau L, Dudovitz RN, Nelson BB, Karp EA, Kuo AA. The diagnostic odyssey of autism spectrum disorder. Pediatrics. 2018;141(Supplement 4):S272–S279. doi:10.1542/peds.2016-4300C
16. Moher D, Shamseer L. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
17. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
18. Jayanath S, Ozonoff S. First parental concerns and age at diagnosis of autism spectrum disorder: a retrospective review from Malaysia. Malaysian J Med Sci. 2020;27(5):78–89. doi:10.21315/mjms2020.27.5.8
19. García R, Irarrázaval M, López I, Riesle S, Cabezas M, Moyano A. Survey for caregivers of people in the autism spectrum in Chile: first concerns, age of diagnosis and clinical characteristics. Andes Pediatr. 2021;92(1):25–33. doi:10.32641/andespediatr.v92i1.2307
20. Zuckerman KE, Lindly OJ, Sinche BK. Parental concerns, provider response, and timeliness of autism spectrum disorder diagnosis. J Pediatr. 2015;166(6):1431–1439.e1. doi:10.1016/j.jpeds.2015.03.007
21. Garrido D, Carballo G, Artis J, Garcia-Retamero R. Timing of parents’ concerns related to autism spectrum disorder and its diagnosis: a mediation analysis. Span J Psychol. 2018;1–8. doi:10.1017/sjp.2018.64
22. Del Fortea Sevilla MS, Escandell BMO, Castro SJJ. Detección temprana del autismo: profesionales implicados. Rev Esp Salud Publica. 2013;87(2):191–199. doi:10.4321/S1135-57272013000200008
23. Young RL, Brewer N, Pattison C. Parental identification of early behavioural abnormalities in children with autistic disorder. Autism. 2003;7(2):125–143. doi:10.1177/1362361303007002002
24. Gibbs V, Aldridge F, Sburlati E, Chandler F, Smith K, Cheng L. Missed opportunities: an investigation of pathways to autism diagnosis in Australia. Res Autism Spectr Disord. 2019;57(October2018):55–62. doi:10.1016/j.rasd.2018.10.007
25. Bachmann CJ, Gerste B, Hoffmann F. Diagnoses of autism spectrum disorders in Germany: time trends in administrative prevalence and diagnostic stability. Autism. 2018;22(3):283–290. doi:10.1177/1362361316673977
26. Bello-Mojeed MA, Omigbodun OO, Bakare MO, Adewuya AO. Pattern of impairments and late diagnosis of autism spectrum disorder among a sub-Saharan African clinical population of children in Nigeria. Glob Ment Heal. 2018;4. doi:10.1017/gmh.2016.30
27. Nasri H, Baradaran A, Shirzad H, Kopaei MR. New concepts in nutraceuticals as alternative for pharmaceuticals. Int J Prev Med. 2014;5(12):1487–1499.
28. Shrestha M, Shrestha R. Symptom recognition to diagnosis of autism in Nepal. J Autism Dev Disord. 2014;44(6):1483–1485. doi:10.1007/s10803-013-2005-6
29. Siu AL, Bibbins-Domingo K, Grossman DC. Screening for autism spectrum disorder in young children US preventive services task force recommendation statement. JAMA. 2016;315(7):691–696. doi:10.1001/jama.2016.0018
30. Rosenberg RE, Landa R, Law JK, Stuart EA, Law PA. Factors affecting age at initial autism spectrum disorder diagnosis in a national survey. Autism Res Treat. 2011;2011:1–11. doi:10.1155/2011/874619
31. Zuckerman K, Lindly OJ, Chavez AE. Timeliness of autism spectrum disorder diagnosis and use of services among U.S. elementary school–aged children. Psychiatr Serv. 2016;68(1):33–40. doi:10.1176/appi.ps.201500549
32. Zablotsky B, Colpe LJ, Pringle BA, Kogan MD, Rice C, Blumberg SJ. Age of parental concern, diagnosis, and service initiation among children with autism spectrum disorder. Am J Intellect Dev Disabil. 2017;122(1):49–61. doi:10.1352/1944-7558-122.1.49
33. Becerra-Culqui TA, Lynch FL, Owen-Smith AA, Spitzer J, Croen LA. Parental first concerns and timing of autism spectrum disorder diagnosis. J Autism Dev Disord. 2018;48(10):3367–3376. doi:10.1007/s10803-018-3598-6
34. Hausman-Kedem M, Kosofsky BE, Ross G, et al. Accuracy of reported community diagnosis of autism spectrum disorder. J Psychopathol Behav Assess. 2018;40(3):367–375. doi:10.1007/s10862-018-9642-1
35. Smith B, Chung MC, Vostanis P. The path to care in autism: is it better now? J Autism Dev Disord. 1994;24(5):551–563. doi:10.1007/BF02172137
36. Howlin P, Asgharian A. The diagnosis of autism and Asperger syndrome: findings from a survey of 770 families. Dev Med Child Neurol. 2007;41(12):S0012162299001656. doi:10.1017/S0012162299001656
37. Howlin P, Moore A. Diagnosis in autism - A survey of over 1200 patients in the UK. Autism. 1997;1(2):135–162. doi:10.1177/1362361397012003
38. Höfer J, Hoffmann F, Kamp-Becker I, et al. Pathways to a diagnosis of autism spectrum disorder in Germany: a survey of parents. Child Adolesc Psychiatry Ment Health. 2019;13(1):1–10. doi:10.1186/s13034-019-0276-1
39. Noterdaeme M, Hutzelmeyer-Nickels A. Early symptoms and recognition of pervasive developmental disorders in Germany. Autism. 2010;14(6):575–588. doi:10.1177/1362361310371951
40. Alotaibi AM, Craig KA, Alshareef TM, et al. Sociodemographic, clinical characteristics, and service utilization of young children diagnosed with autism spectrum disorder at a research center in Saudi Arabia. Saudi Med J. 2021;42(8):878–885. doi:10.15537/smj.2021.42.8.20210297
41. Crane L, Chester JW, Goddard L, Henry LA, Hill E. Experiences of autism diagnosis: a survey of over 1000 parents in the United Kingdom. Autism. 2016;20(2):153–162. doi:10.1177/1362361315573636
42. Kishore MT, Basu A. Early concerns of mothers of children later diagnosed with autism: implications for early identification. Res Autism Spectr Disord. 2011;5(1):157–163. doi:10.1016/j.rasd.2010.03.005
43. Sampedro-Tobón ME, González-González M, Vélez-Vieira S, Lemos-Hoyos M. Detección temprana en trastornos del espectro autista: una decisión responsable para un mejor pronóstico. Bol Med Hosp Infant Mex. 2013;70(6):456–466.
44. Ribeiro SHB, De paula CS, Bordini D, Mari JJ, Caetano SC. Barriers to early identification of autism in Brazil. Rev Bras Psiquiatr. 2017;39(4):352–354. doi:10.1590/1516-4446-2016-2141
45. Daley TC. From symptom recognition to diagnosis: children with autism in urban India. Soc Sci Med. 2004;58(7):1323–1335. doi:10.1016/S0277-9536(03)00330-7
46. Quilendrino MIO, Castor MAR, Mendoza NRNP, Vea JR, Castillo-Carandang NT. Parents’ perceptions of autism and their health-seeking behaviors. Clin Epidemiol Glob Heal. 2015;3:S10–S15. doi:10.1016/j.cegh.2015.11.003
47. Ošlejšková H, Kontrová I, Foralová R, Dušek L, Némethová D. The course of diagnosis in autistic patients: the delay between recognition of the first symptoms by parents and correct diagnosis. Neuroendocrinol Lett. 2007;28(6):895–900.
48. Montiel-Nava C, Chacín JA, González-ávila Z. Age of diagnosis of autism spectrum disorder in Latino children: the case of Venezuelan children. Autism. 2017;21(5):573–580. doi:10.1177/1362361317701267
49. Talero-Gutiérrez C, Rodríguez M, De La Rosa D, Morales G, Vélez-van-meerbeke A. Profile of children and adolescents with autism spectrum disorders in an institution in Bogotá, Colombia. Neurol (English Ed). 2012;27(2):90–96. doi:10.1016/j.nrleng.2012.03.001
50. Masri AT, Al Suluh N, Nasir R. Diagnostic delay of autism in Jordan: review of 84 cases. Libyan J Med. 2013;8(1):1–2. doi:10.3402/ljm.v8i0.21725
51. Daniels AM, Mandell DS. Explaining differences in age at autism spectrum disorder diagnosis: a critical review. Autism. 2014;18(5):583–597. doi:10.1177/1362361313480277
52. van ’t Hof M, Tisseur C, van Berckelear-onnes I, et al. Age at autism spectrum disorder diagnosis: a systematic review and meta-analysis from 2012 to 2019. Autism. 2021;25(4):862–873. doi:10.1177/1362361320971107
53. Vig S, Jedrysek E. Autistic features in young children with sigificant cognitive impairment: autism or mental retardation? J Autism Dev Disord. 1999;29(3):235–248. doi:10.1023/a:
54. Sunita BJLC. Early identification of autism: a comparison of the checklist for autism in toddlers and the modified checklist for autism in toddlers. J Paediatr Child Health. 2013;49(6):438–444. doi:10.1111/j.1440-1754.2012.02558.x
55. Carbone PS, Campbell K, Wilkes J, et al. Primary care autism screening and later autism diagnosis. Pediatrics. 2020;146(2). doi:10.1542/peds.2019-2314
56. Desarkar P, Rajji TK, Ameis SH, Daskalakis ZJ. Assessing and stabilizing aberrant neuroplasticity in autism spectrum disorder: the potential role of transcranial magnetic stimulation. Front Psychiatry. 2015;6:1–6. doi:10.3389/fpsyt.2015.00124
57. Pierce K, Gazestani VH, Bacon E, et al. Evaluation of the diagnostic stability of the early autism spectrum disorder phenotype in the general population starting at 12 months. JAMA Pediatr. 2019;173(6):578–587. doi:10.1001/jamapediatrics.2019.0624
58. Why It’s DG. Important to continue universal autism screening while research fully examines its impact. JAMA Pediatr. 2016;170(6):527. doi:10.1001/jamapediatrics.2016.0163
59. Elsabbagh M, Divan G, Koh YJ, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res. 2012;5(3):160–179. doi:10.1002/aur.239
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


