Back to Journals » Cancer Management and Research » Volume 14
Clinical Characteristics and Survival Outcomes of Infiltrating Lobular Carcinoma: A Retrospective Study of 365 Cases in China
Authors Han B, Gu Z, Liu Z, Ling H
Received 26 October 2021
Accepted for publication 6 February 2022
Published 16 February 2022 Volume 2022:14 Pages 647—658
DOI https://doi.org/10.2147/CMAR.S346319
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Boyue Han,1,2,* Zhangyuan Gu,3,* Zhebin Liu,1,2 Hong Ling1,2
1Department of Breast Surgery, Fudan University Shanghai Cancer Center, Fudan University, Shanghai, 200032, People’s Republic of China; 2Department of Oncology, Shanghai Medical College, Fudan University, Shanghai, 200032, People’s Republic of China; 3Department of Breast Surgery, Shanghai First Maternity and Infant Hospital, Tongji University School of Medicine, Shanghai, 200040, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhebin Liu; Hong Ling, Email [email protected]; [email protected]
Purpose: The objective of this study was to compare the demographic characteristics, clinicopathological factors and survival outcomes between infiltrating lobular carcinoma (ILC) and infiltrating ductal carcinoma (IDC) using our single-center database.
Methods: Seventeen thousand two hundred and three breast cancer patients were treated at Fudan University Shanghai Cancer Center (FUSCC) from January 2000 to December 2017. We identified 365 cases with ILC and 16,838 cases with IDC. The Pearson chi-square test was used to compare tumor characteristics, and the Kaplan–Meier methods were used to perform the survival analysis.
Results: ILC had some distinctive characteristics from IDC such as older age (ranged from 61 to 80: ILC 26.8% vs IDC 19.9%, P < 0.001; over 80: ILC 1.6% vs IDC 0.8%, P < 0.001), larger tumor size (ranged from 2 to 5: ILC 45.2% vs IDC 37.1%, P = 0.011), much more hormone receptor expression (ILC 92.9% vs IDC 73.0%, P < 0.001), extremely less HER-2 expression (ILC 7.1% vs IDC 25.9%, P < 0.001). The overall survival and disease-free survival of ILC were worse than IDC (5-year OS, ILC 93.6% vs IDC 94.5%, P < 0.001; 5-year DFS, ILC 88.5% vs IDC 91.6%, P = 0.008). It was worth noting that the ILC patients had a worse overall survival than IDC patients after our propensity score matching study (P = 0.037). The univariate analysis concluded that positive HR (hormone receptor), high expression of Ki-67 and higher pathologic tumor stage were poor prognostic markers of ILC. Multivariate analysis demonstrated that tumor stage was a poor prognostic marker after adjustment for the effects of the above three factors. The most common primary site of metastasis was bone, but the proportion in the ILC group was much higher than that in the IDC group (56.25% vs 36.40%, P = 0.003).
Conclusion: Compared with IDC, ILC survived worse and was more prone to bone metastasis. Therefore, a comprehensive understanding of ILC and specific treatments are needed for further research.
Keywords: infiltrating lobular carcinoma, infiltrating ductal carcinoma, survival, prognosis
Background
Breast cancer is a heterogeneous disease composed of different pathological subtypes.1,2 Infiltrating lobular carcinoma (ILC) accounts for 10–15% of all breast cancers.3,4 Compared with the predominant histological subtype, infiltrating ductal carcinoma (IDC), ILC is recognized as a distinct and understudied disease.4,5 ILC tended to occur in older women.6–8 Especially, the incidence of ILC was linked to hormone replacement therapy among postmenopausal patients.9
Previous studies suggested that ILC was generally more challenging to visualize or palpate than IDC, clinically and mammographically.10,11 The prognosis of ILC has been described as either better or no different from IDCs,10,12,13 so a much deeper understanding of the clinical outcome is needed.14
To investigate clinical features and survival outcomes of ILC, we undertook a comparison of ILC and IDC using our single-center database. We aim to provide a more comprehensive and authentic assessment of the biological phenotypes and clinical characteristics, providing helpful information for clinical therapeutic strategies.
Patients and Methods
Participant Eligibility and Data Collection
The medical records of patients treated from January 2000 to December 2017 at the breast surgery department of FUSCC were reviewed. To analyze the clinical and pathological characteristics of ILC and IDC patients, we studied many variables, including the age of the patients, pathologic tumor size, lymph node status, histological grade, estrogen receptor (ER) and progesterone receptor (PR) status, expression of human epidermal growth factor receptor-2 (HER-2), expression of Ki-67, the surgery type and other treatments (adjuvant/neoadjuvant chemotherapy, radiotherapy, endocrine therapy and target therapy). ER or PR positive were considered HR (hormone receptor) positive status.15 The proportion of metastasis sites (such as bone, brain, liver, lung, lymph nodes, ovary) and the site counts in ILC and IDC were calculated separately.
Statistical Analysis
Comparisons of clinical characteristics between those two groups were examined by using Pearson Chi-square tests. The primary endpoint for this study was overall survival (OS) and disease-free survival (DFS). OS was defined as the number of months from diagnosis to the date of death from any causes. Disease-free survival (DFS) was defined as the time between the first date of diagnosis to any locoregional recurrence, including ipsilateral breast, local/regional lymph nodes of the disease, contralateral breast cancer, any distant metastasis of the disease, or any secondary malignancy, whichever occurred first. OS and DFS curves were obtained using the Kaplan–Meier methods. The impacts of relative factors were assessed in univariate and multivariable Cox proportional hazards models, such as the age, cancer stage, hormone receptor status, of potential prognostic value in correlation with patient survival. A two-sided p-value less than 0.05 was considered statistically significant for all tests. Statistical analyses were performed using SPSS statistical software version 25.0 packages (IBM Corporation, Armonk, NY, USA). Propensity score matching (PSM) was employed (Match Ratio: 1:3) using R software version 3.5.3. (The R Project for Statistical Computing, https://www.r-project.org/). The R packages “MatchIt”, “survminer”, “cmprsk”, and “foreign” with the appropriate libraries were used.
Results
General Information
The clinical characteristics of the two histological subtypes are summarized in Table 1. In this study, there were 17,203 female breast cancer patients enrolled. Three hundred sixty-five patients (2.12%) in total patients were diagnosed as infiltrating lobular carcinoma of the breast (ILC group), and 16,838 patients (97.88%) were diagnosed as infiltrating ductal carcinoma (IDC group).
 |
Table 1 Clinicopathological Characteristics of ILC Patients and IDC Patients |
The study showed a difference in age distribution between the ILC group and the IDC group. ILC patients were usually older than IDC patients, especially in the group whose age ranged from 61 to 80 (ILC 26.8% vs IDC 19.9%, P < 0.001) and in the group whose age was over 80 (ILC 1.6% vs IDC 0.8%, P < 0.001).
Tumor Characteristics
Tumor size of ILC patients was usually larger than the tumor size of IDC patients, especially in the group whose tumor dimension ranged from 2 to 5 (ILC 45.2% vs IDC 37.1%, P = 0.011). The ILC group tended to have more lymph nodes metastasis than the IDC group (N3: ILC 13.7% vs IDC 5.8%, P < 0.01). The proportion of elevated Ki-67 group of ILC patients was much less than that of IDC patients (ILC 25.5% vs IDC 43.1%, P < 0.001). Besides, patients with ILC had a higher HR rate (ILC 92.9% vs IDC 73.0%, P < 0.001) and lower HER-2 expression rate (ILC 7.1% vs IDC 25.9%, P < 0.001).
Molecular Subtypes
We exhibited a subtype distribution map for both groups in Figure 1. Compared with IDC, the ILC patients showed a discrepant distribution of molecular subgroups: luminal A breast cancer was the most frequent (59% in ILC vs 30% in IDC, P < 0.001), followed by luminal B breast cancer (23% in ILC vs 29% in IDC, P < 0.001). The proportion of both triple-negative breast cancer (TNBC) and HER-2 overexpression breast cancer was much more prominent in the IDC patients (6% in ILC vs 13% in IDC; 2% in ILC vs 12% in IDC, P < 0.001) (Figure 1).
Treatments
Compared with IDC group, fewer patients underwent breast conservative surgery (ILC 15.1% vs IDC 18.6%, P = 0.049). This study also demonstrated that fewer percentages of ILC patients were handled with adjuvant chemotherapy (ILC 63.8% vs IDC 71.0%, P < 0.001). Besides, more ILC patients received radiotherapy than IDC patients (ILC 41.1% vs IDC 35.9%, P<0.05).
According to the HR and HER-2 status between ILC and IDC patients, many more patients were treated with endocrine therapy in the ILC group (ILC 80.0% vs IDC 62.9%, P < 0.001), while significantly fewer patients in the ILC group were treated with target therapy (ILC 4.9% vs IDC 13.7%, P < 0.001).
Survival Analysis
In this study, the median follow-up duration was 65.7 months (mean, 68.7 months; range, 3 to 148 months). Figure 2 shows the OS and DFS curves. It showed that the ILC group had a worse survival than the IDC group. The OS in the ILC group was 93.6%, while in the IDC group, it was 94.5% (P < 0.001). Regarding the DFS curve, the 5-year DFS of all ILC patients was 88.5%, while in the IDC group was 91.6% (P = 0.008) (Figure 2). We further conducted DFS curves of the different molecular subgroups in the ILC and IDC cohorts. It was worth noting that IDC patients had a better prognosis than ILC patients in Luminal B (P = 0.012) and TNBC subtype (P < 0.001) (Figure S1).
Propensity score matching (PSM) was employed (Match Ratio: 1:3) to eliminate the bias of demographic and clinicopathological features between ILC and IDC groups (list of variables in Table 2). After matching, the 5-year OS of ILC was still worse than that of IDC (P = 0.037) (Figure 3).
 |
Table 2 Clinicopathological Characteristics of ILC Patients and IDC Patients After the Propensity Score Matching |
 |
Figure 3 OS Kaplan–Meier curve for ILC and IDC after matching propensity score. (ILC vs IDC P = 0.037, Log rank test). |
Univariate and Multivariate Cox Regression Analysis in ILC Group
In univariate Cox regression analysis, positive HR (P < 0.001), high expression of Ki-67 (P=0.001), and cancer stage III (P < 0.001) were correlated with significantly worse DFS in the ILC group. When these elements were put into a multivariate Cox regression analysis for ILC recurrence, cancer stage (P < 0.001) and Ki-67 (P = 0.017) were independent prognostic factors (Table 3).
 |
Table 3 Univariate Analysis and Multivariate Analysis for DFS in ILC Group |
It was remarkable that 5-year OS showed a similar effect. In univariate Cox regression analysis, positive HR (P = 0.036), high expression of Ki-67 (P=0.019), and cancer stage III (P < 0.001) were associated with observably worse 5-year OS in the ILC group. When these elements were put into a multivariate Cox regression analysis, cancer stage III was an independent prognostic factor (P < 0.001) (Table 4).
 |
Table 4 Univariate Analysis and Multivariate Analysis for OS in ILC Group |
The Metastasis Sites in ILC Group and IDC Group
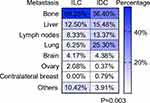
Figure 4 shows the metastasis sites in the ILC group and IDC group. It demonstrated that the most common primary site of metastasis was bone, but the proportion in the ILC group was much higher than that in the IDC group (56.25% vs 36.40%, P = 0.003). The liver was the second most common metastasis site (12.50%), followed by the lymph nodes (8.33%), lung (6.25%) and brain (4.17%) in the ILC group, while the order in the IDC group was the lung (25.30%), liver (15.48%), lymph nodes (13.37%) and brain (4.38%) (P = 0.003) (Table 5). We then compared the number of first metastasis sites in IDC and ILC, and found that there was no statistical difference (Table 6).
 |
Table 5 Metastasis Sites of ILC Patients and IDC Patients |
 |
Table 6 Metastasis Site Counts of ILC Patients and IDC Patients |
Table 7 shows the same second primary tumor occurrence trend after ILC and IDC. The top three malignant tumor happened were contralateral breast cancer (47.37% in ILC vs 37.39% in IDC), thyroid cancer (21.05% in ILC vs 22.41% in IDC), and lung cancer (10.53% in ILC vs 37.39% in IDC 14.87%) (P = 0.824).
 |
Table 7 Second Primary Tumor of ILC Patients and IDC Patients |
Discussion
This study was a population‐based study with over five years of follow‐up time and a relatively large sample of ILC (n = 365) of a single-centre database. The study reflected that in Chinese women, the incidence of the age distribution of both ILC and IDC groups reached the peak in their 40ʹs to 50ʹs, and then it declined afterwards. Compared to patients with IDC, patients with ILC were older, especially in their 60ʹs to 70ʹs.
This study indicated that tumor size was more prominent in the ILC group, wildly when dimension(cm) of tumor ranged from 2 to 5. This conclusion stayed in step with the study of Lee et al.16 The absence of desmoplastic reaction might make the lesion of ILCs impalpable and invisible, as explained in the studies of Jung et al, Li et al and Arpino et al.9,17,18 That was also the reason why patients with ILC were diagnosed at a relatively late stage.
Our study revealed that ILC had a higher incidence of HR expression and a lower rate of HER-2 expression,19 which was consistent with the study of Soslow et al. Anti-HER-2 therapy is generally performed in HER-2 positive breast cancers;20 however, the HER-2 overexpression rate was as low as 7.1%. Clinical case reports have shown that patients with ERBB2-mutated breast cancers respond to targeted HER-2 therapy;21,22 and this was confirmed by responses to neratinib seen in ERBB2-mutated cancers in the SUMMIT trial.23 This emphasizes the importance of precision genetic sequencing, which can help provide therapy alterations. As clinical cancer sequencing becomes more routine, more ILC will benefit from targeted therapy.
In agreement with the study of Pestalozzi et al,24 this study concluded that ILC was treated only a little less often with conservative breast surgery than IDC, probably because ILC was larger and referred to as a multicentric tumor. Previous studies reported that in terms of tumor downstaging, the benefits of neoadjuvant chemotherapy for ILC are limited.25,26 As the pCR (pathologic complete remission) rate for ILC is relatively low,27 locally advanced tumors, given the expected benefits, are minimal, consistent with the relatively low breast conservation rate.
As a general rule, the high expression of Ki-67 indicates that tumors are prone to recurrence and metastasis, which is a poor prognostic index,28,29 and has significant reference value for judging the prognosis of diseases.30–33 This study found that ILC had a lower Ki-67 score than IDC; thus, it explained the poor prognosis of ILC. The hallmark feature of cancer cells is uncontrolled division and reproduction, and many widely used clinical chemotherapeutics target this feature to prevent the rapid proliferation of cancer cells. It has been reported that mitotic activity, measured by the Ki-67 index, significantly reflected chemotherapy sensitivity. Besides, the advantage of chemotherapy is unclear for low Ki-67 patients.34 The study of Mathieu et al hinted that a lower Ki-67 score was a critical element associated with less adjuvant chemotherapy of ILC than IDC.35 Our results showed a high proportion of positive HR and low expression of Ki-67 in ILC, so it was supposed that most ILC patients were probably endocrine-sensitive but chemotherapy-insensitive. Therefore, it accounted for the lower proportion of chemotherapy and the large proportion of endocrine therapy in ILC patients.
In terms of prognosis, data showed that no matter 5-year OS or DFS, the prognosis of ILC patients was worse than that of IDC patients, the results are similar to those reported by Lee et al16 and Arpino et al.18 However, the study of Pestalozzi et al reported that the early-stage prognosis for ILC was better than that for IDC, while late-stage prognosis for ILC was worse.24 Previous studies showed the benefits of breast MRI for ILC, especially in the early detection of masses with irregular or spiculated margins or non-mass enhancing lesions.36 Inspired by this, we could try to use MRI to reduce the delayed diagnosis rate of ILC patients and improve the early-stage prognosis for ILC. Besides, the study of Jayasinghe et al reported that 10-year survival of women with 84% for ILC, compared to IDC for 69% (p = 0.073).12 The difference of prognosis between this study and previous researches exposed a few limitations of this study. For instance, it was only a retrospective but not prospectively designed study. Besides, it was only a single-centre study. Nevertheless, in our study, when excluding prognosis factors by propensity score matching, it was worth noting that the prognosis of ILC was worse than that for IDC.
A previous study of Jayasinghe et al reported a higher risk ratio (RR) with young age at diagnosis, greater tumor size, higher pathologic stage and number of positive lymph nodes.12 In contrast, this study found that positive HR, high expression of Ki-67 and higher pathologic stage were independent prognostic indicators. After adjusting for the effects of the above three factors, survival declined with a higher pathologic stage.
As showed in Teo et al study, the sites of distant metastatic of ILC was different from that of IDC.37 In this study, ILC was less likely to affect livers and lungs than IDC did. Conversely, bone and brain were much more likely to be affected by ILC. An earlier study of Mathew et al found that after diagnosis of distant metastasis, there was no outcome difference between ILC and IDC,38 while the study of Blohmer et al showed that, after diagnosis of the first distant metastasis, survival was much shorter for ILC patients than IDC patients.39 The Cancer Genome Atlas (TCGA) research network recently published results of genomic characterization of 490 IDC and 127 ILC breast cancer cases.2,40 As expected, ILC was prone to luminal A subtype, CDH1 mutations, and loss of E-cadherin by mRNA expression. The E-cadherin gene functions prevent tumor invasion,41 and the loss of E-cadherin in ILC results in an increased capacity for tissue invasion. Therefore, the TCGA results provide possible molecular mechanisms for the different metastasis tendencies of ILC and IDC.
Because of the lack of relevant studies, ILC is treated in the same manner as IDC according to IDC’s international group consensus.42 However, ILC is well established as a distinctive disease process,43 and our study demonstrated the distinct clinical characteristics and survival outcomes of ILC. So a “one size fits all” approach to therapy for all invasive breast carcinomas is not optimized for particular subtypes such as ILC. Thus, clinical trials designed to investigate improvements to the therapeutic management of ILC are needed.
Conclusions
In summary, ILC had some distinct characteristics from IDC, such as older age, larger tumor size, more positive HR expression and less HER-2 expression. Moreover, ILC survives worse than IDC. It demonstrated that bone metastasis in the ILC group was much higher than that in the IDC group. So we should pay attention to the treatment of bone metastases, which is an essential factor in controlling the development of ILC patients. For some advanced patients, genetic testing and targeted therapy is also the future direction we can work. In short, we expect that the comprehensive understanding of ILC will provide beneficial evidence for the clinicians and other clinical trials are necessary to conduct.
Data Sharing Statement
All data generated or analyzed during this study are reflected in the present published article [and its Supplementary Information].
Ethics Statement
This study did not involve animals. All procedures performed in studies involving human participants were following the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ethics Committee Review Board approved this retrospective study of Fudan University Shanghai Cancer Center (050432). The need to obtain informed consent was waived, as the study was a retrospective study, and there was no additional risk to patients. All data were anonymized to maintain patient privacy.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors state that they have no competing interests.
References
1. Sotiriou C, Pusztai L. Gene-expression signatures in breast cancer. N Engl J Med. 2009;360(8):790–800. doi:10.1056/NEJMra0801289
2. Ciriello G, Gatza ML, Beck AH, et al. Comprehensive molecular portraits of invasive lobular breast cancer. Cell. 2015;163(2):506–519. doi:10.1016/j.cell.2015.09.033
3. McCart Reed AE, Kutasovic JR, Lakhani SR, Simpson PT. Invasive lobular carcinoma of the breast: morphology, biomarkers and ‘omics. Breast Cancer Res. 2015;17:12. doi:10.1186/s13058-015-0519-x
4. Sikora MJ, Jankowitz RC, Dabbs DJ, Oesterreich S. Invasive lobular carcinoma of the breast: patient response to systemic endocrine therapy and hormone response in model systems. Steroids. 2013;78(6):568–575. doi:10.1016/j.steroids.2012.11.002
5. Tasdemir N, Ding K, Savariau L, et al. Proteomic and transcriptomic profiling identifies mediators of Anchorage-independent growth and roles of inhibitor of differentiation proteins in invasive lobular carcinoma. Sci Rep. 2020;10(1):11487. doi:10.1038/s41598-020-68141-9
6. Lyu H, Fu LM, Tu XY, et al. [Invasive breast lobular carcinoma with extracellular mucin: a clinicopathological analysis]. Zhonghua Bing Li Xue Za Zhi. 2019;48(10):779–783. Chinese. doi:10.3760/cma.j.issn.0529-5807.2019.10.006
7. de Kruijf EM, Bastiaannet E, Ruberta F, et al. Comparison of frequencies and prognostic effect of molecular subtypes between young and elderly breast cancer patients. Mol Oncol. 2014;8(5):1014–1025. doi:10.1016/j.molonc.2014.03.022
8. Li CI, Anderson BO, Porter P, Holt SK, Daling JR, Moe RE. Changing incidence rate of invasive lobular breast carcinoma among older women. Cancer. 2000;88(11):2561–2569. doi:10.1002/1097-0142(20000601)88:11<2561::AID-CNCR19>3.0.CO;2-X
9. Jung NY, Kim SH, Kim SH, et al. Effectiveness of breast MRI and (18) F-FDGPET/CT for the preoperative staging of invasive lobular carcinoma versus ductal carcinoma. J Breast Cancer. 2015;18(1):63–72. doi:10.4048/jbc.2015.18.1.63
10. Quan ML, Sclafani L, Heerdt AS, Fey JV, Morris EA, Borgen PI. Magnetic resonance imaging detects unsuspected disease in patients with invasive lobular cancer. Ann Surg Oncol. 2003;10(9):1048–1053. doi:10.1245/ASO.2003.03.016
11. Franceschini G, Manno A, Mule A, et al. Gastro-intestinal symptoms as clinical manifestation of peritoneal and retroperitoneal spread of an invasive lobular breast cancer: report of a case and review of the literature. BMC Cancer. 2006;6:193. doi:10.1186/1471-2407-6-193
12. Jayasinghe UW, Bilous AM, Boyages J. Is survival from infiltrating lobular carcinoma of the breast different from that of infiltrating ductal carcinoma? Breast J. 2007;13(5):479–485. doi:10.1111/j.1524-4741.2007.00468.x
13. Toikkanen S, Pylkkanen L, Joensuu H. Invasive lobular carcinoma of the breast has better short- and long-term survival than invasive ductal carcinoma. Br J Cancer. 1997;76(9):1234–1240. doi:10.1038/bjc.1997.540
14. Cao AY, Huang L, Wu J, et al. Tumour characteristics and the clinical outcome of invasive lobular carcinoma compared to infiltrating ductal carcinoma in a Chinese population. World J Surg Oncol. 2012;10:152. doi:10.1186/1477-7819-10-152
15. Hammond ME, Hayes DF, Wolff AC, Mangu PB, Temin S. American society of clinical oncology/college of American pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract. 2010;6(4):195–197. doi:10.1200/JOP.777003
16. Lee JH, Park S, Park HS, Park BW. Clinicopathological features of infiltrating lobular carcinomas comparing with infiltrating ductal carcinomas: a case control study. World J Surg Oncol. 2010;8:34. doi:10.1186/1477-7819-8-34
17. Li CI, Anderson BO, Daling JR, Moe RE. Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA. 2003;289(11):1421–1424. doi:10.1001/jama.289.11.1421
18. Arpino G, Bardou VJ, Clark GM, Elledge RM. Infiltrating lobular carcinoma of the breast: tumour characteristics and clinical outcome. Breast Cancer Res. 2004;6(3):R149–156. doi:10.1186/bcr767
19. Soslow RA, Carlson DL, Horenstein MG, Osborne MP. A comparison of cell cycle markers in well-differentiated lobular and ductal carcinomas. Breast Cancer Res Treat. 2000;61(2):161–170. doi:10.1023/A:1006479113769
20. Riedlinger GM, Joshi S, Hirshfield KM, Barnard N, Ganesan S. Targetable alterations in invasive pleomorphic lobular carcinoma of the breast. Breast Cancer Res. 2021;23(1):7. doi:10.1186/s13058-020-01385-5
21. Ali SM, Alpaugh RK, Downing SR, et al. Response of an ERBB2-mutated inflammatory breast carcinoma to human epidermal growth factor receptor 2-targeted therapy. J Clin Oncol. 2014;32(25):e88–91. doi:10.1200/JCO.2013.49.0599
22. Ben-Baruch NE, Bose R, Kavuri SM, Ma CX, Ellis MJ. HER2-mutated breast cancer responds to treatment with single-agent neratinib, a second-generation HER2/EGFR tyrosine kinase inhibitor. J Natl Compr Canc Netw. 2015;13(9):1061–1064. doi:10.6004/jnccn.2015.0131
23. Hyman DM, Piha-Paul SA, Won H, et al. HER kinase inhibition in patients with HER2- and HER3-mutant cancers. Nature. 2018;554(7691):189–194. doi:10.1038/nature25475
24. Pestalozzi BC, Zahrieh D, Mallon E, et al. Distinct clinical and prognostic features of infiltrating lobular carcinoma of the breast: combined results of 15 International Breast Cancer Study Group clinical trials. J Clin Oncol. 2008;26(18):3006–3014. doi:10.1200/JCO.2007.14.9336
25. Delpech Y, Coutant C, Hsu L, et al. Clinical benefit from neoadjuvant chemotherapy in oestrogen receptor-positive invasive ductal and lobular carcinomas. Br J Cancer. 2013;108(2):285–291. doi:10.1038/bjc.2012.557
26. Tsung K, Grobmyer SR, Tu C, Abraham J, Budd GT, Valente SA. Neoadjuvant systemic therapy in invasive lobular breast cancer: is it indicated? Am J Surg. 2018;215(3):509–512. doi:10.1016/j.amjsurg.2017.11.011
27. Thomas M, Kelly ED, Abraham J, Kruse M. Invasive lobular breast cancer: a review of pathogenesis, diagnosis, management, and future directions of early stage disease. Semin Oncol. 2019;46(2):121–132. doi:10.1053/j.seminoncol.2019.03.002
28. Robertson S, Stalhammar G, Darai-Ramqvist E, et al. Prognostic value of Ki67 analysed by cytology or histology in primary breast cancer. J Clin Pathol. 2018;71(9):787–794. doi:10.1136/jclinpath-2017-204976
29. Ellis MJ, Suman VJ, Hoog J, et al. Ki67 proliferation index as a tool for chemotherapy decisions during and after neoadjuvant aromatase inhibitor treatment of breast cancer: results from the American College of Surgeons Oncology Group Z1031 trial (alliance). J Clin Oncol. 2017;35(10):1061–1069. doi:10.1200/JCO.2016.69.4406
30. Van Asten K, Slembrouck L, Olbrecht S, et al. Prognostic value of the progesterone receptor by subtype in patients with estrogen receptor-positive, HER-2 negative breast cancer. Oncologist. 2019;24(2):165–171. doi:10.1634/theoncologist.2018-0176
31. Yuan P, Xu B, Wang C, Zhang C, Sun M, Yuan L. Ki-67 expression in luminal type breast cancer and its association with the clinicopathology of the cancer. Oncol Lett. 2016;11(3):2101–2105. doi:10.3892/ol.2016.4199
32. Besusparis J, Plancoulaine B, Rasmusson A, et al. Impact of tissue sampling on accuracy of Ki67 immunohistochemistry evaluation in breast cancer. Diagn Pathol. 2016;11(1):82. doi:10.1186/s13000-016-0525-z
33. Focke CM, Burger H, van Diest PJ, et al. Interlaboratory variability of Ki67 staining in breast cancer. Eur J Cancer. 2017;84:219–227. doi:10.1016/j.ejca.2017.07.041
34. Zhu X, Chen L, Huang B, et al. The prognostic and predictive potential of Ki-67 in triple-negative breast cancer. Sci Rep. 2020;10(1):225. doi:10.1038/s41598-019-57094-3
35. Mathieu MC, Rouzier R, Llombart-Cussac A, et al. The poor responsiveness of infiltrating lobular breast carcinomas to neoadjuvant chemotherapy can be explained by their biological profile. Eur J Cancer. 2004;40(3):342–351. doi:10.1016/j.ejca.2003.08.015
36. Amin AL, Sack S, Larson KE, et al. Does the addition of breast MRI add value to the diagnostic workup of invasive lobular carcinoma? J Surg Res. 2021;257:144–152. doi:10.1016/j.jss.2020.07.035
37. Teo K, Gomez-Cuadrado L, Tenhagen M, et al. E-cadherin loss induces targetable autocrine activation of growth factor signalling in lobular breast cancer. Sci Rep. 2018;8(1):15454. doi:10.1038/s41598-018-33525-5
38. Mathew A, Rajagopal PS, Villgran V, et al. Distinct pattern of metastases in patients with invasive lobular carcinoma of the breast. Geburtshilfe Frauenheilkd. 2017;77(6):660–666. doi:10.1055/s-0043-109374
39. Blohmer M, Zhu L, Atkinson JM, et al. Patient treatment and outcome after breast cancer orbital and periorbital metastases: a comprehensive case series including analysis of lobular versus ductal tumour histology. Breast Cancer Res. 2020;22(1):70. doi:10.1186/s13058-020-01309-3
40. Metzger-Filho O, Ferreira AR, Jeselsohn R, et al. Mixed invasive ductal and lobular carcinoma of the breast: prognosis and the importance of histologic grade. Oncologist. 2019;24(7):e441–e449. doi:10.1634/theoncologist.2018-0363
41. Vleminckx K, Vakaet L, Mareel M, Fiers W, van Roy F. Genetic manipulation of E-cadherin expression by epithelial tumour cells reveals an invasion suppressor role. Cell. 1991;66(1):107–119. doi:10.1016/0092-8674(91)90143-M
42. Carcoforo P, Raiji MT, Langan RC, et al. Infiltrating lobular carcinoma of the breast presenting as gastrointestinal obstruction: a mini review. J Cancer. 2012;3:328–332. doi:10.7150/jca.4735
43. McCart Reed AE, Kalinowski L, Simpson PT, Lakhani SR. Invasive lobular carcinoma of the breast: the increasing importance of this special subtype. Breast Cancer Res. 2021;23(1):6. doi:10.1186/s13058-020-01384-6
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.