Back to Journals » Vascular Health and Risk Management » Volume 19
Clinical Characteristics and Treatment Outcomes of Acute Ischemic Stroke with Atrial Fibrillation Among Patients Admitted to Tertiary Care Hospitals in Amhara Regional State: Retrospective-Cohort Study
Received 20 November 2023
Accepted for publication 13 December 2023
Published 19 December 2023 Volume 2023:19 Pages 837—853
DOI https://doi.org/10.2147/VHRM.S447936
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Zenaw Debasu Addisu,1,2 Teshale Ayele Mega2
1Department of Pharmacy, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia; 2Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Correspondence: Zenaw Debasu Addisu, Email [email protected]
Background: Atrial fibrillation (AF) is the leading cause of a surge in hospital expenses for the treatment of strokes. However, evidence regarding clinical features and survival of patients admitted with acute ischemic stroke (AIS) plus AF in Ethiopia is lacking.
Objective: We assess clinical characteristics, survival, and predictors of mortality of patients with acute ischemic stroke and atrial fibrillation among patients admitted to Tertiary Care Hospitals in Amhara regional state.
Methods: A retrospective cohort study was done on patients diagnosed with AIS who received care at Tibebe Ghion and Felege Hiwot hospitals from November 2018 to November 2021. Data were analyzed using SPSS version 25. Cox regression analysis was used to identify predictors of in-hospital mortality. Kaplan–Meier analysis was used to identify survival rates and mean survival time. The hazard ratio was used as a measure of the strength of the association and statistical significance was declared at p-value < 0.05.
Results: Of 378 patients with AIS, 58.7% were male. AF was diagnosed in 102 (26.9%) patients. Compared with patients without AF, patients with AF were more likely to have Glasgow Coma Scale < 8 (83.3 vs 4%), valvular heart disease (56.9 vs 4.7%), and coronary heart disease (11.8 vs 4%). Patients with AF had a significant incidence of in-hospital mortality (38 per 1000 vs 17 per 1000) person-days. Glasgow Coma Scale < 8: (AHR=12.69, 95% CI: [2.603– 61.873]), aspirational pneumonia (AHR=2.602, 95% CI: 1.085– 6.242), acute renal failure (AHR=6.114, 95% CI: [1.817– 20.576]), hypokalemia (AHR=1.179, 95% CI: [1.112,-3.373]), atrial fibrillation (AHR=1.104, 95% CI: [1.015– 5.404]), HIV/AIDS (AHR=8.302, 95% CI: [1.585– 43.502]) and chronic liver disease (AHR=4.969, 95% CI: [1.192– 20.704]) were indicators of in-hospital mortality.
Conclusion: In the current study, hospital mortality was greater in AIS associated with atrial fibrillation. Stroke-related complications were significant predictors of mortality. Hence, effective strategies should be in place to curb the impacts of these factors.
Keywords: acute ischemic stroke, atrial fibrillation, clinical characteristics
Background
Stroke is the second-most leading cause of death following ischemic heart disease, contributing to 9% of all fatalities worldwide.1 It also ranks as the fourth-largest global cause of disease burden.2 The World Health Organization (WHO) describes acute stroke as quickly developing neurological signs of focal (or global) abnormalities in brain function, with symptoms lasting 24 hr or more or resulting in death with no obvious cause apart from vascular origin.3 Stroke contributes significantly to morbidity, mortality, and disability in both developed and developing countries. It causes persistent problems in individuals such as physical dependence, cognitive deterioration, depression, and seizures.4
According to the American Heart Association (AHA), strokes are categorized as either ischemic (87%) or hemorrhagic (13%).5 Ischemic stroke, even substantially less lethal, has a 30-day mortality rate of 9% to 23%, compared to 46.5% for hemorrhagic stroke.6 Of these, approximately 25–40% are cardioembolic strokes attributable to atrial fibrillation.7
Atrial fibrillation (AF) is the most prominent supraventricular tachyarrhythmia and the leading cause of ischemic stroke in the elderly.8 It is also the most common arrhythmia that is associated with a high risk of stroke, particularly cardioembolic stroke.9 The prevalence of stroke events due to AF has tripled over the recent 30 years. AF can be divided into the first detected episode, recurrent arrhythmia, paroxysmal, persistent, and permanent.10 The guidelines recommend 24-hr Holter electrocardiogram (ECG) monitoring after acute ischemic stroke.11
It has been revealed that AF is one of the key contributing factors to hospital expenditures for stroke care.12 AF alone raises the risk of ischemic stroke by approximately five times across all ages,13 and the prevalence rises sharply with age, from 2% in individuals under the age of 50% to 40% in those over the age of 90.14 In addition, studies have shown that AF is a predictor of death in patients with acute ischemic stroke and can worsen hospital mortality in cardioembolic and atherothrombotic subtypes.15,16
Because the overall incidence of cardiovascular disease in developing countries is expected to rise by about 150% over the following 20 years as a result of an “epidemiological shift” from transmissible illnesses and malnutrition to more chronic disease conditions, as a result, subsequent success in the healthcare system depends on resolving this problem.17
The incidence and cost of chronic diseases such as stroke and other cardiovascular disorders are rising in sub-Saharan Africa. It adds to the burden of tropical diseases and stresses the region’s scarce health-care resources.18 In accordance with the WHO report of 2017, stroke fatalities accounted for 6.23% of all deaths in Ethiopia. Furthermore, the country’s age-adjusted stroke death rate is 89.82 per 100,000 people. Ischemic stroke has been identified as the sixth major cause of death.19 In SSA, there are many young stroke patients, leading to a greater number of years of potential productivity and years of life lost (YLL).20,21 This is also true in Ethiopia, where the rising incidence of stroke in Ethiopia is a threat to the healthcare system.22 Facilities for stroke treatment as well as rehabilitation are scarce.23 Indeed, patients with AF increased the costs of acute hospitalization significantly. Transferring patients from a hospital to a nursing facility, rather than the patient’s home, can considerably raise the expense of post-hospital stroke care.24
Despite this, very few studies have been carried out in Ethiopia on the outcomes of strokes.25,26 These studies showed that ischemic stroke is more prevalent than hemorrhagic stroke and the overall mortality rate related to stroke was reported. Another hospital-based study by Greffie et al reports that AF occurred in 27 (28.7%) of the cases. The study also shows that AF was more prevalent in patients with ischemic stroke than hemorrhagic stroke.27 There is limited information on characteristics, treatment outcome, and case fatality of acute ischemic stroke with atrial fibrillation in Ethiopia. Therefore, this study aimed to assess clinical characteristics, survival, and predictors of mortality of patients with acute ischemic stroke and atrial fibrillation among patients admitted to Tertiary Care Hospitals in Amhara regional state.
Method
Study Design and Setting
A retrospective cohort study was employed from November 2018 up to November 2021 at Tibebe Ghion Specialized Hospital (TGSH) and Felege Hiwot Comprehensive Specialized Hospital (FHCSH), two specialized referral public hospitals in Bahir Dar City, North-Western Ethiopia. Bahir Dar City is located 587 km northwest of Addis Ababa, the capital city of Ethiopia.
Tibebe-Ghion comprehensive specialized hospital was established in 2018. It is a teaching hospital under the college of medicine and health sciences of Bahir Dar University located in Bahir Dar, Ethiopia. The hospital provides a tertiary-level health-care service and it is administered by Bahir Dar University.
Felege Hiwot comprehensive referral hospital was established in 1963. It is a referral hospital located in Bahir Dar. It provides health-care services with, surgical, gynecological, and acute care units, orthopedic wards, and outpatient departments.
Study Population and Patient Enrollment
The study population was all patients with acute ischemic stroke with atrial fibrillation admitted to the medical department of Tibebe Ghion Comprehensive Specialized Hospital and Felege Hiwot Comprehensive Specialized Hospital between November 2018 and November 2021 who were ≥18 years of age, acute ischemic stroke who was diagnosed according to the WHO guideline for the evaluation and managements of ischemic stroke. Patients with a history of AF confirmed by a prior electrocardiogram (ECG) or diagnosed by the attending physicians based on an ECG and/or 24-hr ECG monitoring upon admission were enrolled in this study. Missing AIS patient medical records, patients with incomplete medical records, patients with cerebral hemorrhage, and patients with TIA were excluded. Candidates who fulfilled the inclusion criteria were recruited using a consecutive sampling technique. The power analysis of this study was performed with Epi info 7.25 software using a 19% probability of death among patients with acute ischemic stroke and atrial fibrillation and 10% among patients with acute ischemic stroke only in another similar setting,28 80% power, and 2:1 ratio, of unexposed to exposed, and 5% significance level. Accordingly, the final sample size computed based on the above assumption is 475 which comprises 190 patients for acute ischemic stroke with atrial fibrillation and 285 patients for acute ischemic stroke only. However, due to a limited number of admissions, the study included all samples that met inclusion criteria during the study period.
Among the 470 eligible patients’ charts, 92 patients’ charts were eliminated for a variety of reasons. Therefore, 378 (AIS with AF = 102, AIS alone = 276) patients were included in the analysis Figure 1.
 |
Figure 1 Flow chart showing a selection of patients diagnosed with acute ischemic stroke in two hospitals from November 2018 to November 2021. |
Those patients with acute ischemic stroke and atrial fibrillation (AIS plus AF) were included in the exposed cohort, and those patients with acute ischemic stroke only (AIS alone) were included in the non-exposed cohort.
Data Collection Procedures and Study Variables
Records of acute ischemic stroke patients admitted at Tibebe Ghion Comprehensive Specialized Hospital and Felege Hiwot Comprehensive Specialized Hospital over a 3-year period (November 2018–November 2021) were reviewed using an English version checklist. The data abstraction tool was developed after reviewing different relevant literature. The checklist contains sociodemographic factors, disease-related variables and co-morbidities, clinical presentation on admission such as the Glasgow Coma Scale (GCS), time of hospital admission after ischemic stroke onset, and stroke-related complications during hospitalization (hospital stay), which were extracted from patient medical records. Furthermore, the checklist also contained medication-related factors (dosage regimen, type, and class of medications of previous medication) Antiplatelets, Anticoagulants, Antihypertensives, Statins Antidiabetic drugs. For the purpose of calculating the median survival time to event (death), the start time of the treatment and the point at which mortality occurred were also recorded. From January 22 to February 6, 2022, the data was accessed for research purposes, and data extraction was performed.
Outcome Definition and Measurement
In hospital mortality of patients with acute ischemic stroke in the presence or absence of atrial fibrillation, the mean survival time to mortality was considered as the outcome variable. The incidence of mortality was reported as person-days and the mean survival time to mortality was reported in days (Figure 2). Data on mortality were taken from the patient’s discharge summary notes. The written authorization of the attending physician served as confirmation of the patient’s mortality.
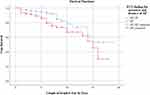 |
Figure 2 Kaplan-Meier estimate of survival rates in patients with atrial fibrillation and patients without atrial fibrillation. |
Data Quality Management
The primary investigator trained: two nurses and two pharmacists to build a shared common awareness of how to collect data and equip them with a checklist. The principal investigator provided on-site supervision and feedback to data collectors on a daily basis. Clarity and consistency were checked on all completed data-collecting forms. The data were reviewed regularly for consistency, completeness, clarity, and accuracy. Any errors, doubts, or incompleteness were addressed appropriately.
Statistical Analysis
The data analyses were carried out using the Statistical Package for the Social Sciences (SPSS) version 25. A descriptive analysis was carried out, and the results were presented in texts, tables, and diagrams. The mean, median, and interquartile range were used to present continuous variables. A chi-square test was performed to test for variation in baseline characteristics. Multivariate Cox regression was carried out to identify predictors of in-hospital mortality. Bivariate Cox regression was carried out to pick variables for multivariable Cox regression. Variables with p-value <0.2 in bivariate regression were considered for multivariable Cox regression. Kaplan Meier analyses were used to identify the survival rates and median survival time. The hazard ratio was used as a measure of the strength of the association and a p-value <0.05 was considered to declare statistical significance at a 95% confidence interval.
Operational Definition
- Ischemic stroke: patients who fulfilled the WHO’s case definition of stroke had brain CT scan results and standard 12 leads ECG report.
- Acute ischemic stroke is defined as an ischemic stroke in which symptoms appear within 24 hr to 7 days.29
- Atrial Fibrillation: The evaluation is made by reviewing the attached 12 lead ECG strips if available or if an ECG reading report with index of AF was found in the case records.
- Glasgow Coma Scale (GCS) is defined as good if GCS is between 13 and 15 or moderate if GCS is between (9–12), and GCS is defined as poor if GCS below 8.30
- Treatment outcome: in this study, treatment outcome refers to the status of patients during hospital discharge (in-hospital mortality) upon in-hospital treatment. In-hospital treatment includes all treatment given by the stroke team as soon as the patient arrives at the hospital, patient management according to national standard treatment guidelines, anticoagulation, pharmacotherapy for risk factors, treatment to provide to prevent complications, and treatments that provide specific care.
- Survival status: The status of the patient’s survival to the outcome (death) or censored.
- Censored: Time to event is not observed for reasons such as whether the subject had left against medical recommendation prior to experiencing an event.
- Time to death: was the time between the date of diagnosis of AIS and the date of in-hospital death.
Results
Socio-Demographic Characteristics
Of the 378 eligible patient’s charts, more than half, 222 (58.7%) of the patients were male and 244 (64.55%) were rural residents. Besides 274 (72.5%) were married, while 81 (21.7%) were widowed. The majority, 204 (54%) of patients were farmers, followed by 55 (14.6%) unemployed. Regarding religion, 317 (83.9%) were Orthodox Christians. Of the total patients, 264 (69.8%) had no formal education (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Patients Diagnosed with AIS from FHSCH and TGSCH from November 2018 to November 2021 (n=378) |
Baseline Characteristics of the Participants
Of the 378 patients admitted with AIS, 102 (26.9%) were diagnosed with AF. This group consisted of 58 (56.9%) valvular atrial fibrillation (VAF) patients and 44 (43.1%) non-valvular atrial fibrillation (NVAF) patients. Table 2 shows the baseline characteristics of AIS patients with the presence or absence of AF upon hospital admission. According to Trial of Org 10,172 in Acute Stroke Treatment (TOAST) criteria, 95 patients in the AF group were diagnosed as cardioembolic, accounting for 93.1% (95/102) of the patients and the remaining were categorized as strokes of undetermined etiology.
 |
Table 2 Baseline Characteristics of Acute Ischemic Stroke Patients with Atrial Fibrillation and Those Without Atrial Fibrillation (n=378) |
Female patients with AIS had a greater and considerably higher frequency of AF (52.9 vs 47.1%, P=0.005). AIS plus AF had significantly higher frequency in all age groups except those under the age of 53 and those between the ages of 54 and 64. Patients in the AIS plus AF group had a considerably higher frequency of a GCS of less than 8 (85 (83.3%) versus 11 (4%)), but mild and severe brain damage had a significantly higher frequency in the AIS alone group, ie, mild brain injuries (2 (2%) vs 184 (66.6%)) and for moderate brain injuries (15 (14.7%) vs 81 (29.3%)), respectively.
Regarding comorbidity, patients with AIS Plus AF had a significantly higher frequency of valvular heart disease (ie, CRVHD, prosthetic heart valve, and mechanical heart valve) (58 (56.9%) vs 13 (4.7%)), CHD (12 (11.8%) vs 11 (4%)), and DCMP (9 (8.8%) vs 8 (2.9%)) and a significantly lower frequency of Hypertensive status. Moreover, there is no apparent variation in time from symptom manifestation to hospitalization, alcohol consumption, and HHD, between groups. Although smoking was significantly higher in a patient with AIS plus AF, hyperlipidemia and current alcohol consumption were more common among patients with AIS alone. Only 17 (16%) of the AF group received oral anticoagulants prior to stroke onset, and 10 of these patients had an international normalized ratio (INR) on admission of less than 2.
Neurologic Deficits During Admission of Acute Ischemic Stroke Patients with and without Atrial Fibrillation
Table 3 compares the clinical presentation of neurologic deficits at admission in patients with AIS plus AF and AIS alone. The most common neurological deficit during hospital admission in the AF group was right or left-side body weakness 99 (97.1%) followed by Aphasia 86 (84.3%), loss of consciousness 69 (67.6%), and facial palsy 61 (59.8%) similarly most non-AF group presented with right or left-side body weakness 99 (97.1%) followed Aphasia 249 (90.2%), hemiparesis 125 (45.3%), and loss of consciousness 116 (42.0%).
 |
Table 3 Comparison of Neurologic Deficits During Admission Among Patients with Acute Ischemic Stroke Patients Plus Atrial Fibrillation and Those without Atrial Fibrillation |
In-Hospital Treatment Prescribed to the Study Participants
Regarding medications prescribed during hospitalization, patients with AF showed a greater rate of statin use ie, 101 (99%) followed by antiplatelet 95 (93.1%), antithrombotic 77 (75.5%), antibiotics 42 (41.2%), and only 39 (38.2%) patients were prescribed with anticoagulants. Other common prescribing medications like anticonvulsants (3(2.9%)), potassium chloride supplements (7(6.9%)), and diuretics (1(1%)) are less frequently prescribed in a patient with AIS plus AF. Similarly, among patients without AF statins 271 (98.5%), were prescribed more frequently followed by antiplatelet 270 (98.2%), antithrombotic 180 (65.5%), antibiotics 73 (26.5%), and antihypertensive 87 (31.6%) as shown in Table 4.
 |
Table 4 In-Hospital Treatment Prescribed of Patients with Acute Ischemic Stroke Plus Atrial Fibrillation and without Atrial Fibrillation |
In-Hospital Complications Among the Study Participants
Acute renal failure (22.5% vs 3.3%), hypokalemia (18.6% vs 10.1%), aspirational pneumonia (42.2% vs 28.7%), and Hemorrhagic transformation (11.8% vs 4.3%) are considerably more likely to be an in-hospital complication in AF groups than in non-AF groups, respectively. Although the difference is not statistically significant, the incidence of urinary tract infection, urine incontinence, and increase in intracranial pressure is higher in the groups without AF. Table 5 shows complications that occur in hospitals.
 |
Table 5 Stroke-Related Complications During Hospital Stay in a Patient with Acute Ischemic Stroke Plus Atrial Fibrillation and without Atrial Fibrillation |
Treatment Outcome of the Study Participants
About 59% (61) of patients from the AIS plus AF group and 68.8% (190) patients from the non-AF group were discharged with improvement. Eight (7.8%) patients from AIS plus AF group and 19 (6.88%) patients from the AIS alone group were discharged without improvement. Due to various social reasons, such as self and family requests, 7 (6.66%) patients from the AIS plus AF group and 43 (15.5%) patients from the AIS alone group were discharged against medical recommendation. According to our findings, in-hospital mortality from acute ischemic stroke was 13.22%. Among these, 26 (25.5%) patients were from the AF group and 24 (8.7%) patients were from the AIS alone group.
The in-hospital fatality rate of acute ischemic stroke patients with AF was 25 per 100, while those without AF were 8.7 per 100. The incidence rate of mortality for acute ischemic stroke with atrial fibrillation was 38 per 1000 person-day. For survival analysis, all patients that met inclusion criteria and patients who had started in-hospital treatment were included in the analysis. The in-hospital survival rate was 30.2% with a mean survival time was 12.75 days (95% CI: 11.241 −14.268). The estimated cumulative survival rate of AIS-with AF patients at the 1st, 7th, 10th, 14th, and 15th days was 93.1%, 75.4%, 66.9%, 54.4%, and 45.3%, respectively. The probability of survival was highest on the first day of admission, but it was shortened as follow-up time increased. On the other hand, the incidence rate of mortality for acute ischemic stroke without atrial fibrillation was 17 per 1000 person-day. The in-hospital survival rate was 52.8% with a mean survival time was 15 days (95% CI: 13.523 −16.59). Kaplan–Meier analysis with the Log rank test evaluated in-hospital survival rate for patients with AF compared to patients without AF, which was significantly different (P=0.011 Figure 2). The median follow-up time for this cohort was 5.49 (±3.575) days, which ranged from 1 day to a maximum of 19 days.
As documented on the death certificate, the most prevalent causes of death in the AF group were respiratory failure related to aspirational pneumonia (9), AF itself (4), brain herniation (3), hemorrhagic transformation (2), multiorgan failure (2), and cardiogenic shock (2). Among these, there were eight neurological causes of death in the AF group, compared to five in the without AF group, and non-neurological causes of death were also higher in the AF group (Supplementary Material).
Predictors of in Hospital Mortality
A bivariate Cox regression analysis was performed to assess the predictors of in-hospital mortality. Variables that were significant at p <0.2 level in the bivariate cox regression model were the presence of AF, cardiovascular diseases such as DCMP, chronic liver disease, HIV/AIDS, stroke-related complications such as aspirational pneumonia, acute renal failure, hypokalemia, and hemorrhagic transformation, comorbidities such as hyperlipidemic status during admission, and hypertension status of the patient associated with in-hospital mortality, and they were candidates for multivariable cox regression (Table 6).
Accordingly, a multivariable cox-regression analysis found that Glasgow Coma Scale (GCS) less than 8 ie, severe brain injury (unconscious) during hospital admission increased the hazard of death by 12.6 times (AHR=12.69, 95% CI: 2.603–61.873) compared to patients who had GCS of 9–12. Besides, those Patients with chronic liver disease during hospitalization had a nearly fivefold higher risk of in-hospital mortality (AHR=4.969, 95% CI: 1.192–20.704). Similarly, the presence of comorbid HIV/AIDS increased the hazard of death by 8.302 times (AHR=8.302, 95% CI: 1.585, 43.502). In addition, patients who acquired Stroke-related complications of aspirational pneumonia during hospitalization or hospital stay had 2.6 times higher risk of in-hospital mortality (AHR=2.602, 95% CI: 1.085–6.242). In addition, patients who developed Acute Renal Failure during hospitalization or hospital stay were 6.114 times more likely to die during the hospital stay (AHR=6.114, 95% CI: 1.817, 20.576), whereas patients who developed Hypokalemia during hospitalization or hospital stay by 17.9% increased the hazard of in-hospital mortality (AHR=1.179, 95% CI: 1.112, 3.373). Moreover, the presence of atrial fibrillation during hospitalization or hospital stays increased hospital mortality by 10.4% (AHR=1.104, 95% CI: 1.015, 5.404).
Discussion
This study assesses clinical characteristics, survival, and predictors of mortality of patients with AIS and AF. In this study, clinical characteristics such as GCS of less than 8, comorbidity with any type of valvular heart disease, coronary heart disease, and in-hospital stroke-related complications were higher in patients suffering from acute ischemic stroke and atrial fibrillation.
The current study found that mortality from AIS plus AF was approximately three times higher than that of the acute ischemic stroke alone group at hospital discharge (25.5% versus 8.7%, p<0.001). The incidence rate of mortality for acute ischemic stroke plus AF was 38 per 1000 person-days. In contrast, the mortality rate for acute ischemic stroke without AF was 17 per 1000 person-days. There were also statistically significant differences in median survival time between patients with acute ischemic stroke plus AF and acute ischemic stroke alone (P=0.011). The Cox regression analysis showed that Glasgow Coma Scale (GCS) less than 8, aspirational pneumonia, hypokalemia, Acute Renal Failure, HIV/AIDS, chronic liver disease, and Atrial Fibrillation were independent predictors of in-hospital death.
This study found that 26.9% AIS patients were diagnosed with AF. These results indicate that the frequency of AF in patients with AIS is higher in the study area than studies conducted in China, Bangladesh, and Malaysia, where AF was found in 20.3%, 17.6%, and 6.5% of study participants, respectively.31–33 This difference may be explained in part by differences in patient background and ethnicity and due to differences in the study area. Of 102 acute ischemic strokes with AF patients, 52.9% were female patients, while 47.1%, were male patients. A Multicenter Multinational Hospital–A-based study in Europe has also reported 57.9% females.34 However, in contrast to our finding, Mallick et al31 reported male predominance. Furthermore, the current study revealed that patients with AF were older at the time of stroke onset, with a mean age at stroke onset of (65.75 years ±16.4 years vs 63 years ±13.58 years). The findings were consistent with those of previous studies conducted in Cameroon,17 and Bangladesh,31 but the Multicenter Multinational Hospital-Based Registry in the European community34 revealed a somewhat higher mean age at a stroke on set (77.3 years ±9.6 years vs 70.6 years ±12.9 years). The disparity could be explained by differences in sample size, research area, and age disparities in the studied population.
Clinical Characteristics
In this study, the clinical characteristics of each patient at hospital admission and throughout their hospitalization were assessed. Regarding stroke severity at the time of hospitalization, despite, the NHISS was proven to be more accurate than GCS in assessing stroke severity,35 GCS was the only functional stroke severity assessment scale utilized by physicians in our study area. Hence, the current study found that severe stroke with GCS less than 8 was significantly higher with a patient in the AF group (83.3% vs 4%, p<0.001). The findings were consistent with those of studies by Sen Lin et al9 and Niamh et al,36 who revealed that severe stroke was linked to the atrial fibrillation group, and they reported stroke severity with higher median NIHSS score at the time of hospital admission (10 vs 4, p<0.001) and (6 vs 4, p=0.008), respectively.
The present study shows that 58 (56.9%) AIS patients with AF suffered from valvular atrial fibrillation (VAF) due to the presence of valvular heart disease (CRVHD, prosthetic heart valve, mechanical heart valve), while (43.1%) of patients in this group suffered from non-valvular atrial fibrillation, which is significantly higher than the study conducted in Italy after the incidence of acute ischemic stroke. The study demonstrated that VAF was reported only in 7% of acute ischemic stroke patients.8 Furthermore, research conducted in Spain found that atrial fibrillation, which is primarily associated with rheumatic mitral valve disease, was responsible for 21.9% of cardiac causes of embolic stroke.37 This difference may be explained due to the high incidence of rheumatic heart disease in most developing countries including Ethiopia.
Moreover, the study revealed that compared to patients without AF, patients with AF were a higher proportion, coronary heart disease, and with a lower frequency of hypertension, and hyperlipidemia (LDL ≥100 mg/dl). This finding is supported by Niamh et al36 and Lin et al.9
The current study also showed that patients with AF are more likely to have stroke-related complications like acute renal failure (22.5% vs 3.3%), hypokalemia (18.6% vs 10.1%), aspirational pneumonia (42.2% vs 28.7%), and hemorrhagic transformation (11.8% vs 4.3%). This finding was in line with the Austrian Stroke Registry,38 and Lin et al9 showed that there was an association between the development of complications and acute ischemic stroke with atrial fibrillation patients.
Mortality and Its Predictors
The study found that overall in-hospital mortality rate of AIS was 13.22%. In-hospital mortality rates of AIS patients with AF were higher. The incidence rate of mortality for acute ischemic stroke with atrial fibrillation was 38 per 1000 person-day. The in-hospital survival rate was 30.2% with a mean survival time of 12.75 days (95% CI: 11.241 −14.268). On the other hand, the incidence rate of mortality for AIS without AF was 17 per 1000 person-day. The in-hospital survival rate was 52.8% with a mean survival time of 15 days (95% CI: 13.523 −16.59). The case fatality of AIS with the AF group was approximately 3 times higher than without the AF group (25.5% vs 8.7%, p<0.001). These results fall in line with results of two previous studies, Ritu et al39 and Kannikar et al40 report high case fatality in the AF group (17% vs 8%) and (14.1% vs 6.2%), respectively. Even though we assess in-hospital mortality rate with the median (IQR) follow-up day of 5.49 days, the mortality rate of AIS with AF in the study area is higher than that of the 28-day mortality rates study in Japanese15 AIS patients with and without AF (11.3% vs 3.4%; p < 0.001) and 30-day mortality rate in Canadian perspective registry of 12,686 AIS patients with AFs (22.3% vs 10.2%; p<0.001).41 The possible reasons may be due to the AF group having high hospital stroke-related complications, as well as a higher mean age, differences in study design, sample size, AIS care in health system and stroke severity.
In the current study, patients who had a GCS of less than 8 during hospital admission was a predictor of in-hospital mortality, which increased the hazard of death by 12.6 times (AHR=12.69, 95% CI: 2.603–61.873; p<0.002). This finding is supported by studies conducted by Mittal et al42, Shah et al43 and Bhatia et al44 reported GCS score of <8 as a predictor of mortality.
This study identified aspirational pneumonia as another predictor of mortality. Patients who acquired aspirational pneumonia during a hospital stay had 2.6 times increased chance of in-hospital mortality (AHR=2.602, 95% CI: 1.085–6.242; p=0.032). A consistent finding was reported from Thailand40 showing Aspirational pneumonia (AOR=2.60, 95% CI: 2.38–2.84) were independent predictors of in-hospital mortality. Similar studies in the Netherlands45 and Taiwan46 found that a day of pneumonia following an acute ischemic stroke was a significant predictor of mortality or poor outcome at discharge.
In the current study, patients who developed Stroke-related complications of acute renal failure during their hospital stay were 6.114 times more likely to quickly dying (AHR=6.114, 95% CI: 1.817, 20.576; p=0.003) as compared with those of patients who do not develop ARF during the hospital stay. This finding is supported by studies conducted by Fahad et al,47 where acute kidney failure was an independent predictor of in-hospital mortality (AOR=2.2, 95% CI: 2–2.2; P<0.0001). Similarly, Khatri et al48 also reported that acute renal failure was associated with increased in-hospital mortality in a patient with acute ischemic stroke (AOR=3.08, 95%1.49–6.35; P<0.0001). The similarity could be explained by the fact that acute ischemic stroke patients are at risk of acute kidney failure due to volume depletion, contrast exposure, and pre-existing comorbid diseases. Physiologic imbalances and altered metabolism related to ARF include increased inflammation and oxidative stress, which could both hypothetically worsen outcomes.49,50
Studies show that hypokalemia is a common electrolyte abnormality and complication encountered in hospitalized patients.51 In the present study, patients who had hypokalemia during their hospital stay increased the hazard of in-hospital mortality by 17.9% (AHR=1.179, 95% CI: 1.112, 3.373; p=0.013). Consistent with the present study, the study by Gariballa and his colleagues52 reports that lower plasma potassium on admission to the hospital increased chance of in-hospital death, by 73% (AHR 1.73, 95% CI: 1.03 − 2.9). Similarly, Fan et al51 also report that Hypokalemia was associated with poor outcomes (AOR=2.42, 95% Cl=1.21–4.86, P=0.013).
The current study found that patients with HIV/AIDS comorbidity increased their risk of in-hospital mortality by 8.302 times (AHR=8.302, 95% CI: 1.585, 43.502; p=0.012). This finding is consistent with research conducted in Thailand, which found that HIV/AIDS was linked with a greater risk of in-hospital mortality (AOD=4.12; 95% CI: 196–866; P=0.001).53 This may be because HIV infection increased the chance of getting an infection while in acute hospitalization and was associated with higher inpatient mortality.
This study also revealed that patients with chronic liver disease during hospitalization had a nearly fivefold higher risk of in-hospital mortality (AHR=4.969, 95% CI: 1.192–20.704; p=0.028) than those without a chronic liver disease concomitant condition. Similar to our findings, a study conducted in America54 showed that liver impairment was highly linked with in-hospital fatality in a patient with acute ischemic stroke (AOD=1.60; 95% CI: 1.51–1.71; P 0.001). This may be in part explain potential interactions between chronic liver disease and stroke therapy that may impact the prescription of some drugs.54
There are several strategies used to maintain sinus rhythm after an acute ischemic stroke with different cardiovascular comorbidities. The study compares two treatment strategies for patients with AF in heart failure: medical therapy and catheter ablation (CA), emphasizing the importance of CA in terms of a lower risk of all-cause mortality.55 In another study, which compared treatment techniques of rate control and rhythm control in NVAF patients, no difference in fatality rates was reported.56 Furthermore, studies have shown that Artificial Intelligence (AI) algorithms can assist health-care professionals in selecting the most effective AF treatment helping determine the best treatment strategy and helping to improve the treatment outcome.57
In this study, the only treatments prescribed to maintain sinus rhythm in a patient with AF and AIS were rate controllers. The results of this study also showed that AF was a predictor of in-hospital fatalities. However, AF was not the only significant independent predictor of death. When AF was present, hospital mortality increased by 10.4% (AHR=1.104, 95% CI: 1.015, 5.404; p=0.003) which was a substantial increase. This finding is consistent with study by Kimura et al15 according to this study AF was linked to a higher risk of hospital mortality (AOR=1.27, 95% CI, 1.06–1.51; P=0.0001). Similarly, Thygesen and his colleagues58 also reported that AF raised the possibility of death within a month by 1.55 (AHR=1.55, 95% CI: 1.20–2.01; p=0.013).
Limitations
This study was not without limitations. Short-term follow-up, the study only kept track of in-hospital outcomes, which is one limitation of the study. Because this was a retrospective study, it may not be possible to trace all the necessary information from the patient chart such as inadequate echocardiographic examinations documented in the record. Besides, the small sample size due to the limited number of admissions may potentially have an impact on the study’s statistical strength. The effect of some potential predictors of mortality, such as acute ischemic stroke etiology, and atrial fibrillation subtype were not properly documented in the patient’s medical file, and thus they were completely excluded from the analysis.
Conclusion
In this study, clinical characteristics such as GCS of less than 8, comorbidity with any type of valvular heart disease, coronary heart disease, and in-hospital stroke-related complications were higher in patients with acute ischemic stroke and atrial fibrillation. In-hospital mortality rate for acute ischemic stroke associated with atrial fibrillation was particularly higher than patients without atrial fibrillation and had a reduced chance of survival during hospital stay. Despite the significant mortality rate among acute ischemic stroke with atrial fibrillation patients, atrial fibrillation was not demonstrated to be a strong independent predictor of death, stroke-related complications, aspirational pneumonia, acute renal failure hypokalemia, and atrial fibrillation were found to be independent predictors for in-hospital mortality. Hence, effective strategies should be in place to curb the impacts of these factors. Since this study was conducted in a small number of hospitals, further prospective, nationwide, studies are needed. We also suggest that future studies examine the impact of some potential predictors of mortality, including the etiology of acute ischemic stroke and atrial fibrillation subtype.
Ethical Considerations
The study was approved by the Ethics Review Committee of the School of Pharmacy, Addis Ababa University through a letter reference number of ERB/SOP/489/15/2022. The consent was waived due to the retrospective nature of the study. The confidentiality of the study participants was maintained by not disclosing their identification details and by using anonymized data. The study was conducted in full compliance with the principles of the “Declaration of Helsinki” Good Clinical Practice (GCP).
Acknowledgments
The authors thank the data collectors and all staff members of the study settings for their valuable contributions. We would also like to thank Addis Ababa University for providing this opportunity to conduct this research. This paper is based on the thesis of Zenaw Debasu Addisu. It has been published on the institutional website: http://www.aau.edu.et/wp-content/uploads/2023/07/AAU-Prospective-Graduate-2023-2.pdf.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. The Top 10 Causes of Death. World Health Organization; 2020.
2. Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6(2):182–187. doi:10.1016/S1474-4422(07)70031-5
3. Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ. 1976;54(5):541–553.
4. Tripathi M, Vibha D. Stroke in young in India. Stroke Res Treat. 2011;2011:1.
5. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi:10.1161/CIR.0000000000000152
6. Godoy DA, Piñero GR, Koller P, et al. Steps to consider in the approach and management of critically ill patient with spontaneous intracerebral hemorrhage. World J Crit Care Med. 2015;4(3):213. doi:10.5492/wjccm.v4.i3.213
7. Topcuoglu MA, Liu L, Kim D-E, et al. Updates on prevention of cardioembolic strokes. J Stroke. 2018;20(2):180. doi:10.5853/jos.2018.00780
8. Marini C, De Santis F, Sacco S, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke. 2005;36(6):1115–1119. doi:10.1161/01.STR.0000166053.83476.4a
9. Lin S, Wu B, Hao Z-L, et al. Characteristics, treatment and outcome of ischemic stroke with atrial fibrillation in a Chinese hospital-based stroke study. Cerebrovascular Dis. 2011;31(5):419–426. doi:10.1159/000323221
10. Markides V, Schilling RJ. Atrial fibrillation: classification, pathophysiology, mechanisms and drug treatment. Heart. 2003;89(8):939–943. doi:10.1136/heart.89.8.939
11. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. doi:10.1161/STR.0b013e318284056a
12. Diringer MN, Edwards DF, Mattson DT, et al. Predictors of acute hospital costs for treatment of ischemic stroke in an academic center. Stroke. 1999;30(4):724–728. doi:10.1161/01.STR.30.4.724
13. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham study. stroke. 1991;22(8):983–988. doi:10.1161/01.STR.22.8.983
14. Jørgensen HS, Nakayama H, Reith J, et al. Acute stroke with atrial fibrillation: the Copenhagen stroke study. Stroke. 1996;27(10):1765–1769. doi:10.1161/01.STR.27.10.1765
15. Kimura K, Minematsu K, Yamaguchi T. Atrial fibrillation as a predictive factor for severe stroke and early death in 15 831 patients with acute ischaemic stroke. J Neurol Neurosurg. 2005;76(5):679–683. doi:10.1136/jnnp.2004.048827
16. Arboix A, Garcı́a-Eroles L, Massons JB, et al. Atrial fibrillation and stroke: clinical presentation of cardioembolic versus atherothrombotic infarction. Int J Cardiol. 2000;73(1):33–42. doi:10.1016/S0167-5273(99)00214-4
17. Ntep-Gweth M, Zimmermann M, Meiltz A, et al. Atrial fibrillation in Africa: clinical characteristics, prognosis, and adherence to guidelines in Cameroon. Europace. 2010;12(4):482–487. doi:10.1093/europace/euq006
18. Connor MD, Walker R, Modi G, et al. Burden of stroke in black populations in sub-Saharan Africa. Lancet Neurol. 2007;6(3):269–278. doi:10.1016/S1474-4422(07)70002-9
19. Misganaw A, Haregu TN, Deribe K, et al. National mortality burden due to communicable, non-communicable, and other diseases in Ethiopia, 1990–2015: findings from the global burden of disease study 2015. Popul Health Metr. 2017;15:29. doi:10.1186/s12963-017-0145-1
20. Owolabi MO, Sarfo F, Akinyemi R, et al. Dominant modifiable risk factors for stroke in Ghana and Nigeria (SIREN): a case-control study. Lancet Glob Health. 2018;6(4):e436–e446. doi:10.1016/S2214-109X(18)30002-0
21. Lemogoum D, Degaute J-P, Bovet P. Stroke prevention, treatment, and rehabilitation in sub-saharan Africa. Am J Preventive Med. 2005;29(5):95–101. doi:10.1016/j.amepre.2005.07.025
22. Gebremariam SA, Yang HS. Types, risk profiles, and outcomes of stroke patients in a tertiary teaching hospital in northern Ethiopia. E Neurological Sci. 2016;3:41–47.
23. Fekadu G. Current challenges and strategies in management and prevention of stroke. J Neurol Stroke. 2019;9:149–153. doi:10.15406/jnsk.2019.09.00366
24. Brüggenjürgen B, Rossnagel K, Roll S, et al. The impact of atrial fibrillation on the cost of stroke: the Berlin acute stroke study. Value Health. 2007;10(2):137–143. doi:10.1111/j.1524-4733.2006.00160.x
25. Greffie ES, Mitiku T, Getahun S. Risk factors, clinical pattern and outcome of stroke in a referral hospital, Northwest Ethiopia. Clin Med Res. 2015;4(6):182–188. doi:10.11648/j.cmr.20150406.13
26. Beyene D, Asefa H. A two year retrospective cross-sectional study on prevalence, associated factors and treatment outcome among patients admitted to medical ward (stroke unit) at Jimma University Medical Center, Jimma, South West, Ethiopia, 2018. Palliat Med Care. 2018;5(4):1–6.
27. Greffie ES, Mitiku T, Getahun S. High prevalence of atrial fibrillation in stroke patients admitted to university of Gondar hospital, Northwest Ethiopia. Ethiop Med J. 2016;54(4):207–212.
28. Wu C-S, Chen P-H, Chang S-H, et al. Atrial fibrillation is not an independent determinant of mortality among critically Ill acute ischemic stroke patients: a propensity score-matched analysis from the MIMIC-IV database. Front Neurol. 2022;12:2609. doi:10.3389/fneur.2021.730244
29. Allen LM, Hasso AN, Handwerker J, et al. Sequence-specific MR imaging findings that are useful in dating ischemic stroke. Radiographics. 2012;32(5):1285–1297. doi:10.1148/rg.325115760
30. Temesgen TG, Teshome B, Njogu P. Treatment outcomes and associated factors among hospitalized stroke patients at Shashemene Referral Hospital, Ethiopia. Stroke Res Treat. 2018;2018:1.
31. Mallick AK, Ali MA, Kafiluddin M, et al. Study on outcome of ischemic stroke patient with atrial fibrillation. KYAMC J. 2018;8(2):8–12. doi:10.3329/kyamcj.v8i2.35696
32. Dulli DA, Stanko H, Levine RL. Atrial fibrillation is associated with severe acute ischemic stroke. Neuroepidemiology. 2003;22(2):118–123. doi:10.1159/000068743
33. Aziz Z, Sidek NN, Ngah BA, et al. Clinical characteristics of atrial fibrillation in first-ever ischemic stroke patients; results from Malaysia national neurology registry. Int J Cardiovasc Res. 2016;8602:2.
34. Lamassa M, Di Carlo A, Pracucci G, et al. Characteristics, outcome, and care of stroke associated with atrial fibrillation in Europe: data from a multicenter multinational hospital-based registry (The European Community Stroke Project). Stroke. 2001;32(2):392–398. doi:10.1161/01.STR.32.2.392
35. Mansour OY, Megahed MM, Abd Elghany EHS. Acute ischemic stroke prognostication, comparison between Glasgow Coma Score, NIHS Scale and Full Outline of UnResponsiveness Score in intensive care unit. Alexand J Med. 2015;51(3):247–253. doi:10.1016/j.ajme.2014.10.002
36. Hannon N, Sheehan O, Kelly L, et al. Stroke associated with atrial fibrillation–incidence and early outcomes in the north Dublin population stroke study. Cerebrovascular Dis. 2010;29(1):43–49. doi:10.1159/000255973
37. Capmany RP, Arboix A, Casañas-Muñoz R, et al. Specific cardiac disorders in 402 consecutive patients with ischaemic cardioembolic stroke. Int J Cardiol. 2004;95(2–3):129–134. doi:10.1016/j.ijcard.2003.02.007
38. Steger C, Pratter A, Martinekbregel M, et al. Stroke patients with atrial fibrillation have a worse prognosis than patients without: data from the Austrian Stroke registry. Eur Heart J. 2004;25(19):1734–1740. doi:10.1016/j.ehj.2004.06.030
39. Saxena R, Lewis S, Berge E, et al. Risk of early death and recurrent stroke and effect of heparin in 3169 patients with acute ischemic stroke and atrial fibrillation in the International Stroke Trial. Stroke. 2001;32(10):2333–2337. doi:10.1161/hs1001.097093
40. Kongbunkiat K, Kasemsap N, Travanichakul S, et al. Hospital mortality from atrial fibrillation associated with ischemic stroke: a national data report. Int J Neurosci. 2015;125(12):924–928. doi:10.3109/00207454.2014.986266
41. Saposnik G, Gladstone D, Raptis R, et al. Atrial fibrillation in ischemic stroke: predicting response to thrombolysis and clinical outcomes. Stroke. 2013;44(1):99–104. doi:10.1161/STROKEAHA.112.676551
42. Mittal SH, Goel D, Govil T, et al. Identification of mortality-related predictive factors in hospitalized patients with ischemic stroke. Astrocyte. 2015;1(4):272. doi:10.4103/2349-0977.161613
43. Shah B, Bartaula B, Adhikari J, et al. Predictors of in-hospital mortality of acute ischemic stroke in adult population. J Neurosci Rural Pract. 2017;8(04):591–594. doi:10.4103/jnrp.jnrp_265_17
44. Bhatia R, Garg RK, Gaur SPS, et al. Predictive value of routine hematological and biochemical parameters on 30-day fatality in acute stroke. Neurol India. 2004;52(2):220.
45. Vermeij FH, Scholte op Reimer WJM, de Man P, et al. Stroke-associated infection is an independent risk factor for poor outcome after acute ischemic stroke: data from the Netherlands Stroke Survey. Cerebrovasc Dis. 2009;27(5):465–471. doi:10.1159/000210093
46. Chen LF, Chang C-Y, Hsu L-C, et al. Bacterial pneumonia following acute ischemic stroke. J Chin Med Assoc. 2013;76(2):78–82. doi:10.1016/j.jcma.2012.10.005
47. Saeed F, Adil MM, Khursheed F, et al. Acute renal failure is associated with higher death and disability in patients with acute ischemic stroke: analysis of nationwide inpatient sample. Stroke. 2014;45(5):1478–1480. doi:10.1161/STROKEAHA.114.004672
48. Khatri M, Himmelfarb J, Adams D, et al. Acute kidney injury is associated with increased hospital mortality after stroke. J Stroke Cerebrovascular Dis. 2014;23(1):25–30. doi:10.1016/j.jstrokecerebrovasdis.2012.06.005
49. Himmelfarb J, McMonagle E, Freedman S, et al. Oxidative stress is increased in critically ill patients with acute renal failure. J Am Soc Nephrol. 2004;15(9):2449–2456. doi:10.1097/01.ASN.0000138232.68452.3B
50. Heuschmann PU, Kolominsky-Rabas PL, Misselwitz B, et al. Predictors of in-hospital mortality and attributable risks of death after ischemic stroke: the German stroke registers study group. Arch Inter Med. 2004;164(16):1761–1768. doi:10.1001/archinte.164.16.1761
51. Gao F, Wang CT, Chen C, et al. Effect of hypokalemia on functional outcome at 3 months post-stroke among first-ever acute ischemic stroke patients. Med Sci Monit Int Med J Clin Res. 2017;23:2825.
52. Gariballa SE, Robinson TG, Fotherby MD. Hypokalemia and potassium excretion in stroke patients. J Am Geriatr Soc. 1997;45(12):1454–1458. doi:10.1111/j.1532-5415.1997.tb03195.x
53. Cumming K, Tiamkao S, Kongbunkiat K, et al. Impact of HIV on inpatient mortality and complications in stroke in Thailand: a National Database Study. Epidemiol Infect. 2017;145(6):1285–1291. doi:10.1017/S095026881600340X
54. Parikh NS, Merkler AE, Schneider Y, et al. Discharge disposition after stroke in patients with liver disease. Stroke. 2017;48(2):476–478. doi:10.1161/STROKEAHA.116.016016
55. Şaylık F, Çınar T, Akbulut T, et al. Comparison of catheter ablation and medical therapy for atrial fibrillation in heart failure patients: a meta-analysis of randomized controlled trials. Heart Lung. 2023;57:69–74. doi:10.1016/j.hrtlng.2022.08.012
56. Kılıç R, Güzel T, Aktan A, et al. The effect of treatment strategy on long-term follow-up results in patients with nonvalvular atrial fibrillation in Turkey: AFTER-2 subgroup analysis. Aging Clin Exp Res. 2023;35(8):1695–1704. doi:10.1007/s40520-023-02467-y
57. Hayıroğlu Mİ, Altay S. The role of artificial intelligence in coronary artery disease and atrial fibrillation. Balkan Med J. 2023;40(3):151. doi:10.4274/balkanmedj.galenos.2023.06042023
58. Thygesen SK, Frost J, Eagle KA, et al. Atrial fibrillation in patients with ischemic stroke: a population-based study. Clin Epidemiol. 2009;1:55. doi:10.2147/CLEP.S4794
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

