Back to Journals » Journal of Blood Medicine » Volume 14
Correlation Between Hypercoagulable State and Severity Level of Ischemic Stroke With Covid-19 Infection
Authors Amalia L
Received 4 August 2023
Accepted for publication 6 October 2023
Published 11 October 2023 Volume 2023:14 Pages 537—542
DOI https://doi.org/10.2147/JBM.S429357
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Lisda Amalia
Department of Neurology, Medical Faculty, Universitas Padjadjaran, Bandung, Indonesia
Correspondence: Lisda Amalia, Department of Neurology, Medical Faculty, Universitas Padjadjaran, Jl. Eykman 38, Bandung, 40161, Indonesia, Email [email protected]
Background: Hypercoagulable state in acute ischemic stroke patients with COVID-19, was found to occur in most cases, may affect the severity and clinical outcome of acute ischemic stroke with COVID-19. Ischemic stroke patients with COVID-19 infection have worsen prognosis in mortality regarding hypercoagulable state condition.
Objective: The study aims to determine the relationship between the hypercoagulable state and the severity of acute ischemic stroke patients with COVID-19.
Methods: This study is a retrospective analytic study using a cross-sectional method in acute ischemic stroke who meet the criteria must have focal clinical symptoms or global dysfunction lasting more than 24 hours, be caused by vascular factors, be confirmed positive for COVID-19, NIHSS (admission and discharge), and have an examination of D-dimer and/or fibrinogen. Chi-Square is used for data processing relationship analysis.
Results: A total of 32 patients met the inclusion and exclusion criteria of this study. Elevated D-dimer and/or fibrinogen were found in 28 patients (87.5%), confirming a hypercoagulable state. In this study, the average value of D-dimer was 5.3 mg/mL, and fibrinogen was 479 mg/dL. Based on the admission NIHSS score, it was found that most of the patients had moderate strokes with an average NIHSS score of 12. The chi-square test results showed no relationship between the hypercoagulable state and the severity of acute ischemic stroke as measured by NIHSS admission (p=0.333), but it was closely related to NIHSS exit (p=0.02). The finding supports that 40.62% of acute ischemic stroke patients with COVID-19 confirmed to have a hypercoagulable state had a death discharge status.
Conclusion: There is no significant relationship between hypercoagulable state and stroke severity on admission, but it closely related to NIHSS on discharge and high mortality in acute ischemic stroke patients with COVID-19.
Keywords: hypercoagulable state, acute ischemic stroke, degree of severity, NIHSS
Introduction
Stroke is defined by the World Health Organization (WHO) as a sudden decline in focal or global neurological function that develops rapidly and lasts more than 24 hours or causes death caused by vascular disorders. Stroke is the biggest cause of death and disability in the world. Based on data from the World Stroke Organization (WSO) for 2022, more than 12 million new stroke events occur yearly, with a death rate of 6.5 million.1 After entering the COVID-19 pandemic, it was found that stroke accounts for 1–6% of all complications occurs due to infection with COVID-19. Acute ischemic stroke, which is defined as a decrease in blood supply to the brain and causes neurological deficits, is the most common cerebrovascular complication (CVD) in COVID-19 patients.2 Increased coagulation factors were found in acute ischemic stroke patients with COVID-19, indicating a relationship between hypercoagulable states due to COVID infection -19 with acute ischemic stroke and also influence for improving clinical outcome.3
Differences in characteristics of stroke patients with and without Covid-19, among others, stroke patients with COVID-19 showed more large vessel occlusion (LVO) (17.9% Covid-19, 8.1% non-Covid-19), experienced a degree more severe stroke according to NIHSS (score 8 Covid-19, score 5 non-Covid-19), higher D-dimer value, higher degree of disability (Rankin score) (score 4 Covid-19, score 3 non-Covid-19), and higher mortality (19.8% Covid-19, 6.9% non-Covid-19).4
The National Institute of Health Stroke Scale (NIHSS) is a tool to qualitatively and systematically measure the severity of stroke by measuring neurological functions, including levels of consciousness, sensory response, motor movements, speech and communication skills, and attention. A high NIHSS score indicates worse neurological decline. In acute ischemic stroke patients with COVID-19, the NIHSS score was found to be higher compared to acute ischemic stroke patients without COVID-19.3,5 This study aims to determine the relationship between hypercoagulable conditions and the degree of severity in acute ischemic stroke patients with COVID-19.
Methods
The subjects of this study were obtained from the medical records of patients treated at the Department of Neurology at Dr. Central General Hospital. Hasan Sadikin Bandung in the period March 2020 – December 2022. These patients must have focal clinical symptoms or global dysfunction lasting more than 24 hours and caused by vascular factors. COVID-19 infection status was confirmed positive using a Real-Time Polymerase Chain Reaction (RT-PCR) test. The hypercoagulable state is determined by increased D-dimer values (normal values ≤0.55 mg/mL) or increased fibrinogen levels (normal values 238–498 mg/dL). Impaired neurological function was assessed using the National Institute of Health Stroke Scale (NIHSS). NIHSS scores are classified into four categories: mild stroke (1–4), moderate stroke (5–15), moderate stroke (16–20), and severe stroke (21–42). The Trial of Organization 10,172 in Acute Stroke Treatment (TOAST) classification is used to determine the causes and mechanisms of stroke, namely large-artery atherosclerosis (LAA), cardioembolism (CE), small-vessel occlusion (SVO), stroke of other determined etiology, and stroke of undetermined etiology. Patient demographic information, risk factors, and clinical outcomes were recorded. Subjects excluded were patients with hemorrhagic stroke, patients without NIHSS scores on admission, and patients with poor medical records. Sampling using the total sampling method. Chi-Square is used for data processing relationship analysis.
Subjects who met the inclusion criteria expressed their willingness to participate in this study by signing informed consent after obtaining an explanation. The ethics committee of Universitas Padjadjaran Bandung received the research ethics approval under the ethical clearance number 612/UN6.KEP/EC/2023 and complies with the Declaration of Helsinki. Writing informed consent was obtained from the study participants.
Result
Of the 545 acute ischemic stroke patients treated at Dr. Hasan Sadikin Bandung during the vulnerable period of March 2020 – December 2022, 32 patients were declared to have met the research criteria. Most patients were women, over 55, and had moderate strokes (NIHSS mean=12). Hypertension is the biggest risk factor (78.1%), followed by dyslipidemia (46.9%) and heart disease (40.6%). Table 1 shows the characteristic distribution of acute ischemic stroke patients with COVID-19.
 |
Table 1 Characteristics of Research Subjects |
The hypercoagulable state was confirmed in 28 patients (87.5%). Increased D-dimer was found in 83.87%, while increased fibrinogen was found in 38.46%. The average D-dimer and fibrinogen values were 5.3 mg/mL and 479 mg/dL. 81.25% of patients had strokes of other determined etiology based on the TOAST classification. The average NIHSS admission score with hypercoagulable conditions was 13.32 (moderate stroke), while patients without hypercoagulable conditions were 7.5 (moderate stroke). There were 40.62% of patients were discharged dead. Most had higher NIHSS admission scores and were confirmed to be hypercoagulable. Table 2 shows the relationship between the hypercoagulable state and the severity of acute ischemic stroke with COVID-19.
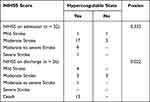 |
Table 2 Correlation Between Hypercoagulable State with NIHSS |
Based on the chi-square test, we found no relationship between the hypercoagulable state and the severity of acute ischemic stroke in COVID-19 patients at admission (p=0.333). It was found that the hypercoagulable state was associated with the severity of acute ischemic stroke using NIHSS on discharge. (p=0.02).
Discussion
Coagulopathy is one of the clinical manifestations of severe Coronavirus Disease of 2019 (Covid-19), and causes a poor prognosis of the disease. Covid-19 patients experience a severe inflammatory state that causes an increase in the activation of the coagulation cascade, an increase in thrombin, and a hypercoagulable state, thereby increasing the risk of thrombosis in the blood vessels of the brain and spinal cord. Acute ischemic stroke accounts for 1–6% of all complications due to COVID-19.2,6,7 Although there are several reports of strokes in young COVID-19 patients, we found that the average age of acute ischemic stroke patients with COVID-19 is 61.6, and the most common risk factor was hypertension (78.1%). This is consistent with research by Hidayat et al and Luo et al, who reported 69% and 66% yields, respectively.8,9
Based on the TOAST classification, most of our subjects had strokes of other determined etiology (81.25%). Luo et al reported consistent results, namely cryptogenic stroke in 35% of acute ischemic stroke patients with COVID-19. This is consistent with a study by Yaghi et al, who found that stroke patients with COVID-19 were more likely to experience cryptogenic strokes, suggesting a specific mechanism for developing acute ischemic stroke in patients with COVID-19.3,8
The most frequently suggested mechanism of acute ischemic stroke in COVID-19 patients is a hypercoagulable state due to the coagulation cascade caused by the immune response to COVID-19 infection.3 In line with other studies, hypercoagulable state was also confirmed in most of our patients (87.5%). An increase in D-dimer which was considered a consistent laboratory finding in COVID-19 patients was confirmed in 83.87% while an increase in fibrinogen was found in 38.46%.10 This is supported by research by Hidayat et al who reported an increase in D-dimer in 98.1% of stroke patients at the University of Indonesia Hospital.11
In our study, the mean and median D-dimer were 5.36 mg/mL and 2.36 mg/mL, respectively, well above the normal value of 0.55 mg/mL. Yaghi et al in a New York study found similar results, confirming D-dimer with a median of 3.91 mg/mL in acute ischemic stroke patients with COVID-19.3 In Spain, Fàbregas found slightly lower results (median: 1.76 mg/mL).9 Based on several previous studies, increased D-dimer is associated with higher mortality.12
Based on a systematic review by Tan et al, COVID-19 patients were found to have moderate to severe strokes.13 In this study, the National Institute of Health Stroke Scale was used at admission and most of the subjects had moderate strokes (12.5) which is consistent with findings. Hvaneon’s et al reported a mean NIHSS score of 9.7 and Nannoni et al in their systematic review (median: 5).6,14 Compared with stroke patients without COVID-19, acute ischemic stroke patients with COVID-19 also showed higher NIHSS scores on admission.3,6 This is why we hypothesize that hypercoagulable conditions will affect the severity of acute ischemic stroke in patients with COVID-19.
Based on our study, patients with hypercoagulable states showed a mean NIHSS score on admission of 13.32, while patients without hypercoagulable conditions showed a mean score of 7.5. These findings show a linear relationship between hypercoagulable state and stroke severity on admission. However, we found no significant relationship between the hypercoagulable state and the severity of acute ischemic stroke at admission (p=0.333). We suspect that higher NIHSS scores on admission in acute ischemic stroke patients with COVID-19 in some studies are due to the severity of COVID-19 infection and other patient risk factors. As most patients with higher admission NIHSS scores were found to have cardioembolic strokes, we consider that acute ischemic stroke is exacerbated by the hypercoagulable state resulting from COVID-19 infection, not solely its cause.2
It was previously known that D-dimer above 1 mg/mL on admission was associated with a higher probability of in-hospital death and was a predictor of mortality. In a study by Tang et al, non-survivors showed a D-dimer rate of 2.12 mg/mL, while survivors showed 0.61 mg/m.12 This is consistent with our study finding 8.29 mg/mL in non-survivors and 3.25 mg/mL in survivors. This also shows that acute ischemic stroke patients with hypercoagulable conditions have a higher risk of dying.2,9 The presence of Covid-19 complications such as thrombosis can affect the patient’s prognosis and mortality.7
SARS-CoV-2 infection in several conditions can trigger an exaggerated immune reaction, otherwise known as a cytokine storm, which can activate secondary hemostasis or coagulation cascade. This causes excessive fibrin degradation product (FDG) production, reflected in the increase in D-dimer or fibrinogen in COVID-19 patients, causing a hypercoagulable state. The coagulation cascade will form a thrombus that can travel through the vascular system, increasing the risk of acute ischemic stroke in COVID-19 patients.2,7
The lack of research subjects is the main limitation of this study. D-dimer and fibrinogen tests are not done in many acute ischemic stroke patients, with COVID-19 being the main cause. This study did not consider hypercoagulable conditions due to genetic disorders or causes other than COVID-19. In addition, this study was only conducted at a central general hospital, so it cannot represent other types of hospitals. More in-depth and multicentre studies are needed to determine whether there is a relationship between hypercoagulable states and acute ischemic stroke severity in COVID-19 patients and to determine the relationship between D-dimer and acute ischemic stroke severity on admission.14
Conclusion
There was no significant relationship between the hypercoagulable state and the severity of acute ischemic stroke in COVID-19 patients at admission, but it closely related to NIHSS on discharge and high mortality in acute ischemic stroke patients with COVID-19. The presence of Covid-19 complications such as thrombosis in acute stroke can affect the patient’s prognosis and mortality.
Acknowledgment
The authors would like to thank the Neurology Department of Dr. Hasan Sadikin Bandung General Hospital staff for their contributions to this study.
Disclosure
The author reports no conflicts of interest in this work.
References
1. Feigin VL, Brainin M, Norrving B, et al. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int J Stroke. 2022;17(1):18–29. doi:10.1177/17474930211065917
2. Amalia L. Characteristic of acute ischemic stroke patients based on TOAST classification during COVID-19 pandemic era: a single centre study. Int J Gen Med. 2023;16:581–588. doi:10.2147/IJGM.S394017
3. Yaghi S, Ishida K, Torres J, et al. SARS-CoV-2 and stroke in a New York Healthcare System. Stroke. 2020;51(7):2002–2011. doi:10.1161/STROKEAHA.120.030335
4. Li Y, Li M, Wang M, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. Stroke Vasc Neurol. 2020;5(3):279–284. doi:10.1136/svn-2020-000431
5. Finsterer J, Scorza FA, Scorza CA, Fiorini AC. Ischemic stroke in 455 COVID-19 patients. Clinics. 2022;77:100012. doi:10.1016/j.clinsp.2022.100012
6. Nannoni S, de Groot R, Bell S, Markus HS. Stroke in COVID-19: a systematic review and meta-analysis. In: International Journal of Stroke. Vol. 16. SAGE Publications Inc; 2021:137–149.
7. Amalia L. Kelainan Neurologi akibat Kondisi Hiperkoagulasi pada Pasien Coronavirus Disease-19. JNI. 2023;12(1):58–66. doi:10.24244/jni.v12i1.452
8. Luo W, Liu X, Bao K, Huang C. Ischemic stroke associated with COVID-19: a systematic review and meta-analysis. J Neurol. 2022;269(4):1731–1740. doi:10.1007/s00415-021-10837-7
9. Martí-Fàbregas J, Guisado-Alonso D, Delgado-Mederos R, et al. Impact of COVID-19 infection on the outcome of patients with ischemic stroke. Stroke. 2021;52(12):3908–3917. doi:10.1161/STROKEAHA.121.034883
10. Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID‐19. J Thromb Haemost. 2020;18(5):1023–1026. doi:10.1111/jth.14810
11. Hidayat R, Widjaya N, Djuliannisaa Z, et al. Ischemic stroke in COVID-19 patients: a cross-sectional study from an Indonesian COVID-19 referral hospital. Egypt J Neurol Psychiatr Neurosurg. 2022;58(1):93. doi:10.1186/s41983-022-00528-z
12. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi:10.1111/jth.14768
13. Tan YK, Goh C, Leow AST, et al. COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J Thromb Thrombolysis. 2020;50(3):587–595. doi:10.1007/s11239-020-02228-y
14. de Havenon A, Zhou LW, Yaghi S, Frontera JA, Sheth KN. Effect of COVID-19 on acute ischemic stroke severity and mortality in 2020: results from the 2020 National Inpatient Sample. Stroke. 2023;54(5). doi:10.1161/STROKEAHA.122.041929
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
