Back to Journals » Psychology Research and Behavior Management » Volume 17
Deficiency in Self-Control: Unraveling Psychological and Behavioral Risk Factors for Obsessive-Compulsive Symptoms in College Students
Authors Muhetaer P, Leng J , Hu P
Received 26 December 2023
Accepted for publication 15 March 2024
Published 20 March 2024 Volume 2024:17 Pages 1329—1338
DOI https://doi.org/10.2147/PRBM.S456685
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Mei-Chun Cheung
Palizhati Muhetaer, Jie Leng, Ping Hu
Department of Psychology, Renmin University of China, Beijing, People’s Republic of China
Correspondence: Ping Hu, Email [email protected]
Objective: Obsessive-compulsive disorder (OCD) is a complex mental disorder to treat. However, there are some deficiencies in research performed to date about the psychological and behavioral factors that may trigger obsessive-compulsive symptoms (OCS). Based on the Psychopathology of Self-Control Theory which states that deficits in self-control underpin psychiatric symptoms, this study investigated the factors influencing OCS among college students.
Methods: A total of 5599 non-clinical Chinese college students were recruited to complete the Chinese version of the Self-Control Scale, Aitken Procrastination Inventory, and Symptom Checklist-90. Pearson’s correlation analyses and the bootstrap method were performed to test our hypothesis.
Results: The following results were obtained: (a) There were significant correlations among self-control, procrastination, anxiety, and OCS. (b) When controlling for the effects of age and sex, self-control remained a significant negative predictor of OCS. (c) The mediating roles of procrastination and anxiety, and the chain mediating role of procrastination and anxiety were the three predicted pathways linking self-control and OCS.
Conclusion: This study highlights the significance of self-control deficiencies in OCS. It provides new insights into the psychological and behavioral factors that increase the risk of OCS with important practical implications for early intervention in OCD.
Keywords: obsessive-compulsive symptoms, self-control, procrastination, anxiety, chain mediating effect
Introduction
The World Health Organization has named obsessive-compulsive disorder (OCD) as one of the top 10 most disabling diseases.1 This disorder can be a severe burden, as it is challenging to treat; some OCD patients also do not respond to multiple treatment attempts.2 Therefore, early disease identification, including a better understanding of prodromal stages, could help improve treatment and disease progression, improving outcomes. Obsessive-compulsive symptoms (OCS) are more common than diagnosed OCD and can be regarded as an early risk marker for OCD.3 OCS can also be found in the general population, such as college students.4 A previous study reported a high prevalence of OCS among university students, with a rate of 58.53%. OCS may exist to varying degrees in patients with other mental disorders, potentially exacerbating their problems.5 Therefore, studying college students’ OCS is of great practical significance. There should be increased awareness of OCS to help improve the recognition and treatment of OCD. However, research has usually focused on confirmed cases of OCD, and OCS have rarely been studied in the general population.6,7 As a result, the factors associated with their onset and the mechanisms involved in their emergence have not been clarified.8 Specifically, there is insufficient awareness of the potential psychological and behavioral triggers of OCS.
Self-Control and Obsessive-Compulsive Symptoms
Self-control refers to the ability with which an individual can handle their own problems regarding their actions and mental state.9 It is a complex construct composed of multiple components, such as control motivation, control capacity and control effort.10 The Psychopathology of Self-Control Theory proposes that deficits in self-control underpin psychiatric symptoms, and individuals who lack essential self-control are more likely to be involved in short-term oriented risky behaviors and experience more negative emotions.11 The concept of self-control is often used to understand psychopathological phenomena, such as depression and anxiety,12 but is not often used to understand OCS. Moreover, in the few studies that have focused on this issue, only indirect evidence was obtained. For instance, cognitive experiments found that patients with OCD had longer stop-signal reaction times than a control group, indicating deficits in a neuropsychological domain known as inhibitory control, which can be a component of broader self-control.13 Meanwhile, researchers demonstrated that loss of self-control was a significant predictor of OCD.14 However, the authors measured constructs including locus of control (internal control/ powerful others/ chance) and fear of losing control (eg, “I worry that I will sometimes do things impulsively ”), yet they did not measure the level of self-control ability directly. Moreover, the sample size of this study was small, which may hinder the generalizability of the findings. Against this background, there is a need to directly examine the attenuating effect of self-control on OCD, preferably with a large sample to improve the generalizability of the results. The present study was established to examine the relationship between self-control and OCS, and explore the psychological mechanisms further.
Potential Mediating Effect of Procrastination
Generally, procrastination is the voluntary delay of an intended action, despite knowing the possible negative consequences.15 Procrastination is among the most common manifestations of low self-control among university students. Literature shows that 91.1% of Chinese college students procrastinate to varying degrees.16 In addition to its detrimental effects on students’ academic performance, procrastination harms their mental health.17 According to the Psychopathology Theory of Self-Control, individuals with low self-control tend to have an immediate orientation, whereby they seek immediate rather than delayed gratification. Moreover, they prefer those simple tasks that entail little skill or planning, and they avoid activities that require diligence, tenacity and persistence.11 Given that, individuals with low self-control are likely to procrastinate, especially on effortful tasks that demand inhibition and attentional efforts. Consistent with this, research has found that self-control negatively correlates with procrastination.18
In addition, procrastinators more often have recurrent negative thoughts,19 and there is a direct and significant positive correlation between rumination and procrastination.20 Rumination has also been shown to be common in individuals diagnosed with OCD. Those individuals who exhibit high rumination are more likely to have more severe OCS.21,22 Additionally, the specific emotional processing style of frequent procrastinators may exacerbate OCS. They cannot be self-compassionate and are prone to generating more negative emotions when experiencing failure.23 As procrastination worsens, the original tasks become more stressful.24 Thus, the procrastinators experience negative emotions, such as guilt, frustration, and sadness.25 Research has shown that negative emotion dysregulation partly contributes to the psychiatric etiology of OCS.26 Taking these findings together, procrastination leads to uncontrolled ruminative thinking and negative emotions. These cognitive and emotional problems in procrastinators are likely to trigger OCS. Although a few researchers have found no direct link between procrastination and OCD,27 others have revealed a direct positive association.28 Thus, we assume that procrastination may mediate the relationship between self-control and OCS, and people with higher self-control are less likely to procrastinate and thus experience lower OCS.
Potential Mediating Effect of Anxiety
As mentioned above, procrastination may induce negative emotions,25 which may increase OCS. Therefore, we assume that emotion may mediate the procrastination-OCS association. Anxiety is an emotion characterized by heightened sympathetic nervous system activity, such as increased blood pressure, subjective feelings of tension, and cognition that involves worry.26 Putting off tasks and not completing them may result in overwhelming stress in the long term. Literature shows that procrastinating behaviors are associated with anxiety and that task procrastination can amplify individuals’ symptoms of anxiety.29,30 People who frequently procrastinate may become sensitive to the anxiety induced by procrastination.27
Anxiety is also associated with increased levels of OCD.31 Despite that researchers found that other emotions such as disgust, anger, and shame can also trigger OCD,32,33 and that sensitivity to anxiety is crucial in exacerbating OCS.34 Some researchers have suggested that compulsive behaviors are performed to escape or reduce anxiety. Others have interpreted OCD as extreme anxiety.35 It has been proposed that some individuals uncontrollably engage in compulsive behaviors and thoughts in response to anxiety caused by uncertainty.36 Ahadi and Narimani found that anxiety was significantly positively correlated with total OCD scores, and the symptoms of checking and doubt in patients with OCD were best predicted by anxiety.37 Neuroimaging evidence also suggests an association between anxiety and OCS.38 Hence, anxiety may act as a mediator between procrastination and OCS.
Moreover, decreased self-control is directly and positively related to anxiety.39 Englert and Bertrams found that the experimental manipulation of state anxiety increased anxiety in participants with depleted self-control.40 Bertrams et al further found that higher self-control capacity predicts lower anxiety-impaired cognition.41 These results suggest that self-control may help individuals to deal with anxiety. Conversely, individuals with low self-control also have deficits in emotional regulation.40 Therefore, they may be unable to alleviate their anxiety well. Given the above, it is reasonable to deduce that self-control predicts anxiety, and may further influence OCS through it.
In summary, we suppose that individuals with low self-control are more likely to procrastinate, leading to negative emotions, which in turn affect OCS.
Method
Participants and Procedure
All participants in this study were recruited from a university in China. The results of 5599 aged 18–30 years newly enrolled undergraduate, postgraduate, and doctorate students were analyzed as valid. This was after excluding 461 participants (7.61% of the total data) who answered the probe question (Please select “undecided” for this item) incorrectly or failed to complete all measures.
Inclusion criteria: Students who volunteered to participate in this study.
Exclusion criteria: Students suffering from a mental disorder or with a history of mental disorder (these criteria were mentioned in the questionnaire guidance).
Participants were told to complete the questionnaires voluntarily and anonymously during the matriculation medical examination. The freedom to withdraw from the study at any time and the need to provide authentic answers were also emphasized before the investigation. This study was conducted with the informed consent of the participants and was approved by the ethics committee at the author’s university (IRB-22-001).
Measures
Self-Control Scale
The level of self-control was measured using the Chinese version of the Self-Control Scale revised by Tan and Guo.42 This scale has the following five sub-dimensions, each containing 2 to 6 items: impulse control (eg, people say I am impulsive), healthy habits (eg, getting up in the morning is difficult for me), resisting temptation (eg, I can resist temptation very well), focusing on work (eg, sometimes I get distracted by something fun instead of finishing tasks on time), and controlling entertainment (eg, sometimes I consume alcohol or use the internet too much). Participants chose the extent of fit of each item on a 5-point scale from 1(not at all) to 5 (completely). Higher scores indicated a higher level of self-control. The Chinese version of the Self-Control Scale showed good reliability and was found to be valid for assessing self-control among the Chinese population. Cronbach’s α coefficient of this scale was 0.86 in a previous study,42 and 0.91 in the current study.
Aitken Procrastination Inventory (API)
The tendency to procrastinate was assessed by the Aitken Procrastination Inventory (API), which includes 19 items (eg, I always wait until the last minute to start doing things) rated on a 5-point Likert scale ranging from 1 (false) to 5 (true). After reversing the scoring of certain items, the scores were summed. The total score is between 19 and 95, with higher scores indicating higher levels of procrastination (Aitken, 1982).43 API has been widely used on Chinese college student, and its Cronbach’ s α coefficient was found to be 0.80 in a previous study,44 while it was 0.89 here.
Symptom Checklist-90 (SCL-90)
Anxiety and OCS were measured using Symptom Checklist-90 (SCL-90). SCL-90 is a multidimensional symptom self-report scale with 90 items, each item rated on a 5-point scale of distress (0 to 4) from “not at all” to “extremely”.45 Anxiety and OCS were assessed using 10 items each. OCS include meaningless thoughts, impulses, behaviors, other performance, and more general perception disorders such as poor memory (eg, unwanted thoughts or ideas that do not leave your head).
Anxiety includes symptoms and experiences associated with anxiety, which generally include jitteriness, nervousness, and resulting physical signs such as tremors46 (eg, nervousness or shakiness inside). SCL-90 is reliable and can be used to study mental health in the Chinese population. It was previously reported that Cronbach’s α coefficients of obsessive-compulsive symptom and anxiety in SCL-90 were 0.87 and 0.83 among Chinese college student.47 In the present study, the corresponding values were 0.87 and 0.86, respectively.
Data Analyses
Harman’s single-factor test was used to test for common method bias. Descriptive and Pearson’s correlation analyses, used to test the correlations of all variables, were performed as preliminary analyses, as well as Bonferroni correction to control for multiple comparisons. A structural equation model (SEM) was used to examine the fit of our hypothetical model and the mediating roles of procrastination and anxiety in the relationship between self-control and OCS, using Mplus 7. And the bias-corrected percentile bootstrap method (sample = 1000, 95% confidence interval) was also used to test the chain mediating effects of procrastination and anxiety.
Results
The mean age of the valid sample was 21.47 (SD=2.82), and 62.85% of the participants were women. Harman’s single-factor test showed eight factors with characteristic roots greater than 1 with the first principal factor explaining 26.32% of the variance (<40%), which implied that there was no serious common method bias in our study.
Preliminary Analyses
As shown in Table 1, OCS was significantly negatively correlated with self-control (see Figure 1), and positively correlated with procrastination and anxiety. Self-control was significantly negatively correlated with procrastination and anxiety. Meanwhile, anxiety was significantly positively correlated with procrastination. After controlling for the effect of sex (dummy coding: 0=men, 1=women) and age, self-control (β=–0.48, p<0.001, R2=0.23) had a significantly negative predictive effect on OCS.
 |
Table 1 Descriptive Statistics and Pearson’ s Correlation Coefficients of the Study Variables (n=5599) |
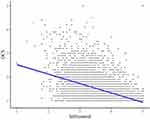 |
Figure 1 Scatter Plot of Self-control and OCS. |
Mediating Effect Analyses
Model fit indices showed that our data fit the chain mediating model well (χ2/df=33.43, CFI=0.99, TLI=0.96, RMSEA=0.08, SRMR=0.02). Figure 2 shows that after controlling for age and sex, self-control was a direct and significant negative predictor of OCS(β=–0.17 p<0.001), procrastination (β=–0.71, p<0.001), and anxiety (β=–0.34, p<0.001). Moreover, procrastination had a significantly positive effect on anxiety (β=0.04, p<0.05). Procrastination (β=0.07, p<0.001) and anxiety (β=0.70, p<0.001) also had significant positive predictive effects on OCS. Next, we examined the power of the mediating effects using RMSEA.48 The results showed that this power was 0.99, indicating our sample size was reasonable for constructing the SEM model.49
 |
Figure 2 The Chain Mediating Effect of Procrastination and Anxiety. Notes: *p<0.05, ***p<0.001. |
The chain mediating effects of procrastination and anxiety are presented in Table 2. According to the results, the total indirect effect was significant [effect=–0.31, BootSE=0.01, 95CI (–0.33,–0.28)], which accounted for 64.66% of the total effect. The total indirect effect included three pathways, and the 95% confidence intervals did not include zero, indicating that all of the indirect effects were significant. When procrastination served as a mediator, the indirect effect accounted for 11.01% of the total effect. When anxiety served as a mediator, the indirect effect accounted for 49.19% of the total effect. Finally, the chain mediating effect explained 4.43% of the total effect.
 |
Table 2 Indirect Effect of Procrastination and Anxiety (n=5599) |
Discussion
Self-control is a complex concept with multiple components (eg, control capacity, control motivation),10 and is considered necessary in almost every aspect of human life.50 This study focused on the effect of self-control on OCS and found that, after controlling for the effects of sex and age, self-control had a negative predictive effect on OCS. Based on a large sample and direct measurements of self-control, this study provides empirical support for the influence of self-control on OCS. The results also strengthen the evidence for a relationship between self-control and OCD,51 and expand the scope of explanation of the Psychopathology of Self-Control Theory to OCS.
Moreover, we found that procrastination was a partial mediator between self-control and OCS. This means that people with lower levels of self-control are more likely to procrastinate and thus experience OCS. This result is partly consistent with the findings of Qing et al,52 who reported a partial mediating role of procrastination between self-regulation and mental health problems in college students. As the Psychopathology of Self-Control Theory proposed, individuals with low self-control have a here-and-now orientation, and they tend to seek immediate rather than delayed gratification.11 Thus, self-control can significantly reduce procrastination.18,53 Furthermore, a correlation has been found between procrastination and OCS.54 Procrastinators are prone to developing negative thoughts about themselves, setting the stage for ruminative thinking and more negative evaluations of intrusive thoughts and subsequent pathological counter-compulsive thinking.55
Additionally, the mediating effect of anxiety between self-control and OCS was found to be significant in the present study. This indicates that individuals with lower self-control tend to experience a higher level of anxious affect, which increases their risk of developing OCS. Previous studies have shown a positive correlation between OCS and anxiety.56,57 Some researchers have suggested that compulsive behavior is intended to reduce anxiety. Specifically, compulsive behavior may be a non-adaptive coping strategy for relieving anxiety.58 However, in previous studies, the subjects were limited to OCD patients,29 and the results of the present study suggest that the association between anxiety and OCS may not be limited to clinical samples but rather reflects coping patterns that exist in a more general population.
The role of procrastination in OCS was indirect. People who often procrastinate may become sensitive to anxiety induced by procrastination.27 Researchers found that procrastination can directly trigger negative emotions like anxiety, which further contribute to the OCS.59,60 In summary, based on the results of mediating effect analyses, besides directly influencing OCS, self-control affects OCS indirectly in three ways: procrastination, anxiety, and the chain mediating effect of procrastination and anxiety. These results deepen our understanding of the psychological mechanisms linking self-control and OCS.
Notably, anxiety has a greater indirect effect on OCS than procrastination and the chain mediating path, which may have several explanations as follows. First, there was a high correlation between anxiety and OCS.35 Next, previous literature presents inconsistent results on the relationship between procrastination and OCD. This may be due to differences in the measuring instruments and sample types used in different studies. For example, a study found a significant correlation between procrastination and OCD by using Aitken Procrastination Inventory and an adolescent sample,28 while another suggested no correlation by using The General Procrastination Scale and a sample of college students.27 Moreover, there may be variables that moderate the effects of procrastination on anxiety and OCS. For example, individuals with high vulnerability are more likely to develop negative emotions following procrastination and may be more likely to start to exhibit OCS than individuals with low vulnerability.61 In addition, self-regulation may also serve as a moderator on the effect of procrastination.62 Hence, the effect of stress resulting from procrastination on OCS might be partially buffered by the effect of moderators.
Finally, some limitations of this study should be addressed in future research. First, the effect size of procrastination is small. In addition to the possible impact of moderators, another reason for this could be the suppressing effects as variables inversely predicted OCS in our model. Previous studies yielded results of a significant positive correlation or no relationship between procrastination and OCS. Our results support the former, albeit with a small effect size. Although this result is significant, there may be other effectively mediating variables that can explain the association between self-control and OCS. Second, this study focused on non-clinical samples, so in addition to excluding patients with known diagnosed mental disorders, the measurement of Y- BOCs should also be performed to exclude patients with clinical OCD to ensure that the sample is more consistent with the purpose of the study. Besides, more women than men participated in the study. The participants came from a university with the top-ranked humanities department in China, and women constitute the majority of students at this college. Further research could assess whether an imbalance in the sex of subjects would affect the obtained results. Moreover, more demographic and clinical data need to be collected to serve as control variables or to screen participants. In addition, this study featured a cross-sectional design, meaning that causation could not be inferred from our correlational findings.
Besides the possibility that procrastination causes a negative affect and, then, to OCS, obsessive-compulsive tendencies may cause procrastination. In the future, it will be necessary to conduct longitudinal or experimental research to test the driving effect between variables. Finally, this study relied on self-reporting methodologies. The bias in self-reporting may jeopardize the internal validity of the study. Experimental methods (eg, intervening in procrastination behavior) or obtaining data from various sources (eg, parents and peer) could compensate for this shortcoming.
Conclusion
This study explored the internal mechanisms of self-control and OCS. A significant pathway involving lack of self-control→procrastination→anxiety→OCS was identified. These results facilitate the development and application of the Psychopathology of Self-Control Theory. The present study is expected to provide insights into OCD prevention. First, deficits in self-control may be an early psychological warning sign for the onset of OCD for specific groups of people. Then, procrastinating regulatory strategies to relieve anxiety may be an indirect protective factor and representing a more operational approach. Finally, considering the strong predictive power of anxiety on OCS, training to relieve anxiety can be used as a preventive therapy to help individuals directly alleviate OCS. Some limitations of this study, such as the lack of use of professional scales to screen samples, should be noted and improved in future work.
Data Share Statement
The data of the present study supporting the conclusions will be made available on request by the corresponding author.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki, and the study has been reviewed and approved by the ethics committee of the Department of Psychology, Renmin University of China (ethical approval number: IRB-22-001).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgment
The authors sincerely thank anonymous reviewers’ constructive comments and each participant for their cooperation during the investigation.
Funding
The research was supported by National Social Science Foundation of China (Major Program): 19ZDA021.
Disclosure
The authors declare that there is no conflict of interest.
References
1. Stein DJ, Costa DL, Lochner C, et al. Obsessive-compulsive disorder. Nat Rev Dis Primers. 2019;5:52. doi:10.1038/s41572-019-0102-3
2. Zhang H, Zhou P, Liu N, Zhang N. Research progress of biomarkers related to the efficacy of cognitive-behavioral therapy for obsessive-compulsive disorder. Chin J Psychiatry. 2022;55:413–418. doi:10.3760/cma.j.cn113661-20211121-00335
3. Pagliacci D, Durham K, Fitzgerald KD, Marsh R. Obsessive-compulsive symptoms among children in the adolescent brain and cognitive development study: clinical, cognitive, and brain connectivity correlates-ScienceDirect. Biol Psychiatry Cogn Neurosci Neuroimaging. 2020;6(4):399–409. doi:10.1016/j.bpsc.2020.10.019
4. Ji G, Wei W, Yue KC, et al. Effects of the COVID-19 pandemic on obsessive-compulsive symptoms among university students: prospective cohort survey study. J Med Internet Res. 2020;22:e21915. doi:10.2196/21915
5. Shuqayrat MA. Obsessive-compulsive symptom prevalence among university students and associated demographic variables. Arab J Psychiatr. 2021;32:79–85. doi:10.12816/0058768
6. Vivan AD, Rodrigues L, Wendt G, Bicca MG, Braga DT, Cordioli AV. Obsessive-compulsive symptoms and obsessive-compulsive disorder in adolescents: a population-based study. Braz J Psychiatry. 2013;36:111–118. doi:10.1590/1516-4446-2013-1113
7. Park LS, Burton CL, Dupuis A, et al. The Toronto obsessive-compulsive scale: psychometrics of a dimensional measure of obsessive-compulsive traits. J Am Acad Child Adolesc Psychiatry. 2016;55:310–318. doi:10.1016/j.jaac.2016.01.008
8. Menzies RE, Zuccala M, Sharpe L, Dar NI. Are anxiety disorders a pathway to obsessive-compulsive disorder? Different trajectories of OCD and the role of death anxiety. Nord J Psychiatry. 2021;75:170–175. doi:10.1080/08039488.2020.1817554
9. Dan F. A review of the studies of children’s self-control ability. J Shenyang Normal University Soc Sci Edit. 2001;25:68–72. doi:10.3969/j.issn.1674-5450.2001.01.019
10. Kotabe HP, Hofmann W. On integrating the components of self-control. Perspect Psychol Sci. 2015;10:618–638. doi:10.1177/1745691615593382
11. Vaughn MG, Delisi M, Beaver KM, Wright JP, Howard MO. Toward a psychopathology of self-control theory: the importance of narcissistic traits. Behav Sci Law. 2007;25:803–821. doi:10.1002/bsl.789
12. Geng Y, Gu J, Wang J, Zhang R. Smartphone addiction and depression, anxiety: the role of bedtime procrastination and self-control. J Affect Disord. 2021;293:415–421. doi:10.1016/j.jad.2021.06.062
13. Boisseau CL, Thompson BH, Caldwell HC, Pratt E, Farchione T, Harrison BD. Behavioral and cognitive impulsivity in obsessive-compulsive disorder and eating disorders. Psychiatry Res. 2012;200:1062–1066. doi:10.1016/j.psychres.2012.06.010
14. Froreich FV, Vartanian LR, Grisham JR, Touyz SW. Dimensions of control and their relation to disordered eating behaviors and obsessive-compulsive symptoms. J Eat Disord. 2016;4:1–9. doi:10.1186/s40337-016-0104-4
15. Sirois F, Pychyl T. Procrastination and the priority of short-term mood regulation: consequences for future self. Soc Personal Psychol Compass. 2013;7:115–127. doi:10.1111/spc3.12011
16. Shu YF, Yang BX, Ruan J. Study on procrastination and its distribution among college students in 5 universities of Wuhan city. Chin J Health Educ. 2019;35:309–322. doi:10.16168/j.cnki.issn.1002-9982.2019.04.005
17. Geng J, Han L, Gao F, Jou M, Huang CC. Internet addiction and procrastination among Chinese young adults: a moderated mediation model. Comput Human Behav. 2018;84:320–333. doi:10.1016/j.chb.2018.03.013
18. To PY, Lo BC, Ng TK, Wong BP, Choi AW. Striving to avoid inferiority and procrastination among university students: the mediating roles of stress and self-control. Int J Environ Res Public Health. 2021;18:5570. doi:10.3390/ijerph18115570
19. Stainton M, Lay CH, Flett GL. Trait procrastinators and behavior/trait-specific cognitions. J Soc Behav Pers. 2020;15:297–312. doi:10.1080/00926230152035859
20. Hairston IS, Shpitalni R. Procrastination is linked with insomnia symptoms: the moderating role of morningness-eveningness. Pers Individ Dif. 2016;101:50–56. doi:10.1016/j.paid.2016.05.031
21. Wahl K, Van DH, Heinzel CV, et al. Rumination about obsessive symptoms and mood maintains obsessive-compulsive symptoms and depressed mood: an experimental study. J Abnorm Psychol. 2021;130:435–442. doi:10.1037/abn0000677
22. Wang P, Cao W, Chen T, et al. Mediating role of rumination and negative affect in the effect of mind-wandering on symptoms in patients with obsessive-compulsive disorder. Front Psychiatry. 2021;12:755159. doi:10.3389/fpsyt.2021.755159
23. Sirois FM. Procrastination and stress: exploring the role of self-compassion. Self Identity. 2014;13:128–145. doi:10.1080/15298868.2013.763404
24. Khalid A, Zhang Q, Wang W, Ghaffari AS, Pan F. The relationship between procrastination, perceived stress, saliva alpha-amylase level and parenting styles in Chinese first year medical students. Psychol Res Behav Manag. 2019;12:489–498. doi:10.2147/PRBM.S207430
25. Pychyl TA, Lee JM, Thibodeau R, Blunt A. Five days of emotion: an experience sampling study of undergraduate student procrastination. J Soc Behav Pers. 2012;15:239–254. doi:10.1080/00926230152035859
26. Kazdin AE. Encyclopedia of Psychology; 2000. Available from: https://www.apa.org/pubs/books/4600100.
27. Hutchison TE, Penney AM, Crompton JE. Procrastination and anxiety: exploring the contributions of multiple anxiety-related disorders. Curr Issues Pers Psychol. 2018;6:122–129. doi:10.5114/cipp.2018.73054
28. Temel K, Mücahit K, Murat B, Ibrahim G. Associations between academic competence and obsessive-compulsive symptoms among adolescents. Procedia Soc Behav Sci. 2010;5:309–313. doi:10.1016/j.sbspro.2010.07.094
29. Macher D, Paechter M, Papousek I, Ruggeri K. Statistics anxiety, trait anxiety, learning behavior, and academic performance. Br J Educ Psychol. 2012;27:483–498. doi:10.1007/s10212-011-0090-5
30. Wang Y. Academic procrastination and test anxiety: a cross-lagged panel analysis. J Psychol Couns Sch. 2021;31:122–129. doi:10.1017/jgc.2020.29
31. Awais A, Chetan B, Douglas G, et al. Associations among comorbid anxiety, psychiatric symptomatology, and diabetic control in a population with serious mental illness and diabetes: findings from an interventional randomized controlled trial. Int J Psychiatry Med. 2017;53:126–140. doi:10.1177/0091217417749795
32. Knowles KA, Jessup SC, Olatunji BO. Disgust in anxiety and obsessive-compulsive disorders: recent findings and future directions. Curr Psychiat Rep. 2018;20:1–10. doi:10.1007/s11920-018-0936-5
33. Abramowitz A, Berenbaum H. Emotional triggers and their relation to impulsive and compulsive psychopathology. Pers Indiv Differ. 2007;43:1356–1365. doi:10.1016/j.paid.2007.04.004
34. Storch EA, Wu MS, Small BJ, et al. Mediators and moderators of functional impairment in adults with obsessive-compulsive disorder. Compr Psychiatry. 2014;55:489–496. doi:10.1016/j.comppsych.2013.10.014
35. Simon DJ. Anxiety and related disorders. All. 2016;Journals:199–232.31. doi:10.1037/14779-009
36. Gillett CB, Bilek EL, Hanna GL, Fitzgerald KD. Intolerance of uncertainty in youth with obsessive-compulsive disorder and generalized anxiety disorder: a transdiagnostic construct with implications for phenomenology and treatment. Clin Psychol Rev. 2018;60:100–108. doi:10.1016/j.cpr.2018.01.007
37. Ahadi B, Narimani M. The role of disgust, anxiety and depression in explaining obsessive-compulsive symptoms in a non-clinical sample. J Health Psychol. 2010;3:37–44.
38. Matsunaga H. Current and emerging features of obsessive-compulsive disorder--trends for the revision of DSM-5. Psychiat et Neurolog Japon. 2012;114:1023–1030.
39. Hamama R, Ronen T, Feigin R. Self-control, anxiety, and loneliness in siblings of children with cancer. Soc Work Health Care. 2000;31:63–83. doi:10.1300/J010v31n01_05
40. Englert C, Bertrams A. The role of self-control strength in the development of state anxiety in test situations. Psychol Rep. 2013;112:976–991. doi:10.2466/15.10.PR0.112.3.976-991
41. Bertrams A, Baumeister RF, Englert C. Higher self-control capacity predicts lower anxiety-impaired cognition during math examinations. Front Psychol. 2016;7:485. doi:10.3389/fpsyg.2016.00485
42. Tan S, Guo Y. Revision of Self-Control scale for Chinese college students. J Clin Psychol. 2008;16:468–470.
43. Aitken ME. A personality profile of the college student procrastinator. Dissertation abstracts international section A. Humanit Soc Sci. 1982;43:722–723.
44. Chen XL, Dai XY, Dong Q. A research of Aitken procrastination inventory applied to Chinese college students. J Clin Psychol. 2008;1:22–24.40. doi:10.3969/j.issn.1005-3611.2008.01.007
45. Derogatis LR, Rickels K, Rock AF. The SCL 90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. 1976;128:280–289. doi:10.1192/bjp.128.3.280
46. Wang ZY. Symptom self-rating scale. Shanghai Psychiatry. 1984;2:68–70.
47. Shi LY, Huang PP, Zhuo L, et al. Reference value and reliability evaluation of SCL-90 scale for college students. Chn J Sch Health. 2013;34:223–224.
48. Preacher KJ, Coffman DL. Computing power and minimum sample size for RMSEA [Computer software]; 2006. Available from: http://quantpsy.org/.
49. Kyriazos TA. Applied psychometrics: sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychol. 2018;9:2207–2230. doi:10.4236/psych.2018.98126
50. Gökalp ZŞ, Haktanir A. An evaluation of the self-report instruments assessing self-control: a systematic review. Scand J Psychol. 2023;64:238–251. doi:10.1111/sjop.12881
51. Timpano KR, Schmidt NB. The relationship between self-control deficits and hoarding: a multimethod investigation across three samples. J Abnorm Psychol. 2013;122:13–25. doi:10.1037/a0029760
52. Qing ZH, Wu CH, Cao JP. The mediating effect of academic procrastination between college students’ time management disposition and mental health. J Changsha University. 2018;32:140–142. doi:10.3969/j.issn.1008-4681.2018.04.037
53. Zhao J, Meng G, Sun Y, Xu Y, Geng J, Han L. The relationship between self-control and procrastination based on the self-regulation theory perspective: the moderated mediation model. Curr Psychol. 2021;40:5076–5086. doi:10.1007/s12144-019-00442-3
54. Jamil L, Ashouri A, Zamirinejad S, Mahaki B. Investigating the structural model of procrastination based on transdiagnostic factors. Med J Islam Repub Iran. 2021;35:120. doi:10.47176/mjiri.35.120
55. Ferrier S, Brewin CR. Feared identity and obsessive-compulsive disorder. Behav Res Ther. 2005;43:1363–1374. doi:10.1016/j.brat.2004.10.005
56. Nadeau JM, Lewin AB, Arnold EB, Crawford EA, Murphy TK, Storch EA. Clinical correlates of functional impairment in children and adolescents with obsessive-compulsive disorder. J Obsessive Compuls Relat Disord. 2013;2:432–436. doi:10.1016/j.jocrd.2013.10.002
57. Storch EA, Larson MJ, Muroff J, et al. Predictors of functional impairment in pediatric obsessive-compulsive disorder. J Anxiety Disord. 2010;24:275–283. doi:10.1016/j.janxdis.2009.12.004
58. Arya A, Soodan S. Obsessive-compulsive disorder: prevalent and debilitating illness. World J Pharm Pharm Sci. 2016;5:328–340.
59. Shahram V. Canonical correlation analysis of procrastination, learning strategies and statistics anxiety among Iranian female college students. Procedia Soc Behav Sci. 2011;30:1620–1624. doi:10.1016/j.sbspro.2011.10.314
60. Momeni F, Kami M. The relationship between emotion dysregulation with obsessive compulsive disorder regarding generalized anxiety disorder symptoms. Asian J Psychiatr. 2021;22:235651299.
61. Monroe SM, Hadjiyannakis H. The social environment and depression: focusing on severe life stress. In: Handbook of Depression. Guilford Press; 2002:314–340. Available from: https://api.semanticscholar.org/CorpusID:149800369.
62. Yang Z. Does procrastination always predict lower life satisfaction? A study on the moderation effect of self-regulation in China and the United Kingdom. Front Psychol. 2021;12:690838. doi:10.3389/fpsyg.2021.690838
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
