Back to Journals » Open Access Journal of Contraception » Volume 15
Demographic, Sociocultural, and Behavioral Predictors of Modern Contraceptive Uptake Among Couples in Northern Ghana
Authors Allotey NK , Bosoka SA
Received 12 August 2023
Accepted for publication 24 February 2024
Published 11 March 2024 Volume 2024:15 Pages 23—40
DOI https://doi.org/10.2147/OAJC.S430288
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Naa-Korkor Allotey,1,2 Samuel Adolf Bosoka3,4
1Ethics and Research Management Department, Research and Development Division, Ghana Health Service, Accra, Ghana; 2Department of Population, Family and Reproductive Health, School of Public Health, University of Ghana, Accra, Ghana; 3Disease Surveillance Unit, Volta Regional Health Directorate, Ghana Health Service, Ho, Ghana; 4Department of Epidemiology and Biostatistics, Fred N. Binka School of Public Health, University of Health and Allied Sciences, Ho, Ghana
Correspondence: Naa-Korkor Allotey, Email [email protected]; [email protected]
Background: Despite efforts to increase modern contraceptive use in Ghana, prevalence rates remain low; particularly in Northern Ghana. This study, therefore, sought to determine the predictors of modern contraceptive use among couples in Northern Ghana. This research was the baseline assessment for a broader study aimed at determining the effect of an intervention to improve outcomes of modern contraception.
Methods: The study was a cross-sectional design. Data was collected from 508 couples (1016 participants), using a multistage sampling technique; both members of each couple were interviewed separately. Univariate and stepwise multivariate logistic regression were used to identify predictors associated with modern contraceptive use. Qualitative data were analyzed to triangulate the findings from the quantitative data.
Results: More than 97% of couples were Muslims. Qualitative data indicates that Muslims are less inclined to use Modern Contraceptives. Most participants had no education. The regression model shows that all demographic characteristics were not significant in Model 3 for men. Socio-culturally, men who gave the reason of “unconcerned” for men’s non-involvement in contraceptive adoption, had less odds of using modern contraception (AOR=0.19). Men with high subjective norms were more than 15 times more likely to use modern contraception. Female farmers were less likely to use contraceptives (AOR= 0.45). Women who reported that “nothing prevented men” from getting involved in contraceptive adoption had greater odds of adopting modern contraception (AOR= 11.15). Women with good perceived behavioral control were more likely to use modern contraception (AOR=5.03). Women with high enacted stigma and men and women with high interspousal communication were more likely to adopt modern contraception.
Conclusion: Taking cognizance of demographic and sociocultural characteristics and behavioral constructs is needed when determining the predictors of modern contraceptive use among couples in Northern Ghana.
Keywords: predictors, modern contraceptive use, couples, demographic, sociocultural, behavioral, Northern Ghana
A Letter to the Editor has been published for this article.
A Response to Letter by Miss Shahid has been published for this article.
Introduction
Modern contraception has long been proven to be effective in reducing unwanted pregnancies and to help couples plan their families. The use of various modern contraceptive (MC) techniques in family planning could save up to 35% of maternal fatalities, 13% of infant mortality, and 25% of under-five mortalities.1 Studies also show that using various types of modern contraception in family planning promotes gender equity and educational and economic empowerment for women.2
Taking all these benefits into account, Ghana identified modern contraception as the primary tool for slowing population growth.3 Despite the laudable policies in place, there has been a minimal increase in modern contraceptive prevalence rates (mCPRs), from 18.8% in 1994 to 25% in 2017.4 Modern contraceptive (MC) use is particularly low in Ghana’s three traditional northern regions; ie, Upper West, Upper East and Northern regions.5,6 The traditional Northern Region, in particular, had the lowest MC uptake in 2017 (17%).4 Moreover, family planning acceptor rates in the traditional Northern Region were 18.4% in 2014, 18.1% in 2015, and 21.7% in 2016 (DHMIS, 2016). These rates were below the national family planning acceptor target rate of 23.3%.6
The literature identifies that there are positive, negative and existential predictors influencing MC uptake. These predictors are mostly demographic and sociocultural factors. Positive factors include education, economic empowerment and urban dwelling. Negative predictors include gatekeepers of women and challenges with geographic access. Existential or bi-polar predictors include male involvement.7
In Ghana, several predictors, mostly demographic and sociocultural, have been identified to influence MC uptake in various parts of Ghana.1,8 For example, Eliason et al1 and Adongo et al8 found that women with no formal education, socio-cultural beliefs and interspousal spousal communication were predictors of MC uptake in the northern part of Volta Region, Northern and Southern regions of Ghana. Another important finding by Adongo et al was the stigmatization linked to MC use in Northern Ghana. Other studies in Northern Ghana9,10 identified cultural and religious unacceptability, desire to continue participants’ education, small families preferences and not married as factors influencing MC use.
In general, among couples, studies on predictors associated with MC use among couples are limited.11,12 Nevertheless, Tilahun et al11 and Tumlinson et al12 showed that knowledge, attitude and interspousal communication influenced MC uptake among couples.
In addition, most studies are generally limited to the study of demographic and sociocultural predictors of MC use, with few studies on behavioral constructs as predictors.11,13 Particularly, no study has been identified that has studied the association between the MC uptake and the four behavioral constructs of the Theory of Planned Behavior (TPB); (subjective norms, attitude and perceived behavioral control, intention to use) and of stigma; especially among couples in northern Ghana. Therefore, this study sought to identify the predictors of modern contraceptive uptake among couples in Northern Ghana.
Methods and Materials
Study Design
This study was the baseline assessment using cross-sectional design to inform a larger study aimed at determining the effect of an intervention based on health behavior models on the outcomes of modern contraception including MC uptake.
Study Site
The study was conducted in the Tolon and Kumbungu districts of the Northern Region; one of the 16 regions of Ghana. Tolon has six subdistricts with a population of 87,181 in 2016, while Kumbungu has five subdistricts, with a population of 88,791. In each district, two subdistricts were selected; a rural and an urban subdistrict. Both districts are of the Dagomba ethnic group. The major religion practiced in both districts is Islam.
Study Participants
This study involved couples (women and their male partners). The participant couples needed to have been together for at least two years and should have at least two children. Men in polygamous marriages were included but only one wife (of his choice) was selected. The women were 16–49 years and women who reported pregnancy at the time of the survey were excluded (Pregnant women were excluded because we needed to determine if participants were “currently using MCs”). The women’s male partners had to be between the ages of 16–59 years.14
Sampling
A combination of purposive and multistage sampling was used. The Northern Region was purposively selected because, at the time of the study, the region had the lowest mCPR.4 In the region, Tolon and Kumbungu districts were also purposively sampled because they had one of the lowest acceptor rates per three-year trend (2014–2016) data from the Ghana Health Service Routine database named DHIMS2. Moreover, at the district level, sub-districts were categorized along the rural and urban divide, and rural and urban subdistricts were randomly selected for each district. The designation of urban and rural sub-districts was based on the information given by the district health authorities. The designation is done based on the authorities’ assessment of the sub-districts’ economic activities and population (Communication with district health authorities, 2018).
Communities were also randomly selected from lists of communities that excluded communities with challenges of geographical access because of cost. An average of ten communities were randomly selected for each subdistrict and a total of forty-one communities were involved in the study. In each community, twelve or thirteen, consenting couples were recruited.
Sample Size Estimation
The sample size was computed using STATA software version 15. The calculated sample size was 336. Stigma related to MC use was identified in the formative stage of the study and this necessitated a need to compensate for a possible high loss to follow-up (25%) and non-response rate (25%).15,16 Thus, the total sample size was 504 couples (ie, 1008 participants). This sample was allocated to each of the four selected subdistricts.
Data Collection Techniques
Both quantitative and qualitative data collection techniques were used. Quantitative data was collected using structured and semi-structured questions.
The qualitative data collected were as follows: eight focus group discussions (FGDs), four in-depth interviews (IDIs), eight key informant interviews (KIIs), four Rapid Assessment Process (RAP; a type of in-depth interview which uses community opinion leaders that interviewees were comfortable with).17 Participants of the FGDs were segregated into groups based on the husbands’ MC behavior and residency. Automatically, wives of men who were using contraception were considered users as well (While the extrapolation of men’s MC behavior on their wives may not be an accurate estimation of the wives’ MC behavior, we wanted to make it easier for the wives to respond to the invitation and participate in the FGDs by coming along with the husbands. This strategy was generally successful). Therefore FGDs were segregated as rural/urban users, men and their wives, and rural/urban men non-users and their wives.
Tools and Measures
Demographic characteristics were age (in complete years), religion (Christian/ Muslim/ Traditional), education, employment, duration of marriage, type of marriage (monogamous/polygamous), residency (rural/urban), socioeconomic status (SES). The sociocultural characteristics were: “success in preventing pregnancy in the past”, “ideal birth spacing period” and “ideal number of children” (which refers to the number of children a particular participant desires; that is for himself or herself) “whether men should be involved in the decision to adopt modern contraception”. Most participants who responded yes were further asked “why men were not involved in MC adoption”. The options were, “they did not have time”, “they did not have enough information” and were “unconcerned”. We further determined if these reasons influenced the decision to use MCs.
We also conducted an assessment of behavioral or psychological constructs, using different items for men and women for each construct and using validated tools. The validated tools were used to measure constructs of the Theory of Planned Behavior (TPB); attitude, perceived behavioral control and subjective norms, which are predictors of intention to use (also a construct of TPB). Moreover, validated tools were used for the sub-constructs of stigma. The validated tools were adapted, taking into consideration the cultural idiosyncrasies (including heavy stigma) of participants. The adaptation was important to improve the internal consistencies of the tools. The validated tools were as follows: Condom Use Self-Efficacy Scale (CUSES),18 Contraceptive Attitude Scale (CAS)19 (James-Hawkins and Broaddus quoting Keyes, 1998), Intention to Use,20 Adolescent Sexual and Reproductive Health Stigma Scale.21
The constructs are described as the follows for the purposes of this study: Attitude is the personal view or opinion of MC adoption; perceived behavioral control is a person’s perception of the ease or difficulty of adopting MCs; subjective norms is the belief that a “significant other” or someone or group of people of importance will approve of him or her adoption of MCs. The sub-constructs of stigma under this study were self-stigma and enacted stigma. Enacted stigma refers to the experience or perception of unfair treatment by others because one is using MCs. Self-stigma refers to the shame resulting from peoples’ prejudicial treatment, preventing one from talking about his experiences and stopping a person from seeking family planning services. The constructs were measured with both positive (forward) and negative (backward) items. Annex Table 1 gives details of items used to measure the constructs and their Cronbach’s Alpha (which was more than 0.7). All items used to measure the constructs were obtained through factor analysis (eigenvalues>1.0). The construct items were measured with 5-point Likert scales. The Variance Inflation Factor (VIF) for the male and female questionnaire are found Annex Tables 2a and 2b.
Interspousal communication was measured by 3 items; interspousal communication on “whether to adopt family planning”, “the number of children to have” and “when to have the next child”.
Contraceptive uptake was measured with a combination of two items: “whether the participant was using contraceptives currently” or “had used contraceptives in the past 3 months”. Participants who responded “yes” to any of the two questions were asked which type of contraceptive method. The type of contraceptive method used produced answers that included traditional contraceptive methods such as coitus interruptus and abstinence. We segregated the answers to this question into: participants using traditional methods and those using modern contraceptives (MCs). MC uptake was measured using only those who reported using MC methods; that is, any type of modern contraceptive method.
Quality Assurance
To ensure that participants, who were mostly illiterates, understood the questions, the questionnaires were given to a professional Dagbani translator. Research assistants (RAs), also, needed to be fluent in Dagbani. During training, RAs were taken through each question and ensured that the meaning was well understood by all and could be adequately explained to participants. Moreover, RAs were grouped into pairs of male and female, which we designated as “RA couples”. The female RA interviewed the wife and the husband was interviewed by the male RA.
Ethical Consideration
The study protocol was approved by the Ghana Health Service Ethics Review Committee; (approved protocol number GHS-ERC:006/02/18). The study was aligned with the requirements for the Declaration of Helsinki. Study participants’ well-being and rights of participants took precedence in the study. Each husband and wife were approached by the RA couple and invited to participate in the study. Participation in the study was strictly voluntary and participants could end the interviews at any point without reprisal and were assured of confidentiality. A written informed consent was sought from participants before being recruited into the study; with literate participants signing and the illiterate thumbprinting in the presence of a witness. The informed consent by participants included the publication of anonymized responses. Privacy was ensured for all participants during interviews, with husbands being interviewed separately from the wives. The data collected has been anonymized. All participants were informed of the purpose of the study as part of the information sheet. Also, participants who were unable to read had the purpose explained to them in the presence of a witness. All data collected was protected and could be accessed only by the principal investigator and the study team. Compensation for participants’ time was given in the form of bars of washing soaps. Permission was sought to record proceedings for the qualitative data.
Data Management and Data Analysis
The data collection tools for the quantitative data were converted into an electronic version using Open Data Kit (ODK) Collect. Data were then exported into STATA/MP version 15.0 for analysis. Descriptive analyses were used to describe demographic and socio-cultural characteristics. Additionally, descriptive analyses were used to determine construct levels. Continuous variables were reported as mean with standard deviation and categorical variables were reported as proportions. Behavioral constructs were categorized as high or low, using the mean as a cut-off for the aggregated score for each construct. Univariate and multivariate logistic regression was used to measure the strength of the association between the dependent (MC uptake) and independent variables. Crude odds ratios (CORs) were estimated for each outcome. All variables with significance levels of less than 0.05 were considered significant. In order to identify a parsimonious multivariable model for both men and women, the three groups of predictors were introduced into the model in a stepwise manner. Model 1 was a demographic variable. In Model 2 sociocultural variables were included and finally in Model 3, behavioral constructs were introduced. It is worth noting that we did not include religion in the model because over 97% of participants were Muslims. This was done because the qualitative data showed that religion influenced MC use. Data were presented using tables and graphs.
 |
Table 1 Contraceptive Usage by Religion in Northern Ghana, 2019 |
Qualitative data were transcribed, coded, and analyzed manually. The information so generated was used to triangulate the quantitative data.
Results
Table 1 shows that a higher percentage of Christians almost 23 (70%) reported using MCs while 193 (19.9%) of Muslims reported using MCs. We, carried out a cross tab of MC for religion (Table 1) to demonstrate the uptake level for each religion. From Table 2, male respondents had a mean age of 39.4 years (SD= 8.0) while females’ mean age was 32.2 years (SD=6.8). The majority of participants were Muslims 993 (97.7%). Additionally, about two-thirds of the men had no education while 451 (88.8%) of the women had no education. Most men were farmers (91.3%) and 53.7% of women were farmers while 18.5% were traders/artisans. Participants were almost similarly distributed in all wealth quintiles, both males and females.
 |
Table 2 Background Characteristics of Participants in Northern Ghana, 2019 |
Concerning Sociocultural characteristics, (Table 3) a similar percentage of men and women wanted less than 3 years of birth spacing. Furthermore, over sixty percent of women (60.4%) compared with about 40% of men wanted between 6–10 children. Percentages were similar for reasons given by men and women on “why men do not get involved in contraception adoption” except the reason of, “nothing prevents them”; which was significantly different.
 |
Table 3 Socio-Cultural Characteristics of Participants in Northern Ghana, 2019 |
Behavioral characteristics of participants (Table 4) showed that 10% more women than men had a good attitude towards modern contraceptives. In addition, the percentages were similar for women and men for subjective norms, perceived behavioral control, stigma enacted and the interspousal communication items on MCs and the number of children wanted. However, there were significant differences between men and women on self-stigma (67.9% men versus 52.4% women; p<0.001).
 |
Table 4 Behavioural Characteristics of Participants in Northern Ghana, 2019 |
Figure 1 shows the percentage of contraceptive use by sex. There were more women than men who reported using any type of contraceptives. There were also more females than males using MCs (23.8% of females versus 16.9% of males).
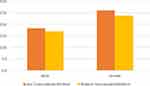 |
Figure 1 Percentage of Participants reporting Contraceptive Use by Sex in Northern Ghana, 2019. |
Figure 2 also shows the types of contraceptives used by participants. More men reported using condoms (41.1%) and depomedrol (34.0%) of men who reported using contraceptives. About twenty-one percent of the women who reported using MCs mentioned combined oral contraceptives (CoCs).
 |
Figure 2 Reported Current Use of Contraception by Sex in Northern Ghana, 2019. |
Predictors of Modern Contraceptive Use
Almost all Crude odds ratios (CORs) for sociocultural variables and behavioral constructs were significant for both men and women. Qualitative data showed that Muslims generally avoided the use of contraceptives. Below are quotes from a man and woman respectively:
Yes, in our Muslim religion, it is said that we should not practice family planning
Man; Rural Men Non-Users- FGDYes, my husband is a Muslim leader in the community, he preaches sermons to my hearing and there are times he comes home and sits me down that I should avoid the use of contraceptives or other matters related to life and religion. That a Muslim wife should not practice contraceptive
Wife; Rural Wives of Men Non-Users-FGD.
In Table 5, education was a predictor of MC in men in Model 1 and 2; particularly men with secondary education. For instance, Model 2 showed that men with secondary (AOR= 5.5 [95% CI: 1.95, 15.54]) were more likely to use MCs. However, in Model 3, the education for men was no longer significant.
 |
Table 5 Predictors of Modern Contraceptive Use in Men, Northern Ghana, 2019 |
Additionally, male farmers (in Model 3) were less likely to use MCs (AOR= 0.04 [95% CI: 0, 0.65]) than their rural counterparts; even though in Models 1 and 2 there was no significance. Similarly, in Model 1, men within the fourth wealth quintile of SES had less odds of using MCs (AOR= 0.25 [95% CI: 0.1, 0.66]) but the significance was lost in Models 2 and 3 (Table 5). Nevertheless, the influence of SES as a factor for uptake was confirmed by the FGDs in the following quote:
There are some people with the intention that they want to give birth to plenty of children. As the proverb in Dagbani says, “The person who gives birth to plenty children is wealthy”. So it is a wise saying and people keep practising it.
Wife: Wives of Men Users, FGD.Quantitative data did not show that polygamy was a significant predictor of MC use but qualitative data showed a strong link. This is shown in the following quote:
Now you cannot have three wives and again able to practice contraceptive.…
Man; Urban Men Non-User-FGD.Somebody came that she and her rival came and did jadelle; that rival came and removed hers and later went and told her husband that the rival had come to do jadelle. Therefore she came that we should remove it for her …….- Midwife: KII.
In Table 6, women who were between 40–49 years old had less odds of using MCs (AOR=0.4[95% CI: 0.18, 0.89]) but significance was lost in Model 3. Female farmers were also less likely to use MCs; even in model 3 (AOR=0.38 [95% CI: 0.18, 0.81]). Additionally, female traders had less odds of using MCs in Model 3 AOR=0.37 [95% CI: 0.14, 0.97]). The following demographic variables were not significant: age for men and women, child survival, and position of the wife in a polygamous home.
 |
Table 6 Predictors of Modern Contraceptive Use in Women, Northern Ghana, 2019 |
Under sociocultural characteristics, the “Ideal birth spacing period” was not quantitatively significant for both men and women, but qualitative data showed that postpartum spacing was practiced by participants as shown in the quote below:
One thing is that, after your wife gives birth, you must appreciate her and let her go to your family member’s home or to her relatives to stay for a while; for 2 years or a year and months and later return home. Man: RAP by Pastor.
The only knowledge we have is to stay away from your wife when the baby is very small.
FGD –Man: Men Non-UsersMoreover, men who reported, the “ideal number of children” as 10 or less, (1–5: AOR: 6.24([95% CI: 1.06, 36.81]) and 6–10: AOR: 5.62 [95% CI: 1.55, 20.39]) were more likely to use contraceptives. Women (Table 6) who reported an ideal number of children of 1–5 were more likely to use MCs (AOR:4.20 [95% CI: 1.19, 14.84). However, this predictor lost its significance in Model 3 for both men and women. The qualitative data confirmed that some men wanted more children in the following quotes: “That is why I said it depends on the man. There are some of the men who are interested in having many more children” Wife: Wives of Rural Men Users Rural: FGD
As the saying goes in Dagbani, ‘The person who gives birth to plenty children is wealthy.
Wife: Wives of Men Users: FGDFrom another perspective, we suspected that the reasons why men do not get involved in MC adoption were predictors of MC uptake and therefore we introduced these reasons into the models. Upon introduction to the model, we identified that men (Table 5) who gave the reason “unconcerned” was significant; even in model 3 [AOR: 0.07 [95% CI:0.01, 0.39]). In addition, women (Table 6) who gave the reason “nothing prevents men” from getting involved with MC adoption were strongly more likely to use modern contraceptives; even in model 3 (AOR= 15.02 [95% CI:3.54, 63.76]).
Women (Table 6) who reported that they had been successful in preventing unwanted pregnancy in the past, had greater odds of using MCs; even in Model 3 (AOR= 7.75 [95% CI: 2.00, 30.01]).
The introduction of behavioral predictors into the model in model 3 showed that men (Table 5) with good subjective norms had the strongest likelihood (AOR=17.88 [95% CI: 4.58, 69.84]) to use MCs. Women with good subjective norms also had about 3 times the odds of using MCs (Table 6). Furthermore, men (Table 5) and women (Table 6) with high PBC were about six times more likely to use MCs. Women with a sense of high self-stigma and stigma enacted were also more likely to use MCs. Finally, men and women who reported good interspousal communication on family planning, were more likely to use MCs (Men: AOR: 16.17 ([95% CI: 4.91, 53.27] Versus Women: AOR=12.79 [95% CI: 5.42, 30.20]) (Tables 5 and 6).
Quantitatively, self-stigma was not a significant predictor for men but qualitative data showed that participants with stigma were less inclined to use MCs as shown in the following quotes.
There was a time I was seated somewhere and someone came and asked me about how to use contraceptives? I responded that he could take his wife to the hospital for them to attend to her. However, he exclaimed” oyi!”(meaning ‘wow!’), I cannot do that because people will get to know about it.
Man; Men Non-Users: FGDTruly there are some people that feel shy.
Man: Men Non-Users: FGDDiscussion
We aimed at assessing demographic, sociocultural and behavioral predictors of MCs in this study. We found that more women than men (about 7%) reported using any type of contraceptives. Similarly, more women than men reported using MCs. The difference in reported MC use could be attributed to the perception of women that their partners will not accept their MC use. This implies that MC adoption was carried out covertly by women without the knowledge of their husbands. This assertion was confirmed by a midwife in the KIIs and also aligns with literature.22,23 For example, Mosha et al24 documented that women in Tanzania used the MC without the consent of their husbands to protect their health and that of their children.
Moreover, more Christians than Muslims reported using MC in terms of percentages. The odds of MC use and its association with religion could not be confirmed quantitively because the sample was highly skewed in favor of Muslims. Nevertheless, qualitative data showed that MC adoption was not patronized by Muslims. This finding is consistent with other studies in Ghana and Nigeria.25,26 The finding, however, does not align with the tenets of Islam. In the tenets of Islam, nonpermanent forms of MCs are allowed. This statement was communicated by a Muslim cleric and confirmed by literature.27 The majority of participants being Muslims serves as a point of intervention.
Men with secondary or tertiary education showed more odds of using MCs but significance was lost with the introduction of behavioral constructs. This may be attributed to the influence of behavioral predictors on the decision by educated males and the likelihood of using contraceptives. This finding may be linked to the impression that MC use will be “killing the child”28 and therefore may have had poor attitude to MCs.
SES did not have a significant association with MC uptake in men, even though men in the fourth wealth quintile in Model 1 were significantly less likely to use MCs. Qualitative data however showed that men with wealth were linked to a high number of children. This finding is contrary to results by Joshi29 and Muralidharan et al.30 One probable explanation for this variance is that in the Dagomba society, men with high number of children are considered affluent as was reported in the qualitative data. As a result, if a man is financially endowed, it is assumed that he can sustain a big family. The assertion is buttressed by the high number of children that the men desired as part of the sociocultural variables.
Women farmers and traders were less likely to use MCs; possibly because such women wanted more children to help them with work.31 However, the finding that female farmers and artisans are less likely to use MCs is contrary to expectation because women see the plight of their children when they are not well-fed.24 More research is therefore needed. Interventions were not geared towards changing the occupation of women, but rather interventions aimed at using MCs to space the children, which is accepted socio-culturally.
Finally, qualitative data showed that polygamy influenced contraceptive uptake because polygamy fueled rival competition for more children.32 There are, however, positive aspects of competition as was observed in the qualitative data. A woman adopts family planning because she perceives that the rival has a better quality of life. When the woman enquired, she realised that the co-wife used modern contraceptives to space her children. Of course, the positive aspects of competition were dependent on the approval of the husband as has been documented by Izugbara.33
Under the socio-cultural variables, men whose ideal number of children was 1–5 children and 6–10 children had greater odds of using MCs but there was a loss of significance in Model 3. Women, with an ideal number of children 1–5 were also more likely to use MCs. The desire for less number of children for both males and females is an indication of the probable presence of unmet needs.34 The finding also served as a point an intervention to help reduce the number of children participants were having.
Men who desired as many as 6–10 children were also more likely to use MC. This stands to reason because in a study population where over 40% of marriages are polygamous, it infers that men were expected to have children from all the wives while polygamous women report for themselves alone. Qualitative data confirmed men generally wanted more children. In a cultural context where men are considered wealthy if they have more children, it suggests that men who wanted less than 10 children considered that they had enough children and therefore could consider using MCs.35,36
Furthermore, when asked why males are not active in MC adoption, men who gave “unconcerned” as a reason were less likely to use MCs. The lack of interest of men in getting involved in reproductive health including contraception has been documented. Men explain that MC adoption is the business of women. This assertion has also been made in studies from Tanzania and Cameroon.24,35,36 Women who reported that “nothing prevents” men from getting involved in MC adoption were 15 times more likely to use MCs. This is an unexpected finding. Perhaps the women who gave that reason were more liberated and decided to adopt MCs. This is because it has been documented that when women are involved in decision-making in reproductive health, outcomes are better. For example, according to Mosha et al,24 women in urban areas were more likely to decide to use MCs because they felt at liberty to discuss MC adoption with their partners. Further studies are needed to ascertain the reason for the strong association.
Women who had been successful in the past in preventing pregnancy were strongly likely to use contraception. Moreover, men and women with high PBC had better odds of using MCs. This finding is consistent with previous studies.37,38 It stands to reason because when a woman has been successful in preventing pregnancy, she will find it easier to adopt modern contraception. Further studies are needed to analyze success in past pregnancy prevention and high PBC.
Subjective norms’ were the strongest proximal predictor of contraceptive uptake among men but the strength of the relationship was inconsistent with the literature because it has been documented to be the weakest TPB construct.20,37,39 The differences may be due to the interdependent culture of Dagombas. That is, the opinions of others have a significant influence on one’s decisions, while Azjen20 for example conducted his study in an individualistic society.
Both men and women with high interspousal communication increase the odds of MC use. This finding is consistent with several studies.1,8,12,31 An explanation of this finding could be that couples were able to exchange practical information regarding MC options through communication. Moreover, close communication helped to use MC efficiently and regularly.40
Both qualitative and quantitative data confirmed the presence of stigma among participants. The characteristics of the stigma were found in several ways; particularly in women. Firstly, both male and female participants denied using MCs. In some cases, a woman would go to the health facility to access family planning services under the pretense of “going to fetch water”. Secondly, stigma was observed by participants when community members were “speaking evil about you” or “you becoming the talk of the town” because participants were using MCs. One would term this type of stigma “Contraceptive Stigma”. The presence of stigma has been found to prevent other members of a community from accessing family planning services; even if clients require such services.41
Interestingly, the findings indicate that women who reported self-stigma and “enacted stigma” were more likely to use contraceptives. It may be attributed to women knowing the benefits of MCs. Therefore, even though the women felt highly stigmatized by society, they covertly adopted MCs. Such an assertion aligns with other studies.42,43 However, further studies would be needed to ascertain why women with high enacted stigma accessed MC. The presence of Contraceptive stigma presented a point of intervention.
Strengths and Limitations
This study took cognizance of male involvement in the MC adoption among couples. We also assessed behavioral outcomes in relation to MC adoption, which has not been widely studied. The study was conducted in a largely Muslim population and therefore can inform policymakers on predictors influencing MC uptake. However, the study design was cross-sectional and therefore is not as robust as the case control. Further studies using case-control would be needed.
Conclusions and Recommendations
This part of the research was the baseline assessment for a broader study which aimed at determining the effect of an intervention based on health behavior theories on outcomes of MCs including MC uptake. The demographic and socio-cultural predictors of MCs were being a Muslim (as was identified in the qualitative study) and ideal number of children. For women, barriers preventing MC uptake were being a female farmer or artisan/trader.
The behavioral construct influencing MC use in women is PBC while subjective norms mostly influence men. Participants who had high inter-spousal communication on MC adoption were more likely to use MC. Stigma (including stigma enacted) was also a predictor of MC use.
Interventions were premised on Islamic tenets as the backbone. Additionally, the presence of MC stigma was also a point of intervention.
It would therefore be instructive for health authorities to aim at interventions that increase the positive predictors of MC use and reduce the barriers to improve MC use; thereby contributing to improving MC prevalence.
Abbreviations
MC, Modern Contraceptives; TPB, Theory of Planned Behavior; PBC, Perceived Behavioral Control.
Disclosure
The authors report no conflicts of interest in this work on policy implications.
References
1. Eliason S, Awoonor-williams JK, Eliason C, Novignon J, Nonvignon J, Aikins M. Determinants of modern family planning use among women of reproductive age in the Nkwanta district of Ghana: a case – control study. Rep. 2014;11(65):1–10.
2. Apanga PA, Kumbeni MT, Ayamga EA, Ulanja MB, Akparibo R. Prevalence and factors associated with modern contraceptive use among women of reproductive age in 20 African countries: a large population-based study. BMJ Open. 2020;10(9):e041103. doi:10.1136/bmjopen-2020-041103
3. Ghana National Population Council. Ghana’s Development Agenda and Population Growth: The Unmet Need for Family Planning National Population Council with the Support of the POLICY Project. Accra; 2006.
4. GSS, GHS, ICF. Ghana Maternal Health Survey 2017: Key Findings. Rockville, Maryland, USA: GSS, GHS, ICF; 2018.
5. Achana FS, Bawah AA, Jackson EF, et al. Spatial and socio-demographic determinants of contraceptive use in the Upper East region of Ghana. Reprod Health. 2015;12(1):1–10. doi:10.1186/s12978-015-0017-8
6. Apanga PA, Adam MA. Factors influencing the uptake of family planning services in the Talensi district, Ghana. Pan Afr Med J. 2015;20:1–9. doi:10.11604/pamj.2015.20.10.5301
7. Blackstone SR, Nwaozuru U, Iwelunmor J. Factors influencing contraceptive use in Sub-Saharan Africa: a systematic review. Int Q Community Health Educ. 2017;1(1):1–13.
8. Adongo PB, Tabong PT, Azongo TB, et al. A comparative qualitative study of misconceptions associated with contraceptive use in southern and northern Ghana. Front Public Health. 2014;2:1–7.
9. Amalba A, Mogre V, Appiah MNA, Mumuni WA. Awareness, use and associated factors of emergency contraceptive pills among women of reproductive age (15–49 years) in Tamale, Ghana. BMC Women's Health. 2014;14(114):1–6. doi:10.1186/1472-6874-14-114
10. Yidana A, Ziblim S, Azongo TB, Abass YI. Socio-Cultural determinants of contraceptives use among adolescents in Northern Ghana. Public Heal Res. 2015;5(2013):1.
11. Tilahun T, Coene G, Luchters S, et al. Family planning knowledge, attitude and practice among married couples in Jimma Zone, Ethiopia. PLoS One. 2013;8(4):1–8. doi:10.1371/journal.pone.0061335
12. Tumlinson K, Speizer IS, Davis JT, Fotso JC, Kuria P, Archer LH. Partner communication, discordant fertility goals, and contraceptive use in urban Kenya. Afr J Reprod Health. 2013;17(3):79–90.
13. Shattuck D, Kerner B, Gilles K, Hartmann M, Ng T, Guest G. Encouraging contraceptive uptake by motivating men to communicate about family planning. Malawi Male Motiv Proj. 2011;101(6):1089–1095.
14. GSS, GHS, ICF International. Ghana Demographic and Health Survey, 2014. Rockville, Maryland, USA: GSS, GHS, ICF International; 2015.
15. Hermanides H, Holman R, Gras L, et al. Loss to follow-up and mortality rates in HIV-1-infected patients in Curaçao before and after the start of combination antiretroviral therapy. AIDS Res Hum Retroviruses. 2013;29(10):1300–1305. doi:10.1089/aid.2012.0362
16. Sibanda EL, Weller IVD, Hakim JG, Cowan FM. The magnitude of loss to follow-up of HIV-exposed infants along the prevention of mother-to-child HIV transmission continuum of care: a systematic review and meta-analysis. AIDS. 2013;27:2787–2797. doi:10.1097/QAD.0000000000000027
17. Beebe J. Rapid Assessment Process: An Introduction. Rowman Altamira; 2004.
18. Brafford LJ, Beck K. Development and validation of a condom self-efficacy scale for college students. J Am Coll Heal. 1991;39(5):219–225. doi:10.1080/07448481.1991.9936238
19. James-Hawkins L, Broaddus M. The association of attitudes about contraceptives with contraceptive use in a random sample of Colorado women. Soc Sci J. 2016;53(2):167–173. doi:10.1016/j.soscij.2016.03.001
20. Ajzen I. The theory of planned behaviour: reactions and reflections. Psychol Heal. 2011;26(9):1113–1127. doi:10.1080/08870446.2011.613995
21. Hall KS, Manu A, Morhe E, et al. Development and validation of a scale to measure adolescent sexual and reproductive health stigma: results from young women in Ghana. J Sex Res. 2018;55(1):60–72. doi:10.1080/00224499.2017.1292493
22. Kushitor M, Henry EG, Danquah A, et al. Covert contraceptive use amongst the urban poor in Accra, Ghana: experiences of health providers. Reprod Health. 2022;1–12. doi:10.1186/s12978-022-01516-5
23. Akoth C, Oguta JO, Gatimu SM. Prevalence and factors associated with covert contraceptive use in Kenya: a cross- sectional study. BMC Public Health. 2021;21:4–11. doi:10.1186/s12889-021-11375-7
24. Mosha I, Ruben R, Kakoko D. Family planning decisions, perceptions and gender dynamics among couples in Mwanza, Tanzania: a qualitative study. BMC Public Health. 2013;13(523):1–13. doi:10.1186/1471-2458-13-523
25. Doctor HV, Phillips JF, Sakeah E. The influence of changes in women’s religious affiliation on contraceptive use and fertility among the Kassena-Nankana of Northern Ghana. Stud Fam Plann. 2009;40(2):113–122. doi:10.1111/j.1728-4465.2009.00194.x
26. Ijadunola MY, Abiona TC, Ijadunola KT, Afolabi OT, Esimai OA, OlaOlorun FM. Male Involvement in family planning decision making in Ile-Ife, Osun State, Nigeria. Afr J Reprod Health. 2010;14(4):43–50.
27. Atighetchi D. The position of Islamic tradition on contraception. Med Law. 1994;13:1994.
28. El Hamri N. Approaches to family planning in Muslim communities. J Fam Plann Reprod Heal Care. 2010;36(1):27–31. doi:10.1783/147118910790291019
29. Joshi L. Male participation in family planning: human behaviour perspective. J Nepal Health Res Counc. 2015;13(3):4–8.
30. Muralidharan A, Fehringer J, Pappa S, Rottach E, Das M, Mandal M. Transforming Gender Norms, Roles, and Power Dynamics for Better Health: Evidence from a Systematic Review of Gender-Integrated Health Programs in Low- and Middle- Income Countries. Washington DC: Futures Group, Health Policy Project; 2015.
31. Wegs C, Creanga AA, Galavotti C, Wamalwa E. Community dialogue to shift social norms and enable family planning: an evaluation of the family planning results initiative in Kenya. PLoS One. 2016;11(4):1–23. doi:10.1371/journal.pone.0153907
32. Bove R, Valeggia C. Polygyny and women’s health in sub-Saharan Africa. Soc Sci Med J. 2009;68:21–29. doi:10.1016/j.socscimed.2008.09.045
33. Izugbara C, Ibisomi L, Ezeh AC, Mandara M. Gendered interests and poor spousal contraceptive communication in Islamic northern Nigeria. J Fam Plan Reprod Heal Care. 2010;36(4):219–224. doi:10.1783/147118910793048494
34. Bradley J, Mursagulova N, Nosa M, Searing H. Supply and demand challenges to modern contraceptive use in Azerbaijan. Eur J Contracept Reprod Health Care. 2007;12(June):175–183. doi:10.1080/13625180701330530
35. Greene ME. Changing women and avoiding men health programmes. IDS Bull. 2000;31(2):49–59. doi:10.1111/j.1759-5436.2000.mp31002007.x
36. Egbe TO, Ketchen SA, Egbe E-N, Ekane GEH, Belley-Priso E. Risk factors and barriers to male involvement in the choice of family planning methods in the buea health district, south west region, Cameroon: a cross-sectional study in a semi-urban area. Women Heal Open J. 2016;1(3):82–90. doi:10.17140/WHOJ-1-112
37. Mayaki F, Koubenan DR. Impact of perceptions about children and procreation on family- planning practices. J Reprod Infant Psychol. 2014;32(3):292–303. doi:10.1080/02646838.2014.888545
38. Delva W, Michielsen K, Meulders B, Groeninck S. HIV prevention through sport: the case of the Mathare Youth Sport Association in Kenya. AIDS Care. 2010;22(8):1012–1020. doi:10.1080/09540121003758606
39. Kalolo A, Kibusi SM. The influence of perceived behaviour control, attitude and empowerment on reported condom use and intention to use condoms among adolescents in rural Tanzania. Reprod Health. 2015;12(105):1–9. doi:10.1186/s12978-015-0097-5
40. Link CF. Spousal communication and contraceptive use in Rural Nepal: an event history analysis. Stud Fam Plann. 2012;42(2):83–92. doi:10.1111/j.1728-4465.2011.00268.x
41. Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Heal. 2013;103(5):813–821. doi:10.2105/AJPH.2012.301069
42. Koffi TB, Weidert K, Bitasse EO, et al. Engaging men in family planning: perspectives from married in Lomé, Togo. Glob Heal Sci Pract. 2018;6(2):317–329. doi:10.9745/GHSP-D-17-00471
43. Anasel MG, Mlinga UJ. Determinants of contraceptive use among married women in Tanzania: policy implicationa. Af Populat Stud. 2014;28(2):978–988. doi:10.11564/28-0-550
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
