Back to Journals » Clinical Interventions in Aging » Volume 19
Development and Validation of a New Nomogram Model for Predicting Acute Ischemic Stroke in Elderly Patients with Non-Valvular Atrial Fibrillation: A Single-Center Cross-Sectional Study
Received 25 August 2023
Accepted for publication 28 December 2023
Published 10 January 2024 Volume 2024:19 Pages 67—79
DOI https://doi.org/10.2147/CIA.S437065
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Maddalena Illario
Jiongchao Guo,1,* Yuan Zhou,1,* Bingfeng Zhou2
1Department of Cardiology, the Third Affiliated Hospital of Anhui Medical University, Hefei, Anhui, People’s Republic of China; 2Department of Cardiology, Hefei BOE Hospital, Hefei, Anhui, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Bingfeng Zhou, Department of Cardiology, Hefei BOE Hospital, Hefei, Anhui, 230000, People’s Republic of China, Tel +8613956078803, Email [email protected]
Background and Aims: Non-valvular atrial fibrillation (NVAF) patients face a 3– 5 times greater risk of acute ischemic stroke (AIS) compared to those without NVAF. This study aims to establish a novel clinical prediction model for AIS in elderly patients with NVAF by incorporating relevant biomarker indicators.
Methods: A total of 301 individuals diagnosed with NVAF were selected for this investigation at the Third Affiliated Hospital of Anhui Medical University. Based on the presence of AIS, patients were categorized into two groups: the Stroke Cohort and the Non-Stroke Cohort. Predictor screening was performed using the least absolute shrinkage and selection operation (LASSO) regression algorithm. The binary logistic regression equation was applied to fit the model, followed by internal validation using the bootstrap resampling method (1000 times). Receiver operating characteristic (ROC) curve, calibration degree curve plots, and clinical decision curve analysis (DCA) were generated, respectively. Finally, a nomogram was constructed to present the prediction model.
Results: The final results of this study revealed that neutrophil-to-lymphocyte ratio (NLR), red cell distribution width (RDW), lipoprotein(a) (Lp(a)), systolic pressure, history of stroke, hyperlipidemia were independent risk factors for AIS in elderly patients with NVAF (P< 0.05). And the high-density lipoprotein cholesterol (HDL-C) was an independent protective factor (P< 0.05). By incorporating these indicators, a nomogram prediction model for predicting AIS in elderly patients with NVAF was constructed. Comparative analysis between the nomogram predictive model and CHA2DS2-VASc score revealed that the AUC of the nomogram predictive model surpassed that of the CHA2DS2-VASc score (AUC: 0.881vs 0.850).
Conclusion: NLR, RDW, Lp(a), SP, history of stroke, hyperlipidemia, and HDL-C emerge as independent prognostic factors for acute ischemic stroke in elderly patients with non-valvular atrial fibrillation. The predictive utility of the nomogram model may potentially surpass that of the CHA2DS2-VASc scoring system.
Keywords: acute ischemic stroke, non-valvular atrial fibrillation, nomogram, clinical risk prediction model
Introduction
Atrial fibrillation (AF) is a form of electrophysiological anomaly leading to the loss of synchronized atrial contractions, thereby elevating the risk for thrombus formation and cardioembolic ischemic stroke (IS).1 In the United States, from 2010 to 2030, the projected number of atrial fibrillation cases is expected to rise from 1.2 million to 2.6 million, with the incidence increasing from 5.2 per 10,000 people to 12.1 per 10,000 people.2 The overall stroke incidence rate among AF patients in China is 24.8%, with NVAF accounting for around 24.2% of cases. A stratified, multi-stage sampling study conducted from 2020 to 2021 involving 114,039 residents across 22 provinces, autonomous regions, and municipalities in mainland China revealed that the incidence of AF among residents aged ≥18 is 1.6%.3
Due to the extended average lifespan and the high prevalence of AF-related risk factors, the incidence of AF is anticipated to escalate further. AF significantly augments the risk of IS occurrence.4,5 AF patients face a 3–5 times greater risk of AIS compared to those without NVAF. Moreover, AF-associated strokes often exhibit higher rates of disability and fatality, resulting in elevated hospitalization and mortality rates. Some studies have pointed out that the rhythm control of AF patients is associated with a higher hospitalization rate.6 Consequently, the primary focus of AF intervention lies in stroke prevention, chiefly through anticoagulation therapy.7 A recent study indicated that there was no significant difference in the major prognosis between AF patients in the effective therapeutic range group for warfarin and those in the non-vitamin K antagonist oral anticoagulants (NOACs) group. Both of these medications can be considered as the first choice for anticoagulant therapy in AF patients.8,9 Currently, the CHA2DS2-VASc scoring system has been predominantly employed to assess the risk of stroke in individuals with AF. This scoring system represents the most widely utilized method for stratifying stroke risk in atrial fibrillation patients. Nevertheless, this scoring system possesses certain shortcomings, such as its reliance solely on clinical variables, and lack of relevant biomarkers. Additionally, despite its high sensitivity to stroke risk prediction, the CHA2DS2-VASc score demonstrates relatively low specificity.10,11 Research has indicated suboptimal performance of this score in predicting strokes or other ischemic cerebrovascular events in real-world settings,12,13 particularly within specific populations, such as those with impaired kidney function and Asian patients.14,15
Considering the lower age threshold for increased stroke risk among Asian AF patients, the CHA2DS2-VASc score might lead to insufficient anticoagulation treatment in this demographic. Inadequate anticoagulation is a significant factor contributing to stroke incidence among atrial fibrillation patients.16 As the understanding of AF’s pathophysiology and associated biomarkers deepens, Hijazi and colleagues proposed the ABC stroke score—a novel biomarker-based predictive scoring system for stroke or systemic embolism risk,17 It remains unaffected by underlying comorbidities. However, the latest 2020 ESC guidelines do not prioritize the use of the ABC score, as it does not exhibit a clear advantage over the CHA2DS2-VASc score in long-term stroke prediction efficacy, thereby constraining its clinical application.18
Currently employed models for predicting stroke risk in atrial fibrillation patients each exhibit limitations. Hence, seeking a new predictive model suitable for the region to assess the risk of AIS in NVAF patients could lead to ongoing improvements in the model’s performance and enhanced predictive efficacy. Therefore, this study aims to establish a novel clinical prediction model for AIS in elderly patients with NVAF by incorporating relevant biomarker indicators.
Methods
Study Subjects
A total of 301 elderly individuals (age > 60 years) were selected consecutively from May 2020 to May 2023 for this investigation at the Third Affiliated Hospital of Anhui Medical University. They were patients diagnosed with NVAF. Their clinical data was amassed for retrospective analysis. The principle of blinding was applied during data collection, and the clinical data collectors were unaware of the purpose and design of this study. At the same time, the assessors of the CHA2DS2-VASc score were also unaware of whether AIS had occurred in NVAF patients in this study. Based on the presence of AIS, patients were categorized into two groups: the Stroke Cohort (143 cases, NVAF patients with concurrent AIS) and the Non-Stroke Cohort (158 cases, patients with isolated NVAF). Inclusion criteria consisted of ① ECG or 24-hour Holter monitoring confirming episodes of atrial fibrillation, with patients being above 60 years of age; ② Echocardiography confirming non-valvular heart disease; ③ All stroke cases adhered to ischemic stroke diagnostic criteria, confirmed through cranial CT or MRI scans showing cerebral infarction. Additionally, the duration of atrial fibrillation exceeded the duration of stroke history; ④ Complete clinical data, especially comprehensive biomarker test results. Exclusion criteria encompassed any of the following: ① Hemorrhagic stroke; ② History of rheumatic heart disease or echocardiographic evidence of rheumatic heart valve disease; ③ Post-artificial heart valve replacement; ④ History of malignancy. (Figure 1).
 |
Figure 1 Flow chart of the study selection. Abbreviation: NVAF, non-valvular atrial fibrillation. |
Guidelines for Diagnosis
The diagnostic criteria for atrial fibrillation align with the relevant standards outlined in the “2023 Chinese Guidelines for Atrial Fibrillation Diagnosis and Treatment”. Acute ischemic stroke diagnostic criteria adhere to the relevant standards delineated in the “2018 Chinese Guidelines for the Diagnosis and Treatment of Acute Ischemic Stroke”.
Observational Indices
Patients’ baseline data was retrospectively collected via the hospital’s medical record system. This included age, gender, smoking history, alcohol consumption history, comorbidities (hypertension, diabetes, coronary heart disease, stroke, heart failure, hyperlipidemia), atrial fibrillation type, and CHA2DS2-VASc score. Additional data collected upon admission encompassed blood pressure, fasting laboratory biomarker indices, which included: triglycerides (TG), total cholesterol (TC), HDL-C, low-density lipoprotein cholesterol (LDL-C), Lp(a), homocysteine (HCY), fasting blood glucose (FBG), uric acid, serum creatinine (Scr), cystatin C, glomerular filtration rate (GFR), D-dimer, neutrophil count (NC), lymphocyte count (LC), platelet count (PLT), hematocrit (HCT), and RDW. Furthermore, the neutrophil-to-lymphocyte ratio (NLR) was computed. Echocardiographic parameters included: left atrial dimension (LAD), left ventricular end diastolic dimension (LVEDD), and left ventricular ejection fraction (LVEF).
Statistic Analysis
Two researchers employed SPSS 26.0 (IBM Corporation, Armonk, NY, USA) for data recording and statistical analysis. The LASSO algorithm was implemented utilizing the glmnet package in R version 4.2.2 (Chinese Academy of Sciences). Normally distributed numerical variables were presented as mean ± standard deviation (SD), while non-normally distributed variables were presented as median (interquartile range). Categorical data was conveyed as frequency (percentage). Variable selection was conducted through the LASSO regression algorithm, employing 10-fold cross-validation with a P-value threshold of <0.1. Optimal penalty coefficients were determined based on λ (Lambda) corresponding to one standard error, minimizing mean squared error (MSE). The model was fitted using binary Logistic regression equation, and internal model validation was carried out via bootstrap resampling (1000 iterations). Model performance and calibration were evaluated through the ROC curve, calibration curve, and DCA. Furthermore, a nomogram was created to visually present the predictive model. Statistical significance was set at α = 0.05 for all tests. All tests were two-tailed, with P < 0.05 considered statistically significant.
Result
Comparison of Baseline Data
Patients in the Stroke Cohort exhibited higher levels of age, proportion with a history of hypertension, stroke history, hyperlipidemia, systolic blood pressure, persistent atrial fibrillation, CHA2DS2-VASc score, TC, HDL-C, Lp(a), D-dimer, NC, NLR, and RDW compared to the Non-Stroke Cohort. These differences attained statistical significance (P<0.05). Conversely, LC and GFR were lower in the Stroke Cohort compared to the Non-Stroke Cohort, also exhibiting statistical significance (P<0.05). Other variables’ comparisons yielded no statistically significant differences (P>0.05) (Table 1).
 |
Table 1 Comparison of Baseline Data in the Non-Stroke Group and Stroke Group |
LASSO Regression for Predictive Variable Selection
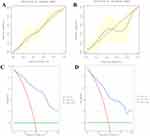
After integrating the 15 significantly different variables from the comparative analysis of atrial fibrillation patients’ general characteristics into the LASSO regression, a refined selection resulted in 8 meaningful variables. The outcomes of the LASSO regression indicated that systolic blood pressure, stroke history, hyperlipidemia, HDL-C, Lp(a), RDW, NLR, and D-dimer were predictive factors for AIS in elderly patients with NVAF (Figure 2A and B).
 |
Figure 2 (A and B) Predictor plots screened by least absolute shrinkage and selection operator (LASSO) regression analysis. |
Binary Logistic Regression
The 8 predictive variables identified through LASSO regression were incorporated into a multivariable binary logistic regression. The results revealed that systolic blood pressure, stroke history, hyperlipidemia, Lp(a), RDW, and NLR were independent risk factors for AIS in elderly patients with NVAF (P<0.05). HDL-C emerged as a protective factor for AIS in elderly patients with NVAF (P<0.05). D-dimer displayed no significant statistical meaning (P>0.05) (Table 2).
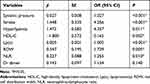 |
Table 2 Multivariate Logistic Regression Analysis of Influencing Factors for AIS in Elderly Patients with NVAF |
Construction and Validation of Predictive Model
Building upon the 6 independent risk factors (systolic blood pressure, history of stroke, hyperlipidemia, Lp(a), RDW, NLR) and 1 protective factor HDL-C, as identified through LASSO regression and multivariable logistic regression, a nomogram predictive model was established. Each variable was allocated a corresponding score on the x-axis. Summation of scores across variables yielded the total score associated with AIS occurrence in NVAF patients. Higher total scores on the x-axis corresponded to an increased likelihood of AIS occurrence (Figure 3). For example, consider an NVAF patient with SP of 130 mmHg, corresponding to a score of approximately 18; Hyperlipidemia, corresponding to a score of approximately 25; Lp(a) of 400, corresponding to a score of approximately 35; RDW of 13, corresponding to a score of approximately 20; NLR of 8, corresponding to a score of approximately 30; HDL-C of 2, corresponding to a score of approximately 25; and stroke, corresponding to a score of approximately 24. By adding up the aforementioned scores, the total score is 177. According to the corresponding AIS occurrence probability chart, the probability of experiencing MACE is approximately 90%, and the patient is considered to be at high risk for AIS (Figure 3).
Internal model validation demonstrated that the AUC for the modeling dataset was 0.915, while the validation dataset exhibited an AUC of 0.860. This indicates a robust predictive capacity in the model established by this study (Figure 4A). The model’s goodness of fit was assessed using a calibration curve. Results showcased that the slope of predicted probability closely aligned with actual probability, highlighting the model’s strong predictive performance (Figure 4B).
DCA was plotted with probability on the x-axis and clinical net benefit rate on the y-axis. Both the modeling and validation datasets displayed clinical net benefit rates ranging from 0% to 100% (Figure 5A and B). This suggests a high clinical benefit of our model in predicting NVAF patients with concurrent AIS (Figure 5C and D).
Comparison of Nomogram Predictive Model and CHA2DS2-VASc Score Prediction Efficacy
Comparative analysis between the nomogram predictive model and CHA2DS2-VASc score revealed that the AUC of the nomogram predictive model surpassed that of the CHA2DS2-VASc score (AUC of nomogram predictive model: 0.881, 95% CI: 0.8430–0.9193, sensitivity: 0.7552, specificity: 0.8797; AUC of CHA2DS2-VASc-60 score: 0.850, 95% CI: 0.8177–0.8965, sensitivity: 0.7832, specificity: 0.7841) (Figure 6A). The DCA plots for both models exhibited clinical net benefit rates spanning 0% to 100%, signifying high clinical utility for both models. (Table 3) (Figure 6B).
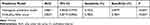 |
Table 3 Comparison of ROC Curve Between Nomogram Predictive Model and CHA2DS2-VASc Score |
Discussion
The risk of AIS among NVAF patients is 3 to 5 times higher than that among individuals without AF, and AF-associated strokes tend to be more debilitating and fatal.7 Hence, the focus of AF intervention centers on stroke prevention. While CHA2DS2-VASc may be better at identifying truly low-risk patients, its scoring capacity is not discriminatory enough for truly high-risk, elderly patients.19 In light of this, the quest for novel predictive models tailored to assessing cerebrovascular risk in AF patients can lead to continuous refinement, thereby bolstering predictive efficacy and reducing stroke rates. The use of additional clinical, laboratory, imaging markers, and novel stroke prediction models may further assist in the decision to anticoagulate the AF patient for stroke prevention. This study’s findings indicated that systolic blood pressure, history of stroke, hyperlipidemia, Lp(a), RDW, and NLR are independent risk factors for AIS in elderly patients with NVAF. HDL-C is identified as a protective factor for AIS in elderly patients with NVAF (P<0.05). Furthermore, The predictive utility of the nomogram model may potentially surpass that of the CHA2DS2-VASc scoring system.
Before our study, previous research has proposed several alternative stroke prediction models for AF. First is The Thrombolysis in Myocardial Infarction-Atrial Fibrillation (TIMI-AF) score. This model is based on the AF-TIMI 48 randomized clinical trial.20 A single-center retrospective study of NVAF patients indicated that the TIMI-AF score outperformed CHA2DS2-VASc in identifying cardiovascular event risk and disabling stroke.21 However, this model is primarily focused on patients receiving anticoagulant therapy, and evidence supporting its applicability in untreated patients is lacking. Further validation in larger prospective studies is necessary. In comparison, our study’s model incorporates inflammation and lipid-related markers and defines applicability to individuals over 60 years old, potentially offering higher predictive value.21 Additionally, another predictive model known as The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) score, based on the self-titled cohort, was created to better identify those patients at highest risk for stroke while also considering bleeding risk.22 This model incorporates renal dysfunction into CHADS2 and strongly considers age categories.23 It may aid in risk stratification for atrial fibrillation patients with very low to low stroke risk (CHA2DS2-VASc score of 0 or 1 [male] and 1 or 2 [female]).24 However, in comparison to our study, this model does not include hyperlipidemia, lipid, and inflammation related markers. Furthermore, it lacks substantial evidence from large-scale prospective studies, thus requiring further validation of its reliability. Our study builds upon previous research on biomarker prediction in NVAF patients and seeks to explore new and improved prediction models for assessing AIS risk in NVAF patients. We believe that future research in this direction should prioritize the predictive value of lipid and inflammation-related markers.
The present study unveils that the NLR is notably elevated within the stroke-afflicted group when compared to the non-stroke cohort, signifying NLR is an independent risk factor for the occurrence of AIS in elderly patients with NVAF. The NLR stands as a potential novel inflammatory marker. Within a cohort study conducted by W. SALIBA encompassing 32,912 Israeli AF patients, a conspicuous correlation between the NLR and the inaugural occurrence of stroke in AF patients has been discerned.25 This association possesses a dose-response pattern, remaining independent from factors included in the CHA2DS2-VASc score.25 Furthermore, NLR retains a distinct association with the presence of left atrial thrombi and an independent escalation in stroke risk within the AF cohort.13,25–27 The prospective mechanisms underlying these interconnections are multifaceted. On one facet, neutrophils contribute to the progress of cerebral infarction by secreting a multitude of inflammatory mediators, exacerbating endothelial cell dysfunction, destabilizing the blood-brain barrier, and inciting secondary cerebral injuries or hemorrhagic conversions.28–30 On the other hand, heightened lymphocyte levels potentiate the upregulation of anti-inflammatory cytokines such as Interleukin (IL)-10, consequently repressing inflammatory cytokines like Tumor Necrosis Factor-α and IL-6. This orchestrated interplay engenders an anti-inflammatory effect, thereby fostering neural function amelioration.31 Moreover, empirical substantiation underscores the notion that lymphocytes harbor neuroprotective attributes. Regulatory T cells and B cells perform a regulatory function in AIS, culminating in the mitigation of ischemic tissue volume reduction and the improvement of neural function deficiency.32 In culmination, the NLR emerges as a latent prognostic biomarker for the risk of cerebrovascular events in atrial fibrillation patients. Within observational studies encompassing NVAF-associated Ischemic Stroke, NLR exhibits a correlation with elevated inpatient mortality rates and augmented National Institutes of Health Stroke Scale (NIHSS) scores.33 These findings allude to the conceivable utility of NLR as an auxiliary biomarker for stratifying the risk of AIS. Therefore, the inclusion of NLR within our model is necessary.
Within this study, it has been ascertained that the RDW emerges as an independent risk factor of AIS occurrence in NVAF patients. Within a comprehensive cohort analysis, encompassing a substantial populace, a median follow-up of 18.8 years revealed a twofold surge in the incidence of AIS among the high RDW subset of NVAF individuals, an alignment that resonates harmoniously with the outcomes of the present study.34 The potential mechanisms underlying the augmentation of AIS jeopardy in NVAF patients precipitated by heightened RDW are multifarious. Elevated RDW levels, indicative of a compromised homeostasis of erythrocytes, might be underpinned by the effects of inflammation and oxidative stress. Moreover, an elevated RDW might instigate atrial cell damage, thereby instigating atrial structural remodeling and thrombus formation.35 Previous studies have clarified a meaningful correlation between RDW values and the CHA2DS2-VASc scoring of NVAF patients, concurrently underscoring RDW as an independent prognosticator for elevated CHA2DS2-VASc scores.36 Consequently, it is imperative that we incorporate RDW within our predictive model.
In this study, it has been observed that the levels of Lp(a) conspicuously exceed those of the non-AIS subgroup. The outcomes of the logistic regression analysis substantiate Lp(a) as an independent risk factor for AIS occurrence in NVAF patients, an alignment that harmonizes with antecedent studies.37,38 Elevated serum Lipoprotein (a) is an identified risk element for left atrial thrombosis in the milieu of chronic AF.39 A Mendelian randomization study by Mohammadi-Shemirani posits Lp(a) as a latent pathogenic peril associated with atrial fibrillation.40 The precise pathophysiological mechanisms by which Lp(a) augments the vulnerability of NVAF patients to AIS remain nebulous, potentially involving the following reasons: Lp(a) assumes a role in fomenting inflammatory responses, potentially detracting from atrial remodeling and electrophysiological conduction intrinsic to atrial fibrillation.33 The oxidized phospholipids which are inclined to conjoin with Lp(a) may upregulate inflammatory mediators such as interleukin-8 and monocyte chemotactic protein, thereby exacerbating the inflammatory cascade.33,34 Additionally, due to the structural resemblance between the surface of lipoprotein (a) and tissue plasminogen activator, Lp(a) is enabled to perturb fibrinolysis by interfering with plasminogen binding.35 Furthermore, Lp(a) is endowed with the capacity to neutralize tissue factor pathway inhibitors, which counters thrombogenesis via the extrinsic coagulation pathway.36 Therefore, the conclusions drawn from this study are consistent with previous research, supporting the inclusion of these two indicators in our model.
The present study reveals that elevated systolic blood pressure and hyperlipidemia are independent risk factors for the occurrence of AIS in patients with NVAF. The 2021 APHRS guidelines indicated that the etiology of AIS in NVAF patients is multifaceted, encompassing elevated systolic blood pressure and hyperlipidemia.41 This concurs with the findings of our study, underscoring the imperative of rigorously managing lipid levels and blood pressure in elderly individuals with NVAF, and considering pharmacological intervention for those with inadequate control.41 Notably, a history of prior stroke independently heightens the likelihood of AIS incidence in NVAF patients. In the subset of patients already afflicted by ischemic stroke, the prevalence of prior stroke is higher, which was similar to the outcomes in our study.42
Elevated HDL-C levels are regarded in this study as a protective factor against AIS development in NVAF patients. Lopez et al in their study encompassing a cohort of 13,969 individuals followed over a mean period of 18.7 years, of which 1433 experienced atrial fibrillation, demonstrated that an HDL-C level ≥1.55 mmol/L was a protective factor against atrial fibrillation after adjusting for age, gender, and ethnicity.43 Furthermore, prior research has illustrated a discernible correlation between HDL-C and the incidence of NVAF-associated cerebral infarction, a finding that resonates with our study results.44–46 The precise pathophysiological mechanisms by which HDL-C confers protection against AIS in NVAF patients remain to be fully elucidated. However, it is conceivable that HDL-C exerts its effect through modulating endothelial functionality, exerting anti-inflammatory and antioxidative influences, inhibiting cellular apoptosis, and mitigating platelet activation.
This study introduces an innovative nomogram predictive model for predicting the occurrence of AIS in elderly patients with NVAF. Within this model, we have incorporated novel laboratory-associated predictive factors (NLR, Lp(a), RDW, HDL-C) alongside clinically pertinent variables (systolic blood pressure, prior history of stroke, hyperlipidemia). The proposed model may present superior predictive capabilities than the CHA2DS2-VASc score. This model furnishes clinicians with an innovative tool for predicting the risk of AIS in elderly NVAF patients, enabling early initiation of anticoagulant therapy to enhance patient prognosis. Currently, anticoagulant therapy for patients with NVAF is primarily guided by the CHA2DS2-VASc score. However, the lack of laboratory markers in this scoring system, may lead to delays in initiating anticoagulant treatment for some high-risk patients. Our study proposes a new model that incorporates four laboratory markers: Lp(a), HDL-C, RDW, and NLR. These are all laboratory markers easily obtainable during hospitalization. For patients with a CHA2DS2-VASc score of 0 or 1, which typically does not recommend anticoagulant therapy, a reassessment can be conducted using these markers to reduce the risk of thrombosis. This approach is particularly applicable for evaluating thrombotic risk in patients without prior cardiac dysfunction or diabetes. Moreover, traditional scoring systems entail intricacies during application. By contrast, the proposed scoring system’s simplicity, cost-effectiveness, and user-friendly parameter acquisition make it amenable to widespread clinical utilization.
Limitations
The present study is subject to the following constraints: 1. This study constitutes a single-center retrospective investigation, characterized by a relatively modest sample size, thereby potentially engendering selection bias. 2. The study’s failure to discern between distinct atrial fibrillation subtypes has led to an absence of differentiation concerning cerebral infarction etiology. 3. The study has omitted previously well-established markers such as cardiac troponin and natriuretic peptides, which definitively impact atrial fibrillation-related cerebral infarction. 4. The model has yet to stratify the elderly population by age, thus leaving the predictive value across diverse elderly age segments uncertain. 5. Previous studies have suggested that race and geographical location can influence the risk of thrombosis. However, since this study was conducted at a single center located in a geographically homogeneous area where over 95% of the population belongs to the same race, it was difficult to collect data on variables related to different geographic locations and races. Further multicenter studies are needed to clarify these factors. 6. This study mainly focused on people over 60 years old, and thus did not explore the factors that may affect thrombosis risk in different age groups of elderly individuals. This is considered one of the limitations of this study.
Future Directions
This study builds upon previous research on biomarker prediction for assessing the risk of AIS in patients with NVAF. It aims to explore new and improved predictive models for evaluating AIS risk in NVAF patients. The results of this study indicate that lipid and inflammatory markers such as RDW, NLR, HDL-C, and Lp(a) may have predictive value for AIS in NVAF patients. Therefore, in future research in this area, the predictive value of lipid and inflammation-related markers in predicting AIS combined with NVAF should be emphasized. Additionally, the proposed predictive model in this study needs further validation in future research.
Conclusion
NLR, RDW, Lp(a), SP, history of stroke, hyperlipidemia, and HDL-C emerge as independent prognostic factors for acute ischemic stroke in elderly patients with non-valvular atrial fibrillation. The predictive utility of the nomogram model may potentially surpass that of the CHA2DS2-VASc scoring system.
Abbreviations
NVAF, Non-valvular atrial fibrillation; AIS, acute ischemic stroke; LASSO, least absolute shrinkage and selection operation; ROC, regression algorithm; Receiver operating characteristic; DCA, curve; Clinical decision curve analysis; NLR, neutrophil-to-lymphocyte ratio; RDW, red cell distribution width; Lp(a), lipoprotein(a); SP, systolic pressure; AUC, the area under the ROC curve; AF, Atrial fibrillation; TG, triglycerides; TC, total cholesterol; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; HCY, homocysteine; FBG, fasting blood glucose; UA, uric acid; SCr, serum creatinine; GFR, glomerular filtration rate; NC, neutrophil count; LC, lymphocyte count; PLT, platelet count; HCT, hematocrit; LAD, left atrial dimension; LVEDD, left ventricular end diastolic dimension; LVEF, left ventricular ejection fraction; MSE, minimizing mean squared error; IL-10, Interleukin; NIHSS, National Institutes of Health Stroke Scale; TIMI-AF, The Thrombolysis in Myocardial Infarction-Atrial Fibrillation score; ATRIA, Anticoagulation and Risk Factors in Atrial Fibrillation score.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request. The data are not publicly available due to their containing information that could compromise the privacy of patients.
Ethics Approval and Consent to Participate
The study protocol and informed consent procedures were approved by the Ethics Committee of the Third Affiliated Hospital of Anhui Medical University. All methods were performed following the Declaration of Helsinki. Informed written consent for publication without direct personal identification details was obtained from all the participants.
Acknowledgments
The authors would like to extend their sincere thanks to MM F, YT H, and YZ for their contribution to reviewing this manuscript and the acquisition of data. We also extend our gratitude to JC G, YH, BF Z, and MM F for their contributions. We would like to express our gratitude and give credit to Ref 17 for proposing the ABC stroke risk score, which served as a valuable reference in our study.
Author Contributions
Jiongchao Guo and Yuan Zhou have made equal contributions and should be considered as a co-first authors. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare no conflicts of interest statement.
References
1. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019;74(1):104–132. doi:10.1016/j.jacc.2019.01.011
2. Khurshid S, Healey JS, McIntyre WF, Lubitz SA. Population-Based Screening for Atrial Fibrillation. Circulation Res. 2020;127(1):143–154. doi:10.1161/CIRCRESAHA.120.316341
3. Of the Report TW. Report on cardiovascular health and diseases in China 2021: an updated summary. J Geriatr Cardiol. 2023;20(6):399–430. doi:10.26599/1671-5411.2023.06.001
4. Chung MK, Refaat M, Shen W-K, et al. Atrial Fibrillation: JACC Council Perspectives. J Am Coll Cardiol. 2020;75(14):1689–1713. doi:10.1016/j.jacc.2020.02.025
5. Baman JR, Passman RS. Atrial Fibrillation. JAMA. 2021;325(21):2218. doi:10.1001/jama.2020.23700
6. Kılıç R, Güzel T, Aktan A, Demir M, Arslan B, Ertaş F. The effect of treatment strategy on long-term follow-up results in patients with nonvalvular atrial fibrillation in Turkey: AFTER-2 subgroup analysis. Aging Clin Exp Res. 2023;35(8):1695–1704. doi:10.1007/s40520-023-02467-y
7. Ding M, Ebeling M, Ziegler L, Wennberg A, Modig K. Time trends in atrial fibrillation-related stroke during 2001-2020 in Sweden: a nationwide, observational study. Lancet Reg Health Eur. 2023;28:100596. doi:10.1016/j.lanepe.2023.100596
8. Aktan A, Güzel T, Aslan B, et al. Comparison of the real-life clinical outcomes of warfarin with effective time in therapeutic range and non-vitamin K antagonist oral anticoagulants: insight from the AFTER-2 trial. Kardiologia Polska. 2023;81(2):132–140. doi:10.33963/KP.a2022.0287
9. Güzel T, Aktan A, Kılıç R, et al. Oral Anticoagulant Use and Long-Term Follow-Up Results in Patients with Non-valvular Atrial Fibrillation in Turkey AFTER-2 Study. Anatol J Cardiol. 2022;26(7):567–576. doi:10.5152/AnatolJCardiol.2022.1597
10. Friberg L, Rosenqvist M, Lip GYH. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33(12):1500–1510. doi:10.1093/eurheartj/ehr488
11. Odum LE, Cochran KA, Aistrope DS, Snella KA. The CHADS₂versus the new CHA2DS2-VASc scoring systems for guiding antithrombotic treatment of patients with atrial fibrillation: review of the literature and recommendations for use. Pharmacotherapy. 2012;32(3):285–296. doi:10.1002/j.1875-9114.2012.01023.x
12. Quinn GR, Severdija ON, Chang Y, Singer DE. Wide Variation in Reported Rates of Stroke Across Cohorts of Patients With Atrial Fibrillation. Circulation. 2017;135(3):208–219. doi:10.1161/CIRCULATIONAHA.116.024057
13. Borre ED, Goode A, Raitz G, et al. Predicting Thromboembolic and Bleeding Event Risk in Patients with Non-Valvular Atrial Fibrillation: a Systematic Review. Thromb Haemost. 2018;118(12):2171–2187. doi:10.1055/s-0038-1675400
14. Alkhouli M, Friedman PA. Ischemic Stroke Risk in Patients With Nonvalvular Atrial Fibrillation: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;74(24):3050–3065. doi:10.1016/j.jacc.2019.10.040
15. Kodani E, Akao M. Atrial fibrillation and stroke prevention: state of the art-epidemiology and pathophysiology: new risk factors, concepts and controversies. Eur Heart J Suppl. 2020;22(Suppl O):O1–O13. doi:10.1093/eurheartj/suaa176
16. Polymeris AA, Meinel TR, Oehler H, et al. Aetiology, secondary prevention strategies and outcomes of ischaemic stroke despite oral anticoagulant therapy in patients with atrial fibrillation. J Neurol Neurosurg Psychiatry. 2022;93(6):588–598. doi:10.1136/jnnp-2021-328391
17. Hijazi Z, Lindbäck J, Alexander JH, et al. The ABC (age, biomarkers, clinical history) stroke risk score: a biomarker-based risk score for predicting stroke in atrial fibrillation. Eur Heart J. 2016;37(20):1582–1590. doi:10.1093/eurheartj/ehw054
18. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
19. Jagadish PS, Kabra R. Stroke Risk in Atrial Fibrillation: beyond the CHA2DS2-VASc Score. Curr Cardiol Rep. 2019;21(9):95. doi:10.1007/s11886-019-1189-6
20. Fanola CL, Giugliano RP, Ruff CT, et al. A novel risk prediction score in atrial fibrillation for a net clinical outcome from the ENGAGE AF-TIMI 48 randomized clinical trial. Eur Heart J. 2017;38(12):888–896. doi:10.1093/eurheartj/ehw565
21. Pérez Cabeza AI, Bravo Marques R, Chinchurreta Capote PA, et al. TIMI-AF score and cardiovascular events in vitamin K antagonists-naïve outpatients with atrial fibrillation. Clin Cardiol. 2018;41(9):1252–1258. doi:10.1002/clc.23035
22. Singer DE, Chang Y, Borowsky LH, et al. A new risk scheme to predict ischemic stroke and other thromboembolism in atrial fibrillation: the ATRIA study stroke risk score. J Am Heart Assoc. 2013;2(3):e000250. doi:10.1161/JAHA.113.000250
23. van den Ham HA, Klungel OH, Singer DE, Leufkens HGM, van Staa TP. Comparative Performance of ATRIA, CHADS2, and CHA2DS2-VASc Risk Scores Predicting Stroke in Patients With Atrial Fibrillation: results From a National Primary Care Database. J Am Coll Cardiol. 2015;66(17):1851–1859. doi:10.1016/j.jacc.2015.08.033
24. Deering TF. Incorporating Stroke and Bleeding Risk Stratification Tools into Atrial Fibrillation Management Making Sense of the Alphabet Soup. J Atr Fibrillation. 2017;9(6):1497. doi:10.4022/jafib.1497
25. Saliba W, Barnett-Griness O, Elias M, Rennert G. Neutrophil to lymphocyte ratio and risk of a first episode of stroke in patients with atrial fibrillation: a cohort study. J Thromb Haemost. 2015;13(11):1971–1979. doi:10.1111/jth.13006
26. Deng Y, Zhou F, Li Q, et al. Associations between neutrophil-lymphocyte ratio and monocyte to high-density lipoprotein ratio with left atrial spontaneous echo contrast or thrombus in patients with non-valvular atrial fibrillation. BMC Cardiovascular Disorders. 2023;23(1):234. doi:10.1186/s12872-023-03270-3
27. Yalcin M, Aparci M, Uz O, et al. Neutrophil-lymphocyte ratio may predict left atrial thrombus in patients with nonvalvular atrial fibrillation. Clin Appl Thromb Hemost. 2015;21(2):166–171. doi:10.1177/1076029613503398
28. Heijman J, Voigt N, Nattel S, Dobrev D. Cellular and molecular electrophysiology of atrial fibrillation initiation, maintenance, and progression. Circulation Res. 2014;114(9):1483–1499. doi:10.1161/CIRCRESAHA.114.302226
29. Y-F H, Chen Y-J, Lin Y-J, Chen S-A. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. 2015;12(4):230–243. doi:10.1038/nrcardio.2015.2
30. Hermann DM, Kleinschnitz C, Gunzer M. Implications of polymorphonuclear neutrophils for ischemic stroke and intracerebral hemorrhage: predictive value, pathophysiological consequences and utility as therapeutic target. J Neuroimmunol. 2018;321:138–143. doi:10.1016/j.jneuroim.2018.04.015
31. Iadecola C, Buckwalter MS, Anrather J. Immune responses to stroke: mechanisms, modulation, and therapeutic potential. J Clin Invest. 2020;130(6):2777–2788. doi:10.1172/JCI135530
32. Liesz A, Zhou W, S-Y N, et al. Boosting regulatory T cells limits neuroinflammation in permanent cortical stroke. J Neurosci. 2013;33(44):17350–17362. doi:10.1523/JNEUROSCI.4901-12.2013
33. Fang Y-N, Tong M-S, Sung P-H, et al. Higher neutrophil counts and neutrophil-to-lymphocyte ratio predict prognostic outcomes in patients after non-atrial fibrillation-caused ischemic stroke. Biomed J. 2017;40(3):154–162. doi:10.1016/j.bj.2017.03.002
34. Hald EM, Løchen M-L, Lappegård J, et al. Red Cell Distribution Width and Risk of Atrial Fibrillation and Subsequent Thromboembolism: the Tromsø Study. TH Open. 2020;4(3):e280–e7. doi:10.1055/s-0040-1716417
35. Korantzopoulos P, Kolettis TM, Galaris D, Goudevenos JA. The role of oxidative stress in the pathogenesis and perpetuation of atrial fibrillation. Int J Cardiol. 2007;115(2):135–143. doi:10.1016/j.ijcard.2006.04.026
36. Kurt M, Tanboga IH, Buyukkaya E, Karakas MF, Akçay AB, Sen N. Relation of red cell distribution width with CHA2DS2-VASc score in patients with nonvalvular atrial fibrillation. Clin Appl Thromb Hemost. 2014;20(7):687–692. doi:10.1177/1076029613478157
37. Ding WY, Protty MB, Davies IG, Lip GYH. Relationship between lipoproteins, thrombosis, and atrial fibrillation. Cardiovascular Res. 2022;118(3):716–731. doi:10.1093/cvr/cvab017
38. Chapman MJ, Huby T, Nigon F, Thillet J. Lipoprotein (a): implication in atherothrombosis. Atherosclerosis. 1994;110:S69–S75. doi:10.1016/0021-9150(94)05385-V
39. Igarashi Y, Yamaura M, Ito M, Inuzuka H, Ojima K, Aizawa Y. Elevated serum lipoprotein(a) is a risk factor for left atrial thrombus in patients with chronic atrial fibrillation: a transesophageal echocardiographic study. Am Heart J. 1998;136(6):965–971. doi:10.1016/S0002-8703(98)70151-6
40. Mohammadi-Shemirani P, Chong M, Narula S, et al. Elevated Lipoprotein(a) and Risk of Atrial Fibrillation: an Observational and Mendelian Randomization Study. J Am Coll Cardiol. 2022;79(16):1579–1590. doi:10.1016/j.jacc.2022.02.018
41. Chao T-F, Joung B, Takahashi Y, et al. 2021 Focused Update Consensus Guidelines of the Asia Pacific Heart Rhythm Society on Stroke Prevention in Atrial Fibrillation: executive Summary. Thromb Haemost. 2022;122(1):20–47. doi:10.1055/s-0041-1739411
42. Wańkowicz P, Nowacki P, Gołąb-Janowska M. Atrial fibrillation risk factors in patients with ischemic stroke. Arch Med Sci. 2021;17(1):19–24. doi:10.5114/aoms.2019.84212
43. Lopez FL, Agarwal SK, Maclehose RF, et al. Blood lipid levels, lipid-lowering medications, and the incidence of atrial fibrillation: the atherosclerosis risk in communities study. Circ Arrhythm Electrophysiol. 2012;5(1):155–162. doi:10.1161/CIRCEP.111.966804
44. Guan B, Li X, Xue W, et al. Blood lipid profiles and risk of atrial fibrillation: a systematic review and meta-analysis of cohort studies. J Clin Lipidol. 2020;14(1):133–142.e3. doi:10.1016/j.jacl.2019.12.002
45. Zhang -X-X, Wei M, Shang L-X, et al. LDL-C/HDL-C is associated with ischaemic stroke in patients with non-valvular atrial fibrillation: a case-control study. Lipids Health Dis. 2020;19(1):217. doi:10.1186/s12944-020-01392-7
46. Suzuki M, Furuya K, Ozawa M, et al. Complex Aortic Arch Atherosclerosis in Acute Ischemic Stroke Patients with Non-Valvular Atrial Fibrillation. J Atheroscler Thromb. 2021;28(7):776–785. doi:10.5551/jat.58339
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.