Back to Journals » Integrated Pharmacy Research and Practice » Volume 13
Drug Use Evaluation of Tenofovir/Lamivudine/Dolutegravir (TLD) Fixed-Dose Combination for Initiation and Transition Among HIV-Infected Individuals Attending Lumame Primary Hospital, North West Ethiopia
Authors Tegegne BA , Alehegn AA , Kassahun M
Received 25 January 2024
Accepted for publication 12 April 2024
Published 18 April 2024 Volume 2024:13 Pages 31—42
DOI https://doi.org/10.2147/IPRP.S455351
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Walid Al-Qerem
Bantayehu Addis Tegegne,1 Agumas Alemu Alehegn,2 Mengistie Kassahun3
1Department of Pharmacy, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia; 2Department of Pharmacy, Lumame Primary Hospital, Lumame, Ethiopia; Health Supplies and Laboratory Equipments Management Directorate Director, Amhara National Regional State Public Health Institute, Bahirdar, Ethiopia; 3Department of Public Health, College of Health Science, Debre Markos University, Debre Markos, Ethiopia
Correspondence: Bantayehu Addis Tegegne, Email [email protected]
Background: A key strategy for quality improvement is drug use evaluation, which looks at the safe, appropriate use of medication principles. Tenofovir/Lamivudine/Dolutegravir (TLD-FDC) usage has not yet been sufficiently examined in published literature. The purpose of this study was to assess how TLD were used by HIV-positive patients Using WHO drug use evaluation standards in Lumame Primary Hospital, North West Ethiopia.
Methods: Using WHO drug use evaluation standards, a retrospective study design was used to evaluate the appropriateness of TLD use. Systematic random sampling was utilized to gather patient medical records containing TLD. Accordingly, 100 records that met the inclusion criteria were selected and reviewed between April 1 and 15, 2021. Five criteria, namely, indication, dose, contraindication, drug interaction, and TLD safety monitoring were used to evaluate the appropriateness of TLD utilization.
Results: 80% of patients were transited to TLD from other regimens. The median time on TLD was found to be 13 months with 9 months to 18 months IQR. The latest CD4 count as well as CD4 count at the initiation or transition of TLD was not done for 75% and 89% of the patients, respectively. 3/4 (75%) of the patients were found to have a scheduled medication refill history. TLD dosing, indications, and contraindications were found to be 100% appropriate. No, TLD safety monitoring tests were done for 21% of the patients in this study. However, viral load, liver/kidney function, and serum creatinine tests were done for 77% (95% CI: 74%– 79%), 5% (95% CI: 2%– 8%), and 14% (95% CI: 11%– 17%) of the patients, respectively. More over, In 93% (95% CI: 91%– 95%) of the patients, the TLD interaction was appropriate; in 7%, it was not. All recording, documenting, and reporting technologies were available and used efficiently, except for the Electronic Dispensing Tool.
Conclusion: Generally, good adherence to national and WHO guidelines was obtained regarding dose, indication, and contraindications. However, improvement in safety monitoring tests and CPT utilization is recommended. Drug interactions satisfied the majority of the criteria’s threshold, while certain standards were not followed.
Keywords: drug use evaluation, lumame primary hospital, Ethiopia, fixed dose combination: tenofovir/lamivudine/dolutegravir
Introduction
The backbone for HIV treatment has been the combination of at least two nucleosides (nucleotide) reverse transcriptase inhibitors (NRTIs) and a third drug from any of the following medication groups: Non-nucleoside reverse transcriptase inhibitors (NNRTIs); Protease inhibitors (PIs); Integrase strand transfer inhibitors (INSTIs): Dolutegravir (DTG) and Raltegravir (RAL). Due to the use of antiretroviral therapy (ART), HIV infection is no longer considered a fatal condition but rather a chronic infection that can be managed over time.1–4 Optimized antiretroviral therapy (ART) regimens can alleviate the burden on health systems and lower the likelihood of the spread of HIV by improving medication adherence, treatment results, and quality of life for individuals living with HIV.5,6
The World Health Organization (WHO) advised including extremely potent ART with lower toxicity and resistance and proven efficacy across varied populations in HIV therapy regimens to attain 95% virologic suppression.7 Afterward, it was suggested that DTG be used as the favored first-line regimen in conjunction with an optimized NRTI backbone: TDF plus 3TC or FTC.8 Additionally, adults, adolescents, and children who have not responded to a non-DTG-based first-line regimen are advised to use DTG as the preferred ARV medication for second-line ART.9 To preserve the benefits of ART, effective prescription, dispensing, and usage along with continuous availability and adherence are essential.10,11
Although the efficacy of ART is indisputable, certain issues persist. Because the treatments cannot completely eradicate the virus, patients will need to take them for the remainder of their lives, putting them at risk for dangerous side effects, drug interactions, and drug resistance.12 On the other hand, inappropriate use of medications is a worldwide issue that primarily affects developing nations. Evidence suggests that prescribing, dispensing, and using ARTs without following treatment protocols is prevalent. This nonadherence may in some manner lead to a rise in pretreatment HIV drug resistance, treatment failure, and resource waste among people beginning or continuing first-line ART in many low- and middle-income countries at large.13
The Ethiopian government has implemented DTG-based regimens in the 2018 National Comprehensive HIV Prevention, Care, and Treatment Guidelines following the WHO’s recommendation. This is a part of the government’s continuous efforts to stop HIV transmission and improve the quality of HIV care and treatment services.5 The use of Tenofovir/Lamivudine/Dolutegravir (TLD) began in Ethiopia in February 2019. It was first presented in the research domain (Lumame Primary Hospital) on April 1, 2019.6 However, there are currently no published studies assessing the appropriate use of ART medications like the TLD in Ethiopia. Hence, assessment drug use patterns helps to spot gaps in the use of medications and put initiatives in place that encourage responsible drug use.14,15
One of the instruments available for assessing the healthcare system is Drug Use Evaluation or Drug Utilization Evaluation (DUE).11,16 DUE, is a crucial quality improvement tool for assessing the safe and appropriate use of pharmaceuticals, medical procedures, and new research ideas. It can evaluate the actual pharmaceutical administration or dispensing procedure (including the right indications, drug selection, dosage, delivery method, length of therapy, and drug interactions) as well as the treatment’s result.17
Thus, the primary objective of the present investigation is to evaluate the rationality of TLD regimen usage. The results of the study will provide fresh data that managed healthcare systems can use to better comprehend, interpret, assess, and enhance the prescription, administration, and use of pharmaceuticals. The results will also assist stakeholders in monitoring TLD use by preventing the establishment of resistant strains, reducing needless spending, minimizing adverse effects, and, most importantly, guaranteeing patient compliance.
Material and Methods
Study Area, Design, and Period
The study was carried out at Lumame Primary Hospital’s HIV care clinic in northwest Ethiopia. The hospital’s catchment area includes 157,048 people. There is a working ART clinic there, and about 271 HIV-positive patients are cared for by an active ART team consisting of physicians, pharmacists, and nurses. We evaluated the level of appropriateness for the use of TLD initiation and transition using WHO drug use evaluation criteria as well as expert thresholds for undertaking drug use evaluation for TLD at Lumame Primary Hospital ART clinic.
The high consumption rate of this medication was used as the criterion for selecting this regimen in this study. The study comprised all HIV-positive patients who were on ART at Lumame Primary Hospital receiving ART between April 1, 2019, and April 1, 2021. Between April 1 and April 15, 2021, the medical records of TLD recipients were reviewed retrospectively. The appropriateness of TLD use was assessed using established criteria developed by WHO as a reference (Table 1) 1 and National Consolidated Guidelines for HIV Prevention, Care, and Treatment.5 The hospital’s Drug and Therapeutics Committee (DTC) approved these criteria after reviewing the WHO’s updated recommendations for first- and second-line antiretroviral regimens in 2020,1 Ethiopian, National Consolidated Guidelines for Comprehensive HIV Prevention, Care and Treatment, 20185 and implementation manual for DTG rollout and ART optimization in Ethiopia, 2019. To assess the appropriateness of TLD utilization, five criteria were used: indication for use, dose, contraindication, drug interaction, and TLD safety monitoring. The presence of a single error in either of the individual criteria was deemed inappropriate. After the criteria are determined, thresholds or standards (benchmarks) are chosen for each criterion to specify the objectives or standards for criteria compliance. An indicator of a threshold is the percentage of charts or records that either adhere to or exceed the specified medical requirements. Though in practice a smaller percentage is more suitable to allow for deviations from standard medication prescription, the ideal threshold would be 100%. For many criteria, therefore, a threshold of 90–95% is usually utilized, under which corrective actions are implemented; however, each case needs to be thoroughly examined before drawing any conclusions.18 A descriptive presentation of the suitability of TLD utilization was made.
 |
Table 1 Drug Use Evaluation Criteria for TLD Initiation and Transition.1,5,19 |
Source and Study Population
This study’s source population consisted of all the medical records of ART patients at Lumame Primary Hospital. A study cohort consisting of ART patients with current TLD regimens was selected, and samples were taken for the actual retrospective analysis from this group.
Inclusion and Exclusion Criteria
All ART patient charts containing the TLD regimen were included in this retrospective study. Nevertheless, the study did not include records for patients who were transferred out or dropped out, had incomplete information, or were only taking TLD for a month.
Study Variables (Dependent and Independent Variables)
The dependent variable for this study was TLD regimen utilization practice. Patient demographics, indications /contraindications, dosing, drug interactions, safety monitoring parameters, availability of recording and documenting, and reporting materials were the independent variables that affect TLD regimen utilization.
Sample Size Determination and Sampling Procedure
In the HIV care clinic of this hospital, 271 patients (263 adults and 8 children) were currently on ART. Based on the requirements set forth by the Joint Commission on Accreditation of Healthcare Organizations (JCAHCO), at least 5% of cases must be reviewed if the average number of cases per quarter exceeds 600; if the average number of cases per quarter is less than 600, at least 30 cases must be reviewed; and if there are fewer than 30 cases per quarter, then 100% of the cases must be reviewed.20 In our setting, about 214 patients were currently taking the TLD regimen. Thus, the total sample size was around 100 ART patient charts, which is significantly more than the minimal sample size (n=30) recommended by JCAHCO to generate a higher point estimate of the population.
The medical record numbers of all ART patients with TLD were listed in the sampling frames, and then systematic random sampling was used to obtain the previously mentioned sample size. The card numbers were used to locate the patient’s medication records. By dividing the study population by the actual sample size, the sampling interval was computed (Kth=214/100 =2.14). Therefore, starting with an initial sample that was chosen at random, the samples were obtained by selecting every second patient’s medical records that satisfied the inclusion requirements, until the sample size was reached. Consequently, 100 patient medical records that satisfied inclusion criteria were chosen.
Data Collection Tools and Procedures
Data were collected from patient cards without disruption of usual patient care or health care processes using a data collection format.21 The data collection format included two parts. The first section includes information regarding the patient source, age, weight, sex, address, TLD status, duration of TLD, Cotrimoxazole preventive therapy, CD4 count, clinical Pneumocystis carinii pneumonia (PCP), clinical stage of AIDS, other regimens the patient has ever used, any ADR experiences and medication refill history. The second part includes information regarding TLD indications, contraindications, dose, medicine interaction, and safety monitoring parameters. Format for collection of data on the availability of recording, documenting, and reporting tools in the ART Pharmacy was also utilized. The specific types of data necessary to evaluate TLD regimen utilization were recorded from sampled patient charts in data collection format. Well-oriented two clinical pharmacists and one general practitioner were involved to shoulder the overall data collection process and effectively discharge their tasks. The principal investigator guided and supervised the data collection process daily.
Quality Control of Data
Principal investigators provided orientation to data collectors and utilized well-designed data-collecting formats to guarantee the quality of the collected data. The data collection formats were pretested to check the validity and reliability of the format. The principal investigator underwent frequent checks on the data collection process to ensure the completeness and consistency of the collected data before undergoing data processing and analysis.
Data Analysis and Manipulation
The collected data were checked for accuracy, consistency, omission, and irregularities. Then it was summarized using standard summary forms. Frequencies and percentages were calculated using Microsoft Excel 2013. The findings were reported in frequencies and percentages with 95% confidence intervals and evaluated according to established criteria and thresholds from both a statistical perspective and a clinical viewpoint.
Results
The Sociodemographic Characteristics
A total of 100 medical charts of patients with TLD fulfilling all inclusion criteria were identified and reviewed. 52%t of the patients were referred from other health facilities, while 48% of the patients were directly starting their ART from this health facility. Based on the documented values, 92% of the patients had a baseline age of 10–49 years and the rest 8% were > 49 years. On the other hand, 22% of the patients had a current age of > 49 years and the remaining 78% were 10–49 years. The mean baseline age was 29 years+3.89 years SD. Current mean age 31 years + 3.92 years SD. Male patients accounted for 41% and females were 59%. Most of the patients were from urban areas (66%). The mean baseline and current weight of the patients were 51.03 kg and 53.90 kg, respectively (Table 2).
 |
Table 2 Socio-Demographic Characteristics of Study Patients, Lumame Primary Hospital, April 2021 (N=100) |
Treatment and Clinical Patient Profiles
As indicated in Table 3, 80% of patients were transited to TLD from other regimens, and 20% of patients initiated TLD directly. Among these transited patients, 60 (75%) of the patients were taking TDF+3TC+EFV and 15 (19%) patients were taking, AZT+3TC+NVP and 5 (6%) were taking other regimens including AZT-3TC-EFV; TDF/3TC/NVP before switching to TLD. Among the 100 patients taking TLD, 45%, 48%, and 7% of patients were taking the drug for a duration of 2–10, 11–20, and >20 months, respectively. The median time on TLD was found to be 13 months with 9 months to 18 months IQR. Only 35% of patients were currently on CPT (Cotrimoxazole preventive therapy). On the other hand, CPT was not started or not documented for 48% of patients, and 17% of patients discontinued CPT. No documented clinical PCP and adverse drug reaction (ADR) experiences were found during the review of the charts.
Currently, 97% of the patients were WHO clinical stage 1, and only 1% and 2% of the patients were found to be in stages 2 and 3 respectively. The latest CD4 count as well as CD4 count at the initiation or transition of TLD was not done for 75% and 89% of the patients, respectively. 15% of the patients were with a latest CD4 count of > 350 cells/mm3 and 10% were with a latest CD4 count of < 350 cells/mm3. On the other hand, CD4 counts of > 350 cells/mm3 and < 350 cells/mm3 were documented in only 5% and 6% of the patients at the initiation and transition of TLD. Three-fourths (75%) of the patients were found to have a scheduled medication refill history.
 |
Table 3 Treatment Overview and Clinical Profile of Research Participants, Lumame Primary Hospital, April 2021 (N=100) |
Adherence to Treatment Guidelines on the Use of TLD
Table 4 illustrates the findings of treatment guidelines compliance about indications, dosage, interactions between medications, and TLD monitoring.
 |
Table 4 TLD Use Pattern for the Study Patients, Lumame Primary Hospital, April 2021 (N=100) |
TLD Safety Monitoring
As summarized in Table 4, no TLD safety monitoring test was done for 21% of the patients in this study. However, viral load, liver/kidney function, and serum creatinine tests were done for 77% (95% CI: 74%–79%), 5% (95% CI: 2%–8%), and 14% (95% CI: 11%–17%) of the patients, respectively.
Appropriate TLD Use
Regarding the overall evaluation of TLD, Table 5 shows that excellent outcomes were achieved when it came to indication, dosage, and contraindications (all 100% suitable). In 93% (95% CI: 91%–95%) of the patients, the TLD interaction was appropriate; in 7%, it was not.
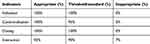 |
Table 5 Summary of Appropriate TLD Utilization Practice for the Study Patients, Lumame Primary Hospital, April 2021 (N=100) |
Availability of Recording/Documenting/Reporting Tools in the ART Pharmacy
The availability of recording/documenting/reporting tools in the ART pharmacy was checked during the study period and summarized in Table 6. In the study, all tools, except the Electronic Dispensing Tool (EDT), were available and effectively used.
 |
Table 6 Summary of the Availability of Recording/Documenting/Reporting Tools in ART Pharmacy During the Study Period, Lumame Primary Hospital, April 2021 |
Discussion
The WHO states that drug use/utilization evaluation (DUE) addresses the social, medical, and economic consequences of pharmaceutical advertising, distribution, prescription, and usage in communities. Evaluation of DUE is a useful method for figuring out whether or not different medications are being used appropriately, and it considerably supports clinical pharmacy practice and pharmacy service delivery. Hospitals DUE is a methodical way to compare drug administration procedures to guidelines or benchmarks. Initiatives to enhance patient outcomes will continue to be included in the DUE initiative.16,22
TLD, a single daily dose regimen that is safer and more effective for HIV-positive individuals, is being launched in African countries. Patients who exhibit virological failure and potential medication resistance may still be moved to therapy with TLD despite the growing accessibility of viral load (VL) testing.23
In this qualitative study, we investigated the past experiences of the TLD regimen use for Initiation and Transition among HIV-positive individuals visiting the ART clinic at Lumame Primary Hospital, Ethiopia. For this regimen’s evaluation, 100 medical records from TLD patients were chosen at random. Although this regimen is new (2–23 months of TLD), the medication refill history revealed that approximately 3/4 (75%) of the patients collect TLD according to their schedule (appointment date).
A crucial element in any pharmacological therapy’s effectiveness is adherence. In particular adherence to ARV medications is the most important factor in predicting HIV viral load control and survival for people with HIV.10 Medication nonadherence is a significant barrier to achieving positive health outcomes, particularly for patients suffering from chronic diseases.24 Poor treatment adherence may be caused by the nature of the disease, treatment protocols, medication side effects, or patient beliefs.25 During the current study, adherence to treatment guidelines in terms of indications, dosing, contraindications, drug interaction, and safety monitoring parameters was reviewed to assess the appropriate use of TLD.
We are unable to compare the practices of this institution to those in other clinical settings because, as far as we are aware, no published research on the evaluation of TLD use has been done. Scientific data on drug use assessments of other ART regimens or even other forms of surveillance are scarce. As a result, the findings were discussed along with the criteria and thresholds developed from National and WHO Consolidated Guidelines. Good outcomes were obtained in the dose, indication, and contraindication scenarios where the result is similar to the 100% threshold value in the overall evaluation of TLD use.1,19
The observed data, however, indicated some deviation from the threshold value in terms of TLD drug interaction. The simultaneous use of drugs is recommended in certain situations based on pharmacological rationality and a thorough understanding of potential interactions. In this study, TLD drug interaction was appropriate in 93% of the cases, which is higher than the 90% threshold.1,19 However, 3% of the patients were taking anticonvulsants, and 4% were taking Rifampicin along with TLD.
DTG has a lesser likelihood of drug-drug interactions than NNRTIs and boosted PIs; but, because of the possibility of chelation, it should not be used in conjunction with laxatives, multivitamin supplements, or antacids that contain cations.26 DTG is inhibited by polyvalent cations (calcium, magnesium, iron, and aluminum). Many pregnant women are prescribed prenatal vitamins containing calcium and iron, as well as medications containing other polyvalent cations such as magnesium or aluminum. It is possible to prevent these interactions by taking DTG two hours before or six hours after consuming drugs or other medicines that contain these compounds.27
Drugs that induce the transporters UDP Glucuronosyltransferase Family 1 Member A1 (UGT1A1) and P-glycoprotein as well as CYP3A4 lower DTG levels. Rifampin, Carbamazepine, Phenobarbital, Phenytoin, and EFV are examples of such medications that should not be taken in conjunction with DTG. To overcome the interaction, the DTG dosing frequency should be increased to twice daily in cases where co-administration is required. Rifampicin’s induction effect may persist even after stopping, and DTG dose adjustment should be considered for up to two weeks after TB treatment is completed.27 When metformin is combined with DTG, the pharmacokinetics of the drug are altered, resulting in increased levels of the drug. DTG inhibits an efflux transporter involved in the elimination of metformin. When taken concurrently, it is advised to keep metformin dosage to a maximum of 1 g per day.28
The concentrations of DTG at the trough were reduced by 37% when dolutegravir and artemether-lumefantrine were administered together. The estimated reductions in the DTG trough concentrations and the Area under the curve (AUC) were 42 and 24%, respectively, when dolutegravir and artesunate-amodiaquine were administered together.29
Another indicator looked at during the study was TLD safety monitoring s. Laboratory tests may be carried out initially to assess immunological function, anemia, and the existence of liver or renal disease. Liver function testing with these assays should be closely monitored in people with co-infection with hepatitis B or C or other liver disorders.5 To detect therapy failure and ascertain whether the client is qualified for DTG transition, viral load testing is also necessary. WHO guidelines state that routine viral load monitoring is a good practice, but it should not be necessary to switch to optimal regimens.30
By blocking the renal Organic Anion Transporter-2 (OCT-2), DTG may result in a slight rise in serum creatinine. Although it usually appears within the first four weeks of treatment, the rise is not a real decrease in renal function or its glomerular filtration rate (GFR). Normal serum creatinine levels are increased by 10–20 µmol/L due to DTG. It is connected to how DTG affects the secretion of tubular creatinine and does not signify a deterioration in kidney function.31
According to the findings of this study, the viral load test was the most frequently performed (77%), but practice in other test parameters (liver/kidney function and serum creatinine test) was poor (5%–14%), and the TLD safety monitoring test was not performed in 21% of the patients, which could be due to a lack of necessary materials for the test or the negligence of health care providers.
Recording, reporting, and documentation are required for the ART clinic and pharmacy services. Checking the use and availability of different instruments in the ART pharmacy was part of the validation process for such acts. Every component, except for EDT, was present and operating as it should have. At service delivery sites, EDT assists with managing the distribution and supply of ART. Positive judgments regarding medicine quantification can be made by health managers utilizing system data, and they can enhance the delivery of pharmaceutical services.32
Limitations of the Study
Because of possible imperfections in documentation completeness, the study’s retrospective design may have an impact on the quality of our results.
Conclusion and Recommendations
According to the results of the current study, the Lumame Primary Hospital ART clinic follows the national and WHO consolidated ART guidelines regarding dosage, indication, and contraindications. These guidelines support the WHO recommendation of DTG in conjunction with a tailored nucleoside reverse transcriptase inhibitor backbone, such as TDF and 3TC or FTC (TLD). The majority of patients have their medications refilled regularly. The recording and reporting systems were encouraging. However, there was some variation in terms of drug interactions, and safety monitoring tests for the use of this drug were also discovered to be ineffective. We believe that future research should look into the underlying factors that contributed to the observed gaps to improve patient care in those hospitals. Furthermore, all health professionals must maintain ongoing awareness and communication about TLD use.
Abbreviations
AIDS, Acquire immunodeficiency syndrome; ART, Antiretroviral therapy; ARV, Antiretroviral; ASM, Appointment Spacing Model; DTG, Dolutegravir; DTC, Drug and Therapeutic Committee; DUE, Drug Use Evaluation; EDT, Electronic Dispensing Tool; EFV, Efaverenz; FDC, Fixed Dose Combination; HAART, Highly Active Anti-Retroviral Therapy; HIV, Human immunodeficiency virus; INSTI, Integrase Strand Transfer Inhibitors; JCAHCO, Joint Commission on Accreditation of Healthcare Organizations; 3TC, Lamivudine; NNRTI, Non-Nucleoside Reverse Transcriptase Inhibitors; Nucleoside (and Nucleotide) Reverse Transcriptase Inhibitors; PCP, Pneumocystis carinii pneumonia; PI, Protease Inhibitors; TDF, Tenofovir Disoproxil Fumarate; TLD, Tenofovir + Lamivudine + Dolutegravir; TLE, Tenofovir + Lamivudine + Efaverenz; WHO, World Health Organization.
Data Sharing Statement
The manuscript contained all the required information.
Ethics Approval and Consent to Participate
The ethical committee at Lumame Hospital granted ethical clearance and approval for this study, which was carried out per the Declaration of Helsinki’s ethical standards. The study’s reference number is LPH/242/2021. The need for informed consent was waived by the Lumame Hospital ethics committee, and the privacy and confidentiality of all patients’ medical records data were properly secured at all times. Since there are currently no published studies assessing ART medications like the TLD FDC in Ethiopia.
Acknowledgments
We appreciate Lumame Hospital allowing us to perform the research on drug usage evaluation. We want to express our sincere appreciation to Global Health Supply Chain -Procurement and Supply Management for their technical assistance with the creation of this research. We are grateful for data gatherers as well.
Disclosure
The authors declared that there are no competing interests in this work.
References
1. World Health Organization. Updated Recommendations on First-Line and Second-Line Antiretroviral Regimens and Post-Exposure Prophylaxis and Recommendations on Early Infant Diagnosis of HIV: Interim Guidelines: Supplement to the 2016 Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection. World Health Organization; 2018.
2. Umar D, Waziri B, Ndagi U, Mohammed S, Usman N, Abubakar-Muhammad H. Impact of tenofovir/lamivudine/dolutegravir (Tld) on the health-related quality of life and clinical outcomes of HIV/AIDS patients at a tertiary health facility in Niger State. 2020. doi:10.21203/rs.3.rs-127277/v1Corpus
3. Dyer M, Kerr C, Fine SM, et al. Comprehensive primary care for adults with HIV [internet]. Baltimore (MD): Johns Hopkins University; 2022 Dec. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567851/
4. Federal democratic republic of Ethiopia ministry of health NCGfCHP. Care Treat. 2018.
5. Federal democratic republic of Ethiopia ministry of health, national consolidated guidelines for comprehensive HIV prevention. Care Treat. 2018.
6. Federal democratic republic of Ethiopia ministry of health, implementation manual for DTG rollout and ART optimization in Ethiopia. 2019.
7. World Health Organization. Transition to New Antiretroviral Drugs in HIV Programmes: Clinical and Programmatic Considerations. World Health Organization; 2017.
8. Katbi M, Adeoye O, Adedoyin A, Faturiyele I, Adegboye A, Bello M. Virologic response among key populations living with HIV following a switch to dolutegravir-based regimen in Southern Nigeria. Int J Virol AIDS. 2020;7:069.
9. Paul NI, Ugwu RO. Dolutegravir (DTG) based fixed dose combination (FDC) of tenofovir/lamivudine/dolutegravir (TLD) and viral load suppression in children in port harcourt, Nigeria. J Sci Res Rep. 2020;52–59. doi:10.9734/jsrr/2020/v26i230224
10. Sohler N, Slawek D, Earnshaw V, et al. Drug use and HIV medication adherence in people living with HIV. Subs abu. 2021;42(3):310–316. doi:10.1080/08897077.2019.1706695
11. Mekonnen BD, Ayalew MZ, Tegegn AA. Rational drug use evaluation based on World Health Organization core drug use indicators in Ethiopia: a systematic review. Drug Healthcare Patient Safe. 2021;13:159–170. doi:10.2147/DHPS.S311926
12. Desai M, Iyer G, Dikshit RK. Antiretroviral drugs: critical issues and recent advances. Indian J Pharmacol. 2012;44(3):288–298. doi:10.4103/0253-7613.96296
13. Gupta RK, Gregson J, Parkin N, et al. HIV-1 drug resistance before initiation or re-initiation of first-line antiretroviral therapy in low-income and middle-income countries: a systematic review and meta-regression analysis. Lancet Infect Dis. 2018;18(3):346–355. doi:10.1016/S1473-3099(17)30702-8
14. Tassew SG, Abraha HN, Gidey K, Gebre AK. Assessment of drug use pattern using WHO core drug use indicators in selected general hospitals: a cross-sectional study in Tigray region, Ethiopia. BMJ open. 2021;11(10):e045805. doi:10.1136/bmjopen-2020-045805
15. Aynalem GA, Bekele TA, Alemayehu FA. Drug use evaluation of vancomycin at medical ward of yekatit 12, hospital medical college, addis ababa, Ethiopia, 2018. Int J. 2020;6(10):381.
16. Gangwar R, Kumar A, Zargar AA, Sharma A, Kumar R. The role of drug utilization evaluation in medical sciences. Global Health J. 2023;7(1):3–8. doi:10.1016/j.glohj.2023.02.002
17. Sart AA, Usan S. Perform an effective medication-use evaluation: December 2017. Phar Purch Prod Magazi. 14(12):1.
18. Jagarlamudi A, Vishali A, Mounika I. Drug Utilization Evaluation of Metronidazole at a Tertiary Care Center in Hyderabad, India. J Drug Delivery Ther. 2019;9(3):272–278.
19. World Health Organization. Drug and Therapeutics Committees: A Practical Guide. World Health Organization; 2003.
20. Joint Commission on Accreditation of Healthcare Organizations. Approved: the Joint Commission’s hospital performance measurement implementation plan through 2008. Jt Comm Perspect. 2007 Mar;27(3):1, 3–5. PMID: 17416141.
21. Holloway K, Green T. Drug and Therapeutics Committees a Practical Guide. France: World Health Organization (WHO); 2003.
22. Mousavi S, Behi M, Taghavi MR, Ahmadvand A, Ziaie S, Moradi M. Drug utilization evaluation of imipenem and intravenous ciprofloxacin in a teaching hospital. Iran J Pharm Res Winter. 2013;12(Suppl).161–7. PMID: 24250684; PMCID: PMC3813373.
23. Kouamou V, Machekano R, Mapangisana T, et al. Tenofovir, lamivudine, and dolutegravir among rural adolescents in Zimbabwe: a cautionary tale. AIDS Res Hum Retro. 2022;38(10):774–778. doi:10.1089/aid.2021.0140
24. Mir SA, Muzamil F, Bhat M, Amin A, Shakeel D. Assessment of medication adherence among patients with chronic diseases: a descriptive cross-sectional study. Int J Basic Clin Pharmacol. 2018;8(1):115. doi:10.18203/2319-2003.ijbcp20185168
25. Lemay J, Waheedi M, Al-Sharqawi S, Bayoud T. Medication adherence in chronic illness: do beliefs about medications play a role? Patient Prefer Adher. 2018;12:1687. doi:10.2147/PPA.S169236
26. Back D, Marzolini C, Gibbons S, et al. HIV Drug Interactions. Liverpool: University of Liverpool; 2018.
27. Considerations for the Introduction of TLD in national programs: PEPFAR guidance on developing clinical and programmatic recommendations. 2018.
28. Zamora, Stajduhar KI, Mollison A, Giesbrecht M, et al. Dolutegravir and lamivudine combination for the treatment of HIV-1 infection HIV/AIDS. Res Pallia Care. 2019;18(1):11. doi:10.1186/s12904-019-0396-7.
29. Walimbwa SI, Lamorde M, Waitt C, et al. Drug interactions between dolutegravir and artemether-lumefantrine or artesunate-amodiaquine. Antimi Agen Chemo. 2019;63(2). doi:10.1128/AAC.01310-18.
30. World Health Organization. Policy Brief: Update of Recommendations on First-and Second-Line Antiretroviral Regimens. World Health Organization; 2019.
31. Lu L, Li X, Liu X, et al. Comparison of renal function biomarkers of serum creatinine and cystatin c in HIV-infected people on dolutegravir-containing therapy. Infect Drug Resist. 2022;15:1695–1706. doi:10.2147/IDR.S347054
32. Mabirizi D, Phulu B, Churfo W, et al. Implementing an integrated pharmaceutical management information system for antiretrovirals and other medicines: lessons from Namibia. Global Health. 2018;6(4):723–735. doi:10.9745/GHSP-D-18-00157
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
