Back to Journals » Journal of Pain Research » Volume 17
Effect of Intermittent Thoracic Paravertebral Block on Postoperative Nausea and Vomiting Following Thoracoscopic Radical Resection of the Lung Cancer: A Prospective Randomized Trial
Authors Ma T, Yu Y, Cao H, Wang H, Wang M
Received 6 December 2023
Accepted for publication 28 February 2024
Published 7 March 2024 Volume 2024:17 Pages 931—939
DOI https://doi.org/10.2147/JPR.S453615
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rushna Ali
Ting Ma,1,* Yulong Yu,2,* Haihua Cao,3 Huiqin Wang,2 Mingcang Wang2
1Anesthesia Department, The First Affiliated Hospital of Zhejiang Chinese Medical University (Zhejiang Provincial Hospital of Chinese Medicine), Hangzhou, Zhejiang, 310000, People’s Republic of China; 2Anesthesia Department, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, Zhejiang, 317000, People’s Republic of China; 3Obstetrical Department, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, Taizhou, Zhejiang, 317000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Mingcang Wang, Anesthesia Department, Taizhou Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, No. 150, Ximen Street, Linhai, Zhejiang, 317000, People’s Republic of China, Email [email protected]
Purpose: To explore the benefits of ultrasound-guided intermittent thoracic paravertebral block (TPVB) combined with intravenous analgesia (PCIA) in alleviating postoperative nausea and vomiting (PONV) during video-assisted thoracic surgery (VATS).
Patients and Methods: 120 patients with lung carcinoma undergoing VATS were included and divided into three groups: group S (single TPVB+PCIA), group I (intermittent TPVB+PCIA), and group P (PCIA). The patients’ NRS scores, postoperative hydromorphone hydrochloride consumption, and intramuscular injection of bucinnazine hydrochloride were recorded. The incidence of PONV and complications were documented.
Results: Compared with the group P, both group I and group S had significantly lower static NRS scores from 1– 48 hours after the operation (P < 0.05), and the dynamic NRS score of group I at the 1– 48 hours after the operation were significantly decreased (P < 0.05). Compared with the group P, the proportion of patients with PONV in group I was significantly lower (P < 0.05), while there was no significant difference in group S. Moreover, the hospitalization period of patients in group I was significantly reduced compared with the other two groups (P < 0.01), and the patient satisfaction was significantly increased compared with the group P (P < 0.05).
Conclusion: Intermittent TPVB combined with PCIA can reduce the postoperative pain and the occurrence of PONV.
Keywords: thoracic paravertebral block, patient-controlled intravenous analgesia, video-assisted thoracic surgery, postoperative nausea and vomiting, postoperative pain
Introduction
Video-assisted thoracic surgery (VATS) is currently the foremost clinical treatment for lung cancer, which has gradually become the standard treatment.1 Compared with traditional thoracotomy, this treatment offers the advantages of reduced trauma, less pain, and increased preservation of postoperative pulmonary function.2 Although the small incision of VATS does mitigate to some extent, many patients undergoing VATS still report significant acute and chronic postoperative pain.3 An early study has reported chronic pain rate of 36% in VATS patients undergoing wedge resection,4 and a survey of thoracic surgery patients in the Netherlands found that 47% of VATS patients reported chronic pain.5 Postoperative pain in thoracic surgery primarily hinders patients’ mobility and reduces their quality of life. At present, the main clinical methods for pain relief include epidural analgesia,6 intercostal nerve block,7 paravertebral block,8 erector spinae block,9 and so on. As a widely used analgesic drug in clinical practice, opioids can act on the μ, κ, and δ receptors on the peripheral nervous system, spinal cord, and brain, resulting in a potent analgesic effect.10 In addition, postoperative nausea and vomiting (PONV) is common in patients undergoing VATS.11 However, opioids are also an independent risk factors for PONV, with the incidence of PONV being related to the dose and duration of opioid use.12 Therefore, clinically reducing the dose of perioperative opioids may help reduce the incidence of PONV.
Paravertebral block (PVB) is considered one of the preferred regional anesthesia technique that can effectively relieve postoperative pain in patients undergoing thoracic and upper abdominal surgery, with the advantages of easy learning, high safety, and simplicity.13 Previous studies have employed an ultrasound-guided single thoracic paravertebral block (TPVB) technique in combination with patient-controlled intravenous analgesia (PCIA) to reduce the incidence of chronic pain in patients undergoing open-heart surgery.14 This treatment was found to reduce the incidence of moderate and severe postoperative pain, as well as PONV. However, opioids remain the main drugs used to control postoperative analgesia, which can still affect the postoperative rehabilitation of patients through PONV. Apart from causing physical discomfort to patients, PONV can also increase arterial pressure, intracranial pressure, intraocular pressure, and the risk of complications such as reflux aspiration, postoperative bleeding, and suture rupture.10 Moreover, the length of the patient’s stay in the postoperative anesthesia recovery room and hospitalization time would be prolonged, and ultimately increases medical costs.15
Therefore, we hypothesized that the use of ultrasound-guided intermittent TPVB combined with PCIA technique for analgesia treatment after thoracoscopic radical lung cancer surgery is promising to address the above problems. The aim of this study is to investigate the advantages of ultrasound-guided intermittent TPVB combined with PCIA, and to find a superior anesthetic method for relieving patients’ postoperative pain, decreasing the incidence of PONV, and promoting patients’ recovery. Our results suggest that intermittent TPVB combined with PCIA can reduce the postoperative pain and the occurrence of PONV.
Methods
Study Design and Participants
This prospective randomized controlled trial was conducted in patients with lung carcinoma undergoing VATS at Hospital of Zhejiang Province Affiliated to Wenzhou Medical University, from June 2021 to December 2021. Patient inclusion criteria included: (i) preoperative chest computed tomography examination and postoperative pathological findings diagnosed as lung cancer; (ii) surgical procedure was VATS; (iii) signed patient informed consent. Exclusion criteria included: (i) allergy to local anesthetic drugs; (ii) hypovolemia, hematological disease or abnormal coagulation function; (iii) infected foci at the puncture site (ie, redness, swelling and heat); (iv) body mass index ≥ 35 kg/m2; (v) chronic opioid and analgesic use; (vi) combined severe hypertension, diabetes mellitus, and long-term use of cortisol hormones; (vii) inability to understand and use the Numerical Rating Scale (NRS, a commonly used pain rating scales)16,17 and PCIA; and (viii) patients who refused to participate in the study.
The sample size of the study was calculated according to our preliminary study, 40 patients in each group would have an 80% power to detect differences in the incidence of PONV between the three groups using two-sided analysis with an error of 0.05. Therefore, 154 cases were sequentially admitted. Among them, 26 did not meet the exclusion criteria, and 8 declined to participate. Ultimately, a total of 120 participants were enrolled according to the inclusion and exclusion criteria set by the study. The patients were divided into three groups via digital randomization: the group S (ultrasound-guided single TPVB combined with PCIA, n=40), the group I (ultrasound-guided intermittent TPVB combined with PCIA, n=40), and the group P (PCIA alone, n=40).
This study completed registration in the Chinese clinical trial registry on June 18, 2021 (registration number: ChiCTR2100047423; Date: 18/06/2021). The study was performed after obtaining approval from the Ethics Committee of Hospital of Zhejiang Province Affiliated to Wenzhou Medical University (K20210507) and written informed consent from the patients. The study adhered to the principles of the Declaration of Helsinki.
Procedure
All patients who underwent elective surgery were subject to preoperative fasting and were not given preoperative medications. Concerning fasting, all enrolled patients’ fasting conditions were determined in accordance with the pre-operative fasting guidelines for adult and children surgical anesthesia (2014). Specifically, abstinence from clear fluids was mandated two hours prior to anesthesia induction, abstention from starchy solid foods and refraining from milk and formula milk were stipulated six hours before anesthesia induction, and avoidance of fatty solid foods was required eight hours before anesthesia induction. Moreover, pre-operative assessment was conducted on the day preceding the surgery, evaluating patients’ susceptibility to PONV using the Apfel scoring system. Accordingly, the risk factors outlined by the scoring system, including female gender, non-smoking status, a history of previous PONV, and postoperative opioid usage, were assigned a score of 1, resulting in a total score range of 0 to 4. PONV risk was categorized as low (scores 0, 1), moderate (score 2), and high risk (scores 3, 4).18
Upon entering the operating room, patients were routinely monitored with electrocardiogram, heart rate, invasive blood pressure, pulse oxygen saturation, and respiration. After opening the peripheral veins, all patients undergo fluid maintenance therapy, primarily for the following reasons:1. Hypovolemia after nighttime fasting is thought to exacerbate PONV; 2. Pre-operative administration of crystalloids and colloids significantly reduces the incidence of PONV, with both crystalloids and colloids found to be equally effective in preventing PONV; 3. Fluid maintenance therapy can allow intravenous anesthetics to continuously enter the body to maintain sufficient depth of anesthesia.19,20 Specifically, all patients were given 5 mL/kg of colloid solution, followed by a 1:2 infusion of colloid solution and crystalloid solution at a rate of 8 mL/kg/h. Patients in the three groups underwent routine induction of general anesthesia with general anesthetic induction drugs including propofol (2–3 mg/kg), fentanyl injection (5 μg/kg), continuous infusion of remifentanil infusion (0.2–0.5 μg/kg/min), and rocuronium. The ventilator parameters were set with a VT of 6–8 mL/kg, RR of 10–14 times/min, and maintenance PETCO2 of 35–45 mmHg. Intraoperative anesthesia was maintained with sevoflurane, remifentanil infusion (0.1–0.5 μg/kg/min), and intermittent additional measures were taken as necessary.
In groups I and S, ultrasound (Sonosite Portable Ultrasound, USA, M-Turbo) was performed under the guidance of the affected TPVB block before the start of surgery after induction of anesthesia. The patient was placed in an upward-facing lateral position with the high-frequency linear probe placed parallel to the T4 vertebral body level and with a 2–3 cm lateral offset to obtain suitable visualization. After confirming the anatomical position of the pleura, transverse process, and paravertebral space, an in-plane needle approach technique was used, ie, the path of the puncture needle from the cephalad to the caudal side was completely visualized on the ultrasound image. In group S, 20 mL of 0.25% ropivacaine injection was injected after bloodless and airless retraction, while in group I, a catheter was placed and fixed, and 20 mL of 0.25% ropivacaine injection was injected through the catheter after pumping back bloodless and airless. A 300 mL of electronic analgesic pump was then connected for programmed intermittent injection of drugs at 6-hour intervals with 20 mL of 0.25% ropivacaine injection, and the analgesic pump was formulated with 10 ropivacaine injections diluted to 300 mL, and the subpleural pressure sign could be observed on the ultrasound image.
Each patient received a 100 mg flurbiprofen injection for analgesia and a 3 mg granisetron injection for PONV prophylaxis before suturing the skin at the end of surgery. After discontinuing all anesthetic maintenance drugs at the end of surgery, patients were sent to the recovery room for resuscitation. Patients were given an intravenous electronic analgesia pump with 12 mg hydromorphone hydrochloride (6 doses in total) diluted to 300 mL (6 mL per bolus, lock time 15 min, no background dose) for each patient after recovery room. If the patient’s NRS score on the ward was still greater than 4, remedial treatment of pain was performed using the appropriate dose of bucinnazine hydrochloride intramuscularly.
Evaluation Parameters
Incidence of PONV in patients, NRS scores in the quiet and dynamic states at 1, 6, 12, 24 and 48 h postoperative time points, the amount of postoperatively hydromorphone hydrochloride used, the number of intramuscular bucinnazine hydrochloride injections, the occurrence of complications such as respiratory depression and pruritus, and any complications such as spinal nerve injury, hematoma, and pneumothorax that occur during follow-up.
Patient Satisfaction Survey
This study conducted a satisfaction survey questionnaire for hospitalized surgical patients, encompassing evaluations of satisfaction in six aspects: medical technical quality, medical processes, medical ethics and professionalism, doctor-patient communication, medical expenses, and hospitalization environment. The Likert five-point scale was employed for representation in the following order: very dissatisfied, dissatisfied, general, satisfied, and very satisfied. Of these, satisfactory and very satisfactory were defined as patients being satisfied.
Statistical Analysis
Means ± standard deviations were used for measurement data, independent t-test for normal distribution, and ANOVA for non-normal distribution. Medians ± quartiles and rates were used for count data, and Kruskal–Wallis test and chi-square test were used. The statistical software was SPSS 22.0, and a significant difference will be defined as a P value <0.05.
Results
Patients’ Characteristics and Operative Data
A total of 120 patients who underwent VATS were enrolled in this study. Figure 1 shows the consort flow chart of the study. None of the patients experienced spinal nerve injury, hematoma, pneumothorax, or other VATS-related complications upon awakening. There were no significant differences in demographic data, American Society of Anesthesiologists (ASA) scores, anesthesia time, and operative time between the three groups of patients. The baseline characteristics of the patients and surgical data are shown in Table 1. Table 2 shows the Apfel scores of the patients from the three groups.
 |
Table 1 Baseline Characteristics and Operative Data of Patients in Three Different Treatment Groups |
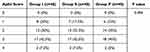 |
Table 2 Apfel Score of Patients in Three Groups |
 |
Figure 1 Flow diagram of the patient inclusion in this study. |
Outcomes
Compared with the group P, the proportion of patients with postoperative nausea (P=0.001) and vomiting (P=0.013) was significantly lower in group I, while there was no significant difference in group S (Table 3). Compared with group P, the length of hospitalization time was significantly reduced in group I (P=0.000), and the patient satisfaction was significantly increased in group I (P=0.013). In contrast, there was no significant difference in the satisfaction of patients between group S and group P. The occurrence of pruritus symptoms did not differ significantly among the three groups, and no other postoperative complications were observed (Table 3).
 |
Table 3 Comparison of Postoperative Clinical outcomes Between Groups |
Static and dynamic NRS scores were recorded for all patients at 1 h, 6 h, 12 h, 24 h, and 48 h after awakening. Compared with group P, static NRS scores were significantly lower in groups I and S at 1 to 48 h after surgery, with more significant decreases at 12 h, 24 h, and 48 h (group I vs group P, 1h after surgery: P=0.011; 6h after surgery: P=0.012; 12–48h after surgery: P=0.000) (group S vs group P, 1h after surgery: P=0.011; 6h after surgery: P=0.012; 12h after surgery: P=0.001; 24–48h after surgery: P=0.000). Compared with group P, dynamic NRS scores at 1 to 48 h after surgery were significantly lower in group I (1h after surgery: P=0.002; 6–48h after surgery: P=0.000), while dynamic NRS scores in group S were significantly lower only at 1 h, 6 h, and 12 h compared with group P (1h after surgery: P=0.002; 6–12h after surgery: P=0.000). Meanwhile, the dynamic NRS scores at 12 to 48 h after surgery were significantly lower in group I compared with group S (P=0.000) (Table 4).
 |
Table 4 Postoperative NRS Scores in Three Groups |
Moreover, the number of pain pump presses and the amount of hydromorphone hydrochloride consumed in the postoperative period were significantly lower in groups I and S than in group P (P=0.000), and the number of presses and the amount of hydromorphone hydrochloride consumed in group I were significantly lower than in group S (P=0.000). The number of patients who received intramuscular bucinnazine hydrochloride in the postoperative period was 0 in group I, which was significantly lower than in groups S and P (P=0.000), and the number of patients who used bucinnazine hydrochloride between groups S and P did not differ significantly (P=0.061) (Table 5).
 |
Table 5 Comparison of Postoperative Analgesic Use in Three Groups |
Discussion
PONV is a prevalent and distressing clinical complication, with reported incidence rates as high as 80% in high-risk patients.21,22 Various studies have indicated that the incidence of PONV is associated with the use of inhalational anesthesia and opioid analgesics, as well as procedures such as cholecystectomy, laparoscopic surgery, and gynecologic surgery, which increase the risk of PONV.23,24 It has been reported that about two-thirds of patients experience moderate to severe early postoperative pain after surgery.25 Opioids are the most widely used and effective analgesics for the treatment of severe pain, including chronic, acute, and postoperative pain.26 Previous clinical studies have typically reduced the incidence of PONV by minimizing the dose of perioperative opioids. Prevention of PONV and reduction of its incidence can alleviate the associated pain and promote the rapid recovery of patients.27,28
TPVB is an efficient method for reducing postoperative pain, with high success rate and easy operation.29 Compared with general anesthesia, TPVB used for surgical anesthesia in thoracic and lumbar spine can reduce immediate postoperative pain, as well as the incidence of PONV, while enhancing patient satisfaction.13 Chen et al have reported that the combination of TPVB and PCIA can effectively reduce opioid use and result in lower NRS scores in comparison to PCIA alone.30 Similarly, a study by Vogt et al has demonstrated that a single TPVB combined with PCIA significantly reduced acute postoperative pain in patients undergoing thoracoscopic surgery compared to PCIA, reducing the 6-month postoperative pain incidence.31 Our study also showed that static, dynamic NRS scores were significantly lower in group I as well as part of group S compared to group P. A survey of analgesia techniques for thoracic surgery in the United Kingdom revealed that a single TPVB combined with PCIA can be used as an alternative to continuous thoracic epidural analgesia during thoracotomy and is gaining popularity.32 A study by Kailaroma et al showed that the benefits of TPVB became more evident with longer follow-up, that patients who received TPVB had less exercise-related pain and less pain at rest, and that the role of TPVB in preventing chronic pain continues to evolve.33
Previous studies have identified and compared the benefits of different types of TPVB. For instance, Chen et al showed that programmed intermittent pushing reduced local anesthetic consumption compared to continuous infusion techniques after VATS.34 However, Unkart et al pointed out that adding continuous perioperative TPVB to single TPVB did not significantly reduce pain scores.35 Nevertheless, the comparison between intermittent TPVB and single TPVB has not yet been reported, and few studies have elucidated the effect of intermittent TPVB on the incidence of postoperative PONV in patients. Intermittent TPVB is delivered regularly by an automatic infusion pump and in recent years is considered to be mostly used for peripheral nerve blocks.36 Theoretically, intermittent infusion can maintain more anesthetized dermatomes for TPVB.37 In this study, we compared the postoperative pain level, the incidence of PONV and patient satisfaction in patients with single-shot TPVB combined with PCIA and intermittent TPVB combined with PCIA. The results of the study showed that both the intermittent TPVB and single-shot TPVB combined with PCIA can reduced the postoperative pain level of patients, and the effect of intermittent TPVB combined with PCIA was more significant. It proved that intermittent TPVB combined with PCIA has good postoperative analgesic effect, which can relieve the postoperative pain of patients undergoing VATS or even eliminate the need for drug analgesia, shorten the hospitalization time of patients and improve the postoperative satisfaction of patients.
Exogenous opioids produce analgesia mainly by acting on Mu-Opioid Receptor in glutamatergic excitatory neurons.38 However, the use of opioids in pain control is also controversial. Apfel et al showed that intraoperative opioid use did not significantly exacerbate PONV, while postoperative opioid use was one of the risk factors for the development of PONV.24,39 Opioids, while acting as analgesics, can have a large number of negative effects on patients, such as nausea, vomiting, dizziness, excessive sedation, addiction, and other side effects.38 Therefore, reducing the use of postoperative opioids may be able to reduce the incidence of postoperative PONV. Ziemann-Gimmel’s study noted an association between opioid-free and a reduced relative risk of PONV.40 The results of this study likewise showed that hydromorphone hydrochloride consumption was significantly less in group I than in groups S and P after surgery. Compared with group P, group I was able to significantly reduce the incidence of postoperative vomiting and nausea complications and had higher patient satisfaction. Meanwhile, there was no significant difference in postoperative vomiting and nausea in group S compared with group P. It was demonstrated that the reduction of hydromorphone hydrochloride use could improve the incidence of nausea and vomiting and postoperative quality of life of patients. The consensus guidelines for the management of PONV15 pointed out that reducing intraoperative and postoperative opioid use is one of the strategies to reduce the incidence of PONV, and intermittent TPVB combined with PCIA can effectively reduce postoperative hydromorphone hydrochloride use, thus achieving the goal of reducing the PONV incidence in patients.
In conclusion, this study found that compared with PCIA alone and single-shot TPVB combined with PCIA, intermittent TPVB combined with PCIA has a better postoperative analgesic effect and can reduce the dose of postoperative opioids, mitigate the incidence of PONV, and shorten the hospitalization time of patients. This technique provides new insights for reducing patient pain after thoracoscopic surgery, promoting rapid patient recovery, and reducing treatment costs.
However, the limitation of our study is that it is a single-institution study with a small sample size. In addition to expanding the sample size in future studies, we also need to explore the costs and benefits, and pay attention to the potential discomfort that intramuscular injection may cause to patients.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article. The authors state that all data in the manuscript are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Committee of Hospital of Zhejiang Province affiliated to Wenzhou Medical University (K20210507). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects and/or their legal guardian(s).
Acknowledgments
Ting Ma and Yulong Yu are co-first authors for this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting or writing, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Medical Science and Technology Project of Zhejiang Province (2022KY1383).
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Flores RM, Park BJ, Dycoco J, et al. Lobectomy by video-assisted thoracic surgery (VATS) versus thoracotomy for lung cancer. J Thorac Cardiovasc Surg. 2009;138(1):11–18. doi:10.1016/j.jtcvs.2009.03.030
2. Nagahiro I, Andou A, Aoe M, Sano Y, Date H, Shimizu N. Pulmonary function, postoperative pain, and serum cytokine level after lobectomy: a comparison of VATS and conventional procedure. Ann Thorac Surg. 2001;72(2):362–365. doi:10.1016/S0003-4975(01)02804-1
3. Neustein SM, McCormick PJ. Postoperative analgesia after minimally invasive thoracoscopy: what should we do? Can J Anaesth. 2011;58(5):
4. Furrer M, Rechsteiner R, Eigenmann V, Signer C, Althaus U, Ris HB. Thoracotomy and thoracoscopy: postoperative pulmonary function, pain and chest wall complaints. Eur J Cardiothorac Surg. 1997;12(1):82–87. doi:10.1016/S1010-7940(97)00105-X
5. Steegers MA, Snik DM, Verhagen AF, van der Drift MA, Wilder-Smith OH. Only half of the chronic pain after thoracic surgery shows a neuropathic component. J Pain. 2008;9(10):955–961. doi:10.1016/j.jpain.2008.05.009
6. Malevic A, Jatuzis D, Paliulyte V, Kontrimavičiūtė E, Ramašauskaitė D, Rutkauskaitė-Valančienė D. Epidural analgesia and back pain after labor. Medicina. 2019;55(2):55. doi:10.3390/medicina55020055
7. Chen T, Zhu Z, Du J. Efficacy of intercostal nerve block for pain control after percutaneous nephrolithotomy: a systematic review and meta-analysis. Front Surg. 2021;8:623605. doi:10.3389/fsurg.2021.623605
8. D’Ercole F, Arora H, Kumar PA. Paravertebral block for thoracic surgery. J Cardiothorac Vasc Anesth. 2018;32(2):915–927. doi:10.1053/j.jvca.2017.10.003
9. Luo R, Tong X, Yan W, Liu H, Yang L, Zuo Y. Effects of erector spinae plane block on postoperative pain in children undergoing surgery: a systematic review and meta-analysis of randomized controlled trials. Paediatr Anaesth. 2021;31(10):1046–1055. doi:10.1111/pan.14255
10. de Boer HD, Detriche O, Forget P. Opioid-related side effects: postoperative ileus, urinary retention, nausea and vomiting, and shivering. A review of the literature. Best Pract Res Clin Anaesthesiol. 2017;31(4):499–504. doi:10.1016/j.bpa.2017.07.002
11. Sun K, Liu D, Chen J, et al. Moderate-severe postoperative pain in patients undergoing video-assisted thoracoscopic surgery: a retrospective study. Sci Rep. 2020;10(1):795. doi:10.1038/s41598-020-57620-8
12. Roberts GW, Bekker TB, Carlsen HH, Moffatt CH, Slattery PJ, McClure AF. Postoperative nausea and vomiting are strongly influenced by postoperative opioid use in a dose-related manner. Anesth Analg. 2005;101(5):1343–1348. doi:10.1213/01.ANE.0000180204.64588.EC
13. Thavaneswaran P, Rudkin GE, Cooter RD, Moyes DG, Perera CL, Maddern GJ. Brief reports: paravertebral block for anesthesia: a systematic review. Anesth Analg. 2010;110(6):1740–1744. doi:10.1213/ANE.0b013e3181da82c8
14. Li XL, Zhang J, Wan L, Wang J. Efficacy of single-shot thoracic paravertebral block combined with intravenous analgesia versus continuous thoracic epidural analgesia for chronic pain after thoracotomy. Pain Physician. 2021;24:E753–E759.
15. Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118(1):85–113. doi:10.1213/ANE.0000000000000002
16. Karcioglu O, Topacoglu H, Dikme O, Dikme O. A systematic review of the pain scales in adults: which to use? Am J Emerg Med. 2018;36(4):707–714. doi:10.1016/j.ajem.2018.01.008
17. Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073–1093. doi:10.1016/j.jpainsymman.2010.08.016
18. Avinash SH, Krishna HM. The impact of the Apfel scoring system for prophylaxis of post-operative nausea and vomiting: a randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2023;39(3):463–467. doi:10.4103/joacp.joacp_553_21
19. Apfel CC, Meyer A, Orhan-Sungur M, et al. Supplemental intravenous crystalloids for the prevention of postoperative nausea and vomiting: quantitative review. Br J Anaesth. 2012;108(6):893–902. doi:10.1093/bja/aes138
20. Chaudhary S, Sethi AK, Motiani P, et al. Pre-operative intravenous fluid therapy with crystalloids or colloids on post-operative nausea & vomiting. Indian J Med Res. 2008;127(6):577–581.
21. Apfel CC, Laara E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91(3):693–700. doi:10.1097/00000542-199909000-00022
22. Sinclair DR, Chung F, Mezei G. Can postoperative nausea and vomiting be predicted? Anesthesiology. 1999;91(1):109–118. doi:10.1097/00000542-199907000-00018
23. Horn CC, Wallisch WJ, Homanics GE, Williams JP. Pathophysiological and neurochemical mechanisms of postoperative nausea and vomiting. Eur J Pharmacol. 2014;722:55–66. doi:10.1016/j.ejphar.2013.10.037
24. Apfel CC, Heidrich FM, Jukar-Rao S, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth. 2012;109(5):742–753. doi:10.1093/bja/aes276
25. Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–157. doi:10.1016/j.jpain.2015.12.008
26. Corder G, Castro DC, Bruchas MR, Scherrer G. Endogenous and Exogenous Opioids in Pain. Annu Rev Neurosci. 2018;41(1):453–473. doi:10.1146/annurev-neuro-080317-061522
27. Hill RP, Lubarsky DA, Phillips-Bute B, et al. Cost-effectiveness of prophylactic antiemetic therapy with ondansetron, droperidol, or placebo. Anesthesiology. 2000;92(4):958–967. doi:10.1097/00000542-200004000-00012
28. Tramer MR. Strategies for postoperative nausea and vomiting. Best Pract Res Clin Anaesthesiol. 2004;18(4):693–701. doi:10.1016/j.bpa.2004.05.003
29. Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105(6):842–852. doi:10.1093/bja/aeq265
30. Chen H, Liao Z, Fang Y, et al. Continuous right thoracic paravertebral block following bolus initiation reduced postoperative pain after right-lobe hepatectomy: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2014;39(6):506–512. doi:10.1097/AAP.0000000000000167
31. Vogt A, Stieger DS, Theurillat C, Curatolo M. Single-injection thoracic paravertebral block for postoperative pain treatment after thoracoscopic surgery. Br J Anaesth. 2005;95(6):816–821. doi:10.1093/bja/aei250
32. Kotemane NC, Gopinath N, Vaja R. Analgesic techniques following thoracic surgery: a survey of United Kingdom practice. Eur J Anaesthesiol. 2010;27(10):897–899. doi:10.1097/EJA.0b013e32833d1259
33. Kairaluoma PM, Bachmann MS, Rosenberg PH, Pere PJ. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg. 2006;103(3):703–708. doi:10.1213/01.ane.0000230603.92574.4e
34. Chen L, Wu Y, Cai Y, et al. Comparison of programmed intermittent bolus infusion and continuous infusion for postoperative patient-controlled analgesia with thoracic paravertebral block catheter: a randomized, double-blind, controlled trial. Reg Anesth Pain Med. 2019;44(2):240–245. doi:10.1136/rapm-2018-000031
35. Unkart JT, Padwal JA, Ilfeld BM, Wallace AM. Treatment of post-latissimus dorsi flap breast reconstruction pain with continuous paravertebral nerve blocks: a retrospective review. Anesth Pain Med. 2016;6(5):e39476. doi:10.5812/aapm.39476
36. Taketa Y, Irisawa Y, Fujitani T. Programmed intermittent bolus infusion versus continuous infusion of 0.2% levobupivacaine after ultrasound-guided thoracic paravertebral block for video-assisted thoracoscopic surgery: a randomised controlled trial. Eur J Anaesthesiol. 2019;36(4):272–278. doi:10.1097/EJA.0000000000000945
37. Kaynar AM, Shankar KB. Epidural infusion: continuous or bolus? Anesth Analg. 1999;89(2):534. doi:10.1097/00000539-199908000-00063
38. Stephan BC, Parsa FD. Avoiding opioids and their harmful side effects in the postoperative patient: exogenous opioids, endogenous endorphins, wellness, mood, and their relation to postoperative pain. Hawaii J Med Public Health. 2016;75:63–67.
39. Apfel CC, Kranke P, Katz MH, et al. Volatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: a randomized controlled trial of factorial design. Br J Anaesth. 2002;88(5):659–668. doi:10.1093/bja/88.5.659
40. Ziemann-Gimmel P, Goldfarb AA, Koppman J, Marema RT. Opioid-free total intravenous anaesthesia reduces postoperative nausea and vomiting in bariatric surgery beyond triple prophylaxis. Br J Anaesth. 2014;112(5):906–911. doi:10.1093/bja/aet551
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
