Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
Effect of the Dynamic Orthotic Garment on Postural Control, and Endurance in Children with Spastic Diplegic Cerebral Palsy: A Randomized Controlled Trial
Authors Emara HA, Al-Johany AH, Khaled OA, Al-Shenqiti AM , Ali ARH , Aljohani MM , Sobh E
Received 3 September 2023
Accepted for publication 14 November 2023
Published 30 January 2024 Volume 2024:17 Pages 419—428
DOI https://doi.org/10.2147/JMDH.S438474
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hatem A Emara,1,2,* Ahmed H Al-Johany,3 Osama A Khaled,1,4 Abdullah M Al-Shenqiti,1 Abdul Rahman H Ali,5 Marwan M Aljohani,1 Eman Sobh6,7,*
1Physical Therapy Department, College of Medical Rehabilitation Sciences, Taibah University, Medina, Saudi Arabia; 2Department of Physical Therapy for Growth and Developmental Disorders in Children and its Surgery, Faculty of Physical Therapy, Cairo University, Cairo, Egypt; 3Medical Rehabilitation Hospital, Ministry of Health, Medina, Saudi Arabia; 4Basic Science Department, Faculty of Physical Therapy, Cairo University, Cairo, Egypt; 5College of Medical Rehabilitation Sciences, Taibah University, Medina, Saudi Arabia; 6Respiratory Therapy Department, College of Medical Rehabilitation Sciences, Taibah University, Medina, Saudi Arabia; 7Chest Diseases Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
*These authors contributed equally to this work
Correspondence: Hatem A Emara, Physical Therapy Department, College of Medical Rehabilitation Sciences, Taibah University, P.O 344, Medina, 41411, Saudi Arabia, Tel +966564156262, Fax +966148618888, Email [email protected]
Purpose: To investigate the effect of dynamic orthotic garments (Thera togs) on foot pressure distribution, postural control, and endurance in children with spastic diplegic CP.
Patients and Methods: This is a single-blind randomized controlled clinical trial involving 34 (8– 10 years) with spastic diplegic CP. The control group received conventional physical therapy (CPT), whereas the study group received CPT in addition to wearing TheraTogs. We recorded foot pressure distribution, trunk control measurement scale, trunk position sense, Pediatric Berg Balance Scale (PBS), and six-minute walking distance (6MWD).
Results: Both groups showed improvement. The study group had significant improvement in foot pressure distribution (p-value 0.003, 0.001, < 0.001 for forefoot, midfoot, and rearfoot mean pressures respectively, and 0.005, < 0.001, and 0.005 for forefoot, midfoot, and rearfoot peak pressures respectively), Pediatric balance scale, The trunk control measurement scale, and Trunk position sense (p-value < 0.001) and six-minute walking distance (p-value 0.029). Our data suggest that adding TheraTogs to conventional physiotherapy improves foot pressure, postural control, and endurance in children with spastic diplegic cerebral palsy.
Conclusion: Both TheraTogs and conventional physical therapy corrected foot pressure distribution, trunk control, improved balance, and increased 6MWD in children with spastic diplegic CP but the improvement was more significant in TheraTogs group.
Clinical Trial Registration: NCT05271149.
Keywords: children with disability, theratogs, foot pressure, balance score, orthotic devices
A Letter to the Editor has been published for this article.
Introduction
Cerebral palsy is a common cause of disability in the pediatric population worldwide.1 It is the most common cause of motor disability in the United States.2 Cerebral palsy involves permanent non-progressive disorders of motor function and of movement and/or posture which may result from non-progressive disturbances in brain development occurring during fetal and/or infant life.3 It consists of a group of motor disorders leading to activity limitation and is usually associated with musculoskeletal and neurologic disorders4,5 including impaired muscle tone, movement, and reflexes, impairment of perception, sensation, behavior, cognition, communication, seizures, dyskinesia with or without sensory and mental deficits such as spasticity, contracture, and incoordination of movement.6
Cerebral palsy is classified according to the number, type, and severity of neurologic disability.3 Spastic diplegia is the most common form of CP where lower limbs are more affected than upper limbs.2 The motor deficits and spasticity of lower extremities in the spastic diplegia form of CP lead to a special walking pattern characterized by equinus ankle position, exaggerated knee flexion with genu valgus, and increased hip adduction and internal rotation.4,5 In addition, abnormal muscle tone may lead to femoral torsion and compensatory tibial torsion which results in toe-in gait and crouch gait and thus decreases the stability during walking. Deformities of the long bones and foot deformities diminish the effectiveness of muscle action and produce a slow gait pattern with high-energy expenditure. In addition to sensory deficits including proprioception which may affect posture control.7,8 Children with spastic diplegic CP had balance problems compared to their healthy peers due to impaired neural motor control and musculoskeletal abnormality.9 Children with CP lead a sedentary lifestyle with limited physical activity which contributes to impaired cardiorespiratory function.10 So, children with CP have a lifelong disability and need continuous care and assistance1 causing severe economic losses and serious inconveniences.11 The function and quality of life can be improved with proper treatment.12
Rehabilitation programs involving the use of flexible dynamic orthotic garments, such as TheraTogs, have been proposed to improve the ability to stabilize the posture, correct or prevent deformities, improve functionality, and enable the user to a more appropriate functional pattern. Conventional physical therapy was the available treatment. In recent decades, new treatment options are available as genetic therapy, robotics, and new technological devices for rehabilitation.13,14 One of the new devices used for rehabilitation is TheraTogs. It is a dynamic orthotic garment, composed of a “breathable”, light, Velcro-adhesive fabric. it provides a smooth passive strength, to correct imbalances or alignments through a combined system of the trunk and lower limbs, along with a system of custom outer straps.15 Few studies discussed the effects of TheraTogs on spatiotemporal gait, posture, foot pressure distribution, balance, and functional performance in children with CP.16,17 The effects of TheraTogs on plantar pressure distribution, postural control, functional performance, and cardiorespiratory endurance in children with spastic diplegic CP are still unclear. To our knowledge, no studies examined the effect of TheraTogs on trunk position sense or six-minute walking distance. There is lack of evidence to justify the use of TheraTogs in clinical practice in children with spastic diplegic CP.16 Therefore, this study aimed to investigate the effect of TheraTogs on the modulation of foot pressure distribution, trunk control, trunk position sense, balance, and endurance in children with spastic diplegic CP to contribute to the clinical decision for using TheraTogs in rehabilitation programs. We hypothesized that the TheraTogs would have positive effects on foot pressure distribution, trunk control, balance, and thus functional performance in children with spastic diplegic CP.
Materials and Methods
Study Design
This is a single-blinded randomized controlled study. Children were randomized using the sealed envelopes method into two groups (Figure 1). All testing procedures were carried out by a blinded assessor independent of patients’ care. Before baseline measurements, all children were interviewed and familiarized with the assessment procedures and the protocol of the study.
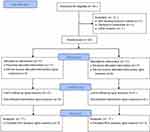 |
Figure 1 Study flow diagram. |
Ethical Issues
The study was conducted according to the Declaration of Helsinki of 1964 and its later amendments, and approved by the Research Ethics Committee of the College of Medical Rehabilitation Sciences, Medina, Saudi Arabia (CMR-PT-2022-09). Informed consent was obtained from the parents or guardians of all children involved in the study. The clinical trial was registered in ClinicalTrials.gov, under the number NCT05271149.
Study Settings
The research was conducted between March 2022 and June 2022. Participants were recruited from the outpatient clinics of Medical Rehabilitation Hospital, Global Rehabilitation Center King Fahd hospital, Al Madinah Al munawarah, Medina, Saudi Arabia.
Study Participants
A total sample size of 34 was determined to be enough to provide 80% power, after carrying out a pilot study on five participants using each of the two treatment methods (a total of 10 participants) and calculating the standard deviation of the foot pressure distribution, as the main outcome measure. We included children with spastic diplegic CP who have toe-in gait and had grade 1, 1+ degrees of spasticity according to the Modified Ashworth Scale (MAS),18 scores I and II on Gross Motor Function Classification System (GMFCS) scores,19 and the child can stand and walk independently. We excluded children who have impaired hearing or vision, or mental disability, those who had lower limb or spine surgery or Botulinum injections of the lower limb muscles within the preceding six months, those who have uncontrolled seizures during the past six months, and those with fixed deformities, dislocations or fractures of the spine or the lower extremities from the study.
Intervention
The control group included (17) children who received the conventional physical therapy program based on neurodevelopmental techniques, proprioceptive training, facilitation of muscle contraction for the anti-spastic muscles, gentle stretching exercises for the tight muscles, gait training, addition to balance, and postural control exercises. This program was given for 1 hour, 3 days a week for 12 weeks. The study group involved (17) children who received the same program of conventional physical therapy given to the control group in addition to wearing individualized full-body TheraTogs orthosis (TheraTogs™ Inc., Telluride, USA). The child wore the orthosis 8 to 10 hours a day during daily life activities for 12 weeks. The child’s guardians were trained and received a DVD recording, with a step-by-step demonstration on the fitting of TheraTogs®. Markings were made in TheraTogs® to facilitate and improve fitting. All necessary support was offered, with weekly monitoring to control the fitting of the orthosis, as well as for possible questions or clarifications. A checklist for orthosis daily use was used to evaluate the actual time the child wore the orthosis and the parents were asked to apply the instructions for orthosis fitting they learned during each visit to ensure they followed the instructions at home (Figure 1).
Data Collection Instruments and Measurements
We recorded demographic data, weight, and height. Each child was evaluated for primary outcomes (static and dynamic foot pressure distribution of both feet and postural control outcomes) and secondary outcomes (six-minute walking distance) before and after 12 weeks of the treatment. A single-blinded assessor performed all measures.
Foot Pressure Distribution
Foot pressure distribution is used to observe the abnormal alignment of the lower limbs and body weight transmission across the lower extremities and foot.20 Dynamic plantar pressure measurements were performed using a pressure platform (FDM-S, Zebris Medical GmbH, Germany). The sampling frequency was set at 100 Hz for dynamic measurements. The platform was used to measure peak and mean plantar pressure for each sub-region of the foot (forefoot, mid-foot, and rear-foot) expressed in kPa. Data presented are for the dominant foot identified by asking the child to kick a football while standing.
Trunk Position Sense
Active position sense of the trunk was assessed using a digital goniometer. Each participant was passively moved to the target position of 30° trunk flexion; they were instructed to hold and memorize this position for 10 seconds with eyes open to understand the test procedure. Once the practice trials were completed, the participant was brought to the neutral position and was instructed to replicate the target position as accurately as he or she could with closed eyes. Participant-perceived target position was measured using a digital goniometer with the reference point at the L1 lumbar spinous process.21
The Trunk Control Measurement Scale
We used the trunk control measurement scale (TCMS) to measure the trunk control. TCMS is proved to be a clinically comprehensive scale developed to assess the static and dynamic components of trunk control among children with spastic CP.22 The TCMS comprises 15 test items measuring both static and dynamic components of the trunk control in sitting. The maximum value for the total TCMS is 58 points (20 for the category “static sitting balance”, 28 for “selective movement control”, and 10 for “dynamic reaching”).23
Pediatric Balance Scale (PBS)
The PBS was used to determine the dynamic balancing abilities of children with CP. It is 14 items each item scored from zero to four and the maximum score is 56. higher scores are the best.24
Six-Minute Walk Test (6-MWT)
The test was performed between 2 lines set at a 30-meter corridor and the track was marked to measure the distance according to standard recommendations of the American Thoracic Society (ATS)25 and under the supervision of one of the researchers and the physiotherapist. Participants were instructed to wear comfortable clothing, shoes, and their splints (as appropriate), and they were allowed to use their walking aid/s as appropriate and rest if they felt tired. Participants were instructed to walk at their own pace as far as possible in six minutes. During the test, the observer verbally encouraged the children and gave them instructions about the remaining time. The distance was calculated to the nearest meter.
Data Analysis
All statistical analyses were carried out using the statistical package for the social studies (SPSS, version 20; IBM, Chicago, IL, USA). Shapiro Wilk test was used to test the normality of outcome measurements. Normal distribution was observed on pre-test scores and demographic data. The t-test and Chi-square test were used for the comparison of participants’ characteristics between both groups. Plantar pressure distribution and the six-minute walking test were normally distributed so Mixed MANOVA was carried out to find out the effect of time, the effect of treatment, and the interaction between time and treatment for the Pediatric Berg Balance Scale, Trunk control measurement scale, and Trunk position sense we used the Mann–Whitney U-test to determine in-between-group differences and Wilcoxon Signed Rank test to determine within-group differences between pre-and post-training tests. The level of significance for all statistical tests will be set at a p-value less than 0.05.
Results
No significant difference was detected between both groups concerning age, sex, height, weight spasticity grades, or GMFCS (Table 1). All children attended the scheduled visits, and the study group used the orthosis as instructed.
 |
Table 1 General Characteristics of Each Group |
Baseline Data
There was no statistically significant difference between the control group and the study group regarding mean foot plantar pressure (forefoot, midfoot, rear foot), Trunk position sense, and Trunk control measurement 6MWD at baseline (Table 2), and pediatric balance scale (Table 3).
 |
Table 2 Plantar Pressure Distribution Before and After Treatment in the Study and Control Groups |
 |
Table 3 Trunk Position Sense, Trunk Control Measurement Scale and the Pediatric Balance Scale at Baseline and Post-Treatment Within and Between Both Groups |
Effect of Treatment
Mean Pressure of the Forefoot
The mean pressure of the forefoot significantly differed across both time points in both groups (Wilks’ Lambda = 0.01; F (1, 32)= 37.56, p ˂0.001). Both groups had significantly higher forefoot mean pressure following the treatment Wilks’ Lambda = 0.31; F (1.32)=8.43, p = 0.04). The study group showed significant improvement in forefoot mean pressure following treatment (Table 2); besides, there was a significant interaction between the treatment and the time (12 weeks) (Wilks’ Lambda = 0.32; F (1.32)= 10.763, p = <0.001).
Mean Pressure of the Midfoot
The mean pressure of the midfoot significantly differed across both time points in both groups (Wilks’ Lambda = 0.04; F (1.32)= 22.458, p ˂ 0.001). Both groups had significantly lower midfoot mean pressure following the treatment (Wilks’ Lambda = 0.35; F (1.32)= 7.10, p = 0.03). The study group showed significant improvement following treatment (p = 0.001; Table 2). There was a significant interaction between the treatment and the time (12 weeks) (Wilks’ Lambda = 0.29; F (1.32)= 11.19, p = 0.001).
Mean Pressure of the Rearfoot
The mean pressure of the rearfoot significantly differed across both time points in both groups (Wilks’ Lambda = 0.03; F (1.32)= 19.89, p ˂ 0.001). Both groups had significantly higher mean pressure of rearfoot following the treatment (Wilks’ Lambda = 0.82; F (1.32)= 16.62, p ˂ 0.001). The study group showed significant improvement following treatment (Table 2). There was a significant interaction between the treatment and the time (12 weeks) (Wilks’ Lambda = 0.34; F (1.32)= 5.94, p = 0.018).
Peak Pressure of the Forefoot
The peak pressure of the forefoot significantly differed across both time points in both groups (Wilks’ Lambda = 0.19; F (1.32)= 21.70, p ˂ 0.001). Both groups had significantly higher peak pressure of the forefoot following the treatment (Wilks’ Lambda = 0.078; F (1.32) = 9.27, p = 0.003). The study group showed significant improvement following treatment (Table 2). There was a significant interaction between the treatment and the time (12 weeks) (Wilks’ Lambda = 0.36; F (1.32)= 6.18, p = 0.04).
Peak Pressure of the Midfoot
The peak pressure of the midfoot significantly differed across both time points in both groups (Wilks’ Lambda = 0.23; F (1.32)= 21.703, p ˂ 0.001). Both groups had significantly lower midfoot peak pressure following the treatment (Wilks’ Lambda = 0.18; F (1.32)= 9.27, p = 0.003). The study group showed significant improvement following treatment (Table 2). There was a significant interaction between the treatment and the time (12 weeks) (Wilks’ Lambda = 1.32; F (1.32)= 6.35, p = 0.014).
Peak Pressure of the Rearfoot
The peak pressure of the rearfoot significantly differed across both time points in both groups (Wilks’ Lambda = 0.17; F (1.32)= 13.07, p = 0.001). Both groups had significantly higher peak pressure of the rearfoot following the treatment (Wilks’ Lambda = 0.14; F (1.32)= 4.50, p = 0.03). The study group showed significant improvement following treatment (Table 2). There was a significant interaction between treatment and time (Wilks’ Lambda = 0.39; F (1.32)= 5.03, p = 0.028).
Six-Minute Walking Test
The six-minute walking distance (6MWD) significantly differed across both time points in both groups (Wilks’ Lambda = 0.06; F (1.32)= 33.73, p ˂ 0.001). Both groups had significantly higher 6MWD following the treatment (Wilks’ Lambda = 0.24; F (1.32)= 2.25, p = 0.033). The study group showed significant improvement following treatment (Table 2). There was a significant interaction between treatment and time (Wilks’ Lambda = 0.19; F (1.32)= 5.03, p = 0.028) (Table 2).
Trunk Control Measurement Scale
The Wilcoxon test revealed that both groups had significantly higher TCMS scores following treatment (p˂0.001). A Mann Whitney U-test revealed that TCMS scores were significantly higher in the study group (median difference = 6, N = 17) compared to the control group (median difference = 2, N = 17, U = 51.00, z = 3.256, p = 0.001; large effect size r = 0.56) (Table 3).
Trunk Position Sense
The Wilcoxon test revealed that both groups had significantly lower trunk position sense scores following treatment (p ˂ 0.001). A Mann–Whitney U-test revealed that trunk position sense scores were significantly lower in the study group (median difference = 4, N = 17) compared to the control group (median difference = 1, N = 17), U = 28.5, z = 4.11, p = 0.033; large effect size = 0.704) (Table 3).
Pediatric Balance Scale
The Wilcoxon test revealed that both groups had significantly higher PBS scores following treatment (p ˂ 0.001). A Mann–Whitney U-test revealed that PBS scores were significantly higher in the study group (median difference = 6, N = 17) compared to the control group (median difference = 2, N = 17), U = 0.001, z = 4.81, p = <0.001; large effect size r = 0.8) (Table 3).
Discussion
Children with diplegic cerebral palsy have abnormal muscle tension resulting in medial femoral torsion which affects toe-in-gait and crouch gait and instability during gait. This misdirection of lower limbs decreases both muscle function and gait efficiency. Those children are at increased risk of falling during ambulation.8,11,26 Ambulation is an essential functional activity and about 54% of children with CP were unable to walk as reported by Kadhim and Miller.27 Therefore, correction of lower extremities position and body balance is an important goal of physiotherapy.
The main results of this RCT are improvement in plantar pressure loading, balance, and endurance in the study and control groups.
The results of this study showed that the foot pressure distribution of both the study and control groups significantly improved following 12 weeks of treatment (Table 2). Similar results were reported in children with CP diplegia who had significant abnormal foot pressure distribution and significantly reduced rearfoot contact compared to control.28 Abd El-Kafy et al found that physical therapy in different ways (strapping, orthosis) significantly improves gait and the effect was significant with Theratogs.29 Similar studies reported that dynamic elastomeric fabric orthosis reduced the crouch position in children with CP with no effect on postural control while standing statically for a short time.30 The ground reaction force (GRF) of the crouch position in children with CP is behind the knee axis, which promotes external knee flexion moment. The plantar flexor and knee extensor muscles in children with CP are not strong enough to overcome these GRFs around the axis of the knee.31
The improvement in foot pressure in the TheraTogs group in this study may be due to improved postural alignment. Wearing TheraTogs orthotic undergarment during physical therapy treatment assists muscle action by helping the correction of the soft tissues and muscle imbalance, and realigning the position of the joints.32 Similar results from previous studies stated that the use of soft orthosis can assist weak muscles and correct abnormal body positions or movement patterns from non-structural sources.33,34
The most interesting finding in this study is improved balance, trunk position sense, and trunk control post-treatment, and adding TheraTogs to conventional physiotherapy in the study group revealed significantly higher post-treatment postural control compared to the control group (p = 0.001) (Table 3). The improved postural control in the studied children may be attributed to several factors including reduced spasticity, increased muscle length, and increased proprioceptive stimulation as wearing TheraTogs provides support to hip muscles and improves force generated by gluteus maximus and gluteus medius muscles which helps orient these muscles to normal.16,35,36 TheraTogs was reported to exert a gentle, passive force to improve alignment via a combined trunk-extremities system. The application of TheraTogs could enhance joint stability and posture.16,36 This results in a unique biomechanical state and improved proprioception which in turn stimulates and modifies the neuro-sensory system and trains muscles to work with the modulated muscle tone, strength, and subsequently improved performance.37 A previous study in stroke patients and hemiplegia showed that wearing TheraTogs improved balance in the standing position. The enhanced proprioceptive awareness and postural alignment provide a sense of safety adding to postural control.38
TheraTogs strapping system could modify and manipulate components of the musculoskeletal and sensory systems to accomplish corrected biomechanical alignment, increase proprioceptive input which improves percept of correct spatial orientation, and increase trunk stiffness, which improves proximal stability and reduce the number of body segments needed to coordinate when trying to balance and move.6,39 it could be explained by the prolonged use of TheraTogs exerts a continuous inhibitory reflex for abnormal internal rotation and hip adduction in the spastic limb leading to improved action of agonist-antagonist muscle groups.38
In our study, we found that the six-minute walking distance was significantly improved in both groups following treatment. This finding is supported by the previous report34 which revealed significantly improved walking speed following the application of protocol including physiotherapy and TheraTogs in patients with hemiplegia. Physiotherapy and TheraTogs improve muscle activity and support which can improve walking distance.38 The improved 6MWD could be attributed to improved gait parameters and postural control which decreases energy consumption during walking.
A recent systematic review reported that dynamic orthosis has a positive effect on gait and the results were better with longer duration (12–18 weeks) and with orthosis as an add-on therapy to conventional rehabilitation programs.40 6MWT is a validated bedside tool for the measurement of muscle endurance.41 A study in multiple sclerosis reported that a six-minute walk test is more informative for the functional state than other gait parameters.42
Rehabilitation services utilization is a complex process and is related to several factors including social, economic, behavioral, and ecological factors. Children with CP need more care and the design of physical therapy programs is encouraged among this special category.43
This study introduced a new physical therapy technique that might lead to improved outcomes of rehabilitation programs. Besides, we studied the long-term effect of wearing TheraTogs.
This study has some limitations that need to be further resolved in future studies, first, we used combined physical therapy with wearing TheraTogs in the study group so we cannot isolate the effect of TheraTogs. However, this limitation could not be overcome at the current time as we could not abolish the standard therapy for those in need. Second, the results of this study can be applied only to children with spastic diplegic cerebral palsy.
Conclusion
Both conventional physical therapy (CPT) and TheraTogs orthosis improve foot plantar pressure distribution, balance scale, and six-minute walking distance in children with spastic diplegic CP. TheraTogs is a useful add-on therapy to CPT programs and is superior to CPT alone in improving foot pressure distribution, achieving better balance, and longer 6MWD. Further studies are warranted to investigate the effect of TheraTogs on physiologic muscle indices such as strength, energy expenditure, range of movement, and quality of life.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors would like to express sincere gratitude to the Deputyship for Research & Innovation, Ministry of Education in Saudi Arabia for funding this research work through project number (442/21). Also, the authors would like to extend their appreciation to Taibah University for its supervision and continuous support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Oskoui M, Coutinho F, Dykeman J, Jetté N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013;55(6):509–519. doi:10.1111/DMCN.12080
2. CDC. Data and statistics for cerebral palsy. Available from: https://www.cdc.gov/ncbddd/cp/data.html.
3. Sadowska M, Sarecka-Hujar B, Kopyta I. Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. 2020;16:1505–1518. doi:10.2147/NDT.S235165
4. Hanssen B, Peeters N, Vandekerckhove I, et al. The contribution of decreased muscle size to muscle weakness in children with spastic cerebral palsy. Front Neurol. 2021:12. doi:10.3389/fneur.2021.692582
5. Howard JJ, Herzog W. Skeletal muscle in cerebral palsy: from belly to myofibril. Front Neurol. 2021;12. doi:10.3389/fneur.2021.620852
6. Patel DR, Neelakantan M, Pandher K, Merrick J. Cerebral palsy in children: a clinical overview. Transl Pediatr. 2020;9(Suppl 1):S125. doi:10.21037/TP.2020.01.01
7. Theologis T. Lever arm dysfunction in cerebral palsy gait. J Child Orthop. 2013;7(5):379–382. doi:10.1007/s11832-013-0510-y
8. Armand S, Decoulon G, Bonnefoy-Mazure A. Gait analysis in children with cerebral palsy. EFORT Open Rev. 2016;1(12):448–460. doi:10.1302/2058-5241.1.000052
9. Crenshaw JR, Petersen DA, Conner BC, et al. Anteroposterior balance reactions in children with spastic cerebral palsy. Dev Med Child Neurol. 2020;62(6):700–708. doi:10.1111/dmcn.14500
10. Waltersson L, Rodby-Bousquet E. Physical activity in adolescents and young adults with cerebral palsy. Biomed Res Int. 2017;2017:1–6. doi:10.1155/2017/8080473
11. Rethlefsen SA, Blumstein G, Kay RM, Dorey F, Wren TAL. Prevalence of specific gait abnormalities in children with cerebral palsy revisited: influence of age, prior surgery, and gross motor function classification system level. Dev Med Child Neurol. 2017;59(1):79–88. doi:10.1111/dmcn.13205
12. Brehm MA, Harlaar J, Schwartz M. Effect of ankle-foot orthoses on walking efficiency and gait in children with cerebral palsy. J Rehabil Med. 2008;40(7):529–534. doi:10.2340/16501977-0209
13. Kim MJ. Rehabilitative Intervention. Available from: http://www.e-hmr.org.
14. Papavasiliou A, Ben-Pazi H, Mastroyianni S, Ortibus E. Editorial: cerebral palsy: new developments. Front Neurol. 2021;12. doi:10.3389/fneur.2021.738921
15. TheraTogs. Therapy you can wear!; 2023. Available from: https://theratogs.com/.
16. Ehlert R, Manfio EF, de Heidrich RO, Goldani R. Cerebral palsy: influence of TheraTogs ® on gait, posture and in functional performance. Fisioterapia em Movimento. 2017;30(2):307–317. doi:10.1590/1980-5918.030.002.ao11
17. El-Shamy SM, El-Kafy EMA. Combined effect of orthotic intervention and conventional exercise training on balance and gait performance in cerebral palsy: a randomized controlled trial. Bull Facul Physical Thera. 2022;27(1). doi:10.1186/s43161-022-00071-1
18. Bohannon RW, Smith MB. Interrater reliability of a modified ashworth scale of muscle spasticity. Phys Ther. 1987;67(2):206–207. doi:10.1093/PTJ/67.2.206
19. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223. doi:10.1111/J.1469-8749.1997.TB07414.X
20. Becerro-de-bengoa-vallejo R, Losa-Iglesias ME, Rodriguez-Sanz D. Static and dynamic plantar pressures in children with and without sever disease: a case-control study. Phys Ther. 2014;94(6):818–826. doi:10.2522/PTJ.20120164
21. Bruyneel AV, Reinmann A, Sordet C, Venturelli P, Feldmann I, Guyen E. Reliability and validity of the trunk position sense and modified functional reach tests in individuals after stroke. Physiother Theory Pract. 2022;1–10. doi:10.1080/09593985.2022.2101407
22. Ravizzotti E, Vercelli S, Pellicciari L, Furmanek MP, Zagnoni G, Piscitelli D. Reliability and validity of the trunk control measurement scale among children and adolescents with cerebral palsy in Tanzania. Percept Mot Skills. 2021;128(2):731–745. doi:10.1177/0031512520983701
23. Heyrman L, Molenaers G, Desloovere K, et al. A clinical tool to measure trunk control in children with cerebral palsy: the trunk control measurement scale. Res Dev Disabil. 2011;32(6):2624–2635. doi:10.1016/j.ridd.2011.06.012
24. PediatricBalanceScale_3. Available from: https://www.sralab.org/sites/default/files/2017-06/PediatricBalanceScale_3.pdf.
25. Crapo RO, Casaburi R, Coates AL, et al. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi:10.1164/AJRCCM.166.1.AT1102
26. El Aziz HG A, Khatib AHE, Hamada HA. Does the type of toeing affect balance in children with diplegic cerebral palsy? An observational cross-sectional study. J Chiropr Med. 2019;18(3):229–235. doi:10.1016/j.jcm.2019.01.005
27. Kadhim M, Miller F. Crouch gait changes after planovalgus foot deformity correction in ambulatory children with cerebral palsy. Gait Posture. 2014;39(2):793–798. doi:10.1016/J.GAITPOST.2013.10.020
28. Galli M, Cimolin V, Pau M, Leban B, Brunner R, Albertini G. Foot pressure distribution in children with cerebral palsy while standing. Res Dev Disabil. 2015;41–42:52–57. doi:10.1016/j.ridd.2015.05.006
29. El-Kafy EM A. The clinical impact of orthotic correction of lower limb rotational deformities in children with cerebral palsy: a randomized controlled trial. Clin Rehabil. 2014;28(10):1004–1014. doi:10.1177/0269215514533710
30. Bahramizadeh M, Rassafiani M, Aminian G, Rashedi V, Farmani F, Mirbagheri SS. Effect of dynamic elastomeric fabric orthoses on postural control in children with cerebral palsy. Pediatric Physical Therapy. 2015;27(4):349–354. doi:10.1097/PEP.0000000000000171
31. Ganjwala D, Shah H. Management of the knee problems in spastic cerebral palsy. Indian J Orthop. 2019;53(1):53. doi:10.4103/ORTHO.IJORTHO_339_17
32. Levitt S, Addison A, Anne C. Treatment of cerebral palsy and motor delay; 2019. Available from: https://www.wiley.com/en-us/Treatment+of+Cerebral+Palsy+and+Motor+Delay%2C+6th+Edition-p-9781119373599.
33. Martins E, Cordovil R, Oliveira R, Pinho J, Diniz A, Vaz JR. The immediate effects of a dynamic orthosis on gait patterns in children with unilateral spastic cerebral palsy: a kinematic analysis. Front Pediatr. 2019;7(FEB). doi:10.3389/FPED.2019.00042/FULL
34. Fergus A. A novel mobility device to improve walking for a child with cerebral palsy. Pediatric Physical Therapy. 2017;29(4):E1–E7. doi:10.1097/PEP.0000000000000451
35. Maguire C, Sieben JM, Frank M, Romkes J. Hip abductor control in walking following stroke - The immediate effect of canes, taping and TheraTogs on gait. Clin Rehabil. 2010;24(1):37–45. doi:10.1177/0269215509342335
36. Flanagan A, Krzak J, Peer M, Johnson P, Urban M. Evaluation of short-term intensive orthotic garment use in children who have cerebral palsy. Pediatric Physical Therapy. 2009;21(2):201–204. doi:10.1097/PEP.0B013E3181A347AB
37. DM Orthotics. Why fabric orthoses are a good option for cerebral palsy. Available from: https://www.dmorthotics.com/news-events/why-fabric-orthoses-are-a-good-option-for-cerebral-palsy.
38. Abdel-Raouf El-Fiky A, Abd El Kafy E. Effect of TheraTogs orthotic undergarment on postural balance control, risk of fall, and walking abilities in Saudi individuals with chronic stroke The awareness of healthcare staff towards post-stroke cognitive impairment: a cross sectional study view project high-intensity laser therapy versus pulsed electromagnetic field in the treatment of primary dysmenorrhea view project. Jokull J. 2016;66(5):23–35.
39. Kwon HY, Ahn SY. Effect of task-oriented training and high-variability practice on gross motor performance and activities of daily living in children with spastic diplegia. J Phys Ther Sci. 2016;28(10):2843. doi:10.1589/JPTS.28.2843
40. Belizón-Bravo N, Romero-Galisteo RP, Cano-Bravo F, Gonzalez-Medina G, Pinero-Pinto E, Luque-Moreno C. Effects of dynamic suit orthoses on the spatio-temporal gait parameters in children with cerebral palsy: a systematic review. Children. 2021;8(11):1016. doi:10.3390/children8111016
41. Kamiya K, Hamazaki N, Matsue Y, et al. Gait speed has comparable prognostic capability to six-minute walk distance in older patients with cardiovascular disease. Eur J Prev Cardiol. 2018;25(2):212–219. doi:10.1177/2047487317735715
42. Chen S, Sierra S, Shin Y, Goldman MD. Gait speed trajectory during the six-minute walk test in multiple sclerosis: a measure of walking endurance. Front Neurol. 2021;12:1097. doi:10.3389/FNEUR.2021.698599/BIBTEX
43. Al Imam MH, Jahan I, Das MC, et al. Rehabilitation status of children with cerebral palsy in Bangladesh: findings from the Bangladesh cerebral palsy Register. PLoS One. 2021;16(5):e0250640. doi:10.1371/JOURNAL.PONE.0250640
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
