Back to Journals » Clinical Interventions in Aging » Volume 19
Effects of Anticoagulant Therapy and Frailty in the Elderly Patients with Atrial Fibrillation
Authors Ding J, Sun Y, Zhang K, Huang W, Tang M , Zhang D , Xing Y
Received 6 December 2023
Accepted for publication 30 January 2024
Published 14 February 2024 Volume 2024:19 Pages 247—254
DOI https://doi.org/10.2147/CIA.S453527
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Jiancao Ding,1 Ying Sun,2 Kan Zhang,2 Wei Huang,2 Mei Tang,2 Dai Zhang,2 Yunli Xing2
1Department of Geriatrics, First People’s Hospital of Zigong, Sichuan, People’s Republic of China; 2Department of Geriatrics, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Yunli Xing, Department of Geriatrics, Beijing Friendship Hospital, Capital Medical University, No. 95, Yongan Road, Xicheng District, Beijing, 100050, People’s Republic of China, Tel +86 13121181469, Fax +86 10 6313 8040, Email [email protected]
Objective: This study explored whether anticoagulation is safe for frail and non-frail elderly patients who have nonvalvular atrial fibrillation (NVAF).
Methods: At hospital discharge, the anticoagulant regimen and frailty status were recorded for 361 elderly patients (aged ≥ 75 y) with NVAF. The patients were followed for 12 months. The endpoints included occurrence of thrombosis; bleeding; all-cause death; and cardiovascular events.
Results: At hospital discharge, frailty affected 50.42% of the population and the anticoagulation rate was 44.04%. At discharge, age (OR 0.948, P = 0.006), paroxysmal NVAF (OR 0.384, P < 0.001), and bleeding history (OR 0.396, P = 0.001) were associated with a decrease in rate of receiving anticoagulation, while thrombotic events during hospitalization (OR 2.281, P = 0.021) were associated with an increase. Relative to non-frail patients, those with frailty showed a higher rate of ischemic stroke (5.33% cf. 3.01%), bleeding (P = 0.006) events, and all-cause mortality (P = 0.001). Relative to the group without anticoagulation, in those with anticoagulation the rate of thrombotic events was lower (6.99 cf. 10.98%) and bleeding events were higher (20.98 cf. 12.72%), but the risk of major bleeding was comparable.
Conclusion: In the elderly patients with NVAF, the decision toward anticoagulation therapy at hospital discharge was influenced by age, bleeding history, paroxysmal atrial fibrillation diagnosis, and absence of thrombosis. Frail patients were at greater risk of bleeding and all-cause mortality. Anticoagulation tended to reduce the risk of thrombotic events.
Keywords: elderly, non-valvular atrial fibrillation, frailty, anticoagulation
A Letter to the Editor has been published for this article.
Introduction
Atrial fibrillation (AF) is a common arrhythmia in the elderly population, affecting up to 12% of people aged 80 years and older1 and can raise the risk of stroke by five-fold.2 AF and related stroke in the elderly seriously affect their quality of life and greatly increase the burden on the healthcare industry.
Frailty is also a common geriatric syndrome that has been associated with adverse events such as disability, hospital-acquired infection, and mortality.3 Frail elderly patients with AF especially may have a higher risk of stroke and bleeding, and are often complicated with sarcopenia, malnutrition, and multiple comorbidities. Additionally, they are more susceptible to drug side effects. However, the presence of frailty is rarely included as a factor in clinical studies of anticoagulation therapy, and this lack of data confounds management decisions.
Although anticoagulation is cost-effective in reducing stroke risk in AF,4 it is sometimes not applied to the elderly, despite indications, especially in those with frailty.5 Relevant studies have shown that elderly patients with AF may need timely anticoagulation, yet there is no unified opinion about whether this therapy will improve prognosis.4,6 More research evidence is needed.
This study explored whether anticoagulation is safe for elderly patients with AF, and the influence of frailty on medical decisions. We conducted an overall evaluation of elderly patients with nonvalvular atrial fibrillation (NVAF), aged 75 years and older, aided by a comprehensive geriatric assessment.
Methods
This study was approved by the Ethics Committee of Beijing Friendship Hospital, Capital Medical University (Research Ethics number 2018-P2-037-02). This study was in compliance with the Declaration of Helsinki.
Participants
The study enrollment comprised elderly patients with NVAF who were hospitalized in the geriatric and cardiovascular departments of Beijing Friendship Hospital from May 2017 to March 2022. All the subjects were aged 75 years or older, and with AF as verified by ECG (electrocardiogram) or 24-hour ECG with onset ≥30 s. AF types included both paroxysmal (terminating within 7 days, with or without intervention) and persistent (lasting more than 7 days). Patients with any of the following were excluded: AF due to hyperthyroidism; AF combined with mechanical valve or moderate-to-severe mitral stenosis; or failure to sign informed consent or to cooperate with the study.
A comprehensive geriatric assessment was conducted of each enrolled patient, which included polypharmacy (ie, more than 5 kinds of medicines)7 and measures for frailty, daily living activities, cognitive status, nutritional status, fall risk, burden of comorbidities, AF stroke risk, and bleeding risk. The assessments included the respective components of the FRAIL index (Fatigue, Resistance, Ambulation, Illness and Loss of weight).8 Each of FRAIL index components was scored with 1 point for presence or 0 (nil) for absence, for a maximum score of 5. Scores of 3 to 5 indicated frailty; patients with scores lower than 3 were characterized as non-frail.
Other scales applied in the present study were: Assessment of Daily Living;9 Mini-Cognitive Assessment (Mini-Cog);10 Mini Nutritional Assessment short-form (MNA-SF);11 Morse Falls Assessment Scale;12 age-adjusted Charlson Comorbidity Index (aCCI);13 CHA2DS2-VASc score;14 and the HAS-BLED score.14
In addition, demographics were recorded and the following clinical data from the medical records: medical history, vital signs, fasting blood; and the estimated glomerular filtration rate (eGFR) calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI)15 equation.
The patients’ anticoagulation regimens were recorded at the time of discharge. The patients were followed up at 1, 3, 6, and 12 months via telephone or medical records. The median follow-up period was 12 (11, 12) months. The study deadline was 31 October 2022. The follow-up data included observed events (below) and anticoagulation status, anticoagulation/antiplatelet regimens, compliance, and whether anticoagulation was used before and after bleeding/thrombosis. Observed events were thromboembolism, bleeding, all-cause death, and cardiovascular events. Thromboembolism included systemic circulation (transient ischemic attack, stroke, peripheral) and pulmonary embolism. Bleeding events were either minor or major, the latter including intracranial, spinal, or retroperitoneal bleeding with direct fatal or surgical treatment required; red blood cell transfusion of 2 or more units; a decrease in hemoglobin concentration of 50 g/L or more; and hemorrhagic shock. Cardiovascular events were acute heart failure and acute coronary syndrome.
Statistical Analysis
All data were analyzed with SPSS 25.0, and patient characteristics are shown as the mean ± standard deviation (x ± SD), median (interquartile range) [M (Q1, Q3)], or percentage (%). Logistic regression was used to analyze factors influencing anticoagulation and compliance. Some variables that may be potential confounders were selected for the univariate analysis; items with P < 0.05 in the results were included in the multivariate analysis, and the 95% confidence intervals (CIs) were calculated. Cox proportional hazards analyses were performed to examine, respectively, the associations between frailty and anticoagulation on bleeding, thrombosis, all-cause death, and cardiovascular events. A pooled hazard ratio (HR) was calculated for each factor; a P value < 0.05 was considered significant.
Results
The study population comprised 361 patients with NVAF (234 men) with a median age of 85 (81, 90) years. Of these, 231 (63.99%) and 130 (36.01%) were with paroxysmal and persistent AF, respectively. The most common diseases were hypertension (83.10%, n = 300), ischemic stroke (52.91%, n = 191), and diabetes (40.72%, n = 147). The overall prevalence of frailty was 50.42% (n = 182). The anticoagulation rate was significantly higher at discharge than at admission (44.04% cf. 22.71%, P < 0.001). In addition, 36.8% received antiplatelets (n = 133). The rate of new oral anticoagulants (NOACs) was 69.51% at admission (n = 57) and 73.58% at discharge (n = 117)). Only 29 patients received the standard doses (ie, rivaroxaban 20 mg, edoxaban 60 mg, dabigatran 220 mg).
Influencing Factors of Anticoagulation
At hospital discharge, 159 of the 361 subjects were given anticoagulation regimens (Tables 1 and 2). Relative to those without anticoagulation regimens, those with anticoagulation were significantly more likely to be: younger and female; with paroxysmal AF (cf. persistent AF); frailty; and bleeding history. They also had significantly higher body mass index (BMI); rate of thrombosis during hospitalization; Assessment of Daily Living, MNA-SF, and Mini-cog scores; and hemoglobin and albumin levels.
 |
Table 1 Patients with or Without Anticoagulation at Hospital Dischargea |
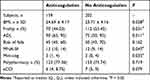 |
Table 2 CGA Items of Patients with or Without Anticoagulation at Hospital Dischargea |
The following were found likely factors for anticoagulation at discharge (Tables 1 and 2): age (OR 0.948, 95% CI 0.913–0.985, P = 0.006); paroxysmal AF (OR 0.384, 95% CI 0.233–0.635, P < 0.001); bleeding history (OR 0.396, 95% CI 0.226–0.694, P = 0.001); and thrombosis during hospitalization (OR 2.281, 95% CI 1.130–4.607, P = 0.021).
Influence of Anticoagulation on Prognosis
After removing 33 patients from the present analysis who died in hospital and 11 patients who were lost to follow-up, 316 patients were followed (203 men and 113 women), and changes in anticoagulation during the follow-up were noted (Figure 1).
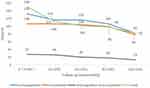 |
Figure 1 Drug compliance of anticoagulation and antiplatelet during follow-up. |
In all, 52 bleeding events were observed. Of these, 4 patients had major bleeding, including 1 patient with gastrointestinal bleeding (from carcinoma of the esophagus) who did not take anticoagulants. Three patients experienced intracranial hemorrhage, one of whom (with no anticoagulant/antiplatelet regimen) suffered from cerebral trauma; another 1 patient suffered from fall, and took aspirin and clopidogrel. One patient took warfarin (2.25 mg/d), and there were cerebral microbleeds in the right temporal lobe and the left cerebellar dentate nucleus. In this last patient, anticoagulation was not stopped after bleeding and major bleeding did not occur again. Furthermore, 29 thromboembolic events were observed, including 13 strokes (8 patients with frailty). There were 51 cardiovascular events and 56 all-cause deaths. Forty-nine patients withdrew from the medication of their own volition.
Differences were analyzed between the patients with and without anticoagulation (Table 3). The patients with anticoagulation had fewer thrombotic events (6.99% cf. 10.98%) and all-cause deaths (17.48% cf. 17.92%), but more bleeding events (20.98% cf. 12.72%). In addition, patients with anticoagulation had poor compliance.
 |
Table 3 Observed Events in Patients with or Without Anticoagulation or Frailtya |
The Cox regression analysis (which was adjusted for age, sex, daily activity, fall risk, cognition, nutrition, comorbidities, stroke, and bleeding risk) showed that anticoagulation tended to increase the bleeding risk (HR 0.584, 95% CI 0.337–1.013, P = 0.056). Anticoagulation was not associated with thromboembolic events (HR 1.618, 95% CI 0.752–3.479, P = 0.218), or all-cause death (HR 1.091, 95% CI 0.639–1.863, P = 0.750; Table 4). The analysis also showed that frailty (after adjusting for age, sex, type of AF, presence of anticoagulation, comorbidities, ability to perform daily living activities, risk of fall, polypharmacy, and cognitive and nutritional status) was associated with an increased risk of bleeding (HR 2.294, 95% CI 1.264–4.160, P = 0.006) and all-cause death (HR 4.947, 95% CI 1.999–12.242, P = 0.001), but fatal bleeding did not increase. The frail group experienced a higher rate of cardiovascular events, but not significantly, and frailty was not associated with thrombosis.
 |
Table 4 Cox Regression Analysis of the Effects of Anticoagulation and Frailty on Clinical Events |
Discussion
Evidence for anticoagulation in elderly patients with AF is relatively insufficient, which leads to caution of administration by physicians.16 The present study followed elderly patients with NVAF after hospital discharge, with particular attention given to the presence of frailty and anticoagulation regimen. It was determined that assignment of an anticoagulation regimen at hospital discharge for our elderly patients with NVAF was negatively influenced by the patient’s age, paroxysmal AF (rather than persistent AF), history of bleeding, and absence of thromboembolism during hospitalization. Yet the anticoagulation rate at discharge (44%) was higher than at admission (23%), suggesting the effectiveness of medical intervention. The prevalence of frailty in the overall population was 50.4%, and frailty significantly increased the risk of bleeding and all-cause death. Ischemic stroke and cardiovascular events were also higher in the frail group, relative to the non-frail. Overall, there was no fatal bleeding caused by anticoagulation. We encourage elderly patients with NVAF, even those who are frail, to try anticoagulation, with close monitoring to ensure safety. However, longer prospective studies of such patients are wanted.
Both the prevalence of AF and frailty increase with age, and they often occur simultaneously. In our study about half of the patients were adjudged frail. This is similar to a previous meta-analysis.17 Frailty affects both the management and the prognosis of AF in the geriatric population. In the present study, frailty not only increased the incidence of all-cause death, but also significantly increased the risk of bleeding (OR 1.64, 95% CI 1.11–2.41). Therefore, an assessment of geriatric frailty should be considered when planning individualized management of AF in older patients.14,18
Paroxysmal AF is often believed, mistakenly, to carry a lower risk of thrombotic events compared with persistent AF.19 Regarding the history of bleeding as a factor for choosing anticoagulation, guidelines have emphasized that anticoagulation should be considered only after correction of the factors that increase the risk of bleeding. But even in patients with AF who have suffered intracerebral hemorrhage, resuming anticoagulation can significantly reduce the risk of death/ischemic stroke/peripheral vascular embolism, while not increasing the recurrence rate of intracerebral hemorrhage.20
Furthermore, it is undeniable that elderly patients with NVAF without anticoagulation have concomitant vulnerabilities, including lower BMI, higher prevalence of frailty, worse daily activities, poorer nutritional and cognitive status, and greater polypharmacy, which all increase the health burden of the elderly population. For example, a study from Spain that included 4724 patients with AF aged 80 years and older found that 43% of the patients were malnourished.21 Malnutrition was not only an independent risk factor for morbidity and mortality, but also was associated with risk of ischemic stroke and major bleeding. For patients with multiple medications, each additional drug was associated with a 4% increased risk of all-cause death (HR 1.04, 95% CI 1.00–1.08), and a 5% increased risk of cardiovascular death (HR 1.05, 95% CI 1.00–1.10).22 We conclude that clinical treatment of elderly patients with NVAF should be guided by a prompt comprehensive geriatric assessment.
NOACs are the most widely used anticoagulant drug, perhaps because they are more effective than warfarin in reducing adverse events such as bleeding and thrombotic events.23 However, in the present study the dose of NOACs generally was lower than the standard dose recommended by guidelines. A previous study of elderly patients with AF who were at high risk of thrombosis showed that the standard dose of anticoagulant drugs did not increase the risk of bleeding, but a reduced dose of NOAC was not effective in lowering the stroke rate.24 In addition, the proportion of antiplatelet therapy in the present study was not low (36.8%), but its effect on stroke prevention was limited.
The patients in this study demonstrated poor compliance with anticoagulation, and those with better cognitive status were more likely to self-withdraw. As they gained information from outer sources, many patients stopped taking anticoagulants for fear of side effects such as bleeding, although they had not experienced bleeding events. This reflects that our study population did not know enough about anticoagulation in AF, and that our health education and monitoring during treatment was insufficient. Patients became focused on the possible harms, but not the benefits of stroke prevention offered by the recommended medical interventions.
Anticoagulation did not increase the risk of adverse outcomes. This study found that anticoagulation was appropriate and beneficial for elderly patients with NVAF. Although the difference in the occurrence of observed events was not statistical between the patients with and without anticoagulation, for the former the incidence of thrombosis was lower while the rate of major bleeding was similar. Patients who took anticoagulants before bleeding and continued anticoagulation also did not suffer a higher rate of major bleeding compared to those who did not.
Several other studies have focused on the effect of anticoagulation on the prognosis of very elderly patients with NVAF. Kim et al4 observed the effects of oral anticoagulants and different regimens on patients’ prognosis, and determined that oral anticoagulants were associated with a lower risk of ischemic stroke (HR 0.91, 95% CI 0.86–0.97) and cardiovascular death (HR 0.52, 95% CI 0.99–0.55), with no difference in major bleeding events (HR 1.02, 95% CI 0.95–1.10). However, a large European cohort study regarding AF (n = 10,177 patients) found a significant reduction in all-cause mortality in patients treated with oral anticoagulants when the frailty index was between 0.05 and 0.36; there was no difference in patients with a higher frailty index.5 The ABC (Atrial fibrillation Better Care) pathway could be helpful in reducing the risk of major outcomes, with a clear trend towards greater benefit for those with high complexity cluster.25,26
Study Limitations
Our analysis has some limitations. Firstly, a short follow-up period may have lowered the rate of long-term adverse events; only hospitalized patients in a single center were included, and the results may not apply to the broader population. Secondly, changes in patients’ frailty may have occurred during the follow-up, but this was not reevaluated. Finally, unlike in a previous study, we did not find that anticoagulation was associated with thromboembolic events. This may be due to definitively unknown confounding factors, leading to indication bias. For example, patients who were at higher risk of bleeding may not have initially received anticoagulants.
Conclusion
Because the effects of anticoagulation in the very elderly with AF are little known, especially in the context of frailty, this study followed patients with NVAF, aged at least 75 years, for 12 months after hospital discharge. It was found that the factors that lowered the rate of anticoagulation administration at discharge were higher age, paroxysmal AF (as opposed to persistent AF), and history of bleeding. Patients were more likely given anticoagulation if they had suffered thrombotic events during hospitalization. Frail patients, compared with the non-frail, showed an increased risk of bleeding, and all-cause death. A geriatric assessment of frailty for older patients with AF is important. Patients given anticoagulant therapy experienced fewer thromboembolic events, and there was no increase in fatal bleeding. It is also worth mentioning that most of the anticoagulant drugs in this study were NOACs, but compliance with anticoagulation was poor. The ABC (Atrial fibrillation Better Care) pathway might be helpful to reduce the risk of major outcomes.
Acknowledgments
We are grateful to the patients who contributed their data for research. We acknowledge the contribution made by the teachers of the Methodology Platform of Beijing Friendship Hospital.
Funding
This work was funded by the National Key R&D Program of China (2021ZD0111000). The authors were solely responsible for the design, implementation, data analysis, writing, and revision of the paper for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Andrade JG, Aguilar M, Atzema C, et al. The 2020 Canadian cardiovascular society/Canadian heart rhythm society comprehensive guidelines for the management of atrial fibrillation. Can J Cardiol. 2020;36(12):1847–1948. doi:10.1016/j.cjca.2020.09.001
2. Choi SE, Sagris D, Hill A, et al. Atrial fibrillation and stroke. Expert Rev Cardiovasc Ther. 2023;21(1):35–56. doi:10.1080/14779072.2023.2160319
3. Cesari M, Prince M, Thiyagarajan JA, et al. Frailty: an emerging public health priority. J Am Med Dir Assoc. 2016;17(3):188–192. doi:10.1016/j.jamda.2015.12.016
4. Kim D, Yang PS, Sung JH, et al. Effectiveness and safety of anticoagulation therapy in frail patients with atrial fibrillation. Stroke. 2022;53(6):1873–1882. doi:10.1161/STROKEAHA.121.036757
5. Proietti M, Romiti GF, Vitolo M, et al. Epidemiology and impact of frailty in patients with atrial fibrillation in Europe. Age Ageing. 2022;51(8):afac192. doi:10.1093/ageing/afac192
6. Oldgren J, Åsberg S, Hijazi Z, et al. Early versus delayed non-vitamin K antagonist oral anticoagulant therapy after acute ischemic stroke in atrial fibrillation (TIMING): a registry-based randomized controlled noninferiority study. Circulation. 2022;146(14):1056–1066. doi:10.1161/CIRCULATIONAHA.122.060666
7. Beezer J, Al Hatrushi M, Husband A, et al. Polypharmacy definition and prevalence in heart failure: a systematic review. Heart Fail Rev. 2022;27(2):465–492. doi:10.1007/s10741-021-10135-4
8. Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a Review. Eur J Intern Med. 2016;31:3–10. doi:10.1016/j.ejim.2016.03.007
9. Krempley T, Schmidt EK. Assessing activity of daily living task performance among autistic adults. Autism Adulthood. 2021;3(1):37–51. doi:10.1089/aut.2020.0042
10. Carnero-Pardo C, Rego-García I, Barrios-López JM, et al. Assessment of the diagnostic accuracy and discriminative validity of the clock drawing and mini-cog tests in detecting cognitive impairment. Neurologia. 2022;37(1):13–20. doi:10.1016/j.nrleng.2018.12.022
11. Liu H, Jiao J, Zhu M, et al. Nutritional status according to the short-form mini nutritional assessment (MNA-SF) and clinical characteristics as predictors of length of stay, mortality, and readmissions among older inpatients in china: a national study. Front Nutr. 2022;9:815578. doi:10.3389/fnut.2022.815578
12. Kim YJ, Choi KO, Cho SH, et al. Validity of the morse fall scale and the Johns Hopkins fall risk assessment tool for fall risk assessment in an acute care setting. J Clin Nurs. 2022;31(23–24):3584–3594. doi:10.1111/jocn.16185
13. Di Donato V, O D, Giannini A, et al. Age-adjusted Charlson comorbidity index predicts survival in endometrial cancer patients. Gynecol Obstet Invest. 2022;87(3–4):191–199. doi:10.1159/000525405
14. Hindricks G, Potpara T, Dagres N, et al.; ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery. for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European society of cardiology (ESC). Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
15. Meeusen JW, Kasozi RN, Larson TS, et al. Clinical impact of the refit CKD-EPI 2021 creatinine-based eGFR. Equation Clin Chem. 2022;68(4):534–539. doi:10.1093/clinchem/hvab282
16. Calsolaro V, Okoye C, Antognoli R, et al. Long-term effectiveness and safety of anticoagulation therapy in oldest old, frail people with atrial fibrillation. Eur J Intern Med. 2021;86:91–97. doi:10.1016/j.ejim.2021.01.020
17. Proietti M, Romiti GF, Raparelli V, et al. Frailty prevalence and impact on outcomes in patients with atrial fibrillation: a systematic review and meta-analysis of 1,187,000 patients. Ageing Res Rev. 2022;79:101652. doi:10.1016/j.arr.2022.101652
18. Guo Q, Du X, Ma CS. Atrial fibrillation and frailty. J Geriatr Cardiol. 2020;17(2):105–109. doi:10.11909/j.issn.1671-5411.2020.02.007
19. Bahri O, Roca F, Lechani T, et al. Underuse of oral anticoagulation for individuals with atrial fibrillation in a nursing home setting in France: comparisons of resident characteristics and physician attitude. J. Am Geriatr Soc. 2015;63(1):71–76. doi:10.1111/jgs.13200
20. Wu VC, Huang YC, Chen SW, et al. Resuming anticoagulation in patients with atrial fibrillation experiencing intracranial hemorrhage. Medicine. 2021;100(32):e26945. doi:10.1097/MD.0000000000026945
21. Raposeiras-Roubín S, Abu-Assi E, Paz RC, et al. Impact of malnutrition in the embolic-haemorrhagic trade-off of elderly patients with atrial fibrillation. Europace. 2020;22(6):878–887. doi:10.1093/europace/euaa017
22. Tsagkaris C, Papazoglou AS, Kartas A, et al. Polypharmacy and major adverse events in atrial fibrillation. J Cardiovasc Pharmacol. 2022;80(6):826–831. doi:10.1097/FJC.0000000000001339
23. Patel P, Pandya J, Goldberg M. NOACs vs. Warfarin for stroke prevention in nonvalvular atrial fibrillation. Cureus. 2017;9(6):e1395. doi:10.7759/cureus.1395
24. Kido K, Shimizu M, Shiga T, et al. Meta-analysis comparing inappropriately low dose versus standard dose of direct oral anticoagulants in patients with atrial fibrillation. J Am Pharm Assoc. 2022;62(2):487–495. doi:10.1016/j.japh.2021.10.027
25. Romiti GF, Proietti M, Vitolo M, et al. Clinical complexity and impact of the ABC (Atrial fibrillation Better Care) pathway in patients with atrial fibrillation: a report from the ESC-EHRA EURO observational research programme in AF general long-term registry. BMC Med. 2022;20(1):326. doi:10.1186/s12916-022-02526-7
26. Trinks-Roerdink EM, Geersing GJ, van den Dries CJ, et al. Integrated care in patients with atrial fibrillation- a predictive heterogeneous treatment effect analysis of the ALL-IN trial. PLoS One. 2023;18(10):e0292586. doi:10.1371/journal.pone.0292586
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
