Back to Journals » Medical Devices: Evidence and Research » Volume 13
Evaluation of Human Esophageal Epithelium Permeability in Presence of Different Formulations Containing Hyaluronic Acid and Chondroitin Sulphate
Authors Pellegatta G, Spadaccini M, Lamonaca L, Craviotto V, D'Amico F, Ceriotti L , Meloni M , Repici A
Received 18 October 2019
Accepted for publication 11 February 2020
Published 4 March 2020 Volume 2020:13 Pages 57—66
DOI https://doi.org/10.2147/MDER.S234810
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Gaia Pellegatta,1 Marco Spadaccini,1 Laura Lamonaca,1 Vincenzo Craviotto,1 Ferdinando D’Amico,1 Laura Ceriotti,2 Marisa Meloni,2 Alessandro Repici1
1Humanitas Clinical and Research Center and Humanitas University, Digestive Endoscopy Unit, Division of Gastroenterology, Rozzano, MI, Italy; 2VitroScreen, Milano, Italy
Correspondence: Gaia Pellegatta
Digestive Endoscopy Unit, Division of Gastroenterology, Humanitas Research Hospital, Via Manzoni 56, Rozzano, MI 20089, Italy
Tel +390282247091
Email [email protected]
Purpose: New medical devices that contain hyaluronic acid (HA) and chondroitin sulphate (CS), with or without antacid components, have been developed for the treatment of gastroesophageal reflux disease (GERD) with the aim of improving oesophageal mucosal defences by creating a film on the oesophageal mucosa and acting as a mechanical barrier against the noxious components of refluxate, both acidic and basic.
Methods: The film-forming and protective efficacy of medical device A based on HA and CS plus aluminium hydroxide, device B combining HA and CS with magnesium trisilicate and device C with only the combination of HA and CS was tested on a reconstructed human oesophageal epithelium (HO2E/S/5) as a biological model in 2 different pH environments, neutral and acidic, to mimic realistic conditions. Caffeine penetration kinetics and Lucifer yellow (LY) permeability modifications induced by these products were compared to those induced by a negative control series (saline solution, code NC) and positive control series (white Vaseline, code V) under neutral and acidic pH conditions.
Results: Under neutral and acidic pH conditions, compared to the negative control, all the products tested reduced (> 80% and 85– 90%, respectively) the caffeine passage, and no significant difference was observed among the products tested. Under neutral and acidic conditions, the LY permeabilities registered with device A and device C were not different from that registered with the negative control, while an LY flux% increase was calculated after 2 hrs of treatment (21.1%) with device B under acidic conditions.
Conclusion: These results confirm the ability of the products tested to interact with the oesophageal epithelium in order to adhere and create a stable protective film for at least 2 hours after their homogeneous distribution on the epithelium surface. Further clinical studies are needed to test these devices in the topical treatment of gastroesophageal reflux symptoms.
Keywords: hyaluronic acid, chondroitin sulphate, gastroesophageal reflux disease, antacid, caffeine, Lucifer yellow
Introduction
In recent years, the development of drugs capable of acting on pathophysiological mechanisms other than acid has been evaluated for the treatment of gastroesophageal reflux disease (GERD), non-erosive reflux disease (NERD) and proton pump inhibitor (PPI)-non-responder patients. Great attention has been paid to the use of those agents that aim to potentiate the defensive properties of oesophageal mucosa with or without the association of antacid components.
The resistance of oesophageal mucosa is due to multiple factors, which can be grouped into three categories: 1) pre-epithelial (salivary secretion, secretion of muco-bicarbonates); 2) epithelial (stratified cells of squamous epithelium that reduce the retro-diffusion of hydrogen ions and favour their neutralization); and 3) post-epithelial (mainly the mucosal blood supply responsible for the (mechanisms of) cellular repair).
In the last few years, new medical devices that contain hyaluronic acid (HA) and chondroitin sulphate (CS) with or without antacid components have been developed to ameliorate oesophageal mucosal defences by creating a film on the oesophageal mucosa and acting as a mechanical barrier against the noxious components of refluxate, both acidic and basic.
HA and CS are two important components of many extracellular matrices and are involved in several important physiological processes, such as wound repair and regeneration, cell proliferation, tissue morphogenesis and matrix organization. HA is a high-molecular-weight glycosaminoglycan and a component of the majority of extracellular matrices that play a key role in tissue healing. In this process, HA is crucial for a range of different activities, including the activation and moderation of the inflammatory response; the promotion of cell proliferation, migration and angiogenesis; the promotion of re-epithelization via the proliferation of basal keratinocytes; and the reduction in collagen deposition that leads to scarring.1 Clinical studies have shown that topical application of HA helps the healing process of venous leg ulcers,2 reduces the incidence of high-grade radio-epithelitis in patients who have undergone radiotherapy for head and neck, breast or pelvic carcinomas,3 and brings fast symptom relief in recurrent aphthous ulcerations of the oral mucosa.4
CS is a natural glycosaminoglycan that is present in the extracellular matrix of skin, cartilage, ligaments and tendons. In the literature, there are data available regarding the anti–inflammatory, tissue morphogenesis, cell proliferation and wound repair properties of CS.5 These effects are related to the capacity of CS to interact with a wide variety of molecules, including matrix molecules, growth factors, protease inhibitors, cytokines, chemokines, and adhesion molecules.6 As both in vitro and in vivo experimental studies have shown that CS specific binding to pepsin reduces peptic activity,7,8 treatments of peptic ulcer with CS have been attempted in the past.9,10 The negative effect of pepsin on oesophageal mucosa may also be neutralized by CS.
The aim of this study was to test the film-forming properties and protective properties of different medical devices, solid tablets containing HA and CS, on a 3D reconstructed human oesophageal epithelium (HO2E/S/5) as a biological model under neutral (pH=7) and acidic (pH=3.3) pH conditions.
In vitro reconstructed human epithelial models are similar in terms of morphology (multi-stratified or epithelium) and biochemical and physiological properties to in vivo human tissues, and currently, they represent the most promising alternative to animal ex vivo explants and submerged cell monolayers as biological models to be adopted in preclinical research.11
The availability of organ-specific biological barrier models is an advantage in preclinical testing: the status, functionality and reproducibility of these barriers are key parameters for assessing the biological effects of medical devices on the part of the body where they are intended to exert their action and allow discrimination between different formulations. Furthermore, the use of reconstructed human 3D tissues presents a series of advantages over traditional tests performed on cell monolayers or in vivo:
- overcome the limited availability of ex vivo explants (ex vivo mucosae are not even available) and ethical concerns regarding ex vivo explants of human and animal origin: the 3D models are commercially available, are produced under standardized conditions and are quality controlled;
- provide a standardized, robust and reproducible model of epithelia and mucosae of human origin with well-characterized and quantifiable barrier properties (eg, cell viability, barrier permeability, biomarkers);
- provide data that are more predictive of human responses through the use of experimental protocols using tissue models, which can reduce toxicological risks. An essential advantage attributable to in vitro 3D human models is the possibility of evaluating products directly on an organized tissue with different cell layers at the same doses used in vivo after acute and repeated exposures.
Last but not least, these models are sustainable with respect to the European Directive n. 2010/63, which promotes the development and validation of alternative methods under the Principle of Replacement, Reduction, and Refinement (3Rs) of the use of animals in research and foresees the replacement of animal testing for scientific and educational purposes once alternatives are scientifically available. This Directive has had a transversal impact on many European legislations dealing with the safety and market entry of chemicals and consumer products (eg, cosmetics, medicines, biocides, etc.) and more recently has been explicitly endorsed by the European Medical Device Regulation n. 2017/745 (MDR).
We mean “film-forming” as protective properties, therefore a modification of epithelial permeability where the product acts as a physical barrier to a probe transport across the tissue, resulting in a protective physical barrier (“film”) on the epithelium. The film-forming and protective efficacy of a medical device based on HA and CS plus aluminium hydroxide (univocal code A, HA:AH:CS are in the ratio 1:20:40), a device combining HA and CS with magnesium trisilicate (univocal code B HA:MT:CS are in the ratio 1:20:40) and a device with only the combination of HA and CS (univocal code C HA:CS are in the ratio 1:40) was tested on a reconstructed human oesophageal epithelium (HO2E/S/5) as a biological model at different pH (neutral and acidic conditions), thereby mirroring different degrees of tissue damage and epithelial permeability.
To mimic realistic exposure conditions and the products’ interaction with physiological fluids (i e saliva), an optimized procedure was adopted: according to the product’s technical forms (powder), the products were dosed as powder obtained from the solid tablets in a previously wetted epithelium (saline solution) in an amount adapted to cover the whole epithelium surface with a homogeneous distribution for 2 hours at room temperature. Caffeine penetration kinetics and Lucifer yellow (LY) permeability modifications induced by these products were compared to those induced by a negative control series (saline solution, code NC) and positive control series (white Vaseline, code V) under neutral and acidic pH conditions. Figure 1 shows the in vitro study protocol.
 |
Figure 1 Scheme of the in vitro experimental design. |
Materials and Methods
Tissue Model
The human oesophageal epithelium (HO2E/S/5) is an epithelium formed after 5 days of airlift culture of the K510 cell line (the final product Oesophageal Epithelium was purchased from Episkin) on inert polycarbonate filters in a chemically defined medium that reproduces the human oesophageal epithelium morphology. The reconstructed human oesophageal epithelium used for this study had a size of 0.5 cm2 and a thickness of at least 80 µm. The morphological structure and its similarity with the human oesophageal tissue are described in Figure 2.
 |
Figure 2 Morphological structure of human 3D reconstructed oesophageal epithelium (A) and its similarity with the biopsy of human full-thickness oesophageal mucosa (B). |
The batch was tested for the absence of hepatitis B, hepatitis C and mycoplasma, and the maintenance medium was tested for sterility.
The inserts containing the tissues at day 5 were placed at room temperature in a multi-well plate filled with an agarose nutrient solution in which they were embedded.
The HO2E/S/5 was then removed from the agarose nutrient solution under a sterile airflow cabin. The inserts were rapidly transferred to 4-well plates previously filled with maintenance medium (1 mL/well) at room temperature and incubated at 37°C, 5% CO2 and saturated humidity.
The day after, the medium was changed, and after the wetting-moisturizing procedure necessary to better recapitulate the realistic interaction of the medical device dispersed in the oesophageal environment, 30 μL of controls (saline solution NaCl 90%, Vaseline) and 30 mg of the test items (GERDOFF, B, C) were directly and uniformly applied topically on the 3D model epithelium to mimic realistic exposure conditions and the interaction with physiological fluids (i e, saliva).
Test Items
All the test items are solid compounds formulated in melt-in-mouth tablets (Table 1).
 |
Table 1 Test Item Characterization |
After 15 minutes of treatment, 100 μL of 0.5% caffeine solution in bi-distilled water (acid or standard) was applied for 2 hours on pre-wetted epithelium without washing out the product. To evaluate the kinetics of caffeine permeability, receptor fluid in the basolateral compartment (1 mL of saline solution) was collected after 15 mins, 1 hour and 2 hours, and the caffeine content was quantified by the UPLC method. After 2 hours of caffeine application and after receptor fluid collection, the pH of the apical compartment was measured (with litmus precision paper range 4.9–9.5), and then the Lucifer yellow assay was performed immediately.
Caffeine Permeability Evaluation
For studies of percutaneous absorption, the OECD guideline 428 recommends the use of caffeine (MW = 194.2, logP o/w = - 0.08) as the reference compound at low lipophilicity. This molecule has been used in several percutaneous absorption studies to evaluate permeability using different models of epidermis reconstructed in vitro.
Due to the ability to overcome the epithelial barrier, even in the absence of damage, caffeine was used as a probe to assess the propensity of a given product to form a protective film: the reduction in the passage of caffeine through the biological model is used as an index of film-forming efficacy. Given its film-forming and occlusive properties, Vaseline was used as a positive control.
Caffeine Penetration Protocol
The culture inserts were placed in 6-well plates previously filled with 1 mL/well of saline solution (basolateral compartment, receptor fluid). Controls and test items were evaluated in triplicate. Thirty milligrams of test items and 30 μL of saline solution (negative control) and white Vaseline (positive control) were applied on the apical surface of pre-wetted HO2E/S/5 tissues for 15 minutes; this time was defined after a preliminary assay that confirmed a homogeneous distribution on the epithelial surface. Then, 0.1 mL (100 μL) of caffeine solution (0.5% w/v (1 mg caffeine/cm2)) under neutral (pH 7) or acidic (pH 3.3) conditions was applied to the treated epithelial surface.
Throughout the experiment, the inserts were placed in a CO2 incubator at a defined temperature. After 15 minutes, 1 and 2 hours, 1 mL of the receptor fluid was withdrawn from the basolateral compartment with a micropipette (Gilson) and replaced with fresh receptor fluid kept at room temperature. The withdrawn samples were stored at 4°C before UPLC/MS analysis. Figure 3 shows the caffeine penetration protocol.
 |
Figure 3 Caffeine penetration protocol. |
At the end of the experiment, the pH of the solution in the apical compartment was measured (with litmus precision paper range 4.9–9.5), and then the Lucifer yellow assay was performed immediately.
Analytical Method for Caffeine
The caffeine concentration was determined by using a 1290 infinity II LC System (AGILENT Santa Clara California) equipped with a C18 reversed-phase column (ACQUITY UPLC BEH-C18, 1.7 μm, 100 x 2.1 mm, WATERS CORPORATION, Massachusetts) set at 25°C. A 5 μL sample was injected for isocratic elution at 0.25 mL/min. The composition of the eluent was 80% water/20% methanol. The wavelength was set at 273 nm. Standard calibration curves for caffeine (0.1 and 1000 mg/L) were used.
Lucifer Yellow Assay
Lucifer yellow (LY) is a fluorescent dye impermeable to the cell membrane and is used to study the paracellular permeability of a substance. When the junctions are unbroken, LY has a very low permeability; if the joints are damaged, LY flow will be much higher. Therefore, this assay is used to verify the integrity of cell junctions in the presence of the substance that needs to be evaluated.
Lucifer Yellow Protocol
The LY flux was evaluated after the caffeine permeability assay and the removal of test items from the surface of the tissues. First, 0.5 mL of LY (500 μM in saline solution) was applied to the epithelial surface, and 1 mL of saline solution was added to the basolateral compartment. After 1 hr at 37°C, the relative passage of LY from the apical to the basolateral compartment was quantified.
The measurement of fluorescence (RFU) was performed in a spectrofluorimeter (TECAN INFINITE M200) with 428 nm excitation and 535 nm emission. For each tissue, the measurement was performed at the basolateral level, and flux was calculated with the following formula:

where BL=basolateral and AP t=0: mean of the RFU of LY 500 μM solution.
Results
Caffeine Quantification Under Neutral pH Conditions
The results of caffeine passage under neutral conditions (pH 7) are reported in Tables 2–4. Table 2 reports micrograms of caffeine quantified in the receptor fluids under neutral conditions expressed as the mean of biological triplicate assays ± standard deviation and coefficient of variation (CV%).
 |
Table 2 Micrograms of Caffeine Quantified in the Receptor Fluid at 15 mins, 1 hr and 2 hrs Under Neutral Conditions |
 |
Table 3 Rate of Caffeine Quantified in the Receptor Fluid at 15 mins, 1 hr and 2 hrs Under Neutral Conditions |
 |
Table 4 Rate of Caffeine Considering the Caffeine Quantified After 2 hrs When the Negative Control Was Applied Under Neutral Conditions as 100% |
The total amount quantified in the negative control (366.44 μg ± 9.66 μg) was considered as a reference for caffeine kinetics on HO2E/S/5 under the adopted neutral experimental conditions. As expected, Vaseline completely inhibited caffeine passage (0.00 ± 0.00). These results allow us to validate the experiment.
In Table 3, the results under neutral conditions are expressed as the percentage of caffeine considering the dose applied (0.5 mg) as 100%.
In Table 4 and Figure 4, the results are expressed as the percentage of caffeine considering the dose quantified when the negative control was applied (366.44 μg) as 100%.
 |
Figure 4 Rate of caffeine considering the caffeine quantified after 2 hrs when the negative control (NC) was applied under neutral condition as 100%. |
Compared to the negative control, all the products tested reduced the caffeine passage by >80%. At each time point, no significant difference was observed among the products tested.
Caffeine Quantification in Acidic pH Conditions
The results of the caffeine passage under acidic conditions (pH 3.3) are reported in Tables 5–8.
 |
Table 5 Micrograms of Caffeine Quantified in the Receptor Fluid at 15 mins, 1 hr and 2 hrs Under Acidic Conditions |
 |
Table 6 Rate of Caffeine Quantified in the Receptor Fluid at 15 mins, 1 hr and 2 hrs Under Acidic Conditions |
 |
Table 7 Rate of Caffeine Considering the Caffeine Quantified After 2 hrs When the Negative Control Was Applied Under Acid Conditions as 100% |
 |
Table 8 pH Measurements |
Table 5 reports the micrograms of caffeine quantified in the receptor fluid under acidic conditions expressed as the mean ± standard deviation and coefficient of variation (CV%). The total amount quantified in the negative control (365.33 μg ± 2.93 μg) was considered the reference of caffeine kinetics on HO2E/S/5 under the adopted acid experimental conditions. It is important to emphasize that despite the treatment with an acidic caffeine solution, no significant difference from negative control tissues exposed to neutral conditions (366.44 μg ± 9.66 μg) was observed. As expected, Vaseline completely inhibited the caffeine passage (0.00 ± 0.00), and these results allow us to validate the experiment.
In Table 6, the results under acidic conditions are expressed as the percentage of caffeine considering the dose applied (0.49 mg) as 100%.
In Table 7 and Figure 5, the results are expressed as the percentage of caffeine considering the dose quantified when the negative control was applied (365.33 μg) as 100%. Compared to the negative control, all the products tested reduced the caffeine passage significantly (85–90% reduction). At each time point, no significant difference was observed among the products tested.
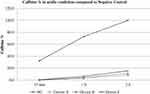 |
Figure 5 Rate of caffeine considering the caffeine quantified after 2 hrs in the negative control as 100% under acidic conditions. |
Lucifer Yellow
LY paracellular flux was assessed at the end of the exposure time (2 hrs). The measured fluorescence results are reported in Figure 6 (pH 7 condition) and Figure 7 (pH 3.3 condition).
 |
Figure 6 Lucifer yellow flux after 2 hrs of treatment followed by product washing under neutral conditions. |
 |
Figure 7 Luciferase yellow flux after 2 hrs of treatment followed by product washing under acidic conditions. |
Figure 6 shows the LY flux % with respect to the amount of LY in the apical compartment at time 0. The negative control (NC) had an LY permeability of 5.6% after 2 hrs of treatment.
The LY permeabilities registered after 2 hours with device A and device C were not different from that registered with the negative control. These results indicate, for the products tested, an absence of direct damage at the tight junction level and the maintenance of barrier functionality after exposure.
In contrast, an LY flux% increase was observed (12.9%) with device B.
Figure 7 shows the LY flux % with respect to the amount of LY in the apical compartment at time 0 under acidic conditions.
Confirming the results observed under neutral conditions, the LY permeabilities registered after 2 hours with device A and device C were not different from that registered with the negative control, while a LY flux % increase (21.1%) was calculated with device B.
pH Measurement
After 2 hours of caffeine application and after receptor fluid collection, the pH of the apical compartment was measured (with litmus precision paper range 4.9–9.5). Table 8 reports the results.
Compared to the negative control, all the tested products induced a pH increase under both conditions. In particular, with device B, a basic value of 8.8 was reached.
This observation directly correlates and explains the observed LY flux increase.
Discussion
The human esophageal epithelium permeability and properties of device A, device B and device C were tested on a reconstructed human oesophageal epithelium (HO2E/S/5) as a biological model under different pH conditions: neutral (pH 7.0) and acidic (pH 3.3).
The adopted experimental conditions mirror realistic exposure in the oesophageal cavity environment: the presence of a significant liquid volume in contact and surrounding the epithelium. To mimic neutral (healthy) and acidic (disease) conditions, two different pH conditions were investigated.
Caffeine penetration kinetics and LY permeability modifications induced in the product-treated series were compared to those induced in the negative control series (saline solution) and the positive control series (white Vaseline) under both the pH conditions tested.
Compared to the negative control, all the products tested significantly reduced the caffeine passage, and at each time point, no significant difference was observed among the different products tested.
These results confirm the ability of these products to interact with the oesophageal epithelium and to adhere and create a stable protective film for at least 2 hours after their homogeneous distribution on the epithelium surface in the presence of a relatively high amount of liquid, represented by the caffeine solutions applied to the apical surface (100 μL).
The oesophageal mucosa is protected against injurious agents by its stratified, multi-layered squamous epithelium, which represents a true mucosal barrier. All the damaging substances, such as the hydrochloric acid and pepsin contained in the gastric refluxate, may impair this barrier and as a consequence may increase the mucosal permeability.
The caffeine permeation assay showed that no modifications of the physiological permeability of the epithelium were induced by the tested products. This result confirms that the human esophageal epithelium permeability and protective properties under the adopted experimental conditions were exclusively related to physiological interaction and protective activity of the epithelium, which maintained its functional role. The results of the LY assay show that after exposure to the negative control, Vaseline, and devices A and C, there was no alteration in the paracellular permeability of the 3D model. In fact, devices A and C and Vaseline create a protective barrier that is positioned above the epithelium without modifying its structure and permeability. The application of device B, which contains magnesium trisilicate, an anti-acidic product, in addition to HA and CS leads to an increase in the permeability of the 3D epithelium under both neutral and acidic pH conditions. These results suggest that this product had an impact at the tight junction level and on epidermal barrier functionality.
To our knowledge, this work is the first study in the literature on the use of 3D human tissue models applied to oesophageal mucosa and on the efficacy and mechanism of action of products CS and HA at different pH (neutral and acidic conditions) mirroring different degrees of tissue damage and permeability.
To date, few studies in the literature have shown the effects of products containing CS and HA on the relief of GERD symptoms. Two small prospective placebo-controlled studies have shown that short-term treatment achieved significant and rapid symptom relief in patients with both erosive reflux disease12 and NERD.13 More recently, a prospective double-blind placebo-controlled trial conducted in several Italian centres showed that the combination of a PPI + HA-CS in syrup was able to relieve symptoms and improve the quality of life more than a PPI alone.14
A recent open-label uncontrolled study showed that administration of orodispersible tablets containing CS, aluminium hydroxide and HA improves non-erosive GERD clinical typical and atypical symptoms and gastric juice-related biochemical parameters (eg, neutrophil, lymphocyte, eosinophil, parietal cells, red blood cells and exudate protein counts).15
Recently, 3D tissue models have been adopted in the field of medical devices for the evaluation of potential irritation and sensitization by medical device extracts on the skin.16–18 This work is the first study in which a 3D oesophageal tissue model, formed from a human cell line culture, is used for testing medical device mechanisms of action. This experimental model brings a great advantage because of the possibility of evaluating the effectiveness of different products on an organized tissue with different cell layers at the same doses used in vivo under different conditions.
In conclusion, all solid formulations tested showed good film-forming properties on a reconstructed human oesophageal epithelium independent of the presence of an antacid in the formulation, mirroring different degrees of epithelial permeability (neutral or acidic pH), and they showed a positive effect on enhancing the barrier integrity under both conditions tested.
Disclosure
CL and MM are full employees of Vitroscreen. The authors report no other conflicts of interest in this work.
References
1. Chen J, Abatangelo G. Functions of hyaluronan in wound repair. Wound Repair Regen. 1999;7:79–89. doi:10.1046/j.1524-475X.1999.00079.x
2. Ortonne JP. A controlled study of the activity of hyaluronic acid in the treatment of venous leg ulcers. J Dermatolog Treat. 1996;7:75–81. doi:10.3109/09546639609089533
3. Liguori V, Guillemin C, Pesce GF, Mirimanof RO, Bernier J. Double‐blind, randomized clinical study comparing hyaluronic acid cream to placebo in patients treated with radiotherapy. Radiother Oncol. 1997;42:155–161. doi:10.1016/S0167-8140(96)01882-8
4. Nolan A, Baillie C, Badminton J, Rudralingham M, Seymour RA. The efficacy of topical hyaluronic acid in the management of recurrent aphthous ulceration. J Oral Pathol Med. 2006;35(8):461–465. doi:10.1111/jop.2006.35.issue-8
5. Yamada S, Sugahara K. Potential therapeutic application of chondroitin sulphate/dermatan sulphate. Curr Drug Discov Technol. 2008;5(4):289–301. doi:10.2174/157016308786733564
6. Volpi N. Anti-inflammatory activity of chondroitin sulphate: new functions from an old natural macromolecule. Inflammopharmacology. 2011;19(6):299–306. doi:10.1007/s10787-011-0098-0
7. Bonfils S, Dubrasquet M, Lambling A. The inhibition of peptic proteolysis by various polysaccharides. Rev Fr Etud Clin Biol. 1960;5:71–74.
8. Galzigna L, Previerocoletti MA. Action of sodium chondroitin sulphate on the enzymatic activity of pepsin. Gazz Med Ital. 1965;124:65.
9. Lenzi G, Rapino P, Ferri S. On the behavior of gastric hydrochloric and peptic activity after administration of sodium chondroitin sulphate. Minerva Med. 1963;54:3421–3424.
10. Baldini E, Tincani GP. Treatment of gastroduodenal ulcer with sodium chondroitin sulphate. Minerva Gastroenterol. 1963;9:25–29.
11. Griesinger C, Desprez B, Coecke S, Casey W Zuang V. Validation of alternative in vitro methods to animal testing: concepts, challenges, processes and tools. Adv Exp Med Biol. 2016;856:65–132.
12. Palmieri B, Corbascio D, Capone S, Lodi D. Preliminary clinical experience with a new natural compound in the treatment of esophagitis and gastritis: symptomatic effect. Trends Med. 2009;9:219–225.
13. Palmieri B, Merighi A, Corbascio D, Rottigni V, Fistetto G, Esposito A. Fixed combination of hyaluronic acid and chondroitin-sulphate oral formulation in a randomized double blind, placebo-controlled study for the treatment of symptoms in patients with non-erosive gastroesophageal reflux. Eur Rev Med Pharmacol Sci. 2013;17:3272–3278.
14. Savarino V, Pace F, Scarpignato C; Esoxx Study Group. Randomised clinical trial: mucosal protection combined with acid suppression in the treatment of non-erosive reflux disease – efficacy of Esoxx, a hyaluronic acid-chondroitin sulphate based bioadhesive formulation. Aliment Pharmacol Ther. 2017;45:631–642. doi:10.1111/apt.13914
15. Iannitti T, Laurino C, Morales JC, et al. A chondroitin sulphate and hyaluronic acid-based dietary formulation improves non-erosive gastroesophageal reflux disease-related symptoms and gastric juice-related biochemical parameters: an open-label uncontrolled study. Adv Health Dis. 2017;1:43–61.
16. Casas JW, Lewerenz GM, Rankin EA, et al. In vitro human skin irritation test for evaluation of medical device extracts. Toxicol In Vitro. 2013;27:2175–2183. doi:10.1016/j.tiv.2013.08.006
17. Kandarova H, Willoughby JA, De Jong WH, et al. Pre-validation of an in vitro skin irritation test for medical devices using the reconstructed human tissue model EpiDerm™. Toxicol In Vitro. 2018;50:407–417. doi:10.1016/j.tiv.2018.02.007
18. De Jong WH, Hoffmann S, Lee M, et al. Round robin study to evaluate the reconstructed human epidermis (RhE) model as an in vitro skin irritation test for detection of irritant activity in medical device extracts. Toxicol In Vitro. 2018;50:439–449. doi:10.1016/j.tiv.2018.01.001
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
