Back to Journals » Nutrition and Dietary Supplements » Volume 16
Factors Associated with Time to Cease Exclusive Breastfeeding Among Infants Aged 6–9 Months, Kirkos Sub-City, Addis Ababa, Ethiopia: Survival Analysis
Authors Mezgebu GS, Getachew L, Feleke FW , Kidane R
Received 19 December 2023
Accepted for publication 17 April 2024
Published 23 April 2024 Volume 2024:16 Pages 37—49
DOI https://doi.org/10.2147/NDS.S444939
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Getachew Sale Mezgebu,1 Luladey Getachew,2 Fentaw Wassie Feleke,1,3 Rediet Kidane2
1Department of Human Nutrition, School of Nutrition, Food Science and Technology, Academic Center of Excellence in Human Nutrition, College of Agriculture, Hawassa University, Hawassa, Ethiopia; 2Department of Nutrition and Dietetics, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia; 3Department of Public Health, School of Public Health, College of Medicine and Health Sciences, Woldia University, Woldia, Ethiopia
Correspondence: Fentaw Wassie Feleke, Tel +251917008650, Fax +251335400643, Email [email protected]
Introduction: Notwithstanding the World Health Organization’s (WHO) guideline for exclusive breastfeeding (EBF) for the first six months of an infant’s life, its prevalence remains low in both developed and developing countries. Although breastfeeding is widely practiced in Ethiopia, only 59% of the children under the age of six months were exclusively breastfed.
Objective: This study aimed to assess the time to cessation of EBF and associated factors among infants aged 6– 9 months in health facilities under Kirkos sub-city, Addis Ababa, Ethiopia.
Methods: An institutional-based cross-sectional study was conducted among 287 mothers attending Kirkos sub-city health facilities from September 1 to 30, 2020. Bivariable and multivariable Cox regression models were fitted to identify factors associated with the time to cessation of EBF.
Results: According to this finding, the median period for EBF discontinuation was 6 months. Early cessation of EBF was 130 (45.8%) days. Mothers with average household monthly income < 15 USD [AHR, 5.31 (95% CI: 2.82, 9.99)] and 15– 30 USD [AHR, 2.59 (95% CI: 1.41, 4.77)], EBF counseling at post-natal care [AHR, 0.18 (95% CI: 0.10, 0.31)], media access [AHR, 1.67 (95% CI: 1.06, 2.63)], child comorbidity [AHR, 0.51 (95% CI: 0.29, 0.88)], bottle feeding [AHR, 3.28 (95% CI: 2.14 5.01)], unfavorable attitude towards EBF [AHR, 3.59 (95% CI: 2.02, 6.40)] were significant factors associated with the hazard of cessation of EBF.
Conclusion: In this investigation, the cumulative survival probability of EBF to 6 months was 45.8%, with a median duration of 6 months (95% CI 5.83– 6.18) months. Unfavorable attitudes, child comorbidity, and bottle feeding were factors associated with earlier cessation of EBF. Media access, household monthly higher income, and EBF counseling at postnatal care were factors associated with prolonged EBF. As a result, supporting behavioral change and media access for effective communication on EBF duration practice following the established standard should be targeted during both ante-natal and post-natal care visits.
Keywords: Addis Ababa, hazard ratio, postnatal care, survival analysis, time to cessation of EBF
Introduction
Breast milk is a natural diet that contains essential nutrients that are easily digestible and sufficient to feed infants with the required nutrients for producing energy and growth throughout the first six months of life.1 Breast milk is the finest source of nutrients for infants, according to scientific evidence. Breast milk includes not just the nutrients needed for a child’s growth and development, but also bioactive substances that help to boost the immune system.2 EBF is a cost-effective intervention for saving children’s lives in which the infant receives only breast milk from his or her mother or a wet nurse or expressed milk until six months and no other liquids/solids except for drops or syrups containing vitamins, mineral supplements, or medicine.3 EBF is adequate in quality and quantity in terms of the nutrients required by the baby.4 EBF can eliminate contamination, which is especially significant in communities with limited resources.5 As a result, breastfeeding in general, and EBF in particular, is one of the most successful interventions in the first 1000 days of life.6,7
Only around one-third of infants are exclusively breastfed for the first six months of life, according to the WHO.8 According to findings from 64 nations encompassing 69% of the births in poor countries, there have been gains in the percentage of exclusive breastfeeding since 1996, with the rate of EBF for the first six months of life increasing from 33% to 37%. Significant gains were recorded in Sub-Saharan African countries, where magnitudes grew from 22% to 30%, and in Europe, where magnitudes increased from 10% to 19%.9
In Ethiopia, breastfeeding has been nearly universal; about 97% of the children are ever breastfed. However, 59% of the infants receive exclusive breast milk with a median duration of 6 months.10 This rate is lower than the health sector transformation plan of Ethiopia.11 A result from Semera logia, Afar region demonstrated that the cumulative proportion of survival probability of EBF to 6 months was 64.5%, with a median duration of 6 months.12
Lack of EBF results in infant and childhood morbidity and mortality, including lifelong effects on productivity, school performance, intellectual development,13 and overall health during adolescence and adulthood lifetime.14,15 Research documented factors related to EBF cessation included younger maternal age,16 lower maternal educational level,16 unplanned pregnancy,17 maternal work outside the home,17 and lack of emotional support, especially from the baby’s father,18 mothers who underwent cesarean section,19 insufficient breast milk secretion, and maternal sickness.
The federal democratic republic of Ethiopia, Ministry of Health has emphasized exclusive breastfeeding practice and has declared “the annual exclusive breastfeeding day”.20 The health extension program aims at improving proper infant and young child nutrition, for instance, the promotion of EBF in Ethiopia.21 Moreover, non-governmental organizations are working towards the improvement of optimal breastfeeding in the country.22
In the Global Targets, the WHO and UNICEF have set a goal that in 2025 at least 50% of the infants will be breastfed exclusively for the first 6 months.23 However, the time to EBF cessation was questioned, and little research looked into factors associated with EBF cessation time. As a result, the objective of this study was to assess the time to cessation of EBF and its associated factors in Addis Ababa Kirkos sub-city health facilities in Ethiopia among women with children aged 6–9 months.
Methods and Materials
Study Area
The study was carried out at Addis Ababa Kirkos sub-city health facilities, in Addis Ababa, Ethiopia. Ethiopia’s capital is Addis Ababa. The city’s estimated population is 4.6 million people. Kirkos is one of Addis Ababa’s 11 sub-cities. According to the sub-city health office data report, the sub-city has a total population of 297,485, an under-five population of 21,285, and an infant population of 6654. According to the sub-city 2019 report, there are two government hospitals, eight health centers, and 23 middle-level clinics.
Study Design and Period
A facility-based cross-sectional study was conducted from September 1 to 30, 2020.
Source and Study Population
All mothers with infants aged 6–9 months who attended pediatrics and child clinics at Kirkos sub-city health facilities were included in the source population. Meanwhile, women with infants aged 6–9 months who attended pediatrics and child clinics at selected Kirkos Sub-city health facilities were chosen as the study population, with those who provided the actual response serving as the study unit. However, the study excluded mothers with mental problems or who were unable to speak, as well as infants living with non-biological mothers.
Sample Size Determination
The sample size was calculated using Open Epi Version 7.01 having the following assumptions: 29.2% and 51.1% the cumulative proportion of survival probability of exclusive breastfeeding to 6 months among mothers getting infant feeding counseling during ANC checkups and not getting infant feeding counseling during ANC checkup, respectively, on a study done in Samara-Logia, Northeastern Ethiopia,12 95% Confidence level which is 1.96, power as 80%, and the ratio of sample size (Unexposed/Exposed) = 1: the sample size with design effect 1.5 was 261 and 10% none response rate. Finally, the sample size became 287 mothers having infants aged 6–9 months.
Sampling Technique and Procedure
A multistage sampling technique was used to recruit the study unit. First, from a total of 33 health facilities from each of the three kinds of facilities, 11 health facilities (1 government hospital, 3 health centers, and 6 private medium clinics) were chosen at random using a lottery procedure. Second, the study respondents were gathered from each chosen health institution using a systematic random sample procedure based on the health facility’s average monthly client size. By referring to the registration books of each health institution, the number of study participants enrolled from each selected facility was estimated proportionally based on their average client size visited per month.
Study Variables and Variable Measurements
Dependent Variable
The dependent variable in this study was the time to cessation of EBF in months. The time to cessation of EBF was assessed using birth recall information. It was assessed by asking the study participants “What was the age of your baby in months when you first tried liquids or semi-solids or solids other than your breast milk?” Then, mothers who exclusively breastfed their infants to less than 6 months were considered as an “event” and those who fed infants to 6 months and beyond were “censored”.
Independent Variables
Socio-demographic and economic characteristics, maternal, and infant health service utilization, infant feeding practices, media access, awareness of EBF practice, and attitude towards EBF practice were all investigated independent variables.
Operational Definitions
Ebf
A situation where the infant has received only breast milk from his/her mother or a wet nurse or expressed milk until six months and no other liquids/solids except for drops or syrups consisting of vitamins, mineral supplements, or medicine.3
Early Cessation of EBF
A time of children who had been ceasing EBF before 6 months of age.24,25
Knowledge on Time to Cessation of EBF
To estimate the knowledge of mothers on time to cessation of EBF, mothers were asked about the ideal duration of EBF and the time to wean off infants. Mothers who correctly identified the duration of EBF as six months were considered knowledgeable.26
Attitude Towards Time to Cessation of EBF Practice
To identify their attitudes towards time to cessation of EBF practice, five questions were presented to mothers. In this study, women who properly recognized the period of EBF as six months were considered to be informed. Five questions were posed to mothers to determine their attitudes regarding EBF practice. Mothers who want to EBF their next baby or who encourage their peers to do so are thought to have a positive attitude towards EBF. Mothers’ practices were assessed using their reports on breastfeeding initiation time, colostrum provision, and EBF duration for the index infant. Mothers who exclusively fed their newborn breast milk during the first six months of life were regarded as having an optimal practice.26
Data Collection Tools and Processes
Data collection was accomplished by a structured questionnaire prepared in Amharic for socio-demographic characteristic variables, maternal and infant health service utilization, and infant feeding practices developed from different pieces of literature including Ethiopian demographic and health survey findings12,26–30 validated in our country setting. First, training was given to data collectors regarding the study objectives, method of data collection tools for data collection and the procedures to be followed for data collection. Two health officers were also recruited to supervise four diploma nurse data collectors who were local fluent speakers.
Data Quality Assurance
Data collectors and supervisors received two days of training on data collection procedures. To ensure language consistency, the questionnaire was developed in English and translated into Amharic by proficient speakers of both languages and then back-translated into English by separate language specialists. Data was gathered using the Amharic version of the questionnaire. Before beginning data collection, the structured questionnaire was double-checked for printing mistakes. The names of the data collectors were recorded to increase accountability for any missing data. Daily, data collectors submitted the collected data to their supervisors, who examined the data for completeness. The questionnaire was assessed on 5% of the mothers having infants aged 6–9 months in Meshualekia health center, which was not part of the study.
Data Processing Management and Analysis
The obtained data were input using Epi data entry program version 4.6.0.6 then cleaned and analyzed using SPSS version 25. Frequency tables, graphs, and other summary statistics were used to depict the socio-demographic and other factors of patients’ mothers. The life table was created to evaluate the chances of EBF ceasing over time. The Kaplan–Meier survival curve with a Log rank test was used to compare the survival of infants on EBF. The proportionality hazard assumption test was used to assess model fitness using a log(-log) vs log(time) graph.
To examine the relationship between dependent and independent variables, a bivariable Cox regression analysis model was performed. All variables in the bivariable Cox regression analysis model that demonstrated a significant correlation with p-value < 0.25 were candidates for the multivariable Cox regression analysis model. A multivariable Cox regression analysis model was used to find factors influencing the cessation time, with P-values less than 0.05 considered statistically significant. AHR at 95% CI was used to determine the degrees of connection between dependent and independent variables.
Ethical Clearance
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by both Institutional Review Board (IRB) of Jimma University and Addis Ababa health research and emergency management directorate with a reference number of IRB/000703/2012 and A/A/H/1621/227. A written authorization letter was also received from the Kirkos sub-city health office, and support letters were then submitted to all health facilities. Participants in this study were informed about the study’s aims, expected outcomes, benefits, and hazards. Finally, before the interview, participants provided verbal and written informed consent, which was formally recorded. Furthermore, the confidentiality of participant information was ensured, and information was recorded anonymously.
Result
Maternal Socio-Demographic Characteristics
A total of 284 (99.0% response rate) participants were interviewed in the study period. The mean ±SD age of the infants was 7.65 ±1.03 months and 179 (63.0%) were females. The majority 230 (81.0%) of the mothers were 25–34 years old, and more than three-quarters were married. More than one-third 109 (38.4%) mothers had a college degree educational status. Concerning household heads 218 (76.8%) were husbands and 41.5% were government employees. About 217 (76.4%) were family size ≤ 4 and one-third (35.2%) were with average household monthly income was 15–30 USD (Table 1).
 |
Table 1 Socio-demographic Characteristics of Study Participants, Kirkos Sub-City Health Facilities, Addis Ababa, Ethiopia, 2020 |
Obstetrics and Health Service Utilization
Concerning obstetrics and maternal service utilization, the majority of the mothers had been pregnant for ≤2 times 187 (65.8%), attended <4 ANC visits during pregnancy of the index child 158 (55.6%), and received counseling about breastfeeding during the ANC visits 232 (81.7%). More than half of mothers delivered the index child at a health center 152 (53.5%) and attended a PNC service 259 (91.2%). Also, about three-fourths of 218 (76.8%) had media access. Concerning comorbidity 74 (26.1%) had a history of mother and childhood illness (Table 2).
 |
Table 2 Obstetrics and Health Service Utilization Characteristics Among Infants 6–9 Months, Kirkos Sub-City Health Facilities Addis Ababa Ethiopia 2020 |
Maternal Knowledge and Attitude Towards the Duration of EBF
Almost all moms 282 (99.3%) have heard about the necessity of exclusive breastfeeding for the first six months postpartum, with 132 (46.5%) receiving the information from a HEW. Eighty-seven percent of the women were judged to have a good level of awareness about the required length of EBF and 256 (90.1%) were judged to have a favorable attitude towards EBF during the first six months postpartum (Table 3).
 |
Table 3 Maternal Knowledge and Attitude Towards Exclusive Breastfeeding, Kirkos Sub-City Health Facilities Addis Ababa Ethiopia 2020 |
Breastfeeding Practice
Regarding breastfeeding practice, about one-fifth of the mothers discarded colostrum and only 243 (85.6%) initiated breastfeeding within one hour after delivery. Eighty-five percent of the mothers were breastfeeding during the time of the interview and 177 (62.3%) ever used bottle feeding (Table 4).
 |
Table 4 Breastfeeding Practice of Mothers, Kirkos Sub-City Health Facilities Addis Ababa Ethiopia 2020 |
Time to Cease EBF
The cumulative survival probability of EBF to 6 months was 45.8%, with a median duration of 6 months (95% CI 5.83–6.18) months. In addition, the range of EBF duration was from 0 to 6 months (Table 5).
 |
Table 5 Life Table of EBF Duration for the First 6 Among Infants Aged 6–9 Months in Kirkos Sub-City, Addis Ababa Ethiopia 2020 |
Nearly five mothers’ common reasons for early cessation of EBF were inconvenience due to breastfeeding (19.4%) and lack of effective breastfeeding skills (14.8%) (Figure 1).
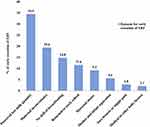 |
Figure 1 Reason for early cessation of EBF among infants aged 6–9 months, Kirkos Sub-city health facilities Addis Ababa Ethiopia 2020. |
Kaplan–Meier curve showed that women who had received infant feeding counseling at ANC and PNC check-ups significantly associated with the duration of EBF. The survival probability of EBF was significantly higher among women who had received infant feeding counseling at ANC check-ups as compared to those who had been deprived of counseling (Log rank test, p < 0.05) (Figure 2).
The survival curve of women who had gotten EBF practice counseling at PNC was constantly above the survival curve of the other group (Log rank test, p < 0.001) (Figure 3).
Factor Associated with Time to Cessation of Exclusive Breastfeeding
Based on the bivariable Cox regression analysis model results (P-values < 0.25), the variables selected for inclusion in the multiple regression model were maternal age, child sex, household head, average household monthly income, family size, ANC, EBF counseling at ANC, EBF counseling at PNC, media access, comorbidity, ever breastfeed, bottle feeding and attitude towards EBF (Table 6).
 |
Table 6 Bivariable and Multivariable Cox Regression Results for Factors Associated with Time to Cease EBF Among Infants Aged 6–9 Months, Kirkos Sub-City, Addis Ababa Ethiopia 2020 |
Finally, compared to mothers with an average monthly income of >45USD, the AHR to cease EBF was 5.31 (95% CI: 2.82, 9.99) times higher among mothers living with a household monthly income of <15 USD and 2.59 (95% CI: 1.41, 4.77) times higher among mothers with monthly income USD of 15–30. Compared to mothers who had not gotten infant feeding practice counseling at PNC, mothers who got counseling were 82% (AHR, 0.18 (95% CI: 0.10, 31)) lower to cease EBF early. Compared to mothers who did not have media access, mothers who had media access were 1.67 times (AHR, 1.67 (95% CI: 1.06, 2.63)) higher to cease EBF early (Table 6).
Compared to mothers who did not have a history of child and mother illness, mothers who had a history were 49% (AHR, 0.51 (95% CI: 0.29, 0.88)) less likely to cease EBF early. Compared to mothers who did not breastfeed previously, mothers who breastfed previously were 88% (AHR, 0.11 (95% CI: 0.06, 0.21)) times less likely to cease EBF (Table 6).
The risk of ceasing EBF among mothers who feed by bottle their infants was 3.28 times (AHR, 3.28 (95% CI: 2.14 5.01)) higher as compared to mothers who had not bottle-fed their infants. Compared to mothers who had favorable attitudes, mothers who had unfavorable attitudes towards the EBF practice were 3.59 times (AHR, 3.59 (95% CI: 2.02, 6.40)) higher to cease EBF (Table 6).
Discussion
According to this study, the cumulative survival probability of EBF to 6 months was 45.8%, with a median duration of 6 months (95% CI 5.83–6.18) months. Unfavorable attitudes, child comorbidity, and bottle feeding were factors associated with earlier cessation of EBF. Media access, household monthly higher income, and EBF counseling at postnatal care were factors associated with prolonged EBF.
The median time for cessation of EBF was similar to a study done in northeastern Ethiopia,12 southern Ethiopia,31 and northern Ethiopia.32 In this, the median time to cease EBF was higher than studies revealed from Indonesia,33 Australia,34 Kinshasa,35 Botswana,36 Colombia,37 and Saudi.38 The rate of early EBF discontinuation was 45.8%, which was higher than the studies revealed from southern Ethiopia 30.4%,39 northwest Ethiopia 21.5%,40 northeastern pastoralist parts of Ethiopia 35.5%,12 Addis Ababa 42.4%,41 mini Ethiopian demographic health survey 41%,10 Taiwan 40.1%,42 Kinshasa 2.8%,35 India 22.85%,43 Indonesia 21.3%,33 and Kenya 2%.44 This finding was lower than the study revealed from southern Ethiopia 48%,45 Dukem Central Ethiopia 75.7%,46 Nepal 50.5%,47 Tanzania 68.7%,48 Saudi 60%,49 and Australia 49%.34 This discrepancy may be explained by sample size, study area, study period, study design, study unit, and the mother’s workload in the city, as women in big cities were more likely to be employed or involved in other jobs that allow them to spend a lot of time outside the home.
Compared to mothers with an average household monthly income of more than 45 USD, mothers with an average household monthly income of <15 USD were 5.31 times higher and 15–30 USD were 2.59 times higher to cease EBF early. This was consistent with the study done in Gurage south Ethiopia.31 This flinging was supported in other low-income societies.50 This might be due to mothers from households with a better income status having a lesser obligation to start working outside during the first six months which allows them the opportunity to practice EBF.
Compared to mothers who had not gotten infant feeding practice counseling at PNC, mothers who got counseling were 82% lower to cease EBF early. The result was in line with a study done in Gurage Zone southern Ethiopia, and northeastern Ethiopia mothers who received counseling on infant feeding were less likely to discontinue EBF.12,31,32,39,40 This revealed that a PNC check-up is a good time to share important information about optimal newborn feeding practices. In addition to the EBF at the health facility level, the launch of an urban health extension program in Addis Ababa has significantly increased access to PNC services, including breastfeeding counseling, at the household level.
Mothers with infants aged 6–9 months who had media access were 1.67 times more likely to cease EBF compared to mothers who did not have media access. The result was inconsistent with studies done in West African countries.51 This might implicate media access solely may not be effective unless specific counseling intervention on EBF practice is provided in the other setting.
Mothers with infants aged 6–9 months who had a history of illness were 49% less likely to cease EBF when compared to mothers with infants who had not a history of illness. This might be because major illnesses and infections such as diarrhea and cough can affect a child’s digestive system which leads to poor appetite.52 These results indicated that the mothers tend to try another option like starting complementary feeding to their children as option early.
Compared to mothers who had not bottle-fed, mothers who fed by bottle were 3.28 times more likely to early cease EBF. This result is consistent with other studies in which child bottle feeding cannot promote the positive, long-term health effects breast milk does.53 This also explains as children started bottle feeding mothers felt that to stop EBF practice.
Mothers with infants aged 6–9 months who have unfavorable attitudes towards the EBF practice were 3.59 times higher to cease EBF when compared to their counterparts who had favorable attitudes. A supporting study found that favorable attitudes were associated with a higher prevalence of exclusive breastfeeding.54,55 This can be because mothers with no good knowledge (not knowledgeable) were more likely to discontinue EBF than their peers. This discovery was supported by research conducted in the Democratic Republic of the Congo, southern and northern parts of Ethiopia.35,40,45 This could be explained by the fact that mothers who were knowledgeable about the composition and benefits of breast milk would have a favorable attitude towards optimal EBF practice. This could be because of the mother’s attitude towards EBF.
Because the data were acquired using a recall-since-birth approach with the possibility of memory bias, the reported time for the discontinuation of EBF for certain infants may have been skewed. There may be a social desirability bias because women self-report the time to EBF cessation.
Conclusion
According to this study, the cumulative survival probability of EBF to 6 months was 45.8%, with a median duration of 6 months (95% CI 5.83–6.18) months. Unfavorable attitudes, child comorbidity, and bottle feeding were factors associated with earlier cessation of EBF. Media access, household monthly higher income, and EBF counseling at postnatal care were factors associated with prolonged EBF.
Throughout the postpartum period, it is imperative to enhance infant feeding counseling at the institutional level. In light of the study area circumstances, it is recommended that policymakers look into the matter to emphasize women’s empowerment and other corrective actions to promote EBF and help achieve the global targets set by UNICEF and the WHO. To assess the combined prevalence and determinants of EBF practice across Ethiopian settings, more systematic review and meta-analysis research is needed.
Abbreviations and acronyms
EBF, Exclusive Breast Feeding, ENA, Emergency Nutrition Assessment, EPI, Expanded Program for Immunization, FANTA, Food and Nutrition Technical Assistance, IYC, Infants and Young Children, IYCF, Infant and Young Child Feeding, UNICEF, United Nations Children Fund, WHO, World Health Organization.
Data Sharing Statement
The datasets used or analysed during the current study are available from the corresponding author upon reasonable request.
Acknowledgment
We thank Jimma University for giving us this opportunity. Our gratitude also goes to the Addis Ababa Kirkos sub-city health office, health facilities staff, and study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. WHO. Infant and young child feeding: model chapter for textbooks for medical students and allied health professionals. World Health Organization. 2009.
2. Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clinics. 2013;60(1):49–74. doi:10.1016/j.pcl.2012.10.002
3. WHO. 10 Facts on Child Health. Geneva; 2012.
4. WHO. Nutrient adequacy of exclusive breastfeeding for the term infant during the first six months of life. Geneva; Available at http://whqlibdoc.who.int/publications/9241562110.pdf. 2002.
5. Kathryn A, Dorothy J. Cultural barriers to exclusive breastfeeding by mothers in a rural area of Cameroon. Afr J Midwifery Wom Health. 2005;1:50::324–8.
6. Moore T, Arefadib N, Deery A, West S The first thousand days: an evidence paper. 2017: Parkville: Centre for Community Child Health, Murdoch Children’s Research Institute; Available at https://www.rch.org.au/uploadedFiles/Main/Content/ccchdev/CCCH-The-First-Thousand-Days-AnEvidence-Paper-September-2017.pdf.
7. Schwarzenberg S, Georgieff M, Daniels S. AAP COMMITTEE ON NUTRITION. advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. 2018;141(2):e20173716. doi:10.1542/peds.2017-3716
8. WHO. Global data Bank on infant and young child feeding. WHO nutrition for health and development, Available at: http://www.who.int/nutrition/databases/infantfeeding/en. 2018.
9. Ahluwalia I, Morrow B, Hsia J. Why do women stop breastfeeding? Findings from the pregnancy risk assessment and monitoring system. Pediatrics. 2005;116(6):1408–1412. doi:10.1542/peds.2005-0013
10. Ethiopian Public Health Institute. - EPHI, federal ministry of health - FMoH, Infant and young Child Feeding. Ethiopia mini demographic and health survey. 2019. Addis Ababa Infant and young Child feeding. Ethiopia. EPHI/FMoH/ICF.
11. FDREFMOH. The federal democratic republic of Ethiopia ministry of health. Health sector transformation plan: 2015/16–2019/20. 2015. Available at https://www.globalfinancingfacility.org/sites/gff_new/files/Ethiopia-health-systemtransformation-plan.pd.
12. Beyene AM, Liben ML, Arora A. Factors associated with the early termination of exclusive breastfeeding among mother-infant dyads in samaraLogia,Northeastern Ethiopia. BMC Pediatric. 2019;19(1):428. doi:10.1186/s12887-019-1803-1
13. Hall J. Effective community-based interventions to improve exclusive breast feeding at four to six months in low- and low–middle-income countries: a systematic review of randomized controlled trials. J Hall Midwifery. 2011;27:502.
14. IYCCFP. Infant and young child feeding practices: collecting and using data: a step-by-step guide, cooperative for assistance and relief everywhere Inc. (CARE). 2010. Available at http://nutritioncluster.net/wp-content/uploads/sites/4/2. 013/12/final-iycf-guide-iycf–practices_eng.pdf.
15. Ahmed R, Ejeta Chibsa S, Hussen MA, et al. Undernutrition among exclusive breastfeeding mothers and its associated factors in Southwest Ethiopia: a community-based study. Women’s Health. 2024;20:17455057241231478. doi:10.1177/17455057241231478
16. Whalen B, Cramton R. Overcoming barriers to breastfeeding continuation and exclusivity. Curr Opin Pediatr. 2010;22:655–63.
17. Hamade H, Chaaya M, Saliba M, Chaaban R, Osman H. Determinants of exclusive breastfeeding in an urban population of primiparas in Lebanon: a cross-sectional study. BMC Public Health. 2013;13(1):702. doi:10.1186/1471-2458-13-702
18. Mueffelmann R, Racine E, Warren-Findlow J, Coffman M. Perceived infant feeding preferences of significant family members and mothers’ intentions to exclusively breastfeed. J Hum Lact. 2015;31:479–89.
19. Suksham J, Manju S, Deepak C. Factors for cessations of exclusive breast feeding at end of 6 weeks in healthy term and late preterm neonates born in a hospital set up in north India. National Journal of Community Medicine. 2012, June 30 ;3(02): 274–8.
20. Chekol D, Biks G, Gelaw Y, Melsew Y. Exclusive breastfeeding and mothers’ employment status in Gondar town, Northwest Ethiopia: a comparative cross sectional study. Int Breastfeed J. 2017;12(1):27. doi:10.1186/s13006-017-0118-9
21. Fetene N, Linnander E, Fekadu B, et al. The Ethiopian health extension program and variation in health systems performance: what matters? PLoS One. 2016;11(5):e0156438. doi:10.1371/journal.pone.0156438
22. Kim S, Rawat R, Mwangi E, et al. Exposure to large-scale social and behavior change communication interventions is associated with improvements in infant and young child feeding practices in Ethiopia. PLoS One. 2016;1:10.
23. WHO. Global targets 2025. to improve maternal, infant and young child nutrition. Available at: http://www.who.int/nutrition/global-target-2025/en/. 2016.
24. WHO. WHO. Global Strategy for Infant and Young Child Feeding; 2010.
25. UNICEF, WHO. Global Strategy for Infant and Young Child Feeding,Geneva. Switzerland; 2006.
26. Asfaw MM, Argaw MD, Kefene ZK. Factors associated with exclusive breastfeeding practices in Debre Berhan District, Central Ethiopia: a cross sectional community based study. International breastfeeding journal. 2015,Dec 10:. ():1–9.
27. Chang P-C, Sin-Fong L, Yang H-Y, et al. Factors associated with cessation of exclusive breastfeeding at 1 and 2 months postpartum in Taiwan. Interna Breast J. 2019;14(1):18. doi:10.1186/s13006-019-0213-1
28. EDHS. Ethiopia Demographic Health Survey 2016, Central statistical agency Addis Ababa. The DHS Program ICF. Rockville. Available at https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf.
29. Lenja A, Demissie T, Yohannes B, Yohannis M. Determinants of exclusive breastfeeding practice to infants aged less than six months in offa district. Interna Breast J. 2016;11(1):1–7. doi:10.1186/s13006-016-0091-8
30. Mekuria G, Edris M. Exclusive breastfeeding and associated factors among mothers in debreMarkos, Northwest Ethiopia: a cross-sectional study. Int Breastfeed J. 2015;10(1):1. doi:10.1186/s13006-014-0027-0
31. Kasahun AW, Wako WG, Gebere MW, Neima GH. Predictors of exclusive breastfeeding duration among 6–12 month aged children in gurage zone, South Ethiopia: a survival analysis. Interna Breast J. 2016;12(1):1–9. doi:10.1186/s13006-017-0107-z
32. Adugnaw E, Gizaw G, Girma M, et al. The median time to stopover exclusive breastfeeding among employed and unemployed mothers of infants aged 6–12 months in Ethiopia, 2019. Sci Rep. 2023;13(1):6259. doi:10.1038/s41598-023-29729-z
33. Tama TD, Astutik E, editors. Exclusive breastfeeding survival and factors related to early breastfeeding cessation in Indonesia. 2nd International Conference on Sports Sciences and Health 2018 (2nd ICSSH 2018); 2019: Atlantis Press.
34. Ayton J, van der Mei I, Wills K, Hansen E, Nelson M. Cumulative risks and cessation of exclusive breast feeding: Australian cross-sectional survey. Arch Dischildhood. 2015;100(9):863–868. doi:10.1136/archdischild-2014-307833
35. Babakazo P, Donnen P, Akilimali P, Ali NMM, Okitolonda E. Predictors of discontinuing exclusive breastfeeding before six months among mothers in Kinshasa: a prospective study. Interna Breast J. 2015;10(1):1–9. doi:10.1186/s13006-015-0044-7
36. Ogwu A, Moyo S, Powis K, et al. Predictors of early breastfeeding cessation among HIV‐infected women in Botswana. Trop Med Interna Health. 2016;21(8):1013–1018. doi:10.1111/tmi.12729
37. Díaz CE, López R, Herrera I, Arena D, Giraldo C, Gonzáles L. Factors associated with breastfeeding in children less than one year of age in the city of Cartagena, Colombia. Colombia Médica. 2011;42(2):26–34. doi:10.25100/cm.v42i2supl1.817
38. Shahrani ASA, Hushan HM, Binjamaan NK, Binhuwaimel WA, Alotaibi JJ, Alrasheed LA. Factors associated with early cessation of exclusive breast feeding among Saudi mothers: a prospective observational study. J Family Med Prim Care. 2021;10(10):3657–3663. doi:10.4103/jfmpc.jfmpc_852_21
39. Belachew T, Haile M, Yeneabat T. Determinants of cessation of exclusive breastfeeding in ankesha guagusa woreda, awi zone, Northwest Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. 2014;14. doi:10.1186/1471-2393-14-262
40. Kelkay B, Kindalem E, Tagele A, Moges Y. Cessation of exclusive breastfeeding and determining factors at the university of Gondar comprehensive specialized hospital, Northwest Ethiopia. Int J Pediatr. 2020;2020:1–9. doi:10.1155/2020/8431953
41. Elyas L, Mekasha A, Admasie A, Assefa E. Exclusive breastfeeding practice and associated factors among mothers attending private pediatric and child clinics, addis ababa, Ethiopia: a cross-sectional study. International Journal of Pediatrics. 2017;2017:1–9. doi:10.1155/2017/8546192
42. Chang P-C, S-F L, Yang H-Y, et al. Factors associated with cessation of exclusive breastfeeding at 1 and 2 months postpartum in Taiwan. Interna Breast J. 2019;14(1):1–7.
43. Mohite RV, Kshirsagar VY, Mohite VR. Prevalence and determinants of cessation of exclusive breastfeeding among primi-para rural Indian mothers. Interna J Commun Med Public Heal. 2019;6(1):24.
44. Kimani-Murage EW, Madise NJ, Fotso J-C, et al. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health. 2011;11(1):1–11. doi:10.1186/1471-2458-11-396
45. Kedir S, Belachew T, Wondafrash M, Kedir S. Time to early cessation of exclusive breast feeding and associated factors among 6–12 months old children: survival analysis. Clin Nutr ESPEN. 2022;50:283–288. doi:10.1016/j.clnesp.2022.04.030
46. Kebede T, Woldemichael K, Jarso H, Bekele BB. Exclusive breastfeeding cessation and associated factors among employed mothers in dukem town, central Ethiopia. Interna Breast J. 2020;15(1):6. doi:10.1186/s13006-019-0250-9
47. Dhakal B, Thapa P. Factors associated with discontinuing exclusive breastfeeding among mothers of infants aged 0-6 months. J Coll Med Sci. 2021;17(3):257–264. doi:10.3126/jcmsn.v17i3.38676
48. Ali F, Msuya SE, Mamseri R, Mgongo M, Mboya IB. Time to cessation of exclusive breastfeeding and associated factors among women with children aged 6-24 months in Kilimanjaro region, Northern Tanzania: a community-based cross-sectional study. PLoS One. 2021;16(10):e0259041. doi:10.1371/journal.pone.0259041
49. Aldalili AYA E, Mahalli AA. Research title: factors associated with cessation of exclusive breastfeeding. J Multidiscip Health. 2021;Volume 14:239–246. doi:10.2147/JMDH.S277819
50. Jiang L, Li X, Wang MC, Osgood N, Whaley SE, Crespi CM. Estimating the population impact of hypothetical breastfeeding interventions in a low-income population in Los Angeles County: an agent-based model. PLoS One. 2020;15(4):1.
51. Issaka AI, Agho KE, Page AN, Burns PL, Stevens GJ, Dibley MJ. Factors associated with early introduction of formula and/or solid, semi-solid or soft foods in seven francophone West African countries. Nutrients. 2015;7(2):948–969. doi:10.3390/nu7020948
52. UNICEF. United Nations Children’s Fund Improving child nutrition: the achievable imperative for global progress. Div Commun UNICEF. 2013;1–132.
53. Gogr M. The disadvantages of baby formula. 2015.
54. Dukuzumuremyi J, Acheampong K, Besig J, Luo J. Knowledge, attitude, and practice of exclusive breastfeeding among mothers in East Africa: a systematic review. International Breastfeeding Journal. 2020;15(1). doi:10.1186/s13006-020-00313-9
55. Pérez-Escamilla R, Lutter C, Segall M, Rivera A, Treviño-Siller S, Sanghvi T. Exclusive breast-feeding duration is associated with attitudinal, socioeconomic and biocultural determinants in three Latin American countries. J Nutr. 1995;125(12):2972–2984. doi:10.1093/jn/125.12.2972
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


