Back to Journals » Journal of Blood Medicine » Volume 14
Factors Influencing Blood Donation Practice Among Health Care Providers of Public Hospitals in Bahir Dar City, North West Ethiopia: A Case Control Study
Authors Tebabal B, Anagaw TF , Adamu A , Atnafu DD
Received 26 May 2023
Accepted for publication 11 August 2023
Published 1 September 2023 Volume 2023:14 Pages 487—498
DOI https://doi.org/10.2147/JBM.S423013
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Belto Tebabal,1 Tadele Fentabil Anagaw,2 Ayinengida Adamu,3 Desta Debalkie Atnafu3
1Department of Public Health, Amhara Regional Health Bureau, Bahir Dar, Ethiopia; 2Department of Health Promotion and Behavioral Science, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia; 3Department of Health System Management and Health Economics, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Correspondence: Tadele Fentabil Anagaw, Tel +251-927692916, Email [email protected]
Background: Blood donation is a technique in which blood is collected from a healthy individual for transfusion to someone else. WHO estimates that it is necessary to donate blood to 2% to 3% of the country’s population to meet blood needs. However, blood donation remains challenging in developing countries.
Objective: This study aimed to identify factors influencing blood donation practices among healthcare providers in public hospitals in Bahir Dar City.
Methods: This institution-based unmatched case-control study was conducted in Bahir Dar City Public Hospitals from May 01 to May 25, 2022. Total sample size was 491 (123 cases and 368 controls) and then the study subject was selected by using simple random sampling technic and collect data through self-administered questionnaire. Bi-variable and multi-variable binary logistic regression analyses were used to determine the association between dependent and independent variables. Finally, the results are presented in charts and tables, and the AOR and CI are reported. Statistical significance was set at P < 0.05.
Results: Fear of anemia (adjusted odds ratio (AOR): 0.02; 95% CI 0.007– 0.078), lack of opportunity (AOR: 0.42; 95% CI 0.22– 0.83), lack of time (AOR: 0.03; 95% CI, 0.005– 0.199), profession (AOR: 0.15; 95% CI, 0.05– 0.42), aware of free medical checkup (AOR: 31.79; 95% CI 13.13– 76.94), willingness to donate blood (AOR: 5.09; 95% CI 2.25– 11.50), blood group type (AOR: 5.67; 95% CI 1.42– 22.68), and higher work experience (AOR: 7.99; 95% CI 2.59– 24.67) were found to be significantly associated with blood donation practice.
Conclusion: This study revealed that multiple factors influenced the practice of blood donation among healthcare providers. Therefore, access to blood donation areas and emphasizing the importance of donor blood donation are important for facilitating blood donation.
Keywords: blood donation, blood donation practice, case control, health care providers
Introduction
Blood donation is the practice of gathering blood from willing donors, who are unlikely to become infected or whose health is negatively affected by blood.1 Blood donation is a technique in which blood is collected from a willing and healthy person for the purpose of transfusion to someone else.2
The availability of blood varies significantly between low- and high-income nations. A country’s general blood supply can be determined by examining the percentage of whole-blood donations. In high-income nations, the median blood donation rate is 31.5 donations per 1000 individuals. As a comparison, 16.4 donations per 1000 people were made in upper-middle-income countries, 6.6 donations per 1000 people were made in lower-middle-income countries, and 5.0 donations per 1000 people were made in low-income countries.3
Studies in different area show there is low practice of blood donation among health care workers. In Nigeria Benin Teaching Hospital medical practitioners 41.4%, Ethiopia Arsi Negele Hospital 39.5%, Tigray region hospital 47.8% and Tikur Anbessa Hospital 38.3% and University of Gondar Hospital 33.2%.4–8
Knowledge, attitude, sex, age, and presence of family members or relatives who have received blood among medical personnel, profession, higher work experience, married health professionals, adequate education, inaccessibility blood bank, fear of anemia, and not being asked to donate blood are factors associated with blood donation practice.4–6
Millions of people require blood donations during various medical emergencies and circumstances. The various medical conditions that require blood to remain alive are insufficient to ensure a safe blood supply to people in need in Ethiopia.7
WHO estimates that it is necessary to donate blood to 2% and 3% of the country’s population; to meet the most basic blood needs of a country, but in Ethiopia less than 0.5% of the population of donate blood.8 Blood transfusions save lives and improve health, but many patients needing blood transfusions do not have timely access to a safe blood source.9
Study shows that the gap between the demand and supply of blood is wide in many low- and middle-income countries, with a global annual blood demand of 304,711,244 and supply of 272,270,243 blood product units for a demand/supply ratio of 1.12. Out Of 195 countries, 119 countries (61%) did not have an adequate blood supply to meet their needs. In these 119 countries, the unmet need totals 102,359,632 units of blood products or 1849 units per 100,000 people worldwide. Not all countries in Central, Eastern, and Western sub-Saharan Africa, Oceania, and South Asia have enough blood to meet their needs.10 Most of the countries in the world are facing a concerning shortage of blood due to a decrease in donations.11,12 This is the worst blood shortage in more than 10 years and poses the risk of raising concerns about patient care.12
Barriers to blood donation include medical reasons, fear (needles, dizziness, etc.), lifestyle barriers, lack of marketing communication, lack of knowledge about blood donation, and negative experiences related to blood donation.13 Rapid access to blood transfusions plays an important role in reducing the morbidity and mortality rates in healthcare settings. Although the global demand for blood has gradually increased, there is still evidence of blood shortages and blood products in developing countries, including Ethiopia.14
According to study done at Addis Ababa, blood availability is insufficient to meet the increased demand for blood and its components. The National Blood Bank of Ethiopia collects nearly 200,000 units of donor blood each year, which is equivalent to 200,000 pints/94,000 liters. The country requires 18,000 units of blood (18,000 pints/8460 liters) per day, but the average daily blood collection is approximately 1100 units (1100 pints/517 liters), which is a shortfall of 16,900 pints/7943 liters.15
Pregnant women, cancer patients, and individuals with an illness that causes anemia often have very important transfusion needs, which complicate a blood crisis because these patients require components or specific blood products.16,17 Patients who have experienced serious injuries from car crashes,18 when the demand for blood is too high, anemia leads to significant morbidity and mortality.7
Continual work is required to create new frameworks and methods that will aid in enlisting more blood donors, owing to the imbalance between the supply and demand for blood.19,20 In Ethiopia, considerable research has been conducted on blood donation at a community level. However, little research has been conducted on the practice of blood donation among health care providers.
Sub-Saharan Africa (SSA) has a very high maternal mortality rate (MMR) according to a global assessment for the year 2019, with a point estimate for 2017 of 542 (UI 498–649) maternal deaths per 100,000 live births. Up to 72% of maternal deaths are attributable to the inability to treat severe fetal hemorrhage with blood. Delayed transfusion has also been linked to higher newborn mortality.21 This study aimed to identify the factors influencing blood donation practices among the healthcare providers of public hospitals in Bahir Dar City, North West Ethiopia.
Methods and Materials
Study Design and Period
An unmatched facility-based case-control study was conducted at public hospitals from May 1 to May 25, 2022, in Bahir Dar City, Ethiopia.
Study Area and Setting
The study was conducted at Bahir Dar City Public Hospital, the capital of the Amhara regional state of northwest Ethiopia, 560 km from Addis Ababa. The region has an elevation of 1801 m above sea level. Total population of Bahir Dar city were 345 084.22 Bahir Dar City administration has 28 governmental health facilities, including three public hospitals, Tibebe Ghion specialized hospital (TGSH), Felege Hiwot comprehensive specialized hospital (FHCSH) and Addis Alem primary hospitals (AAH). Forty-three (43) blood banks are available all over the country in Ethiopia, including ten blood bank centers in Amhara region. Ten blood bank sites serve for blood collection, distribution to hospitals and share information on blood donation to increase blood donation in Amhara region and save people's life by delivering blood. Bahir Dar city public hospitals have blood dispensing units that are collected by the blood banks.
Sources Populations
All health care providers work in public hospitals in Bahir Dar city.
Study Populations
For Cases: Healthcare providers with blood donation practice during or within three years of the study period.
For Controls: Healthcare providers did not have blood donation practices during or within three years of the study period.
Inclusion Criteria
For cases, healthcare providers with blood donation practices in the RBB before or during the study period.
Controls: Health care providers without blood donation practice before or during the study period.
Exclusion Criteria
Cases: Healthcare providers with blood donation practices outside the Bahir Dar district, donated beyond the last three years, with sick leave, annual leave, and maternity leave were excluded from the study.
Controls: Healthcare providers without blood donation practices with sick leave, annual leave, and maternity leave were excluded from the study.
Study Variables
Dependent variables: Blood donation practice.
Independent variables: Sociodemographic characteristics: Age, Sex, Religion, Marital status, educational status, Profession, Work experience, easy accessibility of the blood bank, Attitude and Knowledge of blood donation practice.
Operational Definition
Cases: Healthcare providers with blood donation practice at RBB during and before three years of the study period.
Controls: Health care providers without blood donation practice during and before the study period.
Blood donation practice, having at least one history of blood donation within the last three years in blood bank, was used to label them as having practice.23
Knowledge on blood donation: was measured by using seven questions “of them two questions values five and six points each” to assess knowledge of blood donation. For the “correct” and “incorrect” response, “1” and “zero” scores were used, respectively. The total score was obtained by summing the scores for the seven knowledge questions. The scoring ranged from 0 to 16. Those participants who were answered “eight” or more questions correctly from 16 (≥50%) were considered as knowledgeable.24
Attitude: was measured using 11 questions and responses were coded as if correctly answered as 1 and if not correctly answered 0. The total attitude score was calculated by summing up the individual’s response that range from 0 to 11. Study participants who scored >+50% had favorable attitude and below half were unfavorable attitude. Attitudes: In this study, attitudes were assessed using 11 questions. Similar to knowledge scoring “1” and “zero” were used for favorable and unfavorable attitude, respectively. A total score was calculated to determine the total attitude score. The scores ranged from 0 to 11. Attitude scores of half and more were considered favorable.24
Never donors: if participants do not donate blood in their lives.
Ever donated: Respondents who donate once or more in their lifetime.25
Sample Size Determination and Sampling Procedures
The sample size was calculated based on the double population proportion formula using Epi Info software version 7.2.5.0, and the following assumptions were made: 95% confidence, 90% power, 1:3 ratio of case -to- control, and 10% non-response rate. Based on these assumptions, the reasonable sample size was calculated as 491 (123 cases and 368 controls)26 (Table 1).
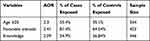 |
Table 1 Sample Size Calculation of Influencing Factors of Blood Donation Practice in the Previous Study Conducted in North East Ethiopia, 202127 |
Data was collected from the three public hospitals, namely TGSH, FHCSH and AAH in Bahir Dar city, with a total of 1766 health care providers. Three public hospitals’ health care workers were included in the study with the total number of health care providers in each hospital were at TGSH (707), FHCSH (903) and AAH (156). After identifying cases and controls that means who had blood donation practices and non-donors at each hospital proportional allocation of cases and controls were done. The cases and controls of each hospital were TGSH (49,147), FHCSH (63,189) and AAH11,28 respectively. Finally, cases and controls were selected by using simple random sampling technique by using random number table in each selected facility.
Data Collection Tools and Techniques
Data collection tool was adapted from similar literatures.26,29,30 A structured self-administered questionnaire was used to collect data from the participants. Six trained nurses were recruited as data collectors, and the principal investigator, as a supervisor, followed the data collection activities. The data collectors received one day training during the data collection procedures. Prior to the primary data collection process, the questionnaire was pretested with 25 healthcare professionals (5% of the sample health care providers) at the neighboring Merawi Hospital. After the pretest, a few questions in the questionnaire were revised for clarity, logical order, skip patterns, and wordiness.
Data Quality Assurance
The questionnaires were translated into the Amharic language and then back into English for consistency. A day of training was provided to the data collectors. The principal investigator controlled the overall activity. Data quality was controlled by pretest the questionnaire before the actual data collection for 5% of the sample size and modifying to the proper data collection materials after pilot study. All the completed questionnaires were examined for completeness and consistency during data management, storage, and analysis.
Data Management and Analysis
The collected data were entered using Epi-data version 3.1 statistical software and then exported to SPSS version 23 for analysis. Descriptive statistics of the collected data were performed using relevant statistical parameters such as frequency and percentage. At 25% level of significance bi-variable binary logistic regression analysis was performed to screen for potentially significant independent variables and using significant independent variables multivariable binary logistic regression analysis was performed to determine the association between the dependent variable and independent variables. The Hosmer-Lemeshow goodness-of-fit test was used to check the adequacy of the final model, and the model was fitted to the data. For multivariable (covariates) binary logistic regression, 95% confidence interval was computed, and variables with p-value <0.05, were considered as statistically significant for the dependent variable.
Results
Socio Demographic Characteristics
This study had a response rate of 100% with 123 cases and 368 controls a total of 491 participants, from the total participants 226 (61.41%) of controls and 42 (34.15%) of cases were in the age group of 23–29 years; 210 (57.1%) of controls and 89 (72.4%) of cases were male healthcare providers; 332 (90.22%) of controls and 112 (91%) of cases were orthodox; 215 (58.4%) of controls and 84 (68.3%) cases were married; 293 (79.62%) of controls and 65 (52.84) of cases were Bachelors (BSc) in educational status; 194 (52.72%) of controls and 42 (34.15%) of cases were nurse professionals; 229 (62.23%) of controls and 54 (43.9%) of cases were 0–6 years’ work experience (Table 2).
 |
Table 2 Socio Demographic Characteristics of Health Care Providers Who are Working in Public Hospitals, Bahir Dar City, Ethiopia, July 2022. (N = 491) |
Easily Accessibility of Blood Bank Donation Center
From a total of 491 participants, 123 cases and 368 controls, 265 (72.01%) of controls, and 95 (77.2%) of cases of health care providers had blood bank access.
Knowledge Related Factors
Of the total participants, 225 (61.14%) controls and 73 (59.35%) cases were responded good health as criteria for donating blood; minimum interval of blood donation was 263 (71.5%) controls and 104 (84.55%) cases were accurate responses; time required for donation was 229 (62.22%) controls and 87 (70.73%) cases had inaccurate responses; benefits of blood donation 265 (72.01%) controls and 90 (73.17%) cases were responded happiness; 167 (45.38%) of controls 68 (55.28%) cases had adequate knowledge (Table 3).
 |
Table 3 Knowledge-Related Influencing Factors of Blood Donation Practice Among Health Care Providers of Public Hospitals, Bahir Dar City, Ethiopia, July 2022 (n = 491) |
Attitudinal Influencing Factors
Of the total participants, 207 (56.25%) controls and 96 (78.05%) cases were family members or close friends who ever needed blood transfusion,187 (50.81%) of controls and 81 (65.85%) of cases had family members or close friends who donated blood. Two hundred and eighty-eight (78.26%) controls and 108 (87.80) patients were overall favorable attitude (Table 4).
 |
Table 4 Attitudinal Influencing Factors of Blood Donation Practice Among Health Care Providers of Public Hospitals, Bahir Dar City, Ethiopia, July 2022 (N = 419) |
Reasons for Not Practicing Regularly Donate Blood
Of the total participants, the reason not to practice/regularly donate blood were 239 (64.94%) of controls 58 (47.15%) of cases were responded lack of opportunity; 154 (41.85%) of controls 5 (4.06%) of cases feared of anemia respectively; mainly identified reasons that not to donate/not to donate blood regularly (Figure 1).
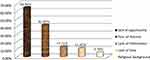 |
Figure 1 Reasons for not practicing blood donation among healthcare providers at public hospitals, 2022, Bahir Dar city, Ethiopia. |
Factors Associated with Blood Donation Practice
The variables age, sex, marital status, education, work experience, profession, how often an individual donates blood, awareness of free medical checkup, blood donation, family member, or close friend who ever received blood transfusion, family member or close friend who donated blood, lack of opportunity, fear of anemia, lack of time, blood group, willingness to donate blood, and overall attitude were associated with the practice of blood donation on Bivariable binary logistic regression at a P-value of less than or equal to 0.25. The results of the Bivariable logistic regression were entered into a multivariable binary logistic regression analysis.
Thus, fear of anemia, lack of opportunity, lack of time, medical doctor by profession, awareness of free medical checkups, willingness to donate blood, blood group type, etc. Work experience was significantly associated with blood donation practice.
The odds of blood donation practice among healthcare providers who reported fear of anemia were 98% lower than the odds for health care providers free from fear of anemia (AOR 0.02 95% CI 0.007–0.078). The odds of blood donation practices by healthcare providers who reported lack of opportunity were 58% lower than the odds for health care providers that they had an opportunity (AOR: 0.42 95% CI 0.22–0.83). The odds of blood donation practice among healthcare providers who reported lack of time were 97% lower than the odds for health care providers free from (AOR: 0.03 95% CI 0.005–0.199). The odds of blood donation practice were 31.79 times higher aware of free medical checkup among non-aware of free medical checkup (AOR: 31.79 95% CI 13.13–76.94). The odds of blood donation practice of health care providers were 5.09 times higher willingness to donate blood than among non-willingness to donate blood (AOR: 5.09 95% CI 2.25–11.50). The odds of blood donation practice in the common blood group were 5.67 times higher than those among those who did not know their blood group status (AOR: 0.5.67 95% CI 1.42–22.68). The odds of blood donation practice of health care providers were 7.99 times higher blood donation practice of work experience of ≥13 years than among 0–6 years’ (AOR 7.99 95% CI 2.59–24.6) (Table 5).
 |
Table 5 Multiple Logistic Regression Analysis of Factors of Blood Donation Practice Among Health Care Providers of Public Hospitals, Bahir Dar City, Ethiopia, July 2022 (N = 419) |
Discussion
In keeping with the objective of this study, an effort was made to identify the variables influencing the practice of blood donation among healthcare providers in public hospitals. The study found that the following variables influenced the practice of blood donation: fear of anemia, lack of opportunity, lack of time, MD by profession, awareness of free medical checkups, willingness to donate blood, blood group type, and work experience.
Health care providers who fear anemia were 98% less likely practicing blood donation than healthcare providers among free from fear of anemia; this result is slightly higher than studies conducted in ALERT Hospital, Ethiopia30 Fear of anemia and not approaching donation were the leading reasons for non-donors. The fact that our study only considered healthcare providers from public hospitals, where participants might have higher exposure, a reliable source of information, and access to blood bank donation centers, may be one of the most plausible causes of the disparities.
Health care providers who thought there was lack of opportunities were 58% less likely to practice blood donation compared to health care providers who thought there were opportunities. This outcome was in line with study conducted in Nigeria27, which may indicate that lack of opportunity is one of influencing factors for blood donation practice. This can be accomplished by fostering opportunities, particularly among healthcare workers, and the need for action to be taken, which gives individuals a chance to expose healthcare providers to practice blood donation.
The odds of voluntary blood donation practice in health care providers who reported lack of time were 97% less likely to practice blood donation compared to health care providers who thought that they had time to donate. This outcome is consistent with that of studies conducted in Nigeria and Ethiopia.27,29 This might be due to the high workload of the hospitals. Therefore, responsible bodies will establish a connection with healthcare institutions, inform them of onsite blood collection time, and make regular use of mobile blood supply facilities.
Health professionals of nursing and Midwife health care providers were 77% and 91% less likely to practice blood donation compared to MDs by profession, respectively. This study is in line with study in Tigray Health healthcare providers with a degree at their level of education were 69% less likely to donate blood than specialists.31 This might be the difference in level of understanding. The higher the status of health professional knowledge, the more practicing blood donation this study is in line with studies done in Bahir Dar Health professionals who were more likely than other professions to donate blood voluntarily.32
Healthcare providers who were aware of free medical checkup were 31.79 times higher blood donation practice than those who were unaware of free medical checkups. Among people who had never donated blood, the blocking factor was fear of the announcement of test results in 6.57%, and fear of health problems after screening (39.3%) was the main reason cited by non-donors.
The odds of practicing blood donation among healthcare providers who were willing to practice blood donation were 5.09 times higher compared to those among healthcare providers with non-willingness. This outcome is consistent with research conducted in various parts of Ethiopia. The results were slightly higher than those of studies conducted in Chiro town of Eastern Ethiopia and lower than those of studies conducted among students at Madda Walabu University and Bale Robe town in Southeast Ethiopia.28,33,34 This discrepancy might be due to differences in the study population and sociodemographic factors, suggesting that willingness to donate blood is a crucial variable that significantly influences practices related to blood donation.
The odds of practicing blood donation among healthcare providers of common blood groups were 5.67 times higher than those of healthcare providers who did not know their blood group type. All common and ever-rare blood groups were represented by participants in their study. This study implies that healthcare professionals donate blood voluntarily and that they do so when there is a need, particularly when there is a scarcity of blood from common blood groups. This study contrasts with that conducted in Northern India.35 This is because of the differences in the study populations and the reasons why they were aware of their own blood groups.
Healthcare providers with >13 years of work experience were 7.99 times higher blood donation practice than compared with health care providers and 0–6yrs. This outcome was similar to the study being practical in Tigray regional state public hospitals, northern Ethiopia and Arsi. In comparison to those with >11 years of work experience, those with one to five years of work experience were less likely to donate blood.5,23 This might be because those with more experience were more frequently exposed to blood donation than those with less experience.
Conclusion
This study revealed that multiple factors influenced the practice of blood donation among healthcare providers. Type of profession, fear of anemia, access to blood bank, lack of time, and work experience were determinant factors for blood donation. Therefore, access to blood donation areas and emphasizing the importance of blood donation for both donors and patients who need blood are important for facilitating blood donation.
Data Sharing Statement
All the necessary data are available from the corresponding author and will be provided upon reasonable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the institutional review board of Bahir Dar University, College of Medicine and Health Sciences with ethical review board (IRB). Written informed consent was obtained from all the participants. The study participants provided written informed consent to withdraw at any point in the data collection, and the data were confidentially secured. All methods were carried out in accordance with the relevant guidelines and regulations and complied with the Helsinki Declaration.
Acknowledgments
This article is presented as part of thesis at Bahir Dar university “Factors Influencing Blood Donation Practice Among Health Care Providers Of Public Hospitals In Bahir Dar City, North West Ethiopia, A Case Control Study” https://ir.bdu.edu.et/handle/123456789/15220. We would like to thank Bahir Dar University, data collectors, supervisors, and the study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
All authors declare that they have no competing interests for this work.
References
1. World Health Organization. Blood Donor Selection: Guidelines on Assessing Donor Suitability for Blood Donation. World Health Organization; 2012.
2. Nureye D, Tekalign E. Opportunities and challenges of blood donation and blood therapy in Ethiopia. Health Sci. 2019;8:122–127.
3. World Health Organization. Global Status Report on Blood Safety and Availability 2021. World Health Organization; 2022.
4. Urgesa K, Hassen N, Seyoum A. Knowledge, attitude, and practice regarding voluntary blood donation among adult residents of Harar town, Eastern Ethiopia: a community-based study. J Blood Med. 2017;8:13. doi:10.2147/JBM.S121460
5. Yirgu AN, Mohammed KH, Diriba SD, Babso AK, Abdo AA. Blood donation and associated factors among employees working at Negele Arsi General Hospital and Medical College, Southeast Ethiopia: a cross-sectional study. J Blood Med. 2021;12:475. doi:10.2147/JBM.S301826
6. Arage G, Ibrahim S, Adimasu E. Blood donation practice and its associated factors among health professionals of University of Gondar Hospital, Northwest Ethiopia: a cross sectional study. BMC Res Notes. 2017;10(1):1–6. doi:10.1186/s13104-017-2618-5
7. Getie A, Wondmieneh A, Bimerew M, Gedefaw G, Demis A, Onida F. Blood donation practice and associated factors in Ethiopia: a systematic review and meta-analysis. Biomed Res Int. 2020;2020:1–8. doi:10.1155/2020/8852342
8. World Health Organization. Screening Donated Blood for Transfusion-Transmissible Infections: Recommendations. World Health Organization; 2010.
9. World Health Organization. Blood Safety and Availability. World Health Organization; 2020.
10. Roberts N, James S, Delaney M, Fitzmaurice C. The global need and availability of blood products: a modelling study. Lancet Haematol. 2019;6(12):e606–e615. doi:10.1016/S2352-3026(19)30200-5
11. Blood Shortage Canadian C. Drought in Namibia the Namibian; 2013.
12. Warner MA, Patel PA, Hensley NB, Mazzeffi M. COVID-19-related blood shortages and cardiac surgery: do we have too many eggs in one basket? J Cardiothorac Vasc Anesth. 2022;36(7):1823–1826. doi:10.1053/j.jvca.2022.02.021
13. Abdelgader A, Al Ghumlas AK. The future of voluntary blood donation in the Kingdom of Saudi Arabia. Transfusion. 2020;60(S1):S28–S34. doi:10.1111/trf.15683
14. Mohammed S, Essel HB. Motivational factors for blood donation, potential barriers, and knowledge about blood donation in first-time and repeat blood donors. BMC Hematol. 2018;18(1):1–9. doi:10.1186/s12878-018-0130-3
15. Gurmu ED, Gezaw MA, Asfaw YM. Utilization of blood and blood products among pediatric patients admitted to St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. Ethiopian J Pediatr Child Health. 2021;16(2):1–13.
16. Guan W-J, Z-y N, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi:10.1056/NEJMoa2002032
17. Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173(5):362–367. doi:10.7326/M20-3012
18. Allon R, Epstein D, Shavit I. Prehospital transfusion of low titer cold‐stored whole blood through the intraosseous route in a trauma patient with hemorrhagic shock. Transfusion. 2020;60(4):875–878. doi:10.1111/trf.15732
19. Li L, Li KY, Yan K, et al. The history and challenges of blood donor screening in China. Transfus Med Rev. 2017;31(2):89–93. doi:10.1016/j.tmrv.2016.11.001
20. Bagot KL, Murray AL, Masser BM. How can we improve retention of the first-time donor? A systematic review of the current evidence. Transfus Med Rev. 2016;30(2):81–91. doi:10.1016/j.tmrv.2016.02.002
21. World Health Organization. WHO African Region Status Report on Blood Availability, Safety and Quality. World Health Organization; 2022.
22. Ambaye E, Regasa ZW, Hailiye G. Early initiation of antenatal care and its associated factors among pregnant women attending antenatal care at public health centres in Bahir Dar Zuria zone, Northwest Ethiopia, 2021: a cross-sectional study. BMJ Open. 2023;13(1):e065169. doi:10.1136/bmjopen-2022-065169
23. Tadesse T, Berhane T, Abraha TH, et al. Blood donation practice and associated factors among health professionals in Tigray regional state public hospitals, northern Ethiopia. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3786-7
24. Enawgaw B, Yalew A, Shiferaw E. Blood donors’ knowledge and attitude towards blood donation at North Gondar district blood bank, Northwest Ethiopia: a cross-sectional study. BMC Res Notes. 2019;12(1):1–6. doi:10.1186/s13104-019-4776-0
25. Seid T, Dimtsu B, Zemene A, Arage G, Mossisa M, Muche T. Voluntary blood donation practice and its associated factors among HealthCare providers, at Axum Town Public Health Facilities, Northern Ethiopia: a cross sectional study. Curr Res Complement Alternat Med. 2017;1(2). doi:10.29011/2577-2201/100007
26. Dejene M, Tefera A, Dires A, Gedamu S, Getachew Y, Ademe S. Low blood donation practice of health sciences college students in Northeast Ethiopia: a cross-sectional study. J Blood Med. 2021;12:43–51. doi:10.2147/JBM.S287398
27. Ayobami SS. Knowledge, attitude and practice of voluntary blood donation among: department of community medicine, faculty of clinical sciences, Ambrose Alli…; 2021.
28. Mohammed AS, Yassin A, Aliyi AA. Voluntary blood donation practice and its associated factors among civil servants in Bale Robe town, Southeast Ethiopia, 2021. SAGE Open Med. 2022;10:20503121221102099. doi:10.1177/20503121221102099
29. Jemberu YA, Esmael A, Ahmed KY. Knowledge, attitude and practice towards blood donation and associated factors among adults in Debre Markos town, Northwest Ethiopia. BMC Hematol. 2016;16(1):1–8. doi:10.1186/s12878-016-0062-8
30. Teferi MY, Woldesenbet SG, Feleke SA, Abebe EH, Adane HT, Alemayehu CM. Assessment of the level and factors associated with knowledge, attitude and practice of blood donation among medical and paramedical personnel in ALERT Hospital, Ethiopia. J Public Health Res. 2021;10(1):1860. doi:10.4081/jphr.2021.1860
31. Tadesse T, Berhane T, Abraha TH, et al. Blood donation practice and associated factors among health professionals in Tigray regional state public hospitals, northern Ethiopia. BMC Res Notes. 2018;11(1):677.
32. Feleke BE. Determinants of voluntary blood donation in the city of Bahir Dar: a case–control study. Asian J Transfus Sci. 2022;16(1):56. doi:10.4103/ajts.AJTS_115_17
33. Mijena GF, Nigussie S, Gobena T, Mitiku H, Abdi H. Voluntary blood donation practice and associated factors among civil servants in Chiro Town of Western Hararghe Zone, Eastern Ethiopia: a cross-sectional study. Res Square. 2019. doi:10.21203/rs.2.11580/v1
34. Darega B, Dida N, Tesfaye T, Lencha B. Voluntary blood donation practices and associated factors among regular undergraduate Madawalabu University Students, Southeast Ethiopia: a facility-based cross sectional study. J Blood Disord Transfus S. 2015;5:S5.
35. Chauhan R, Kumar R, Thakur S. A study to assess the knowledge, attitude, and practices about blood donation among medical students of a medical college in North India. J Fam Med Prim Care. 2018;7(4):693. doi:10.4103/jfmpc.jfmpc_54_17
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
