Back to Journals » Clinical Interventions in Aging » Volume 19
Health Outcomes for Older Patients with Chronic Diseases During the First Pandemic Year
Authors Matovelle P , Oliván-Blázquez B, Domínguez-García M , Casado-Vicente V , Pascual de la Pisa B, Magallón-Botaya R
Received 14 October 2023
Accepted for publication 6 February 2024
Published 6 March 2024 Volume 2024:19 Pages 385—397
DOI https://doi.org/10.2147/CIA.S444716
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Priscila Matovelle,1,2,* Bárbara Oliván-Blázquez,3– 5,* Marta Domínguez-García,6,7 Verónica Casado-Vicente,8,9 Beatriz Pascual de la Pisa,10– 12 Rosa Magallón-Botaya2– 4,8
1Department of Geriatrics, San Juan de Dios Hospital, Zaragoza, Spain; 2Department of Medicine, Psychiatry and Dermatology, University of Zaragoza, Zaragoza, Spain; 3Group B21-20R, Health Research Institute of Aragon (IISA), Zaragoza, Spain; 4Network for Research on Chronicity, Primary Care, and Health Promotion (RICAPPS), RD21/0016/0005, Zaragoza, Spain; 5Department of Psychology and Sociology, University of Zaragoza, Zaragoza, Spain; 6Primary Care Research Unit (GAIAP), Aragon Health Research Institute (IISA), Zaragoza, Spain; 7Aragonese Healthcare Service, Zaragoza, Spain; 8Parquesol Primary Care Center, Valladolid, Spain; 9Department of Medicine, University of Valladolid, Valladolid, Spain; 10Santa María de Gracia Primary Care, Seville, Spain; 11Department of Medicine, University of Seville, Seville, Spain; 12Network for Research on Chronicity, Primary Care, and Health Promotion (RICAPPS), RD21/0016/0015, Zaragoza, Spain
*These authors contributed equally to this work
Correspondence: Bárbara Oliván-Blázquez, Email [email protected]
Background: Worldwide, chronic diseases are prevalent among the older adults, significantly affecting their health and healthcare system. The COVID-19 pandemic exacerbated these challenges, disrupting healthcare services. Our study assesses the impact on older individuals with chronic diseases who were not infected with COVID-19, analyzing comorbidities, medication use, mortality rates, and resource utilization using real data from Aragon, Spain.
Methods: A retrospective observational study, conducted in Aragon, Spain, focused on individuals aged 75 and older with at least one chronic disease, who were not infected of COVID-19. The research used actual data collected during three distinct periods: the first covered the six months prior to the pandemic, the second the six months after the lockdown, and the third the period between six and twelve months. Key variables included socio-demographics, comorbidities, clinical parameters, medication use, and health services utilization.
Results: We included 128.130 older adults. Mean age was 82.88 years, with 60.3% being women. The most common chronic diseases were hypertension (73.2%), dyslipidemia (52.5%), and dorsopathies (31.5%). More than 90% had more than 2 conditions. A notable decline in new chronic disease diagnoses was observed, particularly pronounced in the six to twelve months period after lockdown. Although statistically significant differences were observed in all clinical variables analyzed, they were considered clinically irrelevant. Furthermore, a decrease in healthcare services utilization and medication prescriptions was reported.
Conclusion: Our study highlights a decrease in new chronic disease diagnoses, ongoing reductions in healthcare utilization, and medication prescriptions for older adults with pre-existing chronic conditions, unaffected by COVID-19.
Keywords: chronic diseases, older adults, COVID-19 pandemic, healthcare utilization, comorbidities
Introduction
Chronic diseases are highly prevalent among the older adults. In Spain, data from the National Health Survey reveal that people over 75 years of age usually have an average of 3.2 chronic health problems, while people aged 65–74 years (younger population), manage an average of 2.8.1 The coexistence of two or more chronic diseases in the same individual is commonly defined as multimorbidity.2
Multiple chronic conditions have a major impact on the affected population, leading to poor health outcomes, reduced quality of life, increased health care use,3,4 especially at the Primary Health Care (PHC) level but also in the emergency and hospital admission.5
In addition, there has been a significant increase in pharmaceutical spending, accompanied by a rise in inappropriate prescriptions due to this clinical and social problem.6
Multimorbidity in the older population is as high as 98% and has become a significant public health issue that poses challenges to patients, professionals, and health systems alike.7 A common occurrence in the older population is the association between specific chronic diseases known as multimorbidity patterns8,9 the following patterns are described in the literature: cardiovascular, mental, and neurological, chronic respiratory, metabolic and musculoskeletal disease.10 Another combination of chronic diseases is the well-known metabolic syndrome which includes arterial hypertension, diabetes mellitus, and dyslipidemia, leading to cardiovascular disease, stroke, disability, and death.11
The impact of the COVID-19 pandemic on chronically ill older patients has been particularly pronounced, especially as many rely on PHC facilities for ongoing care and support. These healthcare facilities were forced to adapt to the new circumstances to ensure the safety of patients and medical staff, focused on minimizing the risk of virus transmission. Many PHC centers opted to replace face-to-face medical consultations with telephone or online consultations.12 While these measures were crucial for infection control, they had the unintended consequence of reducing the health system’s capacity to effectively prevent and manage chronic diseases.13 In addition, many patients with chronic diseases were unable to attend regular medical appointments due to the restrictions imposed by the pandemic; lack of knowledge about the virus and fear of contracting the disease discouraged them and their families from visiting health centers.14,15 This has had serious consequences for patients’ health, as the lack of adequate medical care can worsen symptoms and increase the risk of complications.
For instance, individuals requiring regular monitoring of parameters such as blood glucose levels, blood pressure (BP), and anticoagulation therapy faced significant disruptions in their care. According to Prieto Rodríguez, some patients had to adjust their insulin doses independently, which posed potential risks to their glycemic control. Additionally, the monitoring of anticoagulation therapy critical for patients at risk of blood clots, became irregular due to delays and cancellations of medical appointments.14 Furthermore, lockdown measures did not only strained healthcare services but have also had a profound impact on individuals’ lifestyles. The confinement restrictions, which limited outdoor activities and access to recreational spaces, posed significant challenges for maintaining a healthy way of life. Balanced diets and regular physical activity essential components to effectively manage and control chronic diseases were compromised. This disruption had serious consequences for those affected, not only in clinical parameters, but also mentally and physically.16–18
In this line, several studies showed a decline in the incidence of new chronic diagnoses, for example Van den Bulck found that chronic lung problems (42%) and obesity (40%) experienced the most substantial reductions during the first wave of covid-19.19 In a different study, similar results were described in which heart disease, chronic obstructive pulmonary disease (COPD), diabetes, depression, and colon and breast cancer decreased during this first wave, however, there was an increase in the diagnosis of anxiety disorders.20
While most research on new chronic diagnoses has been conducted among patients with COVID-19, there is a notable gap in the analysis of the consequences of the pandemic for chronically ill older people who were not infected with COVID-19. Therefore, the aim of our study is to assess new comorbidities, medication use, mortality rates, and health service utilization among patients with chronic diseases using real data (RD) from PHC registries of patients aged 75 years and older in Aragon, Spain.
Methods
Design and Study Population
This is an observational and retrospective study, using RD taken from BIGAN (Big Data project of the Department of Health of the Government of Aragon) collected over three different time periods. In the north-east of Spain, specifically in the Autonomous Community of Aragon, 150,420 people over 75 years of age are registered.21 The average age of the Aragonese population is 82.7 years, 5 decimals higher than the national average and 3 points higher than the European average.22
Given Spain’s universal health coverage system and its high dependence on public primary care services, the data collected in this study are considered highly representative. It is estimated that these data accurately reflect approximately 85% of the population meeting the inclusion criteria established for this study.22
Our study included individuals aged 75 years and older with a clinical history in the Public Aragon Health Service who had a diagnosis of a chronic disease with a prevalence of more than 5%23 according to the International Classification of Primary Care (CIAP-2)24 and these individuals had not been diagnosed with COVID-19 at the time of inclusion in the study (n=128.130 subjects). The existence of positive COVID diagnostic tests (antigen, Polymerase Chain Reaction, or serology) was assessed in the electronic medical record. Chronic diseases considered in our study included arrhythmias, heart failure, ischemic heart disease, hypertension, dyslipidemia, obesity, overweight, vascular disease, cerebrovascular disease, diabetes, chronic bronchitis, chronic obstructive pulmonary disease, asthma, chronic kidney disease, hypo- and hyperthyroidism, smoking, alcoholism, insomnia, anxiety and depression, self-injury, anemia, dementia, hearing loss, cataracts, glaucoma, osteoarthritis, osteoporosis and dorsopathy.23
The COVID-19 pandemic in Spain started on March 15th 2020, following the declaration of a national state of emergency by the Spanish government. This declaration initiated a strict lockdown, requiring the population to stay at home and adhere to strict measures until May 3th.
Data were collected from each patient at different time periods. The baseline measurement was taken in the six months before the start of lockdown (from 14th September 2019 to 15th March 2020) (n =128.130), the second measurement was taken in the six months following the end of strict lockdown (from 3rd May to 4th November 2020) (n = 123.233) and the third measurement was taken from six to twelve months after the lockdown (from 5th November 2020 to 6th May 2021) (n = 118.903).
Variables
The data were obtained from the electronic medical records of the PHC centers. The socio-demographic variables included in the study were:
- Sex and Age.
- Pharmaceutical benefit: Variable associated with the patient’s income, stratified into three groups according to the level of annual income:
- <18,000 euros/year.
- Between 18,000–100,000 euros/year.
- >100,000 euros/year.
- In addition, there were other categories, such as free prescriptions, mutual insurance and uninsured.
- Residence: Distinguishing between semi-urban/rural and urban health areas, the criterion being a population of less than or more than 10,000 inhabitants, respectively.
- Number of deaths considered for each measurement period.
Other variables included:
- Comorbidity: number of diseases.
- Chronic diseases with a prevalence > 5% and new diagnoses of co-morbid conditions.23
- Clinical parameters: such as blood pressure, glucose levels, HbA1c, creatinine, glomerular filtration rate, HDL cholesterol, LDL cholesterol, triglycerides, as well as weight and body mass index (BMI).
- Number of active medicines dispensed by the pharmacy and their cost. It was decided to consider dispensed medication rather than prescribed medication because some prescribed medications might not have been taken by patients if they did not pick them up at the pharmacy.
- Health services utilization:
- PHC and social services:
- Number of nurse visits.
- Number of general practitioner visits for ordinary or continuous care, whether at health centers or in-home settings.
- Number of visits to other healthcare professionals within health centers, such as social workers.
- Specialized Hospital Services:
- Number of visits to specialized care units within hospitals.
- Number of visits to the emergency department.
- Hospitalizations.
- Admissions to the intensive care unit (ICU).
- Duration of hospital stays for each of these services.
- PHC and social services:
Statistical Analysis
Given the large sample size, parametric statistics were used to determine the characteristics of the population in the study variables, a descriptive analysis of the study variables was carried out using frequencies (percentages) to summarize the categorical variables and measures of central tendency and dispersion (mean and standard deviation) for the continuous variables.
For the study population, mortality due to causes other than COVID-19 (as the patients did not contract COVID-19 was assessed by calculating the crude mortality rate for each of the three periods. The population of Aragon in the middle of each of the three periods was used as the denominator.
Differences in drug consumption were assessed (number of active ingredients and cost) in the study population during each period using a paired samples t-test. The mean and standard deviation of each variable of health and social resources (primary and specialized hospital care) were also calculated. A paired samples t-test was used to compare the difference in the mean as well. To evaluate the differences in the percentage of new diagnoses between the 3 times, Cochran’s Q was used. When the sample size was lower than 100 observations, the Wilcoxon test was used. This statistical test was used for analyzing ICU variables since the number of observations was 15 patients (pre-six months) and 24 patients (six to twelve months). The comparisons by sex were calculated using a Student’s t-test or chi squared test depending on the variable (continuous or categorical). All data were stored and analyzed with databases using IBM SPSS Statistics software (version 25.0).
Ethical Considerations
The studies involving human participants were reviewed and approved by the Aragon Clinical Research Ethics Committee. (Protocol code PI20/175, date of approval 13 May 2020). All procedures contributing to this work comply with the ethical standards of the Aragon Clinical Research Ethics Committee (part of the Government of Aragon’s Department of Health) and with the 1975 Helsinki Declaration, revised in 2008. Data were obtained from clinical records provided in a non-identifiable format by the Aragonese Health Service. Written informed consent from the participants or their legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements (Law 14/2007, of 3 July, on Spanish Biomedical Research). The processing, notification and transfer of personal data were carried out in accordance with European Parliament’s 2016/679 Regulation (EU) and the 3/2018 Spanish Organic Law on the Protection of Personal Data and the Guarantee of Digital Rights.
Results
On September 14, of 2019, a total of 128.130 individuals aged 75 years or older, with at least one chronic disease in their PHC records, were included in the study. These individuals did not have COVID-19 throughout the first year of the pandemic. The sample represents 85% of the older population of Aragon.
The mean age of the population was 82.88 (SD: 5.69) years and 77,316 (60.3%) were women. The 78.5% of the participants had an annual income below 18,000 euros and more than a half of patients (52.5%) resided in urban areas (Table 1). The most prevalent chronic diseases were hypertension, which affected 73.2%, followed by dyslipidemia, with 52.5%, and dorsopathies, with 31.5%.
 |
Table 1 Pre-Lockdown Sociodemographic Data and Chronic Illness of the Population |
In terms of patient comorbidity, 53.2% had 5–9 comorbidities and 39.3% with 2–4 diseases (Table 1).
In terms of new diagnoses of chronic comorbidities, we observed a decline in the number of cases. This decrease was evident when we compared the six months before the pandemic with the six months after. However, what was even more notable to us was the pronounced decline in diagnoses when we compared the initial six months prior to the pandemic with the period between six and twelve months after lockdown. It should be noted that the decrease is not uniform across all diseases; some conditions show a more gradual decline than others, indicating variations in their response to the current health scenario. The incidence of chronic diagnosis per 100,000 population in each wave is calculated. In the period “6 months before” the incidence rate is calculated considering a population of 128.130 people over 75 years of age; “6 months after” considering 123.233 people over 75; 6–12 months considering 118.903 people over 75 years. (Table 2).
 |
Table 2 New Diagnoses of Others Chronic Comorbidities in the Cohort During the 6 Months Before the Lockdown, the First 6 Months and from 6 to 12 Months After the Lockdown |
As for the clinical variables, as shown in Table 3, the values remained constant in the three study periods, despite the statistically significant differences identified in most of them. In terms of mortality for the three different period. We found that there were 4897 deaths in the six months prior to the state of emergency, 4330 deaths in the following six months, and 3968 deaths in the six to twelve months after lockdown.
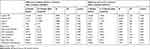 |
Table 3 Comparations of Clinical Variables During 6 Months Before the Beginning of the Pandemic, with 6 Months After the Lockdown. Also 6 Months Before with 6 to 12 Months After the Lockdown |
Considering the population of Aragon aged 75 years and older during these three-time frames21 (excludes COVID-19) rate per 1000 individuals was 32.67 during the six months prior to the beginning of the pandemic, 28.62 during the six first months following the lockdown and 26.12 from six to twelve months following the lockdown. There is a significant decrease (p-value: <0.001) in the mortality rate per 1000 inhabitants.
In terms of number of medications dispensed by the pharmacy and the corresponding expenditure, our analysis demonstrates a decrease when comparing the initial six months before the lockdown with both the subsequent six months and more noticeable drop compare with six to twelve months after it (Figure 1).
 |
Figure 1 Comparation of active number ingredient and cost (euros) during 6 months before the lockdown, the first 6 months and from 6 to 12 months after the lockdown. |
This downward trend persisted throughout the pandemic, reflecting the evolution of health care utilization patterns, as we can see in Table 4 in which the number of consultations by nurses, general practitioners and specialist physicians was reduced after the lockdown. The most notable decrease was in the consultations of general practitioners (at health center or at home) in the 6–12-month period after the state of emergency.
 |
Table 4 Comparations of Number of Health and Social Services During 6 Months Before the Beginning of the Pandemic, 6 Months After the Lockdown, and from 6 to 12 Months After the Lockdown |
Contrary to the above, we can see an increase in the number of visits by social workers and the first and subsequent care provided by specialized physicians in the first six months after the state of emergency. There was also an increase in the number of admissions, and the length of hospital stay has increased in the 6–12-month period after the closure compared to the 6 months before the lockdown.
Discussion
We conducted an analysis of a sizable cohort of 128.130 individuals aged 75 years and older who had a chronic illness and did not contract COVID-19 in a PHC setting, giving us insight into their demographics, clinical and health care utilization during and after the pandemic. It is important to note that other studies about general population with COVID-19, also had also smaller sample sizes.25–27
The refocusing of consultations in PHC during the pandemic has led to a decrease in new diagnoses of chronic comorbidities over time. This finding was evident when we compared the six months before the pandemic with the six months after its onset. However, the decline was even more pronounced when we extended our analysis to twelve months.
It should be mentioned that this reduction did not follow a uniform pattern in all diseases. On the contrary, some conditions showed a more gradual decline than others. Some studies described a reduction in new diagnosis of hypertension, diabetes, and COPD in agreement with our results.25,28,29 As evidenced in both the existing literature and our routine clinical practice, the decline in the incidence of chronic diseases can be ascribed to a combination of factors, including widespread mobility restrictions imposed throughout the country. Additionally, patients displayed a hesitancy to seek face-to-face medical care both during and even after the lifting of restrictions. Furthermore, changes in healthcare delivery models led providers to delay elective healthcare procedures to minimize the risk of virus transmission, despite most healthcare facilities remaining open.15,20,30
In terms of comorbidity, a significant proportion of our cohort had multiple chronic conditions. This observation highlights the complexity of healthcare management in the older population and the potential challenges associated with coordinating care for multiple conditions, which was interrupted during the pandemic. These disruptions contributed to the deterioration of their health.31,32
In parallel, certain aspects of preventive care and/or routine clinical follow-up, such as BP monitoring, BMI assessment, and measurement of abdominal and laboratory parameters, revealed statistically significant results, although with potentially limited clinical significance.
For instance, Coma et al reported a decline in indicators that are key for patients with type 2 diabetes, such as HbA1c levels, BP control in individuals with hypertension, and the regulation of LDL cholesterol levels, crucial for managing ischemic heart disease and stroke.30 Moreover, another study observed an increase in HbA1c levels and a rise in complications among diabetic patients, correlated with the duration of lockdown measures. These findings collectively emphasize that patients with chronic conditions experienced a deterioration in the management of these ailments, consequently increasing their susceptibility to cardiovascular diseases.33
However, we found that new urgent diagnoses also decreased, such as stroke and acute myocardial infarction, among others.20,29 Likewise, it is noteworthy that several countries such as China, Italy, France, and the USA have reported a decrease in the provision of health care and in the diagnosis of new cases of stroke and acute myocardial infarction which reflects the trends observed in our study.34–37 In addition, the decrease in hospital emergency department utilization may be attributed to patient concern about possible SARS-CoV-2 contamination if transferred to the hospital.29
Regarding mortality rates we observed a decline in mortality following the lockdown, this drop may be attributed to several factors. A key factor is the implementation of public health measures, such as social distancing, face mask mandates, and hygiene protocols,18 which inadvertently reduced transmission not only of COVID-19 but also of other respiratory and infectious diseases that predominantly affect older adults. This decline in mortality rates is supported by national reports in the United Kingdom, which confirm significant reductions in non-COVID-19 mortality rates, especially notable in cases of influenza/pneumonia (48%) and chronic lung disease (25%).38 Xiao et al highlighted a significant reduction in the incidence and mortality rates of non-SRAS-CoV-2 diseases, such as injuries, non-SRS-CoV-2 pneumonia, chronic respiratory conditions, and cardiovascular disease, along with a decrease in the utilization of health services typically associated with these conditions.39 However, it should be considered that another study reported increased morbidity and mortality among people with chronic diseases.20 These divergent findings underscore the complexity of the impact of the pandemic on health care outcomes and highlight the need for further research into the underlying factors contributing to these disparities. Also, it is important to consider the delicate balance between implementing highly restrictive preventive measures and the need for population-based educational initiatives focused on disease prevention.
However, it is important to add that several governments around the world implemented restrictive measures to avoid saturation of their healthcare systems, focusing on hospital care and closing health centers to the general population.30,40 As a result, during the pandemic there was an extensive decline in the use of PHC services, as observed in our study, similar results were described in a different report.41 This lapse in follow-up potentially contributed to exacerbation of chronic disease, requiring hospital admissions after the shutdown. In addition, the decrease in mortality rates could also be associated with diagnostic and therapeutic delays in severe and emergent cases.20,42
Furthermore, our study shows the evolution of health care utilization patterns among the older adults. We observed a reduction in the number of consultations with nurses, general practitioners, and specialist physicians after the lockdown, with the most significant decrease occurring in consultations with general practitioners, particularly in the six to twelve months after the state of emergency. A study entitled “The impact of the COVID-19 pandemic on health services utilization in China” revealed that almost all health services utilization parameters (Hospital, PHC and other health facility) had not returned to pre-pandemic levels by June 2020. These persistent reductions and impasses in preventive and therapeutic health care are expected to have substantial secondary consequences on the overall health of the population.15 We also need to consider the suitability and adequacy of the population’s use of healthcare services. On the other hand, we observed an increase in the number of admissions and length of hospital stay in the six to twelve months after lockdown compared to the previous six months. This observation suggests that while outpatient care decreased, there was a rise in demand for inpatient services, possibly due to a delay in seeking care or exacerbation of chronic conditions.15
The pandemic has had far-reaching effects, extending beyond the realm of medical services, and has been regarded as a personal, social, and economic crisis.15,43 Our findings indicate a surge in visits from social workers, as numerous patients grappled with clinical consequences and secondary complications arising from the infection. Additionally, there was a decline in social services, including communal activities and meal services, along with the closure of senior day care centers. Amid these challenges, social workers played a pivotal role in emphasizing the significance of acknowledging contact networks, as the situation has resulted in pronounced social isolation.29
Our study revealed a significant drop in medication use. Spanish records indicate that during the initial pandemic wave, 80% of people had difficulty obtaining their usual drug treatments. Several factors contributed to this lowering, including concerns about virus transmission (9.3%), expired electronic prescriptions (7%), and physical barriers that prevented pharmacy visits (4.3%).44 In addition, one report indicated that prescriptions for chronic medications remained relatively stable, while those for acute medications declined during the COVID-19 waves and associated closures. This reduction coincided with a decline in acute reporting, excluding COVID-19 cases.19
Our study has some limitations. In the first instance, the large sample size included in this analysis means that small variations no matter how insignificant they may be are statistically significant. It is important to recognize that statistical significance does not inherently imply clinical significance. Therefore, it is necessary to be careful when interpreting the results, observing the data obtained within the logic and clinical relevance that can be derived from these results. Secondly, is a retrospective study, there is a possibility of encountering limitations related to missing data or inaccuracies within the BIGAN database. The retrospective nature of the study relies on pre-existing data, and any gaps or errors present in the database could impact the comprehensiveness and accuracy of the findings. Thirdly, our research carried out a longitudinal follow-up of up to one year, but a longer-term study is needed since, due to the saturation of primary care consultations or the fear of contagion from chronically ill patients, these new diagnoses, and consequences a posteriori. Fourthly, it is important to take into account that the data are collected from the electronic record from primary care, so it is possible that the records made from the emergency room or hospital may not have been collected with the same diagnostic labeling system as from primary care. Lastly, this study did not include self- reported data on lifestyle habits and self-perceived control of symptoms maintained by the study population during the months of lockdown.
Conclusion
Our study highlights a significant decline in the diagnosis of new chronic diseases as well as a persistent reduction in health service utilization and medication consumption among older adults with pre-existing chronic conditions who remained uninfected with COVID-19. This drop in healthcare use persisted even after the lifting of lockdown measures. Most remarkably, many healthcare utilization metrics have yet to return to their pre-pandemic levels, emphasizing the enduring impact of the crisis on healthcare delivery for this vulnerable demographic, even a year after the pandemic’s onset.
To better address the consequences of potential future pandemics, it is vital that further research identify the vulnerable patient groups and disease-specific healthcare services most affected by the pandemic.
Declaration of Generative AI in Scientific Writing
During the preparation of this work the author used (Chat GPT, DeepL Write) to improve readability and language. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Acknowledgments
The authors would like to thank the Aragonese Primary Care Research Group (GAIAP, B21_23R) that is part of the Department of Innovation, Research and University at the Government of Aragón (Spain) and the Institute for Health Research Aragón (IIS Aragón); the Research Network on Chronicity, Primary Care and Health Promotion (RICAPPS, ~RD21/0016/0005) that is part of the Results-Oriented Cooperative Research Networks in Health (RICORS) (Carlos III Health Institute); Feder Funds~ “Another way to make Europe”, NextGenerationEU funds and the University of Zaragoza.
Funding
This work was supported by Aragonese Primary Care Research Group (GAIAP, B21_23R), which is part of the Department of Science, Universities and the Knowledge Society of the Government of Aragón (Spain), Feder funds “Another way to make Europe” and the Department for Science, Universities and the Knowledge Society of the Government of Aragon (Spain), through the DGACovid-01 project. The funders have no role in study design, data collection and analysis, publication decision or manuscript preparation.
Disclosure
The authors report no conflicts of interest in this work.
References
1. INE. Proyecciones de Población 2018 Instituto Nacional de Estadística; 2018.
2. Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35(1):75–83. doi:10.1093/epirev/mxs009
3. Souza DLB, Oliveras-Fabregas A, Minobes-Molina E, de Camargo Cancela M, Galbany-Estragués P, Jerez-Roig J. Trends of multimorbidity in 15 European countries: a population-based study in community-dwelling adults aged 50 and over. BMC Public Health. 2021;21(1). doi:10.1186/s12889-020-10084-x
4. Harrison C, Britt H, Miller G, Henderson J. Examining different measures of multimorbidity, using a large prospective cross-sectional study in Australian general practice. BMJ Open. 2014;4(7):4694. doi:10.1136/bmjopen-2013
5. Prados-Torres A, Poblador-Plou B, Calderón-Larrañaga A, et al. Multimorbidity patterns in primary care: interactions among chronic diseases using factor analysis. PLoS One. 2012;7(2):e32190. doi:10.1371/journal.pone.0032190
6. Moore KL, Patel K, John Boscardin W, Steinman MA, Ritchie C, Schwartz JB. Medication burden attributable to chronic comorbid conditions in the very old and vulnerable. PLoS One. 2018;13(4):1–14. doi:10.1371/journal.pone.0196109
7. Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–439. doi:10.1016/j.arr.2011.03.003
8. Glynn LG, Valderas JM, Healy P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract. 2011;28(5):516–523. doi:10.1093/fampra/cmr013
9. Kirchberger I, Meisinger C, Heier M, et al. Patterns of multimorbidity in the aged population. results from the KORA-age study. PLoS One. 2012;7(1):e30556. doi:10.1371/journal.pone.0030556
10. Prados-Torres A, Del Cura-González I, Prados-Torres JD, et al. Multimorbilidad en medicina de familia y los principios Ariadne. Un enfoque centrado en la persona[Multimorbidity in general practice and the Ariadne principles. A person-centred approach]. Aten Primaria. 2017;49(5):300–307. doi:10.1016/j.aprim.2016.11.013
11. Van Ancum JM, Jonkman NH, Van Schoor NM, et al. Predictors of metabolic syndrome in community-dwelling older adults. PLoS One. 2018;13(10):1–12. doi:10.1371/journal.pone.0206424
12. World Health Organization. Pulse Survey on Continuity of Essential Health Services During the COVID-19 Pandemic. Genva: World Health Organization; 2020.
13. Kim E, Kojima N, Vangala S, et al. Impact of COVID-19 on primary care quality measures in an academic integrated health system. J Gen Intern Med. 2022;37(5):1161–1168. doi:10.1007/s11606-021-07193-7
14. Prieto Rodríguez MÁ, March Cerdá JC, Martín Barato A, Escudero Carretero M, López Doblas M, Luque Martín N. Consequences of the COVID-19 lockdown in patients with chronic diseases in Andalusia. Gac Sanit. 2022;36(2):139–145. doi:10.1016/j.gaceta.2020.11.001
15. Xiao H, Dai X, Wagenaar BH, et al. The impact of the COVID-19 pandemic on health services utilization in China: time-series analyses for 2016–2020. Lancet Reg Health West Pac. 2021;9. doi:10.1016/j.lanwpc.2021.100122
16. Balanzá-Martínez V, Kapczinski F, de Azevedo Cardoso T, et al. The assessment of lifestyle changes during the COVID-19 pandemic using a multidimensional scale. Rev Psiquiatr Salud Ment. 2021;14(1):16–26. doi:10.1016/j.rpsm.2020.07.003
17. Li J, Fong DYT, Lok KYW, et al. Global impacts of COVID-19 on lifestyles and health and preparation preferences: an international survey of 30 countries. J Glob Health. 2023;13:06031. doi:10.7189/jogh.13.06031
18. Shivalkar S, Pingali MS, Verma A, et al. Outbreak of COVID-19: a detailed overview and its consequences. In: Coronavirus Therapeutics–Volume II: Clinical Management and Public Health. Springer; 2021:23–45. doi:10.1007/978-3-030-85113-2_2
19. Van den Bulck S, Crèvecoeur J, Aertgeerts B, et al. The impact of the Covid-19 pandemic on the incidence of diseases and the provision of primary care: a registry-based study. PLoS One. 2022;17(7):e0271049. doi:10.1371/journal.pone.0271049
20. Del Cura-González I, Polentinos-Castro E, Fontán-Vela M, López-Rodríguez JA, Martín-Fernández J. What have we missed because of COVID-19? Missed diagnoses and delayed follow-ups. SESPAS Report 2022. Gac Sanit. 2022;36:S36–S43. doi:10.1016/j.gaceta.2022.03.003
21. Instituto Aragonés de Estadísitica. Cifras de población y proyecciones de población[Population figures and population projections]; 2022. Available from: https://www.aragon.es/-/estimaciones-y-proyecciones-de-poblacion.
22. Gobierno de Aragón. Salud y Sanidad|Transparencia Aragón[Health and Sanitation|Transparency Aragón]. Available from: https://transparencia.aragon.es/content/salud-y-sanidad.
23. Calderón-Larrañaga A, Vetrano DL, Onder G, et al. Assessing and measuring chronic multimorbidity in the older population: a proposal for its operationalization. J Gerontol a Biol Sci Med Sci. 2017;72(10):1417–1423. doi:10.1093/gerona/glw233
24. Comité Internacional de Clasificación de la WONCA. Clasificación Internacional de la Atención Primaria: CIAP-2[International Classification of Primary Care: CIAP-2]. Barcelona: Masson; 1999.
25. Sisó-Almirall A, Kostov B, Sánchez E, Benavent-àreu J, González-De Paz L. Impact of the COVID-19 pandemic on primary health care disease incidence rates: 2017 to 2020. Ann Fam Med. 2022;20(1):63–68. doi:10.1370/afm.2731
26. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: a systematic review and meta-analysis. Inter J Infect Dis. 2020;94:91–95. doi:10.1016/j.ijid.2020.03.017
27. Koyyada R, Nagalla B, Tummala A, et al. Prevalence and impact of preexisting comorbidities on overall clinical outcomes of hospitalized COVID-19 patients. Biomed Res Int. 2022;2022:1–12. doi:10.1155/2022/2349890
28. Chudasama YV, Gillies CL, Zaccardi F, et al. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metabol Syndr. 2020;14(5):965–967. doi:10.1016/j.dsx.2020.06.042
29. Vuilleumier S, Spichiger T, Dénéréaz S, Fiorentino A. Not only COVID-19 disease impacts ambulance emergency demands but also lockdowns and quarantines. BMC Emerg Med. 2023;23(1). doi:10.1186/s12873-023-00772-3
30. Coma E, Mora N, Méndez L, et al. Primary care in the time of COVID-19: monitoring the effect of the pandemic and the lockdown measures on 34 quality of care indicators calculated for 288 primary care practices covering about 6 million people in Catalonia. BMC Fam Pract. 2020;21(1). doi:10.1186/s12875-020-01278-8
31. Barrio-Cortes J, Castaño-Reguillo A, Beca-Martínez MT, Bandeira-de Oliveira M, López-Rodríguez C, Jaime-Sisó MÁ. Chronic diseases in the geriatric population: morbidity and use of primary care services according to risk level. BMC Geriatr. 2021;21(1). doi:10.1186/s12877-021-02217-7
32. Ajebli M, Amssayef A, Akdad M, et al. Chronic Diseases and COVID-19: a Review. Endocr Metab Immune Disord Drug Targets. 2021;21(10):1781–1803. doi:10.2174/1871530320666201201110148
33. Ghosal S, Sinha B, Majumder M, Misra A. Estimation of effects of nationwide lockdown for containing coronavirus infection on worsening of glycosylated haemoglobin and increase in diabetes-related complications: a simulation model using multivariate regression analysis. Diabetes Metabol Syndr. 2020;14(4):319–323. doi:10.1016/j.dsx.2020.03.014
34. Rudilosso S, Laredo C, Vera V, et al. Acute Stroke Care Is at Risk in the Era of COVID-19. Stroke. 2020;51(7):1991–1995. doi:10.1161/STROKEAHA.120.030329
35. Aguiar de Sousa D, Sandset EC, Elkind MSV. The Curious Case of the Missing Strokes During the COVID-19 Pandemic. Stroke. 2020;51(7):1921–1923. doi:10.1161/STROKEAHA.120.030792
36. Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 Epidemic on Stroke Care and Potential Solutions. Stroke. 2020;51(7):1996–2001. doi:10.1161/STROKEAHA.120.030225
37. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral Effect of Covid-19 on Stroke Evaluation in the United States. N Engl J Med. 2020;383(4):400–401. doi:10.1056/NEJMc2014816
38. Brett G, Barton F, Smith R; Office for National Statistics UK. Monthly mortality analysis, England and Wales: 2023; 2023. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/monthlymortalityanalysisenglandandwales/july2023.
39. Qi J, Zhang D, Zhang X, et al. Do lockdowns bring about additional mortality benefits or costs? Evidence based on death records from 300 million Chinese people. medRxiv. 2020. doi:10.1101/2020.08.28.20183699
40. Iparraguirre ST, Álvarez RM. La semFYC y la Medicina de Familia en tiempos del Coronavirus[semFYC and Family Medicine in times of Coronavirus]. Aten Primaria. 2020;52(5):291–293. doi:10.1016/j.aprim.2020.04.002
41. Thornton J. Covid-19: a&E visits in England fall by 25% in week after lockdown. BMJ. 2020;m1401. doi:10.1136/bmj.m1401
42. Martinez CB, Badia JG, Roca JM. What about primary care during the pandemic? Aten Primaria. 2020;52(9):598–599. doi:10.1016/j.aprim.2020.10.001
43. Modesti PA, Wang J, Damasceno A, et al. Indirect implications of COVID-19 prevention strategies on non-communicable diseases. BMC Med. 2020;18(1). doi:10.1186/s12916-020-01723-6
44. Nephila Health Partnership. Estudio del impacto de Covid-19 en las personas con enfermedad crónica[Study of the impact of Covid-19 on people with chronic illness]. Madrid: Plataforma de Organizaciones de Pacientes; 2020.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
