Back to Journals » Journal of Blood Medicine » Volume 15
Immuno-Hematological and Biochemical Changes in Patients with Tuberculosis in Dessie Comprehensive Specialized Hospital, Dessie, Ethiopia
Authors Gebreweld A , Fiseha T , Kebede E , Tamir Z , Gebremariam B , Miruts F , Haileslasie H
Received 28 November 2023
Accepted for publication 16 March 2024
Published 22 March 2024 Volume 2024:15 Pages 147—155
DOI https://doi.org/10.2147/JBM.S445857
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Angesom Gebreweld,1 Temesgen Fiseha,2 Edosa Kebede,3 Zemenu Tamir,4 Brhane Gebremariam,5 Fikadu Miruts,1 Haftay Haileslasie1
1Department of Medical Laboratory Sciences, College of Health Science, Mekelle University, Mekelle, Ethiopia; 2Department of Medical Laboratory Science, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia; 3Department of Medical Laboratory Science, College of Medicine and Health Science, Ambo University, Ambo, Ethiopia; 4Department of Medical Laboratory Sciences, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 5Department of Medical Laboratory Sciences, College of Health Sciences, Aksum University, Aksum, Ethiopia
Correspondence: Angesom Gebreweld, Email [email protected]
Background: Tuberculosis (TB) is a serious worldwide health issue, particularly in developing nations like Ethiopia. Patients with tuberculosis experience a range of hematological, immunological, and biochemical alterations. The purpose of this study was to evaluate immunological, hematological, and biochemical alterations of newly diagnosed TB patients at Dessie comprehensive specialized hospital, Dessie, Ethiopia.
Methods: A comparative, cross-sectional study was carried out to evaluate the immuno-hematological and biochemical changes in patients with tuberculosis at Dessie comprehensive specialized hospital from January to July 2018. One hundred sixty-four (164) newly diagnosed TB patients, and 80 apparently healthy controls were included consecutively. The variables were expressed in frequency, percentage, and mean ± SD. To compare mean ± SD of the groups or within the groups, we used an independent sample t-test. Statistical significance was defined as a P value less than 0.05.
Results: Male TB patients had significantly high mean absolute WBC count, neutrophil count, lymphocyte, platelet count, and systemic immune-inflammation compared with male healthy controls (P=0.001, P=0.011 P=0.021, P=0.001, and P=0.018, respectively). The mean platelet count of female TB patients was significantly higher than that of the female control group (P=0.015). However, mean RBC counts, Hgb, HCT, and MPV of TB patients were significantly lower than those of male (p< 0.001) and female healthy controls (P=0.022, 0.015, and 0.001, respectively). The TB patients had developed anemia (23.8%), WBC abnormalities (29.3%), thrombocytosis (11.6%), and thrombocytopenia (9.8%). The cases had significantly higher mean alanine amino transferase, total bilirubin, and glucose level, but the mean total protein, alkaline phosphatase, and total cholesterol of cases were significantly lower than healthy control groups.
Conclusion: TB patients in this study showed significant alterations in a number of hematological and biochemical profiles. This indicates that hematological and biochemical profiles should be monitored and properly interpreted for the differential diagnosis of tuberculosis and evaluation of response to treatment.
Keywords: tuberculosis, pulmonary tuberculosis, immunological markers, hematological parameter, lipid profile, biochemical change
Introduction
Mycobacterium tuberculosis (Mtb) is the causative agent of an infectious disease Tuberculosis (TB). It mostly affects the lower respiratory system (pulmonary TB) and is characterized by a chronic productive cough, low-grade fever, night sweats, and weight loss, but can affect other sites as well, which is called extra pulmonary TB.1
TB continues to be a critical health issue globally. It affects millions of people annually and is one of the top causes of mortality along with human immunodeficiency virus (HIV). In 2021, about 10.6 million new TB cases emerged, and 1.6 million lives were lost. With an estimated TB incidence rate of 126 per 100,000 people per year, Ethiopia stands as the world’s 10th most TB-affected nations.2
Mtb primarily invades macrophages, key players in immunity, creating a conducive environment for itself. The host’s defense against Mtb relies significantly on T cell-driven responses. Various CD4 T cell types, including Th1, Th2, Th17, and regulatory T cells (Tregs), work together or interfere one another to manage the disease.3,4
The protective role of the Mtb specific CD4 Th1 cell response is underscored by its capacity to produce cytokines, notably interferon gamma (IFN-γ) and tumor necrosis factor alpha (TNF-α). These cytokines are crucial for attracting and activating innate immune cells, including monocytes, macrophages, and granulocytes. Individuals with deficiencies in IFN-γ and interleukin-12 (IL-12; which promotes TH1 cell differentiation) were highly vulnerable to tuberculosis. Additionally, the link between reduced CD4 T cell numbers and increased tuberculosis risk in HIV-positive individuals highlights the role of these cells in defense. Tuberculosis can also result in reduced CD4 and CD8 lymphocyte levels in patients who are not HIV-positive.3–5
Normally, the CD8+ T cell reaction to Mtb is not as strong as that of CD4+ T cells. Nevertheless, CD8+ T cells have the ability to influence the function of phagocytes and release substances like granulysin, which can kill mycobacteria. Moreover, cytokines beyond IFN, such as TNF, play a pivotal role in forming granulomas, structured clusters of immune cells that control the pathogen.4
Cholesterol may play a significant role in the cellular immune response. A diet high in cholesterol can increase the sterilization of sputum culture in those suffering from pulmonary tuberculosis (PTB), while insufficient cholesterol levels could negatively impact the function of lymphocytes and macrophages, potentially worsening tuberculosis. Moreover, reduced total cholesterol, HDL, and LDL levels have been observed in individuals with PTB. The degree of smear positivity in PTB patients also exhibits a notable link with serum lipid levels, highlighting its utility in evaluating lipid dyslipidemia in these patients.6–8
Tuberculosis primarily targets the lungs but can also severely impact the hematopoietic system. It causes a range of hematological abnormalities such as elevated ESR, anemia, and increased lymphocytes and platelet counts.9,10
Studies have evidenced a significant association between the presence of acid-fast bacilli in sputum and the occurrence of hematological and biochemical alterations in patients with TB. A deeper comprehension of the immune response to mycobacterial infections has provided insight on the association with blood irregularities. Indicators such as immunological markers, hematological abnormalities, and biochemical alterations may aid physicians in the diagnosis of TB.8,11 However, there is a scarcity of information regarding these indicators in TB patients in our country Ethiopia. To address this gap, this study was conducted to investigate the immunological, hematological, and biochemical alterations of newly diagnosed patients with tuberculosis at Dessie comprehensive specialized hospital in Dessie, Ethiopia.
Methods and Materials
Study Design, Setting, and Population
A comparative, cross-sectional study was carried out to evaluate the immuno-hematological and biochemical alterations between patients with tuberculosis and healthy controls at Dessie comprehensive specialized hospital from January to July 2018. The hospital is located in Dessie town, South Wollo zone of Amhara Regional State, in north-eastern Ethiopia. It is 401 km far from Addis Ababa, the capital city. It serves as a referral hospital for people living in Wollo zones and neighbouring regions.
One hundred and sixty-four newly diagnosed TB patients and 80 apparently healthy controls were included in the study consecutively. The sample size was calculated by taking the following considerations: Power = 80%, Confidence interval = 95%, Ratio = 2:1, Mean ± SD of White blood cells (WBC) for case = 8.48 ± 3.09, and Mean± SD of White blood cells for control = 6.75 ± 1.83. The Mean ± SD of WBCs is taken from a study conducted in Jimma.12
Individuals on anti-TB therapy, younger than 18 years, pregnant women, HIV-positive persons, and those with a chronic illness history, such as hepatitis, diabetes, or renal disease, were not included in the research.
Data Collection Procedure
Trained clinical nurses gathered socio-demographic and clinical data from the study participants through a pretested questionnaire and reviewing medical records.
To perform the complete blood count (CBC), CD4 count determination, and clinical chemistry analysis, about six milliliters of venous blood specimen was collected from each participant (both TB patients and apparently healthy controls) into a di potassium EDTA anticoagulant tube and plain tube, 3 mL each. Sysmex KX-21N automated hematological analyzer (Sysmex corporation Kobe, Japan) was utilized to determine complete blood counts. CD4 T cell count of the study participants was determined using BD FACS count analyzer (Becton Dickinson and Company, California, USA), and Dirui CS T240 auto-analyzer (Dirui Industrial Company) was used to perform biochemical analysis.
To produce quality laboratory results, all manufacturer instructions and standard operating procedures were closely adhered to in every test procedure. To ensure the instruments’ precision and the results’ accuracy, quality control substances were tested alongside the patient specimens, and reagent expiration dates were verified.
According to the World Health Organization guidelines, anemia was identified by hemoglobin (Hgb) levels: less than 13 g/dl for males aged 15 and older and less than 12 g/dl for non-pregnant women. Anemia is categorized as mild, moderate, and severe depending on its severity. Mild anemia is defined as having Hgb concentrations ranging from 11.0 to 12.9 g/dl for men and from 11.0 to 11.9 g/dl for non-pregnant women. Moderate anemia is defined as hemoglobin level between 8.0 and 10.9 g/dl and severe anemia diagnosed when Hgb fell below 8.0 g/dl for both sexes.13
Total WBC > 10.6 × 103/μL and WBC < 3.6 × 103/μL were used to define leukocytosis and leukopenia, respectively. On the other hand, total platelet count > 450 × 103/μL and platelet count < 150 × 103/μL were used to define thrombocytosis and thrombocytopenia, respectively.14
The absolute counts of neutrophils, lymphocytes, monocytes, and platelets were used to calculate neutrophil-to-lymphocyte (NLR), platelet-to-lymphocyte (PLR), monocyte-to-lymphocyte (MLR) ratios and systemic immune-inflammation index (SII) using the following equations: NLR = Neutrophils/Lymphocytes, MLR = Monocytes/Lymphocytes, PLR = Platelets/Lymphocytes, and SII = Platelets × Neutrophils/Lymphocytes.
Data Analysis
Data from the laboratory investigation and questionnaire were entered in to “EpiInfo version 3.1” and then exported to the statistical analysis program SPSS version 20.0 (Statistical Package for the Social Science). The Kolmogorov–Smirnov and Shapiro–Wilk tests were performed to check the normality distribution of continuous variables. Percentages and frequencies were used to report categorical variables, and mean ± standard deviation (SD) was used to express continuous variables. To compare mean ± SD of the groups or within the groups, we used Student’s t-test (independent sample t-test). Statistical significance was defined as a P value less than 0.05.
Ethical Consideration
Ethical Review Board of College of Medicine and Health Science, Wollo University approved the study. The study was conducted according to the principles stated in the Declaration of Helsinki. All the study subjects (cases and controls) were 18 years and above and briefed about the study’s objective and included after obtaining written consent. Participants’ data was coded to maintain confidentiality, and attending doctors were informed of any unusual findings.
Result
Socio-Demographic Characteristics of the Study Participants
In this study, 80 healthy controls and 164 newly diagnosed TB patients were included. There were 93 (56.7%) males and 71 (43.3%) females among the cases, and 43 (53.8%) males and 37 (46.2%) females among the health controls. The sex distribution between TB patients and healthy controls did not differ statistically significantly (p=0.765). Majority of the TB patients were aged between 25 and 34 years 57 (34.8%), had no formal education 70 (42.7), were married 117 (71.3%), and had pulmonary type of tuberculosis 139 (84.8%) (Table 1).
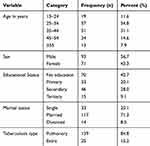 |
Table 1 Distribution of Age, Sex, Educational Status, Marital Status, Tuberculosis Type, and HIV Status of Newly Diagnosed TB Patients at Dessie Referral Hospital, Dessie, Ethiopia (n=164) |
Immuno-Hematological Characteristics Between Healthy Controls and Newly Diagnosed Tuberculosis Patients
Although the average CD4 count of patients with pulmonary TB (565.04 ± 325.49) was lower than that with extra TB (672.88 ± 292.73), the difference was not statistically significant (P=0.124).
Male TB patients had significantly increased average absolute WBC count (7.79 ±3.71 × 103 cells/µL), neutrophil count (4.08 ± 2.74 × 103 cells/µL), lymphocyte (2.83 ±1.90 × 103 cells/µL), platelet count (320.66 ±156.58 × 103 cells/µL), and systemic immune-inflammation (SII) (702.85 ± 1382.55) compared with male healthy control’s mean absolute WBC count (6.05 ± 1.99 × 103 cells/µL; P=0.001), neutrophil count (3.08 ±1.74 × 103 cells/µL; P=0.011), lymphocyte count (2.31 ± 0.65 × 103 cells/µL; P=0.021), platelet count (236.21 ± 59.73 × 103 cells/µL; P=0.001), and systemic immune-inflammation (SII) (345.49 ± 251.40, P=0.018). Compared with female healthy controls, female TB patients had elevated average absolute WBC count, neutrophil count, lymphocyte count, and SII, but the difference was not statistically significant (P=0.139, 0.673, 0.092, and 0.748 respectively). The average platelet count of female TB patients was significantly higher than the female control group (P=0.015) (Table 2).
 |
Table 2 Comparison of Average Values of Hematological Parameters in Healthy Controls and Newly Diagnosed TB Patients |
Mean RBC counts, Hgb, and HCT of TB patients were significantly lower than those male (p<0.001) and female healthy controls (P=0.022, 0.015, and 0.001 respectively). Red cell distribution width (RDW) was significantly higher in female TB patients than female controls (p<0.001). Mean platelet volume (MPV) was significantly decreased in patients with tuberculosis compared to controls (p=0.001) (Table 2).
Hematological Abnormalities of TB Patients
Of the TB patients, about 23.8% (39) had anemia. Mild, moderate, and severe anemia were present in 79.5%, 17.94%, and 2.56% of the anemic patients, respectively. Normocytic anemia 20 (51.3%) was the most prevalent type of anemia, followed by microcytic anemia 18 (46.2%). The prevalence of anemia was higher in pulmonary TB patients 24.5% (34) than extra pulmonary TB patients 20.0% (5) (Table 3).
 |
Table 3 Hematological Abnormalities of TB Patients |
WBC abnormalities were present in 29.3% (48) TB patients: 19.5% (32) of the TB patients had leukocytosis and 9.8% (16) had leukopenia. Neutrophilia, neutropenia, lymphocytosis, lymphocytopenia, monocytosis, and monocytopenia were present in 12.2% (20), 15.2% (25), 23.2% (38), 3 0.0% (5), 7.9% (13), and 14.0% (23) of the patients, respectively (Table 3).
The prevalence of thrombocytosis and thrombocytopenia among the TB patients were 11.6% (19) and 9.8% (16), respectively (Table 3).
Biochemical Parameters
TB patients had significantly high mean Alanine amino transferase (30.70 ± 29.17), total bilirubin (0.839 ± 1.10), and glucose level (119.14 ±59.91) compared with healthy control’s mean Alanine amino transferase (24.91 ± 10.77, P=0.026), total bilirubin (0.538 ±.39, P=0.010), and glucose level (101.35 ± 52.35, P=0.039). However, the mean total protein (6.37 ± 1.26), Alkaline phosphatase (166.23 ±118.49), and total cholesterol (159.56 ±45.43) of TB patients were significantly lower than healthy control’s mean total protein (7.36 ±.61, P<0.001), Alkaline phosphatase (215.34 ± 101.35; P=0.002), and total cholesterol (192.95 ± 61.996; P=0.002) (Table 4).
 |
Table 4 Comparison of Mean Values of Biochemical Parameters in the Newly Diagnosed TB Patients versus Healthy Control |
Discussion
Tuberculosis remains a significant global infectious disease and a primary health concern in Ethiopia. It causes a range of hematological, immunological, and biochemical alterations.2,8,11 The objective of the study presented here was to investigate these changes in newly diagnosed tuberculosis patients at Dessie comprehensive specialized hospital in Dessie, Ethiopia.
This study showed that Male with tuberculosis exhibited significantly elevated average levels of white blood cells, neutrophils, and lymphocytes in comparison to healthy male subjects. This result aligns with previous research from South Eastern Nigeria,15 Saudi Arabia,16 and Pakistan.12 The immune system reaction to tuberculosis may be the cause of the rise in WBC count, neutrophil count, and lymphocyte count in TB patients. Neutrophilia is a sign of repeated continuous inflammatory reaction and this frequently transforms into lymphocytosis when the inflammatory response becomes chronic. However, our finding contradicts with another study in Kirkuk city.17
The average number of platelets in both male and female patients with tuberculosis was significantly elevated compared to the control group, and this is consistent with studies conducted in Iraq,18 Kirkuk city,17 Sudan,19 South Eastern Nigeria,15 Guyana,20 and Jimma University.12 These findings could be explained by reactive thrombocytosis, which can occur in a variety of clinical conditions including infections like pulmonary TB. Platelets, as key players in inflammation and immune responses, release pro-inflammatory cytokines such as IL-6 and TNF, which promote the synthesis of acute-phase proteins and thrombocytosis.21,22
The present study indicated that average RBC counts, Hgb level, and HCT of TB patients were considerably lower than the healthy controls group, for both sex. This agrees with Al-muhammadi et al,18 Amilo et al,15 Al-Omar et al,16 and Jimma.12 Reduced red blood cell life span, impaired marrow response, or poor iron transport from macrophages to the plasma in iron cycle metabolism, and chronic inflammatory disorder could be the cause of the decline in RBC number, Hgb, and HCT in TB patients.23
In this study, anemia had developed in around 23.8% (39) of the TB patients. It was more common in patient with pulmonary TB (24.5%) than in extra pulmonary TB (20.0%). There was mild-type anemia in the majority of the anemic patients. This finding is in line with a research done at St. Paul’s Hospital Millennium Medical College (25%).24 However, the prevalence of anemia is lower than other studies conducted in Jimma (37%),12 Gondar (46%),25 and India (77.3%).26 Study participants’ dietary habits, malabsorption syndrome, and the disease stage at diagnosis could be the contributing factors to the observed disparities. The most common type of anemia was normocytic anemia 20 (51.3%) followed by microcytic anemia 18 (46.2%) which is similar with studies conducted in Jimma University Specialized Hospital12 and Seoul National University Hospital.27
The mean total cholesterol of the TB patients in this study was considerably lower than that of the healthy controls group. Reports from Casimir et al,28 Taparia et al,8 and Șahin and Yildiz29 showed similar outcomes. A low cholesterol level makes one more vulnerable to different diseases like TB. A diet high in cholesterol has been found to hasten the process of bacteriologic sterilization in tuberculosis patients.6,30 Total proteins were also significantly lower in patients with TB than in the healthy control group, which is similar to studies conducted by Șahin and Yildiz29 and Modawe et al,31 but the difference was not significant.
The mean Alanine amino transferase was significantly higher in TB patients than in the healthy control group, and this is consistent with the research done in Guyana.20 However, the finding contradicted with the finding of Modawe et al on Biochemical Parameters in Relation to Tuberculosis in Sudanese Patients, which showed significantly lower alanine amino transferase in TB patients.31
The current study showed that TB patients had significantly higher glucose level than the control group, which is in line with the findings of a study by Bailey and Grant.32 However, Kurup et al stated that blood sugar level did not show any variation between TB patients and the healthy control group.20
In conclusion, patients with tuberculosis had significantly higher mean absolute count of WBC, neutrophils, lymphocytes, and platelets compared to healthy controls. However, mean RBC counts, Hgb, HCT, and MPV of TB patients were significantly lower compared to healthy controls. TB patients had significantly higher mean Alanine amino transferase, total bilirubin, and glucose levels, but the mean total protein, alkaline phosphatase, and total cholesterol of TB patients were significantly lower than healthy control groups. TB has a significant impact on hematological and biochemical profiles. Therefore, the patients infected with TB should have their hematological and biochemical parameters monitored and properly interpreted for the differential diagnosis of tuberculosis and evaluation of response to treatment. Additionally, more studies should be conducted on TB and its effect on biochemical and hematological values in humans in the study area or other areas in the country.
Abbreviations
C, Cholesterol; CBC, Complete blood count; ESR, Erythrocyte Sedimentation Rate; Hgb, Hemoglobin; HIV, Human immunodeficiency virus; IFN-γ, Interferon gamma; MPV, Mean platelet volume; Mtb, Mycobacterium tuberculosis; PTB, Pulmonary tuberculosis; RBC, Red blood cell; RDW, Red cell distribution width; TB, Tuberculosis; WBC, White blood Cell.
Data Sharing Statement
All relevant data are included in the document.
Acknowledgment
We express our gratitude to Wollo University for providing us the fund to carry out this study. We also thank the management and laboratory staff of Dessie comprehensive specialized hospital for their support and cooperation. The authors greatly appreciate each study participants for their collaboration and trust.
Author Contributions
All authors significantly contributed to the manuscript by participating in the ideation, study design, execution, data collection, analysis, and interpretation processes as well as in the writing, editing, and review of the article. All authors have agreed on the approval of the final manuscript to be published in the current journal and to be accountable for all aspects of the work.
Funding
Wollo University, www.wu.edu.et, provided financial assistance for this work. The responsibility of the university was closely monitoring and evaluating the research activity.
Disclosure
The authors state that they have no competing interests.
References
1. Davis CP, Niesel D, Woods G. Baron’s medical microbiology; 2000.
2. World Health Organization. Global tuberculosis report 2022. Geneva: World Health Organization; 2022. Available from: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022.
3. Prezzemolo T, Guggino G, La Manna MP, Di Liberto D, Dieli F, Caccamo N. Functional signatures of human CD4 and CD8 T cell responses to Mycobacterium tuberculosis. Front Immunol. 2014;5:180. doi:10.3389/fimmu.2014.00180
4. Walzl G, Ronacher K, Hanekom W, Scriba TJ, Zumla A. Immunological biomarkers of tuberculosis. Nat Rev Immunol. 2011;11(5):343–354. doi:10.1038/nri2960
5. Al-Aska AI, Al-Anazi A, Al-Subaei S, et al. CD4+ T-lymphopenia in HIV negative tuberculous patients at King Khalid University Hospital in Riyadh, Saudi Arabia. Eur J Med Res. 2011;16(6):285–288. doi:10.1186/2047-783X-16-6-285
6. Pérez-Guzmán C, Vargas MH, Quiñonez F, Bazavilvazo N, Aguilar A, Team OS. A cholesterol-rich diet accelerates bacteriologic sterilization in pulmonary tuberculosis. Chest. 2005;127(2):643–651. doi:10.1378/chest.127.2.643
7. Deniz O, Gumus S, Yaman H, et al. Serum total cholesterol, HDL-C and LDL-C concentrations significantly correlate with the radiological extent of disease and the degree of smear positivity in patients with pulmonary tuberculosis. Clin Biochem. 2007;40(3–4):162–166. doi:10.1016/j.clinbiochem.2006.10.015
8. Taparia P, Yadav D, Koolwal S, Mishra S. Study of lipid profile in pulmonary tuberculosis patients and relapse cases in relation with disease severity-a pilot study. Indian J Sci Appl Res. 2015;2:41–50.
9. Singh K, Ahluwalia G, Sharma S, Saxena R, Chaudhary V, Anant M. Significance of haematological manifestations in patients with tuberculosis. J Associat Phys India. 2001;49(788):90–94.
10. Banerjee M, Chaudhary B, Shukla S. Hematological profile among pulmonary tuberculosis patients in tertiary care hospital. Int J Bioassays. 2015;4(5):3900–3902.
11. Morris CD, Bird AR, Nell H. The haematological and biochemical changes in severe pulmonary tuberculosis. QJM Int J Med. 1989;73(3):1151–1159.
12. Atomsa D, Abebe G, Sewunet T. Immunological markers and hematological parameters among newly diagnosed tuberculosis patients at Jimma University Specialized Hospital. Ethiop J Health Sci. 2014;24(4):311–318. doi:10.4314/ejhs.v24i4.6
13. World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. World Health Organization; 2011.
14. Keohane EM, Otto CN, Walenga JM. Rodak’s hematology-e-book: clinical principles and applications. Elsevier Health Sci. 2019;2019:1.
15. Amilo G, Meludu S, Ele P, Ezechukwu C, Onyenekwe C, Chukwu MI. Haematologic indices in pulmonary tuberculosis with or without HV Co-infection in South Eastern Nigeria. Adv Life Sci Technol. 2013;11:1–7.
16. Al-Omar I, Al-Ashban R, Shah A. Hematological abnormalities in Saudis suffering from pulmonary tuberculosis and their response to the treatment. Res J Pharma. 2009;3(4):78–85.
17. Shareef HA, Amin NRM. Abnormalities of hematological parameters in newly diagnosed pulmonary tuberculosis patients in Kirkuk city. J Babylon Univy Pure Appl Sci. 2012;20(5):1386–1392.
18. Al-muhammadi MO, Al-Shammery HG. Studying some hematological changes in patients with pulmonary tuberculosis in Babylon governorate. Med J Babylon. 2011;8(4):608–618.
19. Bashir AB, Abufatima AS, Mohamedani AA. Reactive thrombocytosis and erythrocyte sedimentation rate in patients with pulmonary tuberculosis. J Med Lab Diagn. 2014;5(3):29–34.
20. Kurup R, Flemming K, Daniram S, Marks-James S, Roberts Martin R. Hematological and biochemistry profile and risk factors associated with pulmonary tuberculosis patients in Guyana. Tuberculosis Res Treat. 2016;2016:1–6. doi:10.1155/2016/6983747
21. Ünsal E, Aksaray S, Köksal D, Şipit T. Potential role of interleukin 6 in reactive thrombocytosis and acute phase response in pulmonary tuberculosis. Postgrad Med J. 2005;81(959):604–607. doi:10.1136/pgmj.2004.030544
22. Trzeciak-Ryczek A, Tokarz-Deptula B, Deptula W. Platelets–an important element of the immune system. Polish J Vet Sci. 2013;16(2):407–413. doi:10.2478/pjvs-2013-0058
23. Devi U, Rao CM, Srivastava VK, Rath PK, Das BS. Effect of iron supplementation on mild to moderate anaemia in pulmonary tuberculosis. Br J Nutr. 2003;90(3):541–550. doi:10.1079/BJN2003936
24. Kahase D, Solomon A, Alemayehu M. Evaluation of peripheral blood parameters of pulmonary tuberculosis patients at St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia: comparative study. J Blood Med. 2020;Volume 11:115–121. doi:10.2147/JBM.S237317
25. Abay F, Yalew A, Shibabaw A, Enawgaw B. Hematological abnormalities of pulmonary tuberculosis patients with and without HIV at the University of Gondar Hospital, Northwest Ethiopia: a comparative cross-sectional study. Tuberculosis Res Treat. 2018;2018:1–6. doi:10.1155/2018/5740951
26. Sulochana S, Subhashini V, Srinivasan C. Pulmonary tuberculosis—a prospective analysis of hematological changes. Asian J Pharm Clin Res. 2018;11(4):169–172. doi:10.22159/ajpcr.2018.v11i4.23177
27. Lee SW, Kang YA, Yoon YS, et al. The prevalence and evolution of anemia associated with tuberculosis. J Korean Med Sci. 2006;21(6):1028–1032. doi:10.3346/jkms.2006.21.6.1028
28. Akpovi DC, Gbaguidi LHS, Anago E, et al. Tuberculosis treatment raises total cholesterol level and restores high density lipoprotein cholesterol (HDLC) in patients with pulmonary tuberculosis. Afr J Biotechnol. 2013;12(41):6019–6024. doi:10.5897/AJB2013.13073
29. Sahin F, Yıldız P. Clinical research Distinctive biochemical changes in pulmonary tuberculosis and pneumonia. Arch Med Sci. 2013;4(4):656–661. doi:10.5114/aoms.2013.34403
30. Heiniger H, Marshall J. Cholesterol synthesis in polyclonally activated cytotoxic lymphocytes and its requirement for differentiation and proliferation. Proc Natl Acad Sci. 1982;79(12):3823–3827. doi:10.1073/pnas.79.12.3823
31. Modawe G, Nail A, Hamad F, et al. Biochemical parameters in relation to tuberculosis in Sudanese patients. Sudan J Med Sci. 2014;9(3):177–181.
32. Bailey SL, Grant P. ‘The tubercular diabetic’: the impact of diabetes mellitus on tuberculosis and its threat to global tuberculosis control. Clin Med. 2011;11(4):344. doi:10.7861/clinmedicine.11-4-344
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
