Back to Journals » Advances in Medical Education and Practice » Volume 14
Impact of a Preclinical Medical Student Anesthesiology Elective on the Attitudes and Perceptions of Medical Students Regarding Anesthesiology
Authors Walsh KL , Yadav A , Cradeur M, Huang H, Lee D , Owusu-Dapaah H, Ji C, Kendall MC, Asher S
Received 28 June 2023
Accepted for publication 21 November 2023
Published 29 November 2023 Volume 2023:14 Pages 1347—1355
DOI https://doi.org/10.2147/AMEP.S427974
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Kendra L Walsh,1,2 Abhishek Yadav,3 Michael Cradeur,1 Henry Huang,3 Daniel Lee,3 Harry Owusu-Dapaah,3 Chao Ji,3 Mark C Kendall,1,3 Shyamal Asher1,3
1The Warren Alpert Medical School of Brown University, Providence, RI, 02903, USA; 2Pharmacy Services, Rhode Island Hospital, Providence, RI, 02903, USA; 3Department of Anesthesiology, Rhode Island Hospital, Providence, RI, 02903, USA
Correspondence: Shyamal Asher, The Warren Alpert Medical School of Brown University, 222 Richmond Street, Providence, RI, 02903, USA, Tel +1 401-527-4775, Email [email protected]
Purpose: First- and second-year medical students typically have limited exposure to the field of anesthesiology, yet recent match data shows growing interest in the specialty. Early, structured exposure to anesthesiology in the form of a preclinical elective may allow medical students to make more informed decisions on their specialty of choice.
Methods: The anesthesiology preclinical elective, BIOL 6704: “Anesthesia: Much More than Putting you to Sleep”, is a one-credit course taught at The Warren Alpert Medical School of Brown University. A survey consisting of fifteen questions assessing changes in attitudes, perceptions, and interest in anesthesiology was distributed to first- and second-year medical students before and after course participation. The results were analyzed using the Wilcoxon’s signed-rank test for paired samples.
Results: The biggest impact of the preclinical elective was observed in the students’ subjective understanding of key aspects of the practice of anesthesiology. Statistically significant improvement was seen in the understanding of airway management, anesthetic pharmacology, basics of ultrasound, vascular access, anesthesiology subspecialties, and an understanding of anesthesiology residency. Overall, results were limited by our small sample size.
Conclusion: Our elective allows medical students to explore anesthesiology early in their medical school career. After taking this course, students noted more familiarity with various topics in anesthesiology. Peer institutions lacking a similar course may consider using our experience to increase interest about the specialty of anesthesiology for future students.
Keywords: anesthesiology, medical education, preclinical curriculum, medical school electives, medical students
Introduction
First- and second-year medical students typically have limited exposure to the field of anesthesiology, contributing to decreased interest in the profession among early medical students as compared to graduates. It has also perpetuated misunderstandings of the roles played by anesthesiologists within the hospital setting.1 In fact, according to a 2020 Association of American Medical Colleges (AAMC) survey, almost 60% of graduating students who matched in anesthesiology had a different specialty preference at the start of medical school.2 This may suggest that early, structured exposure to anesthesiology may allow medical students to make more informed decisions on their specialty of choice.
Growing interest in the field of anesthesiology among graduating medical students is evident by increasing applicant numbers each year since 2016, along with the specialty being among the top five matches for all United States (US) medical graduates in 2023.3,4 The majority of US medical schools follow a two-phase curriculum of preclinical basic science and foundational medicine didactics followed by clerkships.5 Content is largely taught in the context of organ systems generally following trends of medical specialties such as cardiology, neurology, and gastroenterology.6 This model, while a useful framework, leaves little room for anesthesiology, despite the field’s many intersections with multiple organ systems and disease states. Consequently, practicing anesthesiologists seldom provide direct classroom instruction, as other specialties have more “ownership” over certain topics.7–9 A similar pattern has been observed in Canadian medical schools, where one estimate of median teaching hours from anesthesiologists was approximately 2 hours of the total didactic education in 2017.10,11
Shifting curriculum structures at medical schools have allowed for flexibility and personalization of students’ preclinical education, most notably through electives. Depending on the institution, these courses may be taught by students or faculty, and can focus on various medical specialties, medical humanities, research, volunteering, or personal wellness.12 At The Warren Alpert Medical School at Brown University, the authors organized an anesthesiology preclinical elective for first- and second-year medical students. The elective, composed of 10 sessions over 3 months, is designed to provide students early exposure to anesthesiology through hands-on workshops, panel discussions, simulation sessions and presentations. Topics covered include airway management, foundations of ultrasound, basic anesthetic pharmacology and physiology, and a panel discussion of subspecialties within anesthesiology. Furthermore, medical students can shadow faculty and residents in the operating room over multiple days to experience the daily workflow of anesthesiologists and their varied responsibilities.
The goal of this study is to assess changes in attitudes, perceptions, and interest in anesthesiology after participation in a preclinical elective among first- and second-year medical students at The Warren Alpert Medical School of Brown University.
Materials and Methods
The anesthesiology preclinical elective, BIOL 6704: “Anesthesia: Much More than Putting you to Sleep”, is a one-credit course held annually over the fall semester. This pass/fail elective is open to all first- and second-year medical students in the fall semester. The course has been structured with eight to ten 2-hour sessions over the semester that provides participants with an early introduction to anesthesiology through hands-on workshops, panel discussions, simulation sessions, and final student-led presentations. Lectures include airway management, foundations of ultrasound, basic anesthesiology pharmacology and physiology, as well as a panel of anesthesia subspecialties. The sessions and learning objectives are presented in Table 1.
 |
Table 1 Selected Syllabus Information |
Furthermore, students are required to shadow attending and/or resident anesthesiologists in the operating room for at least one occasion to experience the daily workflow and varied responsibilities within the specialty. This aspect of the elective can provide opportunities for networking and mentorship within the Department of Anesthesiology. Depending on students’ and faculty/resident schedules, these sessions ranged from full- to half-day sessions; on average, students participated in one to two half-day experiences.
Administratively, the elective is run by one anesthesiology faculty member, three to five anesthesiology residents interested in medical education, and two medical student leaders who have previously taken the course. In general, the medical student leaders oversee the logistics of the class, while the faculty instructors and residents determine the overall course content and deliver the information during the sessions. Given the voluntary nature of this elective, it has an informal atmosphere and provides a low-risk, inclusive environment for students to learn. Two hospital-based workshops that focus on airway skills and ultrasound are also incorporated into the curriculum, with each having multiple 15-minute stations for students to rotate through. Approximately a week before, students are provided with pre-session videos and assigned readings, essentially a flipped classroom approach, to maximize procedural practice.
The primary aim of this elective is to offer interested preclinical students a more thorough and accurate understanding of the field of anesthesiology. To investigate changes in attitudes, perceptions, and interest in anesthesiology after taking this elective, a voluntary, anonymous pre- and post-elective questionnaire was developed and administered to students during the first and last sessions. Inclusion criteria consisted of active enrollment in the elective; no students were excluded. This survey was distributed by paper and took approximately 5 minutes to complete, with no form of compensation provided to participants. The students were asked to complete the survey and place the questionnaires into a designated box located in the lecture room. Subsequently, these surveys were collected by an investigator not assigned to participate in instruction to any of the participants to maintain anonymity of the responses.
Questions consisted of basic demographics, priorities when choosing a medical specialty, current attitudes and perception regarding anesthesiology, as well as current knowledge of select anesthesia topics (Supplementary Material; Appendix A). The survey questions were adapted from prior questionnaires of medical students in similar elective courses, with additional questions developed by the authors of the current study which were reflective of content to be addressed in the course.13,14 Demographic questions were formatted as multiple-choice answers, with some having the option of selecting “other” and providing free-text responses. The question set on ranking factors for medical specialty choice consisted of seven statements, with participants specifying from 1 to 7 the most to least important factors, respectively. The remaining questions were formatted as 5-point Likert scales, with choices of “Strongly Disagree”, “Disagree”, “Neutral”, “Agree”, and “Strongly Agree.” For data analysis purposes, “Strongly Disagree” equated to a 1 and “Strongly Agree” equated to a 5. The Rhode Island Hospital Institutional Review Board determined that this study is exempt from Human Subjects Research under 45 Code of Federal Regulations 46.104(d) requirements and does not require consent documentation (IRB# 1938431). Participants received an introduction letter describing the study and their completion of the survey indicated willingness to participate in the study.
All analyses were performed using Stata/SE 17.0 (StataCorp LLC). The results were analyzed using the Wilcoxon’s signed-rank test for paired samples. Statistical significance was determined if p < 0.05. Qualitative measures such as medical specialty interests were grouped to form proportions.
Results
A total of eleven students completed the pre-course survey (100%). Out of this cohort, two students dropped out of the elective, but the remaining nine students completed it as well as the post-course survey (87%), and were thus included in the final analysis. There were no new students added into the elective. In general, most enrolled medical students were in their first year of study, male, Asian or White, and had some brief experience with anesthesiology. None of the students reported having an immediate family member who is an anesthesiologist, certified registered nurse anesthetist (CRNA), or anesthesiologist assistant (AA).
When asked about their top medical specialties of interest, students reported anesthesiology as the number-one pick of specialty among the participants. With regard to individual responses, students who had brief interactions with the field of anesthesiology prior to the course indicated interest in the specialty as a potential career choice. Characteristics of participants are presented in Table 2.
 |
Table 2 Participant Demographics and Prior Interactions with Anesthesiology for the Students that Completed the Elective |
Table 3 shows the factors that are most important to first- and second-year medical students when considering a specialty. After the completion of the elective, more students chose “the amount of in-hospital calls during overnights and weekend hours” as a less-important factor when choosing a medical specialty (p = 0.047, Cohen d = 0.587). Regarding the part on preconceived notions or stereotypes about anesthesiology and anesthesiologists, students tended to disagree with the false statements such as “Anesthesiologists defer to the surgeon on deciding whether a patient is optimized for surgery” and agree with factual ones like “Anesthesiologists have a direct impact on patient care” (Table 4).
 |
Table 3 Factors That are Most Important to First and Second Year Medical Students When Considering a Specialty |
 |
Table 4 First- and Second-Year Medical Students’ Current Attitudes and Perceptions Regarding the Field of Anesthesiology |
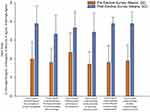
The responses to the final section of questions showed significant improvement in the students’ subjective understanding of topics in anesthesiology (Figure 1). All areas demonstrated an increase of greater than 50% with the largest pre-post change involving the statement of “I have a good understanding of the different subspecialties of anesthesiology”, which increased by 114%.
Discussion
Our study focused on medical students’ subjective experience with the field of anesthesiology and the value of providing early exposure to anesthesiology in the preclinical years of their training. Student participation in the course confirmed their interest in the field of anesthesiology. The biggest impact of the preclinical elective was seen in the students’ self-reported understanding of key aspects of the practice of anesthesiology. Significant improvement was seen in the understanding of airway management, anesthetic pharmacology, basics of ultrasound, vascular access, anesthesiology subspecialties, and an understanding of anesthesiology residency. These skills are a key part of anesthesiology practice and were emphasized during the course through discrete workshops and lectures. A significant improvement is sensible considering preclinical medical school curriculum does not significantly focus on anesthesiology-specific skills such as airway management and vascular access. Furthermore, the shadowing component of the elective may have contributed to the increase in knowledge of the practice of anesthesiology as the students witnessed anesthesia practice firsthand. First- and second-year medical students were able to rotate through a multitude of anesthesia subspecialties and experience the day-to-day practice of anesthesiology.
Following the completion of the course, students considered the number of late hours and weekend in-hospital calls as a less-important factor when choosing a specialty. Since the participants were first- and second-year medical students with limited exposure to clinical rotations, this elective likely provided the students with more perspective in extended hours working weekends and after-hours in hospitals. The vast majority of physicians will experience work hours that include night calls and weekend shifts which is particularly evident in the field of anesthesiology with emergent surgeries. Although our results found this to be a less prominent factor in selecting a specialty, future evaluations with larger class sizes are warranted.
We found no significant change in the respondents’ attitudes and perception regarding anesthesiology. The students who participated in the elective did so voluntarily with interest to learn about the field of anesthesiology. The review of the pre-elective survey responses showed minimal pre-existing misconceptions about the practice of anesthesiology. Thus, this elective served to confirm the students’ attitudes and perceptions of anesthesiology leading to no significant changes in the post-elective survey responses.
There are very few instances in the literature of anesthesiology electives targeted at first- and second-year medical students. Tien et al showed an increase in likelihood of pursuing anesthesiology as a career after a 1-week intensive anesthesiology elective for first-year medical students.13 Curry conducted a survey of US anesthesiology teaching programs which noted about half of the programs had exposure for medical students in their preclinical years, mostly through traditional lectures, but sparse operating room or simulation teaching opportunities.9 Smyth et al found an increase in interest in the field of anesthesiology for second-year students with exposure to anesthesiology-specific skills being a driver for these students.14 Similarly, in the surgical literature, there are data showing improved confidence in surgical practices in first- and second-year medical students after a semester-long general surgery elective.15
One point of consideration is whether medical schools should have mandatory education in anesthesiology prior to students’ graduation. Given the expansive practice of anesthesiologists in healthcare settings—operating room, perioperative areas, intensive care units, labor and delivery floors, as well as rapid response or code teams—students would greatly benefit from exposure to the field. Moreover, anesthesiologists participate in a variety of procedural skills that all physicians would benefit from receiving practice in, such as intubation.16 Medical students have found benefit from even a single week of immersion into anesthesiology, which may help institutions with limited scheduling for additional clerkships beyond classical requirements.17
We note some limitations to our study. The enrollment in the elective consisted of eleven students at the first session and concluded with nine students at the end of the course. Our sample size was small and limited by the number of enrolled preclinical medical students. The small sample size likely impacted our ability to detect small differences in survey results. Additionally, some participants responded with having some form of interactions with anesthesiology prior to the elective. However, this brief exposure during undergraduate studies was limited and did not provide an organized course experience. Furthermore, there is some degree of selection bias in our sample as students voluntarily enrolled in this elective and the course involved only preclinical medical students from a single medical school. In addition, this study was not designed to measure any objective measures of understanding of the practice of anesthesiology given the lack of formalized assessments.
Conclusion
During medical school, time constraints limit the ability of educational institutions to adequately address every specialty, yet it is essential for schools to provide their students with outlets to discover their interests. The pre-clerkship elective, BIOL 6704: “Anesthesia: Much More than Putting You to Sleep”, at The Warren Alpert Medical School of Brown University provided learners an opportunity to explore a specialty that does not receive adequate attention in the preclinical curriculum, with our results noting improvements in students’ familiarity with various aspects of the specialty. This elective can serve as a guide for future preclinical anesthesiology elective courses. Curriculum initiative for preclinical electives is an ongoing process, and future variations of the course should continue to extend education in the field of anesthesiology, providing medical students insight into the future of this specialty.
Abbreviations
AA, Anesthesiologist Assistant; AAMC, Association of American Medical Colleges; ASA American Society of Anesthesiologists; CRNA, Certified Registered Nurse Anesthetist; US, United States.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article and its Supplementary Information Files.
Ethics Approval and Consent to Participate
The Rhode Island Hospital Institutional Review Board determined that this study is exempt from human subjects’ research under 45 Code of Federal Regulations 46.104(d) and does not require consent documentation (IRB# 1938431). Participants received an introduction letter describing the study and the participants completion of the survey indicated their willingness to participate in the study. All methods were carried out in accordance with relevant guidelines and regulations.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare no funding associated with this publication.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. Adudu OP, Le NH, Devito I, Campbell FA, Levine MF. Medical student impressions of anesthesiology and anesthesiologists. Can J Anaesth. 2010;57(8):792–793. doi:10.1007/s12630-010-9334-0
2. Continuity of specialty preference on the matriculating student questionnaire and the 2020 graduation questionnaire. Association of American Medical Colleges. Available from: https://www.aamc.org/data-reports/students-residents/data/report-residents/2020/table-a1-continuity-specialty-preference-matriculating-student-questionnaire.
3. Burton BN, Boulos N, Gabriel RA. Moderately to very competitive: the shifting interest in anesthesiology among medical students. J Clin Anesth. 2019;55:111–112. doi:10.1016/j.jclinane.2019.01.005
4. 2023 main residency match data and reports. National Resident Matching Program. Available from: https://www.nrmp.org/match-data-analytics/residency-data-reports/.
5. What to expect in medical school. Association of American Medical Colleges. Available from: https://students-residents.aamc.org/choosing-medical-career/what-expect-medical-school.
6. Curriculum reports. Association of American Medical Colleges. Available from: https://www.aamc.org/data-reports/curriculum-reports/report/curriculum-reports.
7. Smith AF, Sadler J, Carey C. Anaesthesia and the undergraduate medical curriculum. Br J Anaesth. 2018;121(5):993–996. doi:10.1016/j.bja.2018.06.002
8. Mirman B, Mukhdomi TJ, Rajaguru P, et al. Pain education during the coronavirus pandemic: the introduction of pain medicine during the pre-clinical years. Pain Med. 2022;23(4):609–613. doi:10.1093/pm/pnac001
9. Curry SE. Teaching medical students clinical anesthesia. Anesth Analg. 2018;126(5):1687–1694. doi:10.1213/ANE.0000000000002802
10. Zaman T, Patel V, Cordovani D. Anesthesiologists’ involvement in undergraduate medical education is beneficial to students and the specialty. Can J Anaesth. 2021;68(5):732–733. doi:10.1007/s12630-021-01914-6
11. Hamlin C, Bhangu K, Villafranca A, et al. Participation of Canadian anesthesiology departments in undergraduate medical education. Can J Anaesth. 2017;64(1):16–28. doi:10.1007/s12630-016-0761-4
12. Agarwal A, Wong S, Sarfaty S, Devaiah A, Hirsch AE. Elective courses for medical students during the preclinical curriculum: a systematic review and evaluation. Med Educ Online. 2015;20(1):26615. doi:10.3402/meo.v20.26615
13. Tien M, Aiudi CM, Sviggum HP, Long TR. A peer-designed selective in anesthesiology, critical care, and perioperative medicine for first- and second-year medical students. J Clin Anesth. 2016;31:175–181. doi:10.1016/j.jclinane.2016.02.006
14. Smyth M, Toguri JT, Dow T, Haupt TS, Roberts A, Raju K. Medical student exposure to anesthesiology through the Pre-clerkship Residency Exploration Program: impact on career interest and understanding of anesthesiology. Can J Anaesth. 2019;66(9):1126–1128. doi:10.1007/s12630-019-01403-x
15. Drolet BC, Sangisetty S, Mulvaney PM, Ryder BA, Cioffi WG. A mentorship-based preclinical elective increases exposure, confidence, and interest in surgery. Am J Surg. 2014;207(2):179–186. doi:10.1016/j.amjsurg.2013.07.031
16. Ly EI, Catalani BS, Boggs SD, McGreevey KE, Updegraff AB, Steadman JL. The anesthesiology clerkship: a requisite experience in medical education. Ochsner J. 2020;20(3):250–254. doi:10.31486/toj.20.0094
17. O’Donoghue MA, Martel J. Goal-oriented anesthesia week for MS III students. J Educ Perioper Med. 2016;18(1):E403.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.