Back to Journals » Advances in Medical Education and Practice » Volume 14
Implementation of Team-Based Learning for a Clinical Module of the Ethiopian Undergraduate Anesthesia Curriculum and Students’ Perspectives: A Pilot Cross-Sectional Study
Authors Mulugeta H , Zemedkun A
Received 23 September 2023
Accepted for publication 13 December 2023
Published 15 December 2023 Volume 2023:14 Pages 1413—1424
DOI https://doi.org/10.2147/AMEP.S437710
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Hailemariam Mulugeta, Abebayehu Zemedkun
Department of Anesthesiology, College of Medicine and Health Science, Dilla University, Dilla, Ethiopia
Correspondence: Hailemariam Mulugeta, Dilla University, P.O.Box 419/13, Dilla, Ethiopia, Tel +251 97 041 5208, Fax +251 463 310894, Email [email protected]; [email protected]
Introduction: Team-based learning (TBL) is an active learning strategy that gives students the opportunity to apply conceptual information through a series of tasks that incorporate individual effort, team collaboration, and immediate feedback. This study aimed to report baseline TBL implementation in a clinical module of a fourth-year competency-based undergraduate anesthesia curriculum and explore the perspectives of students.
Methods: In April 2023, 18 students participated in two TBL sessions over two weeks, and readiness assurance test results and post-TBL evaluations were analyzed. Week one TBL implementation scores were compared with week two, establishing a longitudinal analysis over two points in time. Students also participated in an online survey to assess their views on the advantages and design of TBL, their perceptions of its best and worst features, and their suggestions for its implementation.
Results: Of 18 students, 16 (89%) responded to the survey. Most students believed that TBL was an effective educational strategy but expressed concern about the amount of time required for TBL preparation and the need for student readiness. The individual readiness assurance test scores did not differ significantly between weeks 1 and 2 (mean difference [MD] = 0.39, P= 0.519, 95% CI: − 0.824 to 1.60). However, the students’ median [IQR] team readiness assurance test scores increased significantly from week one to week two, from 8 [2] to 10 [1] (p = 0.004). Peer evaluation scores also showed a significant increase in week 2 (MD = 2.4, P = 0.001, 95% CI: − 3.760 to − 0.996).
Conclusion: TBL was successfully implemented for a clinical module at Dilla University—Ethiopia for the first time. Students perceived it positively, but some criticized its preparation time, workload, and minimal facilitator engagement. We suggest convenient and flexible scheduling personalized for each student’s needs when TBL is applied for clinical modules.
Keywords: team-based learning, competency-based education, clinical, anesthetics, pilot implementation, medical education research
Introduction
Team-based learning (TBL) is an active learning instructional approach that gives students the opportunity to apply conceptual information through a series of tasks that incorporate individual effort, team collaboration, and immediate feedback.1 The main goal of TBL is to provide students with the opportunity to practice applying concepts they have learned to solve problems.1,2
Realizing the wide range of TBL delivery methods in medical and health sciences, Haidet et al3 created a guideline for documenting TBL activities in publications. In addition, the TBL framework by Burgess et al (2020) provides useful insights for TBL success.4
The steps of the TBL strategy include planning, readiness demonstrations, and application exercises. Pre-class tasks, such as reading materials, are given to the students during the planning stage. During the readiness demonstration, the students then undergo readiness assurance tests. The students continue by solving realistic problems in teams, and the session is completed with peer evaluation. Consequently, the TBL method makes it possible for one facilitator to oversee multiple teams of 5–7 students in the same classroom.1,4
TBL approach results in better academic, clinical, and communicative outcomes in health professionals’ education (HPE). It motivates students to collaborate to find solutions to issues relevant to their careers and promotes knowledge acquisition and retention, intrinsic subject interest, and independent and lifelong learning.5–9
Evidence also showed that the application of the TBL strategy in HPE results in more favorable attitudes towards learning than for students who attend standard lectures. Students acknowledged that TBL encouraged them to study regularly, generated increased awareness about self-directed learning, and had a positive impact on their learning attitudes. They also perceived that TBL encouraged clinical problem-solving and productive in-class discussion, or that it promoted active learning among peers, motivation, and enjoyment. Ultimately, they felt confident in their mastery of learning outcomes, and it served to improve their own exam performances.10–13
On the contrary, a longitudinal study examining preclinical medical students’ attitudes towards TBL did not find improvement in quality of learning or clinical reasoning ability. However, TBL resulted in a positive attitude in professional development, satisfaction with team experience, and a positive perception towards peer evaluation.14 A systematic review also found mixed results regarding the effectiveness of TBL on improving learning outcomes, particularly knowledge scores and health professional students’ attitudes towards it.15
Furthermore, TBL can be difficult for both facilitators and students, as they must arrange a lot of preparation time. Facilitators can help students overcome difficulties by setting clear expectations and norms for group work, providing instruction, letting them give feedback, and considering their preferences when scheduling sessions.4,16
Despite the controversies and challenges, the TBL strategy is widely recognized as a useful active learning strategy, and its use in HPE classrooms has become more prevalent globally.1,4 In Ethiopia, the Ministry of Education, in collaboration with the Ministry of Health, recently revised the traditional HPE framework into nationally harmonized, competency-based education (CBE) curricula. The previous didactic lecture-based instructions are replaced by active learning strategies such as TBL. However, there is no evidence regarding how TBL is being implemented, and learners’ experiences are unknown because institutions are in the preliminary stages of applying CBE pedagogy.
At the study setting, Dilla University, the TBL pedagogy is being implemented for the undergraduate anesthesiology program for selected modules. This pilot study is therefore aimed to report the baseline TBL use and explore students’ perspectives on participating in the TBL format, which has never been exposed to it. Understanding the TBL implementation challenges, prospects, and students’ views is crucial for continuing educational quality improvement. Other medical and health professional training schools planning TBL implementation in Ethiopia could gain useful insight. Additionally, our findings, from a low-income country, will add additional understanding to the existing TBL literature. Our findings are in accordance with the TBL reporting guidelines by Haidet et al3 and the guidelines for reporting survey-based research by Artino et al.17
Materials and Methods
Study Setting, Context, and Design
Ethiopia is a low-income country found in sub-Saharan Africa. Anesthesiology training in the county is given in three forms: a four-year undergraduate anesthesia program for university students in natural science who have completed a six-month common course of study; a two-year integrated clinical- and research-based anesthesia graduate program for novice anesthetists who have already completed a baccalaureate program in anesthesia, and a three-year anesthesiology residency program for general practitioners who have completed six to seven years of medical degree. The undergraduate baccalaureate anesthesia curriculum in Ethiopia, which was harmonized nationally in 2020, is “competency-based” and incorporates active learning strategies including TBL, case-based discussions (CBD), and problem-based learning (PBL). While the CBD and PBL approaches are widely employed, the TBL is new to the CBE curriculum, which is in the initial phase of its implementation.
In this report, a web-based, cross-sectional survey was employed after a pilot TBL implementation in a selected clinical module for fourth-year undergraduate anesthesiology students at Dilla University, Ethiopia. The TBL approach was introduced from April 1 to April 30, 2023, and an online survey was conducted from May 1 to May 5, 2023.
Participants and Sampling
This study employed convenience sampling technique as it was a module facilitator-initiated pilot TBL implementation study. All eighteen undergraduate anesthesiology students who enrolled in year-four were included. Students were first given training about the pilot TBL implementation frameworks and the objective of implementing the TBL strategy as directed by their CBE curriculum. Then, three teams, with six students each, were formed by the module facilitator (HM). Two TBL sessions were conducted over two weeks. All students were then invited to participate voluntarily in an anonymous web survey after the end of the TBL sessions (Figure 1). Therefore, while the TBL implementation phase was made as part of the curricular requirement in this study, informed consent was obtained from each student for the study’s purpose.
 |
Figure 1 Schematic representation of the study procedure. Abbreviations: TBL, Team-Based Learning; IRAT, Individual Readiness Assurance Test; TRAT, Team Readiness Assurance Test. |
Variables and Assessment Endpoints
During the TBL implementation phase, the following variables were assessed: individual and team readiness assurance test scores, peer evaluation scores, and facilitator evaluation scores. The week one TBL implementation observations were compared with week two to establish a longitudinal descriptive progress report over two points in time. Then, students’ perspectives towards TBL as a pedagogy and its design and facilitation framework were assessed from the online survey.
Design and Facilitation Procedures of the TBL Implementation
Two TBL clinical cases on advanced trauma life support were prepared from the “Anesthesia for Trauma and Orthopedics” module. The TBL clinical case, in week 1, was about an adult involved in a road traffic accident and focused on the initial assessment and management. The second case, in week 2, focused on managing shock after trauma and anesthetic considerations during damage control surgery in place of ongoing shock.
The structured framework of TBL implementation in Table 1 was adapted from Burgess et al.4 It shows the conceptual context through team formation, pre-class preparation, readiness assurance testing, feedback, clinical problem-solving activities through case vignettes, featuring authentic questions for in-depth team discussion, and post-TBL evaluations. This framework was used for each case over two weeks and each session required 2.5 hours, excluding pre-class preparation. The peer evaluation tool was adapted from Burgess et al,18 whereas the facilitator assessed each student’s performance using a team-working skills assessment rubric already in use in our setting.
 |
Table 1 Design and Facilitation Procedures of the Team-Based Learning Strategy for Year Four Undergraduate Anesthesia Students, Dilla University, 2023 |
Survey Data Collection Instrument and Management Procedure
We developed an online data collection questionnaire based on a validated team-learning measurement tool by Thompson et al,19 and recent theoretical perspectives on TBL strategy.1–4 The tool contained three main areas: students’ views on the advantage of TBL, containing 11 statements measured on a five-point Likert scale —from strongly disagree to strongly agree; students’ views towards the design and facilitation processes of TBL, containing 15 statements measured on a five-point Likert scale —from strongly disagree to strongly agree; and four open-ended questions on students’ perception of the best and worst features of TBL, their suggestion points on how TBL should be implemented, and what resources will be required before proceeding to the strategy. One item assessed the extent to which students recommend the TBL strategy for future use on a scale of 1 to 5. The survey tool was first read by three selected senior faculty from the study setting to establish face validity. After checking the clarity of the contents of the survey tool, a Google Forms web survey link was sent to each student via a Telegram messaging app, and participants submitted their responses anonymously. Three text reminders were sent to respondents over five data collection periods from May 1–5, 2023.
Statistical Analysis
Readiness assurance test results and peer and facilitator evaluations were analyzed using IBM SPSS (version 25.0. Armonk, NY: IBM Corp.), and the mean (SD) or median (IQR) scores were compared between weeks 1 and 2 using the independent-samples t-test or Mann–Whitney U-test, as appropriate. We performed a survey data validity check to identify and eliminate careless or inattentive responses from the analysis.13 Accordingly, the following indicators were visualized for each respondent: identical answers to all items on students’ views on TBL advantage, identical answers to all items on students’ views towards the design and facilitation processes of TBL, and a diagonal response pattern in at least one block of items. Respondents with at least two of these three indicators were removed from the analysis. The Likert-scale type responses were then counted for each attribute, converted to percentages, and presented with stacked bar charts. A Pro Word Clouds generator was used to visualize the text data from the open-ended responses. Conclusions were drawn from the data after coding similar types of comments using inductive content analysis.
Results
TBL Implementation Phase
Eighteen students participated in the two-week TBL program. All students (100%), each week, participated in the 10-item IRAT assessment, gave an immediate peer evaluation out of 50%, and their performance assessed by the facilitator out of 20%.
Individual Readiness Assurance Test (IRAT)
Five students improved their scores in week 2 compared to week 1 by one to four points. Nine students scored lower than their first by one to four points on their week 2 assessment. However, there was no statistically significant difference between the students’ mean [SD] IRAT scores at week one (7.33 [1.74]) and week two (6.94 [1.92]) (MD = 0.39, p= 0.519, 95% CI: −0.824 to 1.60).
Team Readiness Assurance Test (TRAT)
Two of the three TBL teams received 8/10 in the first week, whereas one TBL team received 10/10. The TBL team that received 10/10 in week one received the same score as in week two. One of the TBL teams increased its score by one point in week two, while the other, which received 8/10 in week one, maintained the same score. The students’ median [IQR] TRAT scores increased significantly from week one to week two, from 8 [2] to 10 [1] (p = 0.004).
Facilitator’s Assessment of Students’ Performance
Only two (11%) students’ TBL performance over the span of two weeks received 20/20 points from the facilitator. In week 2, 11 (61%) students saw their scores increase by one to four points. The three students’ week two scores were one point lower than their week one score. One student’s score remained unchanged from week 1 to week 2 (10/20). Overall, there was no statistically significant difference between week one (16.0 [10]) and week two (17.5 [10]) in the median [IQR] facilitator scores for student performance (p = 0.134).
Immediate Post-TBL Peer Evaluation
Each student completed a self-evaluation at each TBL session and received evaluations from five members of the TBL team. The mean [SD] evaluation scores of students in week two (47.68 [1.90]) significantly improved from week one (45.30 [2.17]) with an MD of 2.38 points (p = 0.001, 95% CI: −3.760 to −0.997).
Online Survey
At the end of the TBL sessions, 16 out of 18 (88.89%) students completed an online survey. The final response rate was 83.33% because one of the respondents’ responses was deemed careless or inattentive and was not included in the analysis.
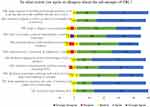
Figure 2 depicts the students’ perspectives on the advantages of TBL. On a 5-point Likert scale, 80% to 100% of respondents either agreed or strongly agreed in all statements about the theoretical benefits of TBL. Figure 3 shows the students’ views on the TBL design and facilitation process. On a 5-point Likert scale, 73% to 94% of respondents viewed it favorably.
Students’ views about the benefits and downsides of TBL are represented as word clouds in Figures 4 and 5, respectively. Tables 2 and 3 show the generated codes together with sample student comments from textual data on their views of TBL.
 |
Table 2 Students’ Views on the Advantages of Team-Based Learning (N = 15) |
 |
Table 3 Students’ Views on the Challenges of Team-Based Learning (N = 15) |
 |
Figure 4 Word cloud text data representation of respondents’ views on the advantages of TBL. |
 |
Figure 5 Word cloud text data representation of students’ views on the disadvantages or challenges of TBL. |
On a scale of 1 to 5, 14 students (93%) gave the TBL technique their highest recommendation as an essential classroom-based teaching strategy. However, in their open-ended comments, they warned that time constraints and student workloads should be carefully planned before implementation. For example, a student said:
Time-management during TBL is my concern. I mean, the time allotted for each TBL session should be varied contextually.
They also noted that facilitators need to understand each student’s and TBL team’s interests and dynamics, and select up-to-date management guidelines, algorithms, videos, and standard books for each TBL session. This is particularly important when TBL is implemented in clinical modules. For example, one student put it as:
Whenever it [TBL] is implemented, the facilitator should know the interest of groups and each team members.
Another wrote:
The facilitator’s suggestion to applicable reading materials and management guidelines, tailored for each session before TBL is very important in my opinion.
Discussion
This study aimed to clarify students’ views on taking part in the TBL class format and to report the first successful implementation of the TBL strategy for a clinical module in a competency-based undergraduate anesthesia program. Most students perceived their experience of each step of TBL implementation positively and about the advantages of the teaching strategy. However, they were concerned about the time required for the TBL process and its associated workload when applied to clinical modules. They recommended careful TBL time scheduling tailored to each student’s needs for future implementation. Some of them also raised concerns about the minimal engagement of the facilitator towards their learning activity and the difficulty in bringing different ideas into one. These findings are further elaborated using the design and facilitation framework of TBL implementation.
Guided with previous evidence,3,20,21 student TBL teams in this study were formed by the facilitator, ensuring there was a diverse mix in each team, and they stayed together until the end of the two TBL sessions to enhance team dynamics, trust, and continuity of learning. Most respondents regarded it positively as promoting effective discussions and peer learning.
The TBL pedagogy is even integrated with a variety technology-enhanced active learning strategies nowadays22 and blended with flipped classrooms23 to enable contemporary medical students for rapid and interactive learning and feedback. Moreover, there is a growing call for interprofessional TBL to enhance shared learning among the various health disciplines.13,24 In our case, we were in the initial stages of implementing the TBL framework for CBE anesthesia curriculum with the available resources. The TBL strategy was provided face-to-face in the classroom, with paper-based readiness assurance tests, problem-solving activities, and post-TBL evaluations.
Pre-class access to up-to-date study materials, such as guidelines, textbooks, and management algorithms, was seen by our participants as a key factor in the success of the TBL approach. This is consistent with Michaelsen et al,2 who suggested that students would typically complete readings as part of the pre-class preparation phase. Facilitators can share diverse types of content, such as videos and prerecorded PowerPoints, electronically for students specific to each session.1,4
The IRAT is completed at the start of the TBL class1,16 or online before the session started.4 It is then completed in teams followed by immediate feedback from the facilitator.4 Most students view the tests as motivating their pre-class preparation, but some have suggested a reward mechanism for those who prepare better. Similarly, Kim et al25 found that the tests have been found to have no positive effects on nursing students’ problem-solving, learning satisfaction, and team efficacy. This may reflect the need for a follow-up mechanism to track pre-class preparation. Employing summative assessments or graded incentive structures on students’ preparation and participation during TBL may be one mechanism to increase overall TBL performance.26,27 However, Eudaley et al28 found no significant difference between graded and ungraded readiness assurance tests in the overall mean percentage score of individual RATs. Additionally, Deardorff et al found that students may have a greater preference for ungraded TBL exercises.29
This study found that only a small percentage of students saw an increase in mean IRAT scores in the second week, with 50% of students scoring lower than week one. This contradicts the findings of Burgess et al,30 which might be due to exam item difficulty levels varying throughout the TBL sessions and in different contexts. However, in each TBL session, the students’ TRAT scores were greater than their IRAT scores, reflecting their survey responses that not all the students were adequately prepared. This is consistent with a meta-analysis by Ngoc et al,31 who found that students scored higher on the TRAT than on the mean IRAT.
In parallel with the previous literature,4,16 participants perceived the presence of real-time expert facilitator feedback and carefully constructed clinical problem-solving activities to promote real-life clinical decision-making skills. Assessments of clinical reasoning ability were also significantly higher in TBL students than in non-TBL students in the context of clinical practice, and students found TBL to be effective, particularly in the areas of problem solving and feedback from specialists.32
Peer evaluation is essential for successful TBL to develop individual behaviors and soft skills that require adaptation, resilience, reflection, and collaboration.4,18,33 The survey participants in our study saw it as encouraging motivation, self- and peer criticism, and accountability for teammates. However, until recently, it was difficult to find standardized systems to implement TBL peer feedback.18,33,34
In agreement with the results of previous studies,1,2,4,16,24,35 most students who responded to an online survey perceived TBL as an effective teaching method that promotes collaborative and self-directed learning, engagement and motivation, and life-long skills, such as critical thinking. However, they noted that the time required for TBL implementation, and its associated workload were the greatest challenges for its application in clinical modules. Burgess et al4 also emphasized that the TBL process is a time-consuming task when designing, organizing, and implementing it and that students may feel overwhelmed by the workload and exhausted by problem-solving discussions. They may also have other clinical and academic obligations that compete for attention and energy.
The facilitator’s role is to create a safe and engaging learning environment, guide the process, provide feedback, and monitor student progress and outcomes.36 However, some students may need more guidance and support from the facilitator, especially when encountering difficult or unfamiliar concepts. Some participants regarded the facilitator’s clinical expertise as a valuable source of learning. Therefore, the facilitator may need to balance being a coach and being a mentor during TBL implementation, depending on the students’ needs and expectations.37
Limitations of the Study and Future Research Implications
We recognize that the exclusion of one respondent’s online survey response from analysis may have resulted in bias. Additionally, the perspectives of the two students who opted out of the online survey may differ from those of their peers who participated in the study. Moreover, the use of web-based survey questionnaires, evaluation rubrics, and peer review forms without pre-testing or validation may have introduced measurement errors. However, face validity, or member checking, was established for each assessment tool. Besides, the tools were already validated in the English language elsewhere.18,19 Though the medium of instruction in Ethiopian higher education is English, it is important to note that there may be cultural differences between Ethiopia and other English-speaking people that could affect the interpretation of the survey questions.
In this study, the facilitator is a senior anesthetist and faculty member with over a decade of teaching experience, has a national certificate in PBL case development and facilitation skills, and has participated in the nationally harmonized CBE anesthesia curriculum development. However, they had no prior TBL expertise, which may have impacted the students’ experiences. We also recognize that faculty development is an essential part of TBL before its implementation. One important challenge to note was the lack of prior TBL implementation experience in our health and medical colleges and the limited number of trained facilitators to implement TBL on a wider scale. Therefore, we only report the TBL implementation from a single institution by including conveniently sampled students due to feasibility issues. The small sample size may have resulted in bias and limited the generalizability of the findings. However, the findings may be useful to other health professional training schools considering TBL adoption through pilot studies.
As a future directive, we suggest additional curricular implementation research about how TBL is being applied in different health science disciplines in Ethiopia. This may include comparing the TBL strategy with other existing instructional methods, such as CBD and PBL, and exploring facilitators’ and students’ perspectives using qualitative, quantitative, and mixed methods. This can help to better understand the existing challenges and opportunities in achieving curriculum milestones in competency based HPE.
Conclusion
The TBL approach was effectively implemented in our undergraduate anesthesia program for the first time. Most students perceived TBL as an efficacious educational strategy that facilitates individual and collaborative learning, motivation, engagement, and development of lifelong soft skills. Its huge time and effort requirements were raised as concerns for its use in clinical modules. Some students may also need more guidance and support from a facilitator throughout the TBL process. To implement TBL for clinical modules, we suggest convenient and flexible scheduling personalized for each student’s needs.
Abbreviations
CBD, Case-Based Discussion; CBE, Competency Based Education; HPE, Health Professional Education; IRAT, Individual Readiness Assurance Test; PBL, Problem Based Learning; TBL, Team Based Learning; TRAT, Team Readiness Assurance Test.
Data Sharing Statement
The datasets used in the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent
This study was approved by the institutional review board of the College of Medicine and Health Science, Dilla University, Ethiopia. Each student gave informed consent for participation in the study and for the publication of anonymized responses.
Acknowledgments
The authors would like to thank the students who participated in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Parmelee D, Michaelsen LK, Cook S, Hudes PD. Team-based learning: a practical guide: AMEE guide no 65. Med Teach. 2012;34(5). doi:10.3109/0142159X.2012.651179
2. Michaelsen L, Knight A, Fink L. Team-Based Learning: A Transformative Use of Small Groups.
3. Haidet P, Levine RE, Parmelee DX, et al. Perspective: guidelines for reporting team-based learning activities in the medical and health sciences education literature. Acad Med. 2012;87(3):292–299. doi:10.1097/ACM.0b013e318244759e
4. Burgess A, van Diggele C, Roberts C, Mellis C. Team-based learning: design, facilitation and participation. BMC Med Educ. 2020;20:1–7. doi:10.1186/s12909-020-02287-y
5. Lang B, Zhang L, Lin Y, Han L, Zhang C, Liu Y. Team-based learning pedagogy enhances the quality of Chinese pharmacy education: a systematic review and meta-analysis. BMC Med Educ. 2019;19(1). doi:10.1186/s12909-019-1724-6
6. Alberti S, Motta P, Ferri P, Bonetti L. The effectiveness of team-based learning in nursing education: a systematic review. Nurse Educ Today. 2021;97:104721. doi:10.1016/j.nedt.2020.104721
7. Ulfa Y, Igarashi Y, Takahata K, Shishido E, Horiuchi S. A comparison of team-based learning and lecture-based learning on clinical reasoning and classroom engagement: a cluster randomized controlled trial. BMC Med Educ. 2021;21(1). doi:10.1186/s12909-021-02881-8
8. Zhang Q, Tang X, Zhao Y, Wang Z. Team-based learning vs. lecture-based learning in nursing: a systematic review of randomized controlled trials. Front Public Health. 2023;10:1044014. doi:10.3389/FPUBH.2022.1044014
9. Joshi T, Budhathoki P, Adhikari A, Poudel A, Raut S, Shrestha DB. Team-based learning among health care professionals: a systematic review. Cureus. 2022;14(1):e21252. doi:10.7759/cureus.21252
10. Vasan NS, DeFouw DO, Holland BK. Modified use of team-based learning for effective delivery of medical gross anatomy and embryology. Anat Sci Educ. 2008;1(1):3–9. doi:10.1002/ase.5
11. Chung EK, Rhee JA, Baik YH, Oh-Sun A. The effect of team-based learning in medical ethics education. Med Teach. 2009;31(11):1013–1017. doi:10.3109/01421590802590553
12. Inuwa IM. Perceptions and attitudes of first-year medical students on a modified Team-Based Learning (TBL) strategy in anatomy. Sultan Qaboos Univ Med J. 2012;12(3):336–343. doi:10.12816/0003148
13. Chan LK, Ganotice F, Wong FKY, et al. Implementation of an interprofessional team-based learning program involving seven undergraduate health and social care programs from two universities, and students’ evaluation of their readiness for interprofessional learning. BMC Med Educ. 2017;17(1). doi:10.1186/s12909-017-1046-5
14. Parmelee DX, DeStephen D, Borges NJ. Medical students’ attitudes about team-based learning in a pre-clinical curriculum. Med Educ Online. 2009;14:1. doi:10.3402/meo.v14i.4503
15. Fatmi M, Hartling L, Hillier T, Campbell S, Oswald AE. The effectiveness of team-based learning on learning outcomes in health professions education: BEME guide no. 30. Med Teach. 2013;35(12):e1608–e1624. doi:10.3109/0142159X.2013.849802
16. Ruder P, Maier MH, Simkins SP. Getting started with team-based learning (TBL): an introduction. J Econ Educ. 2021;52(3):220–230. doi:10.1080/00220485.2021.1925187
17. Artino AR, Durning SJ, Sklar DP. Guidelines for reporting survey-based research submitted to academic medicine. Acad Med. 2018;93(3):337–340. doi:10.1097/ACM.0000000000002094
18. Burgess A, Roberts C, Lane AS, et al. Peer review in team-based learning: influencing feedback literacy. BMC Med Educ. 2021;21(1). doi:10.1186/s12909-021-02821-6
19. Thompson BM, Levine RE, Kennedy F, et al. Evaluating the quality of learning-team processes in medical education: development and validation of a new measure. Acad Med. 2009;84(10 Suppl):S124–S127. doi:10.1097/ACM.0B013E3181B38B7A
20. Michaelsen L, Richards B. Drawing conclusions from the team-learning literature in health-sciences education: a commentary. Teach Learn Med. 2005;17(1):85–88. doi:10.1207/S15328015TLM1701_15
21. Whitley HP, Bell E, Eng M, et al. Practical team-based learning from planning to implementation. Am J Pharm Educ. 2015;79(10):149. doi:10.5688/ajpe7910149
22. McCoy L, Pettit RK, Lewis JH, et al. Developing technology-enhanced active learning for medical education: challenges, solutions, and future directions. J Am Osteopath Assoc. 2015;115(4):202–211. doi:10.7556/JAOA.2015.042
23. Kang HY, Kim HR. Impact of blended learning on learning outcomes in the public healthcare education course: a review of flipped classroom with team-based learning. BMC Med Educ. 2021;21(1). doi:10.1186/S12909-021-02508-Y
24. Burgess A, van Diggele C, Matar E. Interprofessional team-based learning: building social capital. J Med Educ Curric Dev. 2020;7:238212052094182. doi:10.1177/2382120520941820
25. Kim ME, Kim JY. The impact of a team-based learning group readiness assurance test on nursing students’ problem solving, learning satisfaction, and team efficacy: a crossover study. Nurse Educ Today. 2021;100:104819. doi:10.1016/J.NEDT.2021.104819
26. Koh YYJ, Rotgans JI, Rajalingam P, Gagnon P, Low-Beer N, Schmidt HG. Effects of graded versus ungraded individual readiness assurance scores in team-based learning: a quasi-experimental study. Adv Health Sci Educ. 2019;24(3):477–488. doi:10.1007/s10459-019-09878-5
27. Carrasco GA, Behling KC, Lopez O. Weekly team-based learning scores and participation are better predictors of successful course performance than case-based learning performance: role of assessment incentive structure. BMC Med Educ. 2021;21(1). doi:10.1186/s12909-021-02948-6
28. Eudaley ST, Farland MZ, Melton T, Brooks SP, Heidel RE, Franks AS. Student performance on graded versus ungraded readiness assurance tests in a team-based learning elective. Am J Pharm Educ. 2022;86(9):1038–1043. doi:10.5688/AJPE8851
29. Deardorff AS, Moore JA, McCormick C, Koles PG, Borges NJ. Incentive structure in team-based learning: graded versus ungraded group application exercises. J Educ Eval Health Prof. 2014;11:6. doi:10.3352/jeehp.2014.11.6
30. Burgess A, Ayton T, Mellis C. Implementation of team-based learning in year 1 of a PBL based medical program: a pilot study approaches to teaching and learning. BMC Med Educ. 2016;16(1). doi:10.1186/s12909-016-0550-3
31. Ngoc PN, Cheng CL, Lin YK, Wu MS, Chu JS, Tang KP. A meta-analysis of students’ readiness assurance test performance with team-based learning. BMC Med Educ. 2020;20(1). doi:10.1186/S12909-020-02139-9
32. Okubo Y, Ishiguro N, Suganuma T, et al. Team-based learning, a learning strategy for clinical reasoning, in students with problem-based learning tutorial experiences. Tohoku J Exp Med. 2012;227(1):23–29. doi:10.1620/TJEM.227.23
33. Brown T, Rongerude J, Leonard B, Merrick LC. Best practices for online team-based learning: strengthening teams through formative peer evaluation. New Directions Teach Learn. 2021;2021(165):53–64. doi:10.1002/TL.20436
34. Byram J, Robertson K. Development and validation of a peer evaluation tool for team‐based learning. THE FASEB Journal. 2021;35(S1). doi:10.1096/FASEBJ.2021.35.S1.04529
35. Burgess A, Roberts C, Ayton T, Mellis C. Implementation of modified team-based learning within a problem based learning medical curriculum: a focus group study. BMC Med Educ. 2018;18(1). doi:10.1186/s12909-018-1172-8
36. National Health Service (NHS). The facilitator’s toolkit: tools, techniques and tips for effective facilitation; 2009. Available from: www.institute.nhs.uk/fundamentals.
37. Gullo C, Ha TC, Cook S. Twelve tips for facilitating team-based learning. Med Teach. 2015;37(9):819–824. doi:10.3109/0142159X.2014.1001729
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.