Back to Journals » Nursing: Research and Reviews » Volume 12
Improving Nurses’ Knowledge on Sepsis Identification and Management at Mulago National Referral Hospital: A Quasi Experimental Study
Authors Nakiganda C, Atukwatse J, Turyasingura J, Niyonzima V
Received 4 March 2022
Accepted for publication 16 August 2022
Published 14 September 2022 Volume 2022:12 Pages 169—176
DOI https://doi.org/10.2147/NRR.S363072
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Natasha Hodgkinson
Catherine Nakiganda, Joseph Atukwatse, Johnan Turyasingura, Vallence Niyonzima
Department of Nursing, Faculty of Medicine, Mbarara University of Science and Technology, Mbarara City, Uganda
Correspondence: Vallence Niyonzima, Department of Nursing, Faculty of Medicine, Mbarara University of Science and Technology, Mbarara City, Uganda, Tel +256 777842830, Email [email protected]
Background: Sepsis is a global pandemic and public health concern. There is a paucity of data relating to its management and outcomes in the developing world. The surviving sepsis campaign (SSC) guidelines have been developed to improve outcomes of patients with sepsis. There are no documented in-hospital protocols on sepsis management for nurses in Uganda. This study evaluated the effect of an educational intervention on nurses’ knowledge of SSC guidelines in management of patients with sepsis at Mulago National Referral Hospital.
Methods: We used a quasi-experimental design and recruited 40 nurses from neuro-surgical ward and ICU. Pre- and post-intervention assessments were conducted using a validated self-administered questionnaire between October 2020 to February 2021. The intervention was conducted through sessions of presentations, watching videos, and case studies. Data were entered in excel, cleaned, and exported to Stata version 16. Median and interquartile range were used for continuous variables while frequencies and percentages were used for categorical variables. Mean knowledge scores were computed for pre- and post-test evaluation. A paired t-test was used to compare the pre- and post-test knowledge scores at p ≤ 0.05 and 95% confidence interval.
Results: In this study, 57.5% of nurses were from ICU, 67.7% were females and 70% diploma holders. Median age was 32 (IQR= 21.5– 35.5) years. In the post test all nurses were able to score above the preset acceptable score of 50% on the current sepsis guidelines. Mean knowledge score was 3.6 (SD = 1.8) pretest and 8.4 (SD = 1.2) posttest. There was a significant difference in pre and post-intervention mean knowledge scores of 4.9 (SD = 1.90, 95% CI: 4.2– 4.5; t (39) = 16.242, p < 0.001).
Conclusion: The educational intervention improved nurses’ knowledge on SSC guidelines. Regular continuous professional nursing education on sepsis could improve nurses’ knowledge and quality of care for patients with sepsis.
Keywords: nurses, sepsis, knowledge, surviving sepsis campaign guidelines, management
Introduction
Sepsis and septic shock are major healthcare problems associated with significant morbidity and mortality globally.1 Sepsis affects millions of people globally each year, and kills as many as one in four (and often more) people, and greatly increases expenditure related to medical care.2 The worldwide estimates are 288 cases per 100,000 people per year for the last 40 years worldwide.3 Recent estimates suggest 19.4 million yearly cases and 5.3 million deaths from sepsis and septic shock.4 Sepsis has been defined as a life-threatening organ dysfunction from dysregulated host response to infection. On the other hand, septic shock is sepsis with circulatory collapse and cellular mediated abnormalities.5
The International Surviving Sepsis Campaign (iSSC) published guidelines for management of severe sepsis in 2004, with subsequent overall goal of reducing mortality from sepsis and septic shock.2,6 The guidelines have been condensed into a 1-hour bundle with the aim of beginning resuscitation and management immediately.7 These can quickly and easily be completed by nurses with expert knowledge on sepsis management and current knowledge on the new developments in the iSSC guidelines.8 The aim of the international Surviving Sepsis Campaign Guidelines was to provide guidance for clinicians caring for patients with sepsis, septic shock and other sepsis-associated organ dysfunction. Attempts have been made globally to ensure that all health care workers get acquainted with all the components of the sepsis bundle to improve patient outcomes.
The iSSC guidelines recommend the following be completed in 1 hour of patient presentation: obtaining serum lactate levels; blood cultures prior to the administration of antibiotics; administration of broad-spectrum antibiotics; and 30 mL/kg crystalloid for hypotension or serum lactate > 4 mmol/l (36 mg/dl); administration of vasopressors if the hypotension is refractory to fluids with a map ≤ 65mmHg.7
Sub-Saharan Africa is reported to account for a significant proportion of the global burden of sepsis which may also go unrecognized.9 Yet this geographical region has limited reports on the management and outcomes of sepsis syndrome.
In MNRH, however, nurses still use the systemic inflammatory response syndrome (SIRS) criteria to identify patients with sepsis despite its low predictive valve of 0.64 as opposed to 0.74 for Sequential Organ Failure Assessment (SOFA) which is used in the iSSC guidelines. According to the hospital’s head nurse, where the nurses had received a number of in-service training sessions regarding use of the SIRS criteria, little attention has been paid to the iSSC guidelines. This may lead to missed diagnosis and improper management of some patients with sepsis. There is a paucity of literature as to whether training nurses in the current sepsis (iSSC) guidelines could improve their knowledge in identification and management of patients with sepsis. Therefore, this study sought to assess the impact of an educational intervention on nurses’ knowledge on management of sepsis using the iSSC guidelines.
Materials and Methods
Study Design
A descriptive quasi experimental design was used with a pretest and posttest, on nurses working in the ICU and neuro-surgical ward. Baseline knowledge on the SSC guidelines was assessed through a self-administered questionnaire, after which an educational intervention was conducted and a posttest was conducted to determine effect.
Study Area
The study was conducted at Mulago National Referral Hospital (MNRH). The study site is a public tertiary teaching hospital with a capacity of 1500 beds. The intensive care unit has 16 bed capacity while neurosurgical ward has 24 bed capacity with 24 hour nurse coverage. These units handle critically ill patients who are susceptible to developing sepsis and indeed sepsis is one of the common medical diagnoses in these units. The hospital serves as the national referral hospital for the whole country, receiving patients from all districts of the country for specialized health care. It offers both inpatient and outpatient health services.
Study Population
The study enrolled nurses working in the adult intensive care unit and neurosurgical ward at MNRH. These are not specialized nurses but they have acquired experience on the job with a few nurses having completed some in-house short courses on critical care. There was a total of 48 nurses located in these units. The intensive care unit (ICU) had a total of 30 nurses, and the surgical ward had a total of 18 nurses. With MNRH being at the top of the health system referral of Uganda, most of the critically ill patients may end up being referred there and therefore these nurses are most likely to manage such patients hence their level of knowledge on sepsis management may give insight into the nurses’ knowledge on sepsis management nationwide. These two clinical areas were selected because they care for critically ill patients who are most susceptible to infection and are at high risk of developing sepsis.
Sample Size
The intensive care unit (ICU) has a total of 30 nurses, and the surgical ward has a total of 18 nurses, which lead to a total of 48 nurses. For a paired t-test analysis, a priori power analysis gave a total sample size of 20 participants per group to detect a large effect (Cohen’s d=0.5) with α =0.05 and 1-β=0.95.10 The large effect size was used owing to the small population size. To increase the power of the study and allow for an anticipated attrition of ten percent, the researcher aimed to have at least 40 nurse participants in the study.
Sampling Technique
Since the number of nurses working in the general ICU and neurosurgical ward was small, the researchers used a population sampling approach in which all eligible nurses working in the ICU and neurosurgical wards were recruited to the study.
Inclusion: nurses working in the ICU and neurosurgical wards in MNRH at the time of the study with at least 6 months of experience in patient care were eligible to participate in the study. This was done to ensure that there was maximum experience with patient care.
Exclusion: nurses who were away on leave or had other commitments at the time of data collection for baseline knowledge evaluation were not considered eligible to participate.
Data Collection Instrument
A validated self-administered questionnaire was used to assess knowledge on sepsis identification and sepsis management. The questionnaire was adopted with permission from a cross-sectional survey that was performed at the 4th All Africa Anesthesia Conference in Nairobi, Kenya.11 It consisted of 11 fill-in and 18 multiple choice questions related to nurses’ knowledge on sepsis management using the SSC guidelines.
The questionnaire was pretested on nurses working at the Naguru-China Friendship Hospital ICU and surgical unit/ward to ensure the questions designed answer the objectives, after which the tool was adjusted accordingly by the researcher. The tool was further reviewed by expert nurses in critical care and senior ICU physician experienced in care of critically ill patients with sepsis with a content validity index of 0.86.
Data Collection Procedure
Ethical approval was obtained from Mbarara University of Science and Technology Research Ethics Committee (MUST-REC) No. 11/07-20. We sought administrative clearance from Mulago National Referral Hospital management. Two research assistants helped in data collection on the objectives of the study in order to avoid misinterpretations. Two nurses with Masters in critical care nursing and with experience in caring for critically ill patients were employed to assist with training of the participants in sepsis management. The researchers contacted the charge nurses of these units/wards and organized meetings with the nursing staff during which the researcher explained the purpose of the study and the relevant details. Written informed consent was obtained from all study participants before they were given a pre-test questionnaire. Data were collected October 2020 to February 2021.
Pre-intervention phase: we assessed participants’ baseline knowledge on iSSC guidelines using a validated questionnaire based on the international consensus on sepsis management. Participants were assured of confidentiality of their information.
Intervention phase: we conducted an educational intervention one week after completion of the pre-intervention assessment. The training involved conducting three face to face teaching sessions in groups of 12–14 participants per session for a period of three weeks for the two units/wards selected. The intervention was conducted separately for each ward. The participants were a mix of cadres during the teaching sessions so as to maximize participation levels during working hours. We are cognizant of the effect of level of education on knowledge acquisition but considered the accessible population. The sessions ran for one hour each day in the afternoon to avoid disruption in the unit activities in the morning hours when the staff is usually busy. The researchers used PowerPoint presentation on the new definition of sepsis and septic shock, the iSSC guidelines, qSOFA and SOFA criteria, and video clips to ensure a deeper understanding of the material. In addition, they reviewed multiple case scenarios during the intervention phase. The participating nurses were given handout files with a PowerPoint presentation and video clips illustrating care of patients with sepsis using the iSSC guidelines.
Post-intervention phase: one month after the intervention, a post intervention evaluation was done to assess the effects of the educational intervention on the nurses’ knowledge on the use of the iSSC guidelines in the management of patients with sepsis. The period of 4 weeks from the pre to the post intervention assessment was adopted from previous studies.12,13
Data Management and Analysis
The management and analysis were done using Microsoft excel and STATA version 12. Data were sorted, coded and entered into STATA program for analysis. Descriptive statistics (frequencies, means and standard deviations) were reported for normally distributed data and interquartile ranges and median for skewed data. Each item was analyzed separately in addition to the overall evaluation. A paired t-test was done to establish association between knowledge and practice improvement and training intervention.
Results
Demographic Characteristics of the Participants
In total, our sample included 40 participants. Majority of our participants (27 [67.5%]) was female, and 13 (32.5%) were male. Majority of the participants (28 [70%]) held a diploma as the highest level of education and majority (23 [57.5%]) were working in ICU. See Table 1.
 |
Table 1 Demographic Characteristics of the Study Participants (n = 40) |
Baseline Knowledge of Nurses on the iSSC Guidelines
Majority of the participants had never heard about the sepsis guidelines with only 12 (30%) participants reporting having heard about the sepsis guidelines yet did not know the exact guidelines. Majority of the participants (35 [87.5%]) did not know that a lactate measurement of >2mmol/L would warrant a critical value for reporting. About the parameters for assessment of sepsis using the SOFA and qSOFA, only 7 (17.5%) and 11 (27.5%) had knowledge of these parameters respectively and their use. Majority of the participants (25 [62.5%]) reported obtaining blood cultures and administering antibiotics within an hour of diagnosis of sepsis or suspecting sepsis, while only a few participants (8 [20%]) reported correctly on how often patients should be screened for sepsis. Majority of the participants (28 [70%]) did not report correct amount of fluid resuscitation for sepsis and hypotension (Table 2).
 |
Table 2 Baseline Knowledge of Nurses on SSC Guidelines (n=40) |
Nurses’ Post Intervention Knowledge on iSCC Guidelines
In the post intervention evaluation, majority of the participants (32 [80.0%]) showed knowledge improvement on the fact that a lactate value >2mmol/L would warrant a critical value for reporting in presence of sepsis. There was also improvement in the knowledge on the parameters for the manifestation of septic shock in a patient with sepsis in 19 (47.5%) participants. Majority of the participants (38 [95%]) stated correctly that a blood culture test would be the appropriate test to be performed when you suspect sepsis. About the parameters for assessment of sepsis using the SOFA and qSOFA, there was improvement in knowledge of the parameters in 23 (57.5%) and 31 (77.5%) participants respectively. Majority of the participants (31 [77.5%]) also reported correct amount of fluid resuscitation for sepsis and hypotension. See Table 3.
 |
Table 3 Post Intervention Knowledge of Nurses on SSC Guidelines (N=40) |
A Comparison of Nurses’ Baseline Knowledge and Post Intervention Knowledge of Sepsis Management Using the iSSC Guidelines
Prior to the educational intervention, majority of the nurses (34 [85%]) had poor knowledge about the iSSC guidelines, and the total mean sum score of the knowledge was 3.6±1.8 (95% CI: 3.0–4.2) points. However, the knowledge levels increased after intervention with 19 (47.5%) nurses attaining good knowledge and 21 (52.5%) attaining excellent knowledge about the sepsis guidelines, and no one scored below 50% (p<0.001). The post-intervention total mean sum score was 8.4±1.2 (95% CI: 8.0–8.8), giving a statistically significant difference in the mean score of baseline knowledge and post-intervention knowledge of 4.9±1.9 (95% CI: 4.2–4.5; t(39) =16.242, p <0.001). Thus, we reject the null hypothesis and conclude that the intervention had a significant effect of improving the participants’ knowledge. See Table 4.
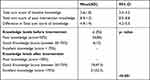 |
Table 4 Comparison of Baseline Knowledge and Post Intervention Knowledge of Participants About the iSSC Guidelines |
Discussion
Baseline knowledge of nurses on sepsis management using the iSSC guidelines was generally low. This could be due to the fact that the participants had never received training on the iSSC guidelines.14 It could also be attributed to limited scope of practice of the study participants, professional identity, insufficient organizational support in continuing nursing education, and the lack of literature exploring what is taught in undergraduate nursing programs about sepsis. Previous studies assert that training on sepsis at lower levels of tertiary education has been identified as a cause for low knowledge levels for nurses in developed countries like Australia.15
Knowledge in this study was categorized according to other literature about knowledge of nurses, where a score above 75% was considered high and adequate for the nurse practitioners.16 Accordingly, 85% of the participants exhibited poor knowledge of iSSC guidelines before the educational intervention. These findings were similar to a study conducted in Egypt where nurses’ knowledge regarding sepsis was low prior to training.17 Egypt is among countries considered to have good healthcare systems in Africa,18 so this finding indicates that in-service training can also bring about positive change in Uganda’s healthcare. Therefore, continuous in-service training for nurses on sepsis recognition and management needs to be encouraged and supported as an integral component of the continuing nursing education for better outcomes of patients with sepsis. Also, there is a need to include clinical nurse specialists in Uganda’s health care system to foster continuous mentorship with the lower nursing cadres. This will ultimately improve patient outcomes. This is supported by a study conducted in Italy which found that knowledge can be improved through educational training and that good knowledge of sepsis guidelines is essential for correct management of sepsis and improved patient outcomes.19,20 Another study by Robson et al, auditing nurses’ knowledge of sepsis also showed an improvement in their knowledge after an educational intervention.21 A similar study by Delaney et al, on impact of an educational intervention on nurses’ competence, showed an improvement in the knowledge of nurses on sepsis management.22 Similarly, studies done in areas outside sepsis have shown that educational intervention significantly improves participants’ knowledge, which can later on be transferred to practice. For example, a study on detection and management of acute kidney injury (AKI) assessed clinicians’ knowledge on AKI and found that only 26% of them were knowledgeable about AKI guidelines compared to 64% after the educational intervention.23 This is evidence that improved knowledge among nurses through educational intervention translates to improved quality of nursing care, which could in turn improve patients’ outcomes. The investigators in this study thus believe that regular in-service training of nurses can significantly improve nursing care of patients with sepsis.
Limitations of the Study
This study was conducted in only two units of the entire national referral hospital in consideration of available time for data collection, which may limit generalizability of the findings to the entire hospital and other hospitals in the country. We recommend that further studies be conducted to include a wider population of nurses of various hospital units and other hospitals, which will allow for generalizability of results.
Due to the nature of the study design as applied to this study, there was no control group with which to compare the results and this could have affected the internal validity of the study. Interventional studies generally recommend a period of at least 6 weeks to collect data after intervention.24 However, in this study, we conducted post-intervention data collection after 4 weeks, as adopted from some studies which have deemed a minimum of 4 weeks after intervention as sufficient.12,13 The argument is that the participants’ memory of the training content could have been still quite fresh, thereby yielding seemingly very good results.
Conclusion and Recommendations
There was generally low level of baseline knowledge among nurses about the iSSC guidelines prior to the educational intervention. The educational intervention, on the other hand, significantly improved the nurses’ knowledge on these guidelines. The iSSC guidelines could be incorporated into continuing medical education schedules in the hospital so that information about sepsis can be shared and well-explained to all healthcare providers (nurses) to improve their knowledge on sepsis. A wider scale study, with a larger sample size and selecting participants from more clinical units which are randomly sampled, could also be more informative.
Abbreviations
AKI, acute kidney injury; ICU, Intensive Care Unit; iSSC, International Surviving Sepsis Guidelines; MAP, mean arterial pressure; MNRH, Mulago National Referral Hospital; MUST- REC, Mbarara University of Science and Technology; qSOFA, quick sequential organ failure assessment; SIRS, systemic inflammatory response syndrome; SOFA, sequential organ failure assessment; SSC, Surviving Sepsis Guidelines.
Data Sharing Statement
The datasets generated and analyzed during the study are available from the corresponding author on request.
Acknowledgments
We acknowledge first mile program for the financial support in this study. We thank the administration of Mulago National referral hospital and participants who participated in this study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article was submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
Research reported in this publication was supported by the first Mile project. The content is solely the responsibility of the authors and does not necessarily represent the official views of the first mile project.
Disclosure
Johnan Turyasingura reports grants from Mbarara University of science and technology, during the conduct of the study. The authors report no other potential conflicts of interest in this work.
References
1. Storozuk SA, MacLeod MLP, Freeman S, et al. A survey of sepsis knowledge among Canadian emergency department registered nurses. Australas Emerg Care. 2019;22(2):119–125. doi:10.1016/j.auec.2019.01.007
2. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi:10.1007/s00134-017-4683-6
3. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
4. Fleischmann C, Scherag A, Adhikari NKJ, et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–272. doi:10.1164/rccm.201504-0781OC
5. Napolitano LM. Sepsis 2018: definitions and guideline changes. Surg Infect. 2018;19(2):117–125. doi:10.1089/sur.2017.278
6. Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008;34(1):17–60. doi:10.1007/s00134-007-0934-2
7. Christa Schorr D, Evans LE, Rhodes A. Surviving sepsis campaign hour-1 bundle. Intensive Care Med. 2018;44(6):925–928. doi:10.1007/s00134-018-5085-0
8. Lewis JM, Feasey NA, Rylance J. Aetiology and outcomes of sepsis in adults in sub-Saharan Africa: a systematic review and meta-analysis. Crit Care. 2019;23(1):1–11. doi:10.1186/s13054-019-2501-y
9. Otu A, Elston J, Nsutebu E. Sepsis in Africa: practical steps to stem the tide. Pan Afr Med J. 2015;21(1):32.
10. Buchner A, Faul F, Erdfelder E, et al. G* power (version 3.1. 2)[computer program]; 2009.
11. Baelani I, Jochberger S, Laimer T, et al. Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Crit Care. 2011;15(1):R10. doi:10.1186/cc9410
12. Lainscak M, Blue L, Clark AL, et al. Self‐care management of heart failure: practical recommendations from the patient care committee of the heart failure Association of the European Society of Cardiology. Eur J Heart Fail. 2011;13(2):115–126. doi:10.1093/eurjhf/hfq219
13. Khademian Z, Mohebi N, Khademian MH. Effects of training on knowledge and attitudes of coronary care unit nurses in relation to teamwork: a quasi-experimental study. J Vasc Nurs. 2020;38(3):132–136. doi:10.1016/j.jvn.2020.05.004
14. Adegbite BR, Edoa JR, Rylance J, et al. Knowledge of health workers relating to sepsis awareness and management in Lambaréné, Gabon. Acta Trop. 2021;219:105914. doi:10.1016/j.actatropica.2021.105914
15. Harley A, Massey D, Ullman AJ, et al. Final year nursing student’s exposure to education and knowledge about sepsis: a multi-university study. Nurse Educ Today. 2021;97:104703. doi:10.1016/j.nedt.2020.104703
16. Sickder HK. Nurses’ Knowledge and Practice Regarding Prevention of Surgical Site Infection in Bangladesh. Prince of Songkla University; 2010.
17. Elsayed HF, Mohamady SH, Elkattan BA-EA. Implementing nursing management protocol regarding early recognition of maternal sepsis. IOSR J Nurs Health Sci. (2019;8(1):30–41.
18. The African Exponent. Top 10 countries with improved healthcare system in Africa 2020;. 2020. Available from: https://www.africanexponent.com/post/7167-top-10-african-countries-with-best-healthcare-system-2020.
19. Nucera G, Esposito A, Tagliani N, et al. Physicians’ and nurses’ knowledge and attitudes in management of sepsis: an Italian study. J Health Soc Sci. 2018;3(1):13–26.
20. Stanislaus D. The impact of training and development on knowledge management. Int J Adv Res Innov Ideas Educ. 2019;5(1):164–175.
21. Robson W, Beavis S, Spittle N. An audit of ward nurses’ knowledge of sepsis. Nurs Crit Care. 2007;12(2):86–92. doi:10.1111/j.1478-5153.2007.00210.x
22. Delaney MM, Friedman MI, Dolansky MA, et al. Impact of a sepsis educational program on nurse competence. J Contin Educ Nurs. 2015;46(4):179–186. doi:10.3928/00220124-20150320-03
23. Xu G, Baines R, Westacott R, et al. An educational approach to improve outcomes in acute kidney injury (AKI): report of a quality improvement project. BMJ open. 2014;4(3):e004388. doi:10.1136/bmjopen-2013-004388
24. Maciejewski MLJB. Quasi-experimental design. Epidemiology. 2020;4(1):38–47.
25. Dellinger RP, LEvy MM, Car;et JM, et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36(1):296–327. doi: 10.1097/01.CCM.0000298158.12101.41
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
