Back to Journals » Clinical Epidemiology » Volume 16
Inflammation-Dependent Association of Lipoprotein (a) with Cardiovascular and Cancer Mortality
Authors Zhang Y, Wang W, Xu L, Lian Z , Huang J, Chang Y, Guo J, Wang Y, Song K, Ji H
Received 18 September 2023
Accepted for publication 18 December 2023
Published 9 January 2024 Volume 2024:16 Pages 1—4
DOI https://doi.org/10.2147/CLEP.S437456
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Henrik Sørensen
Yiwen Zhang,1 Wei Wang,2,* Lili Xu,1 Zhexun Lian,3 Jiale Huang,4 Yaowei Chang,5 Junjie Guo,3 Yangang Wang,1,* Kexiu Song,6 Hongwei Ji7,8,*
1Department of Endocrinology, Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 2Department of Hematology, Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 3Department of Cardiology, Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 4Department of Cardiology, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, People’s Republic of China; 5Department of Cardiology, QingPu Branch of Zhongshan Hospital Affiliated to Fudan University, Shanghai, People’s Republic of China; 6Department of International Medicine, Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China; 7Tsinghua Medicine, Tsinghua University, Beijing, People’s Republic of China; 8Department of Internal Medicine, Beijing Tsinghua Changgung Hospital, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yangang Wang, Department of Endocrinology, Affiliated Hospital of Qingdao University, Qingdao, People’s Republic of China, Email [email protected] Hongwei Ji, Tsinghua Medicine, Tsinghua University, Beijing, People’s Republic of China, Email [email protected]
Cardiovascular disease (CVD) and cancer rank as the two leading causes of death worldwide. Emerging evidence has suggested common mechanisms between CVD and cancer,1 such as oxidative stress and inflammation, which not only mediate the process of atherosclerosis but also promote carcinogenesis and tumor growth.1 Lipoprotein(a) [Lp(a)], an oxidation-specific biomarker,2 has been associated with CVD and cancer. Inflammation may amplify the Lp(a)-associated CVD risk.3 It is likely that inflammation may also enhance Lp(a)-associated cancer risk. If true, it will provide new insights into dual risk of cancer and CVD events, and it may also advance our understanding of collaborative management of CVD and cancer. We therefore sought to examine the association of Lp(a) with CVD and cancer deaths in participants with lower versus higher inflammation levels in a nationally representative cohort.
We performed a secondary analysis by using data from the Third National Health and Nutrition Examination Survey (NHANES III), which was conducted from 1988 to 1994 by the National Center for Health Statistics (NCHS), a part of the Centers for Disease Control and Prevention (CDC). All the data are collected and disseminated by the NCHS staff. Further details about NHANES were introduced in the Supplementary Materials. Each participant, as previously described elsewhere,4 completed a personal interview and underwent a physical examination at the mobile examination center. Serum C-reactive protein (CRP), Lp(a) and other biomarkers were assessed as previously reported.4 A link between NHANES personal identifiers and death certificates from the National Death Index was used for assessing participants’ vital status until 31 December 2019. Of all 31,311 participants underwent examinations of NHANES III, we excluded individuals with incomplete information on covariates or follow-up (N=15,363), who were not fasting or had triglycerides over 400 mg/dL (N=1259) and who had missing data on Lp(a) (N=7886). The final sample includes 6803 individuals (Supplementary Figure 1). Lp(a) was log-transformed and standardized before modelling. A median value of CRP (ie, 0.21 mg/dL) was used as a cutoff point to define systemic inflammation status. We related Lp(a) levels with CVD and cancer mortality using multivariable-adjusted Cox proportional hazards models adjusted for risk factors including age, sex, race, body mass index, history of CVD, history of cancer, current smoking, hypertension, diabetes mellitus, high-density lipoprotein cholesterol level, total cholesterol level, cholesterol-lowering therapy, hypoglycemic medication, and family income. We used R version 4.2.1 for all analyses and the results were expressed as hazard ratios (HRs) and 95% confidence interval (95% CI).
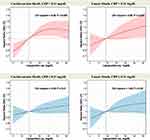
In this study sample (N = 6803, 56.7% females, mean age 46.3±19.4 years), over a median follow-up of 25.8 years, we documented 908 CVD deaths and 552 cancer deaths. As shown in Table 1, Lp(a) was associated with both CVD mortality (HR, 1.09; 95% CI, 1.02–1.17) and cancer mortality (HR, 1.12; 95% CI, 1.02–1.23). In participants with CRP>0.21 mg/dL, per SD increase in log-transformed Lp(a) was associated with 14% (HR, 1.14; 95% CI, 1.03–1.26) and 16% (HR, 1.16; 95% CI, 1.02–1.32) higher hazard of CVD and cancer mortality respectively. In contrast, for those with CRP ≤ 0.21 mg/dL, no evident association between Lp(a) and mortality risk was observed. In restricted cubic splines, we observed similar findings (Figure 1).
 |
Table 1 Association of Lp(a) with Cardiovascular and Cancer Mortality According to CRP Threshold |
In this large nationally representative cohort followed for over two decades, we found that Lp(a) was associated with both CVD and cancer mortality only in individuals with relatively higher CRP levels. Our findings suggested that, inflammation may mediate the effect of Lp(a) on dual risk of CVD and cancer mortality. Recent analyses in MESA3 (Multi-Ethnic Study of Atherosclerosis) demonstrated that Lp(a) was related to incident CVD only with concomitant systemic inflammation. Our results are partially in accordance with this observation, suggesting that the Lp(a)-related risk of CVD mortality is evident only in participants with systemic inflammation. Meanwhile, with a larger sample size and a longer-term follow-up, our study expanded prior findings by focusing not only on CVD but also on cancer mortality, indicating that concomitant elevation of Lp(a) and inflammation may increase both CVD and cancer mortality risk. This implies that the Lp(a)-related risk may be inflammation-dependent in terms of not only atherosclerotic process, but also carcinogenesis.5 This finding may provide new insights into the role of inflammation in collaborative prevention and treatment strategies of CVD and cancer. Despite a large representative cohort and long-term follow up, there are limitations. First, although plasma Lp(a) levels remain relatively stable over the life course regardless of lifestyle, Lp(a) and other biomarkers were assessed only at baseline, which may lead to potential bias. In addition, given the observational nature of our study, further experimental and randomized studies are warranted to confirm our findings.
Ethics Approval and Informed Consent
All the participants provided written informed consent. The Research Ethics Review Board of the National Center for Health Statistics approved the NHANES III (https://www.cdc.gov/nchs/nhanes/irba98.htm). Data and materials produced by the US Centers for Disease Control and Prevention (CDC) are in the public domain and can be used without permission.
Acknowledgment
We wish to thank NHANES program for their effort on data collection and sharing. Yangang Wang and Hongwei Ji are senior authors.
Funding
This study was funded in part by the National Key R & D Program of China (2022YFC2502800), National Natural Science Foundation of China (82103908), the Shandong Provincial Natural Science Foundation (ZR2021QH014), the Shuimu Scholar Program of Tsinghua University, and National Postdoctoral Innovative Talent Support Program (BX20230189). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Koene RJ, Prizment AE, Blaes A, et al. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133:1104–1114. doi:10.1161/circulationaha.115.020406
2. Tsimikas S, Mallat Z, Talmud PJ, et al. Oxidation-specific biomarkers, lipoprotein(a), and risk of fatal and nonfatal coronary events. J Am Coll Cardiol. 2010;56(12):946–955. doi:10.1016/j.jacc.2010.04.048
3. Zhang W, Speiser JL, Ye F, et al. High-sensitivity C-reactive protein modifies the cardiovascular risk of lipoprotein(a): multi-ethnic study of; atherosclerosis. J Am Coll Cardiol. 2021;78:1083–1094. doi:10.1016/j.jacc.2021.07.016
4. National Center for Health Statistics (US). Plan and operation of the third national health and nutrition examination survey, 1988–94. Series 1: programs and collection procedures. In: Vital and Health Statistics Ser 1, Programs and Collection Procedures. National Center for Health Statistics (US); 1994:1–407.
5. Leiva O, AbdelHameid D, Connors JM, et al. Common pathophysiology in cancer, atrial fibrillation, atherosclerosis, and thrombosis: JACC: cardio Oncology State-of-The-Art Review. JACC CardioOncol. 2021;3(5):619–634. doi:10.1016/j.jaccao.2021.08.011
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.