Back to Journals » Clinical Interventions in Aging » Volume 19
Integrating Fall Prevention Strategies into EMS Services to Reduce Falls and Associated Healthcare Costs for Older Adults
Authors Camp K , Murphy S, Pate B
Received 9 December 2023
Accepted for publication 13 March 2024
Published 22 March 2024 Volume 2024:19 Pages 561—569
DOI https://doi.org/10.2147/CIA.S453961
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Kathlene Camp,1 Sara Murphy,1 Brandon Pate2
1Department of Internal Medicine and Geriatrics, University of North Texas Health Science Center, Fort Worth, TX, USA; 2Mobile Integrated Healthcare, MedStar Mobile Healthcare, Fort Worth, TX, USA
Correspondence: Kathlene Camp, Department of Internal Medicine and Geriatrics, University of North Texas Health Science Center, 855 Montgomery Street, Suite 459, Fort Worth, TX, 76107, USA, Tel +1-817-735-0402, Email [email protected]
Purpose: The purpose of this study is to detail the implementation of fall prevention initiatives through emergency medical services (EMS) and associated outcomes.
Methods: Paramedics with MedStar Mobile Healthcare utilized the Stopping Elderly Accidents, Deaths, and Injuries (STEADI) fall prevention model to screen and direct intervention through 9-1-1 emergency response, High Utilization Group (HUG), and 30-day Hospital Readmission Avoidance (HRA) programs. Outcomes from 9-1-1 calls measured the number of older adults screened for falls and identified risk factors. The HUG and HRA programs measured change in quality of life with EuroQol-5D, referral service utilization, falls, emergent healthcare utilization, and hospital readmission data. Analysis included costs associated with reduced healthcare usage.
Results: Emergency paramedics provided fall risk screening for 50.5% (n=45,090) of adults aged 65 and older and 59.3% were at risk of falls, with 48.1% taking medications known to increase the risk of falls. Services provided through the HUG and HRA programs, along with additional needed referral services, resulted in a 37.2% reduction in fall-related 9-1-1 calls and a 29.5% increase in overall health status related to quality of life. Analysis of the HUG program revealed potential savings of over $1 million with a per-patient enrolled savings of $19,053. The HRA program demonstrated a 16.4% hospital readmission rate, in comparison to a regional average of 30.2%, and a cost-savings of $4.95 million or $15,618 per enrolled patient.
Conclusion: Implementation of the STEADI model into EMS services provides an effective and cost-saving model for addressing fall prevention for older adults, provides meaningful and impactful improvement for older adults, and could serve as a model for other EMS programs.
Plain Language Summary: This study explored the feasibility and impact of implementing an evidence-based fall prevention model into emergency medical services for older adults. The outcomes resulted in an efficient and effective manner to screen older adults for falls during emergency response services and connect high-risk older adults with in-home follow-up care from community paramedics. In addition, fall prevention services were provided for vulnerable adults following a recent discharge from hospital care. These initiatives to address fall prevention resulted in a majority of older adults receiving preventive fall risk screening during emergency response calls, significant changes in quality of life measures for adults with multiple comorbidities and fall risk, and significant potential cost savings in reduced healthcare services.
Keywords: fall prevention, emergency providers, Mobile Integrated Healthcare, paramedics, age-friendly
Introduction
Falls are the leading cause of injury among adults aged ≥65 years in the United States. In 2018, there were an estimated 3 million emergency department (ED) visits, more than 950,000 hospitalizations or transfers to another facility (eg, trauma center), and approximately 32,000 deaths resulting from fall-related injuries among older adults.1 These numbers are expected to rise with a growing aging population. In 2022, 17.3% of the population, or approximately 1 in 6 individuals, was 65 or older.2
The cost of falls is significant for the individual, including the loss of functional independence and even possible mortality. Additionally, healthcare costs are associated with hospitalization, medical care, and potential surgical intervention. According to Burns et al, the average cost of a hospitalization, emergency department visit, and an office-based or outpatient visit was $29,562, $4673, and $5625, respectively.3 In 2015, the total cost of fatal and non-fatal falls was estimated at $50 billion4 and that spending has likely increased with our growing aging population. However, significant medical costs have been averted even with implementing a single intervention.5 Falls are shown to be preventable with multifactorial assessments6,7 and interventions including home modifications,5,7 exercise,8,9 and balance training.10 Systematic implementation of fall prevention strategies into workflow processes11,12 and integration into electronic health record documentation12 has been shown to help clinical teams reduce falls in older adults.
Emergency medical services (EMS) are often the first responders to emergent care in the community and coordinate needs with an extended healthcare team. Beyond addressing immediate medical needs and potential ED transportation, they also play a role in non-emergent care. Community Paramedicine (CP), also known as Mobile Integrated Healthcare (MIH), is a patient-centered healthcare model in which EMS clinicians provide regularly scheduled visits in the patient’s home to address health condition management. In 2014, the National EMS Advisory Council (NEMSAC) set a vision, the EMS Agenda 2050, to advance EMS services to deliver a people-centered EMS system.13 This initiative includes delivering evidence-based clinical care and a healthcare system focused on preventing injuries and illness rather than simply responding to and treating them.
Prior research has indicated that fall prevention quality improvement (QI) strategies are multi-faceted and often require a case management approach.14 The Centers for Disease Control and Prevention’s Stopping Elderly Accidents, Deaths, and Injuries (STEADI) initiative15 was developed as a multifactorial approach to fall prevention, and its effectiveness with implementation has been studied in primary care,11,16 community pharmacy-based intervention,17 and within the ED.18 Prior research utilizing paramedics responding to 9-1-1 calls for falls and implementing a fall prevention initiative resulted in the limited adoption of recommendations and a preference for in-home programs.19 However, no studies have addressed the use of EMS providers to screen and implement fall prevention interventions using the STEADI model. In this report, we provide findings on the implementation and effectiveness of screening and follow-up care provided by EMS providers to address fall prevention for older adults.
Methods
Initiative
In 2018, five paramedics from the MedStar Mobile Healthcare MIH team engaged in leadership training with the University of North Texas Health Science Center (UNTHSC) Geriatric Workforce Enhancement Program’s (GWEP) Geriatric Practice Leadership Institute (GPLI) to attain knowledge on leading quality improvement initiatives to enhance healthcare delivery and improve the lives of older adults. Training included using quality improvement tools from the Institute for Healthcare Improvement (IHI) to guide implementation strategies and process improvement.20 The MIH team’s project utilized the IHI Improvement Project Roadmap15 to implement a fall prevention initiative through EMS services. The initiative consisted of two parts: 1) identify individuals at high risk for falls and 2) refer and enroll of high-risk individuals into a relevant MIH program.
Providers and Setting
MedStar Mobile Healthcare is located within Fort Worth, Texas, and provides care within the city and 14 nearby suburban cities covering 434 square miles. A fleet of 75 ambulances responds to 9-1-1 calls. Twenty-seven community paramedics provide expanded in-home services within the MIH program, with 63% of services going to adults 65+ years of age.
Patients and Enrollees
Emergency paramedics identify eligible patients first by screening their age, ≥65, during 9-1-1 calls. Then, if appropriate to the medical situation, the patient or their caregiver are engaged in initial fall risk screening with emergency paramedics. The MIH team receives referrals for patients at high risk for falls in two ways. The first source of referrals is 9-1-1 providers. Patients deemed at high risk for falls by 9-1-1 providers are provided the option to receive expanded services with enrollment in the MIH High Utilization Group program (HUG). The second source of referrals is hospitals and insurance companies. Patients who are deemed at high risk for falls by hospitals are offered enrollment into the Hospital Readmission Avoidance (HRA) program.
Interventions
9-1-1 Emergency Response Fall Risk Screening
At the time of the 9-1-1 call response, paramedics provide an inquiry guided by the STEADI Stay Independent6 fall risk questionnaire to screen all individuals aged 65 years and older for fall risk factors, or their caregivers by proxy as needed. In addition, paramedics review prescriptions or supplements for possible inappropriate medications using the EMR-embedded Beer’s Criteria.21 A modified home environment assessment identifies fall risk factors within the home and home-entry such as clutter, uneven surfaces, loose carpeting, uneven surfaces, and damaged steps. Individuals deemed at high-risk due to a pattern of frequent 9-1-1 calls from poorly managed health conditions which could lead to falls or who are repeated fallers are offered enrollment in the HUG program to receive in-home follow-up care to further assess and provide directed intervention towards identified risk factors.
High Utilization Group (HUG) Program
Community paramedics with the MIH team receive the referral from the 9-1-1- team and contact patients to expand in-home care to further assess and intervene for identified risk factors. Services are provided at a frequency of twice-weekly visits for twelve weeks. The STEADI functional assessments,15 Timed Up and Go (TUG), 30-Second Chair Stand Test, and 4-Stage Balance Test, are performed to assess for physical deficits. In addition, paramedics perform a home safety assessment using the Check for Safety brochure.15 Providers use a motivational interviewing approach to identify patient-centered goals and establish action steps to address risk factors identified during screening. They then connect with community services (ie, home health services, optometry, podiatry, and Area Agency on Aging) based on individual needs.
Hospital Readmission Avoidance (HRA) Program
Referrals are received from local hospital and insurance companies in preparation of patient’s discharge to home. Fall risk assessment is provided as described prior with the HUG program. Services are initiated within 48 hours of discharge and are provided twice a week for four weeks in coordination with additional services, ie home health providers.
Study of the Intervention
A retrospective study design was used to examine patient data for those enrolled in the MIH Program from 2019 to 2022. Since MedStar is our service area’s exclusive ambulance service provider, we can track all 9-1-1 calls for patients enrolled in the MIH program. When a patient is enrolled, the EHR pulls their previous year’s 9-1-1 calls. Once they graduate, the EHR will continue to pull their 9-1-1 encounters until one year after graduation. We also used this data to estimate the economic impact of the intervention program. Additionally, quality-of-life data measured by the EuroQol-5 Dimension was obtained before and after the intervention. This research study #2021-127 was approved as exempt from human subject research by the North Texas Regional Institutional Review Board due to being a demonstration project with public benefit.
Measures
The STEADI initiative provides an evidence-based approach for EMS services to address multiple factors identified to impact fall risk. The STEADI clinical resources15 provide the tools to screen, assess, and direct intervention. In addition, the Beer’s Criteria21 guides potentially inappropriate medications which could increase fall risks. To address primary preventive action, technology specialists integrated automated processes within the EMR to support medication screening, fall risk screening documentation, interventions, and track data on falls, hospitalizations, and emergent medical attention incidents.
In addition to the outcomes associated with screening and intervention, the MIH team utilized the EuroQol-5 Dimension (EQ-5D-3L) tool to evaluate quality of life, which covers five dimensions of health (mobility, self-care, usual activities, pain or discomfort, and anxiety or depression) with three levels of severity in each dimension (no problems, some problems, extreme problems).22 An additional visual analog scale (E.Q. -VAS) is delivered to assess “how good or bad is your health today?” (0=worst health you can imagine, 100=best health you can imagine).21 The tool converts results to an index value that reflects how good or bad a health state is based on the preferences of the general population of a country/region. A score of 10 is the most favorable score.22
Providers collected data on emergency care use, hospital admission during the intervention, and trends in utilization one year before and one year after the intervention. Additionally, the incidence of fall-related 9-1-1 calls in the intervention group was tracked before and after the intervention. A summary of the programs, interventions, and outcomes measured is shown in Table 1.
 |
Table 1 Provider Service Intervention |
Analysis
The number of 9-1-1 calls for falls one year before the intervention was compared to the number of calls one-year post-intervention using a one-tailed, paired-t test for individuals in the HUG and HRA programs. Additionally, calls requiring transport to the ED one year before the intervention and one-year post-intervention were compared using a one-tailed, paired-t test for both groups. Patient quality of life before and after the intervention was also compared using a one tailed, paired-t test. The cost avoidance of ambulance transport, ED visits, and hospital admissions is calculated using an estimated number of incidents avoided times an estimated cost for each service from available data sources.23–25 The estimated number of incidents avoided is calculated assuming any reduction in the number of incidents the year following the baseline data collection year is due to the intervention. For example, if Patient A had 8 ED visits in the year prior to the intervention and 2 ED visits in the year following the intervention, the estimated cost avoidance for this patient would be the estimated ED visit cost times six visits that are avoided. These costs are also presented in aggregate across all patients in the program.
Results
Emergent 9-1-1 calls for older adults resulted in 50.5% (n=45,090) of individuals aged ≥65 years old being screened for risk of falls using the fall risk inquiry. Following screening, 59.3% (n=26,739) of individuals were determined to be at risk of falls due to a score of ≥4 on the fall risk inquiry. Additionally, the EMR data identified that 48.1% (n=21,673) of older adults were using medications that were potentially inappropriate based on Beer’s Criteria21 which could have a detrimental influence on fall risk.
From 2019 to 2022, there was a 250% increase in enrollment for individuals receiving fall risk screening and intervention within the MIH services. Over the four years, 767 older adults received care, which included fall risk screening and active steps to mitigate fall risk using the STEADI model. In the year before the intervention, EMS responded to 43 fall-related 9-1-1 calls on patients enrolled in the HUG compared to 27 fall-related 9-1-1 calls in the year following the intervention, resulting in a 37.2% reduction.
For those that had previously had a fall, the number of falls in the year after the intervention was significantly lower than the number of falls in the year before the intervention for both the HUG group and the HRA group (t(22) = 2, p = 0.027 for the HUG group; t(93) = 5.4, p < 0.001 for the HRA group). Results of the paired-t test also indicated that there is a significant difference in the number of calls that required transport for both the HUG group and the HRA group (t(15) = 1.9, p = 0.041 for the HUG group; t(73) = 5.7, p < 0.001 for the HRA group).
For enrollees who completed pre and post quality of life surveys (n=539), EuroQol scores demonstrated a significant change across all five categories of patient-reported health outcomes, with a 29.5% improvement in overall health status. A breakdown of change over all five categories measured can be seen in Table 2.
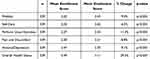 |
Table 2 Quality of Life (EuroQol) Before and After MIH Enrollment (65+ Only) |
For the 90-day High Utilization Group (HUG) program, an analysis revealed potential cost-savings avoidance of ambulance service, ED visits, and hospital admissions, resulting in savings of over $1 million with a per patient enrolled savings of $19,053. For a breakdown of projected costs and avoidance data, see Table 3. Additionally, cost savings of $4.95 million, or $15,618 per patient enrolled, is demonstrated within the HRA program. Enrollees of this program experience a 16.4% hospital readmission rate, compared to an average rate of 30.2% for referrals who did not engage with HRA, resulting in a 45.6% reduction in 30-day readmissions. See Table 4.
 |
Table 3 Cost Savings for the High Utilization Group (HUG) Program |
 |
Table 4 Cost Savings for the 30-Day Hospital Readmission Avoidance (HRA) Program |
Discussion
The high incidence of falls, fall-related injuries, and associated healthcare costs require continued attention from healthcare providers to address this pertinent issue of older adults. EMS services provide a frontline opportunity to address the burden of falls through in-home screening and follow-up intervention. Implementation of the CDC’s STEADI clinical inquiry and assessment tools into the EMR and workflow was identified as a key component in fall prevention5 and confirmed previous research findings that EMS services can provide an efficient method to deliver fall risk screening19 and our results indicated more than 50% of 9-1-1 call recipients, age ≥65, received fall risk screening. Over 59% indicated a risk for falls based on the 12-item inquiry alone; yet, additional research suggests this could effectively be reduced to a 3-item inquiry.11 Also, over 48% were taking medications which have high evidence and strong recommendations indicating a potential contributor to fall risk.21 Our study findings also revealed 14.6% of 9-1-1- calls for adults 65+ years old were fall-related, slightly lower than a 17% nationally reported average.26 The use of 9-1-1 call patterns has also been identified as a potential resource to target fall prevention strategies.27 In addition, providing these services within the home environment provides a unique opportunity to view the home environment for hazards that can negatively impact safe mobility which has been found to both reduce the rate of falls and risk of falling when performed by occupational therapists,7 but the efficacy had not yet been demonstrated with other providers.
Referrals from 9-1-1 paramedics to the MIH program allowed community paramedics to provide follow-up care to address identified risk factors, which aligned with recommendations to use 9-1-1 call patterns to identify and target older adults for fall prevention and medical monitoring strategies.27 From 2019 to 2022, there was a 250% increase in enrollment for individuals receiving fall risk screening and intervention within the MIH services due to engaging with local hospitals and community services.
EMS services to address fall risk and health condition management resulted in significant potential healthcare-related cost savings. For MIH enrollees, a reduction in emergency medical services demonstrated potential savings by avoiding ambulance transportation, emergency care, and hospital admission. Over the four years, an estimated $1 million in ED cost savings and an estimated $5 million in hospital-related readmission costs were avoided resulting in significant savings for payers and hospitals. This cost may even be an underestimation of savings since these figures were based on all-cause ED and hospitalization usage in comparison to specific fall-related healthcare costs estimated to be almost three times higher.3
A significant improvement in quality of life, as indicated across all five dimensions of health status, was recognized for enrollees through the EuroQol survey instrument. Researchers noted a reduction of 37.2% in fall-related 9-1-1 calls due to actions customized based on screenings. Previous research indicates that addressing multiple risk factors can decrease the rate of falls by 24%.7 The frequency of visits may have had a role in solidifying patient engagement and providing sufficient follow-up to action steps, as suggested as a focus to strengthen patient–clinician partnerships.28 Improved quality of life and reduced falls often result in individuals remaining in their homes for an extended period, providing cost-savings associated with caregiver or assisted-care living options.
The ability to measure outcomes associated with enhanced quality of life and fall reduction provides a powerful message to older adults, families, and communities desiring to support aging in place. Simultaneously, the cost-savings for reducing costs associated with effective transitions in care and health condition management within the home will likely convince payers of the value of the role of emergency responders as extended healthcare providers in preventive care. Future research could benefit from exploring the specific outcomes related to addressing fall prevention with the most complex patients, including a closer look at those with multiple comorbidities29 or cognitive impairment30 which have been reported to require enhanced attention.
Integrating workflow processes to address fall risk reduction during emergency response services required coordination and collaboration with key stakeholders. Initial programming and technology support were needed to incorporate Beer’s Criteria into the EMR, not including time to review and implement annual updates. The yearly training and onboarding process to educate current and new paramedics on the tools and documentation of fall risk screening, medication review, home safety observation, and mitigation of the identified risk factors also took time and coordination. This pool of staff and resources may serve as a barrier to smaller EMS service providers with limited budgets. Collaboration with hospital partners, insurance payers, and community organizations who may have shared or aligned goals could assist with leveraging resources to implement services and promptly evaluate outcomes.
A collaborative approach to addressing fall prevention provides additional opportunities to assess community programs and resources to address the identified needs of older adults in preventing falls. Current anecdotal findings indicate that individuals could be connected to the needed resources and intervention. However, limited data describing specific interventions, adherence, and barriers to completing recommendations are available. Future research could explore methods to collect and share information among community partners and primary care providers to measure the uptake and effectiveness of programs that address risk factors for fall prevention.
This study revealed positive outcomes with an EMS-driven initiative to implement fall risk screening and implementation. The details of this study could serve as a model for other EMS organizations to implement fall prevention initiatives within their service lines.
Limitations
Although this initiative and study revealed significant outcomes associated with decreasing risk of falls and associated healthcare costs, results may differ in other EMS services areas of the state or nation. MedStar is the primary emergency service for this region. Other regions may have multiple EMS service providers. Smaller EMS organizations may also not have the resources to support the staff to implement training and workflow changes. Although there was a rise in referrals over the time period of this study, there were a number of individual referrals who refused the program which may bias the intervention to those more prone to behavior change or adherence to recommendations. And despite MedStar’s expanded service area which includes suburban and some rural areas, there were several individuals referred from the hospital who lived outside of the service area and may be more vulnerable due to limited resources in rural areas. Also, this was not a randomized controlled trial, and there may be potential variation in individual responses, but this does reveal a pragmatic approach to the variation of clients in real-life application.
Conclusion
In conclusion, this study was performed to determine the ability and impact of implementing an evidence-based fall prevention model into emergency medical services for community-dwelling older adults. Implementation of the STEADI resources and Beer’s Criteria into EMS services provides an effective and cost-saving model for addressing fall prevention for older adults. With improved quality of life scores, significant healthcare cost savings, and reduced hospital readmissions, this intervention could be a model for implementing fall prevention initiatives into other EMS programs. Additionally, this model can provide important data to demonstrate the value of the role of emergency responders as extended healthcare providers in preventive care.
Funding
This project was supported by grant funding from the Health Resources and Services Administration (HRSA), US Department of Health and Human Services (HHS), under grant number U1QHP28735.
Disclosure
The author(s) report no conflicts of interest in this work.
References
1. Moreland B, Kakara R, Henry A. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years - United States, 2012–2018. MMWR Morb Mortal Wkly Rep. 2020;69(27):875–881. doi:10.15585/mmwr.mm6927a5
2. Bureau USC. QuickFacts. United States Census Bureau; 2022. Available from: https://www.census.gov/quickfacts/fact/table/US/AGE775222#AGE775222.
3. Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res. 2016;58:99–103. doi:10.1016/j.jsr.2016.05.001
4. Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 2018;66(4):693–698. doi:10.1111/jgs.15304
5. Stevens JA, Lee R. The potential to reduce falls and avert costs by clinically managing fall risk. Am J Prev Med. 2018;55(3):290–297. doi:10.1016/j.amepre.2018.04.035
6. Tinetti ME, Baker DI, McAvay G, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331(13):821–827. doi:10.1056/nejm199409293311301
7. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;2012(9):Cd007146. doi:10.1002/14651858.CD007146.pub3
8. Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2017;51(24):1750–1758. doi:10.1136/bjsports-2016-096547
9. Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL. Interventions to prevent falls in older adults: updated evidence report and systematic review for the US preventive services task force. JAMA. 2018;319(16):1705–1716. doi:10.1001/jama.2017.21962
10. Thomas E, Battaglia G, Patti A, et al. Physical activity programs for balance and fall prevention in elderly: a systematic review. Medicine. 2019;98(27):e16218. doi:10.1097/md.0000000000016218
11. Eckstrom E, Parker EM, Lambert GH, Winkler G, Dowler D, Casey CM. Implementing STEADI in academic primary care to address older adult fall risk. Innov Aging. 2017;1(2):igx028. doi:10.1093/geroni/igx028
12. Casey CM, Parker EM, Winkler G, Liu X, Lambert GH, Eckstrom E. Lessons learned from implementing CDC’s STEADI falls prevention algorithm in primary care. Gerontologist. 2017;57(4):787–796. doi:10.1093/geront/gnw074
13. Bergsten D, Gausche-Hill M, Gienapp A, et al. EMS Agenda 2050: a people-centered vision for the future of emergency medical services. Report no. DOT HS 812 664. Washington, DC: NHTSA; 2019. Available from: https://www.ems.gov/issues/planning-for-The-future-ems-agenda-2050/.
14. Tricco AC, Thomas SM, Veroniki AA, et al. Quality improvement strategies to prevent falls in older adults: a systematic review and network meta-analysis. Age Ageing. 2019;48(3):337–346. doi:10.1093/ageing/afy219
15. STEADI-Older adult fall prevention. Centers for Disease Control and Prevention website; 2023. Available from: https://www.cdc.gov/steadi/index.html.
16. Johnston YA, Bergen G, Bauer M, et al. Implementation of the stopping elderly accidents, deaths, and injuries initiative in primary care: an outcome evaluation. Gerontologist. 2019;59(6):1182–1191. doi:10.1093/geront/gny101
17. Blalock SJ, Ferreri SP, Renfro CP, et al. Impact of STEADI-Rx: a community pharmacy-based fall prevention intervention. J Am Geriatr Soc. 2020;68(8):1778–1786. doi:10.1111/jgs.16459
18. Greenberg MR, Goodheart V, Jacoby JL, et al. Emergency department stopping elderly accidents, deaths and injuries (ED STEADI) program. J Emerg Med. 2020;59(1):1–11. doi:10.1016/j.jemermed.2020.04.019
19. Phelan EA, Herbert J, Fahrenbruch C, Stubbs BA, Meischke H. Coordinating care for falls via emergency responders: a feasibility study of a brief at-scene intervention. Front Public Health. 2016;4:266. doi:10.3389/fpubh.2016.00266
20. Quality Improvement Essentials Toolkit. Institute for Healthcare Improvement website; 2017. Available from: https://www.ihi.org/resources/tools.
21. Semla TP, Steinman M, Beizer J, et al. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71(7):2052–2081. doi:10.1111/jgs.18372
22. EQ-5D-3L. EUROQOL website. Available from: https://euroqol.org/eq-5d-instruments/eq-5d-3l-about/.
23. Yun J, Oehlman K, Johansen M. Per visit emergency department expenditures by insurance type, 1996–2015. Health Aff. 2018;37(7):1109–1114. doi:10.1377/hlthaff.2018.0083
24. McDermott KW, Elixhauser A, Sun R. Trends in hospital inpatient stays in the United States, 2005–2014. Available from: www.hcup-us.ahrq.gov/reports/statbriefs/sb225-Inpatient-US-Stays-Trends.pdf.
25. Kwok CS, Abramov D, Parwani P, et al. Cost of inpatient heart failure care and 30-day readmissions in the United States. Int J Cardiol. 2021;329:115–122. doi:10.1016/j.ijcard.2020.12.020
26. Faul M, Stevens JA, Sasser SM, et al. Older adult falls seen by emergency medical service providers: a prevention opportunity. Am J Prev Med. 2016;50(6):719–726. doi:10.1016/j.amepre.2015.12.011
27. Quatman CE, Anderson JP, Mondor M, Halweg J, Quatman-Yates C, Switzer JA. Frequent 911 fall calls in older adults: opportunity for injury prevention strategies. J Am Geriatr Soc. 2018;66(9):1737–1743. doi:10.1111/jgs.15457
28. McMahon SK, Greene EJ, Latham N, et al. Engagement of older adults in STRIDE’s multifactorial fall injury prevention intervention. J Am Geriatr Soc. 2022;70(11):3116–3126. doi:10.1111/jgs.1798
29. Morris RL, Hill KD, Ackerman IN, et al. A mixed methods process evaluation of a person-centred falls prevention program. BMC Health Serv Res. 2019;19(1):906. doi:10.1186/s12913-019-4614-z
30. Thorsteinsdottir B, Peterson SM, Naessens JM, et al. Care transitions program for high-risk frail older adults is most beneficial for patients with cognitive impairment. J Hosp Med. 2019;14(6):329–335. doi:10.12788/jhm.3112
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
