Back to Journals » Clinical Interventions in Aging » Volume 19
Predictive Value of Nutritional Risk for All-Cause Death and Functional Outcomes in Chinese Elderly Patients with Acute Stroke: A 3-Year Follow-Up Study
Authors Cong WJ, Liu ZP, Liang YX, Ye SL, Cai ZM, Chen HM, Liao CW, Lin QL, Feng RQ, Zhou XD, Wu YZ, Sun LQ, Huang XR, Zhang MM, Huang GQ, Zhu BL
Received 28 October 2023
Accepted for publication 9 January 2024
Published 17 January 2024 Volume 2024:19 Pages 109—118
DOI https://doi.org/10.2147/CIA.S447038
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Wen-Jie Cong,1,* Zhi-Peng Liu,2,* Yi-Xin Liang,2 Sheng-Lie Ye,2 Zhong-Ming Cai,2 Hao-Man Chen,2 Cheng-Wei Liao,2 Qun-Li Lin,3 Ren-Qian Feng,2 Xu-Dong Zhou,4 Yan-Zhi Wu,2 Le-Qiu Sun,5 Xue-Rong Huang,6 Man-Man Zhang,7 Gui-Qian Huang,8 Bei-Lei Zhu7
1Department of Acupuncture and Physiotherapy, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China; 2The First Clinical School, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China; 3Department of Neurology, Yongjia People’s Hospital, Wenzhou, Zhejiang, People’s Republic of China; 4Department of Neurology, Pingyang People’s Hospital, Wenzhou, Zhejiang, People’s Republic of China; 5Department of Neurology, Affiliated Yueqing Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, People’s Republic of China; 6Department of Neurology, Ruian People’s Hospital, Wenzhou, Zhejiang, People’s Republic of China; 7Department of Neurology, The First Affiliated Hospital of Wenzhou Medical University Wenzhou Zhejiang People’s Republic of China; 8School of Mental Health, Wenzhou Medical University, Wenzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Bei-Lei Zhu, Tel +86 13567896076, Email [email protected]
Purpose: To explore the predictive value of nutritional risk for all-cause death and functional outcomes among elderly acute stroke patients.
Patients and Methods: A total of 479 elderly acute stroke patients were enrolled in this study. The nutritional risk of patients was screened by the GNRI and NRS-2002. The primary outcome was all-cause death, and the secondary outcome was poor prognosis defined as a modified Rankin Scale (mRS) score ≥ 3.
Results: Based on the NRS-2002, patients with nutritional risk had a higher risk of all-cause death at 3 months (adjusted OR: 3.642, 95% CI 1.046~12.689) and at 3 years (adjusted OR: 2.266, 95% CI 1.259~4.076) and a higher risk of adverse functional outcomes at 3 months (adjusted OR: 2.748, 95% CI 1.518~4.972. Based on the GNRI, compared to those without nutritional risk, patients with mild malnutrition also had a higher risk of all-cause death at 3 months (adjusted OR: 7.186, 95% CI 1.550~33.315) and at 3 years (adjusted OR: 2.255, 95% CI 1.211~4.199) and a higher risk of adverse functional outcomes at 3 months (adjusted OR: 1.947, 95% CI 1.030~3.680), so patients with moderate and severe malnutrition had a higher risk of all-cause death at 3 months (adjusted OR: 6.535, 95% CI 1.380~30.945) and at 3 years (adjusted OR: 2.498, 95% CI 1.301~4.799) and a higher risk of adverse functional outcomes at 3 months (adjusted OR: 2.213, 95% CI 1.144~4.279).
Conclusion: Nutritional risk increases the risk of poor short-term and long-term outcomes in elderly patients with acute stroke. For elderly stroke patients, we should pay attention to early nutritional risk screening, and effective intervention should be provided to improve the prognosis of such patients.
Keywords: acute stroke, malnutrition, nutritional screening, all-cause death, GNRI, NRS-2002
A Letter to the Editor has been published for this article.
Introduction
Stroke is a serious neurological disease with a poor prognosis. Globally, stroke is the second-leading cause of death and the third-leading cause of death and disability combined.1 Elderly individuals are the main population affected by stroke. Reports indicate that over 80% of ischaemic strokes occur in individuals aged more than 65 years.2
Malnutrition is a disease with a high prevalence in elderly stroke patients due to the lack of teeth, the loss of taste, poor mobility and the complications caused by stroke involving dysphagia and cognitive impairments.3–5 Recent studies have found that malnutrition after stroke may be related to various causes of compromised intake, poor digestion and absorption, and abnormalities in metabolic levels and organ function. The screening of nutritional risk is the key first step in the evaluation of nutritional status.6 Many studies have shown that malnutritional risk is associated with poor outcomes in stroke patients.7–9 Early nutritional intervention in patients with nutritional risks improved nutritional status and prognosis. Physical function and neurocognitive function are also improved in stroke patients.10–12 Previous studies were usually conducted in stroke populations of all ages or focused on acute functional improvement and short-term prognosis. The predictive value of nutritional risk for poor prognosis, particularly long-term prognosis(including mortality), of elderly stroke patients has rarely been reported, warranting further exploration.
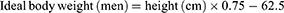
Various nutritional tools have been used for screening the risk of malnutrition.13,14 However, in clinical practice, the measurement of nutritional risk in elderly stroke patients can pose challenges due to the complications of stroke and body composition changes in elderly patients.15,16 The Nutritional Risk Screening 2002 (NRS-2002) is a nutritional screening tool widely used in clinical applications, and its effectiveness has been confirmed by many clinical studies.14,17–19 The geriatric nutritional risk index (GNRI), defined in 2005 by Bouillanne, is calculated by the serum albumin level and the ratio of body weight to ideal body weight.20 Recently, the predictive value of the GNRI for clinical outcomes in patients with heart and renal diseases has been validated in several studies.21,22 However, there is a scarcity of reports that compare of the value of these two screening tools for long-term prognostic prediction in elderly stroke patients.
The purpose of this prospective study was to explore the association between nutritional risk and short-term and long-term prognosis in Chinese elderly stroke patients. Additionally, it aimed to and compare the predictive accuracy of the GNRI with that of the NRS-2002.The results contribute to providing evidence for the study of the correlation between nutritional risk and prognosis of elderly stroke patients, as well as aid in the selection of appropriate nutritional risk screening tools.
Method
Study Population
Five major medical institutions in Wenzhou (the First Affiliated Hospital of Wenzhou Medical University, Yueqing People’s Hospital, Ruian People’s Hospital, Yongjia People’s Hospital, and Pingyang People’s Hospital) participated in this multicentre, prospective study. From October 1 to December 31, 2018, patients who were diagnosed with acute stroke (including ischaemic stroke and haemorrhagic stroke) and met the following conditions were enrolled: a) admitted to the hospitals within one week after the sudden onset of stroke; b) with evidence of acute haemorrhagic stroke (AHS) or acute ischaemic stroke (AIS) on brain computed tomography or magnetic resonance imaging scans; and c) aged over 65. Patients whose data were insufficient to calculate the NRS-2002 or GNRI were excluded from the analysis. Ethical approval was obtained from the Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University, and an approval document was signed to allow implementation. All participants provided informed consent before the investigation (Figure 1).
 |
Figure 1 Flow chart of the patient inclusion process. |
Clinical Data
Demographic data, clinical data, and laboratory data of patients were all collected. Demographic data (age, sex) and clinical data (medical history, neurological functional assessment, and medical treatment) were extracted from the electronic medical record system used in five hospitals. In addition, we supplemented the information not included in the electronic medical record system with data from the clinical visit. If the patient was unable to cooperate, we asked the patient’s relative to assist. Laboratory data were obtained from the first blood sample taken after admission. The severity of stroke was categorized following the National Institute of Health Stroke Scale score (NIHSS).23 Independence in activities of daily living (ADL) was assessed by the Barthel Index.24 Body mass index (BMI) was calculated as weight (kg) / height2 (m2).
Malnutrition Screening Tools
The nutritional risk of acute stroke patients was screened by these two scoring systems.
The GNRI is calculated through the following equation:
In our study, patients were categorized in accordance with the following cutoffs: no risk, ≥98; low risk, ≥92~98; moderate/severe risk, <92. The score component of the NRS 2002 consists of two parts: impaired nutrition status and the presence of a fatal disease. The impaired nutrition status accounts for weight loss > 5% in 3 months, reduced BMI, and the decreased food intake in recent weeks, and there is an additional point added for ≥ 70 years. These scores are then added together, and a score of ≥ 3 indicates the need for nutrition support.22,25
Outcomes
Evaluation of patient outcomes: The primary outcome measure was all-cause death at 3 months and 3 years after discharge from the hospital, and the secondary outcome measure was functional outcome measured by mRS at 3 months and 3 years. The mRS assesses functional prognosis of patients by rating their ability to live independently and their mobility limitations on a scale from 0 to 6. Patients were defined as having a poor prognosis if their mRS score ranged from 3 to 6.
Data Collection and Follow-Up
The data collection was conducted by the same investigator within 48 hours after admission, 3 months after discharge, and 3 years after discharge. We followed up with the patients by telephone at the end of 3 months and 3 years after discharge. Patients who could not be contacted by telephone were considered lost to follow-up.
Statistical Analysis
Categorical variables are expressed as frequencies and percentages. Continuous parameters are expressed as the mean ± SD or median (interquartile range) according to the result of the normality test. Normally distributed continuous variables were analysed using independent samples t-tests. Continuous variables that were not normally distributed and ordered categorical variables were analysed using the Mann‒Whitney U-test. Univariate and multivariate logistic regression statistical methods were used to investigate the relationship between nutritional risk and outcomes in elderly acute stroke patients. Collinearity was checked before regression, and a tolerance ≥ 0.1 and a variance inflation factor < 10 were considered to indicate the absence of collinearity. A P value <0.05 was considered to indicate statistical significance. Statistical analysis was performed using SPSS.26.0. The discrimination of the prediction models was quantified with the area under the receiver operating characteristic (ROC) curve (AUC), and a 95% CI was calculated for each AUC. ROC curve analysis was performed according to the methodology of DeLong et al with MedCalc ver. 20.0.27.
Results
Patient Characteristics
Among the 564 elderly patients with acute stroke who were initially enrolled, 479 were successfully followed for 3 months, and 364 remained in contact for 3 years. The patients included 278 males (58.0%), and the median age was 74 (69~80) years. Of the 479 patients, 381 (79.5%) patients had ischaemic stroke, and 98 (20.5%) had haemorrhagic stroke. The demographic data, clinical data and laboratory features of all patients are shown in Table 1.
 |
Table 1 Baseline Characteristics Stratified by the Mortality |
Nutritional Risk and Primary Outcomes
During the postdischarge follow-up, 26 (5.4%) patients died within three months, while 103 (28.3%) patients died within three years.
The individuals at risk of malnutrition at admission screened by the GNRI accounted for 66.4% (mild malnutrition: 36.7%, moderate and severe malnutrition: 29.7%), while the counterparts screened by the NRS-2002 accounted for 66.2%. The univariate regression analysis showed that nutritional risk increased the likelihood of all-cause death at both 3 months and 3 years in elderly stroke patients (Table 2).
 |
Table 2 Correlations Between at of Malnutrition Risk (Screened by NRS-2002 and GNRI) and Mortality |
The results of multivariate logistic analysis were as follows. The screening of malnutritional risk with both the NRS2002 and GNRI was independently associated with all-cause death at 3 months and 3 years. (Table 3) Upon screening with the GNRI at 3 months after discharge, the odds ratio (OR) for the effect of nutritional risk on all-cause death was 7.186 [95% CI, 1.550~33.315, p = 0.012] for mild and 6.535 [95% CI, 1.380~30.945, p = 0.018] for moderate to severe; when screened with the NRS-2002, the OR was 3.642 [95% CI, 1.046~12.689, p = 0.042]. Upon screening with the GNRI at 3 years after discharge, the OR for the effect of nutritional risk on all-cause death was 2.255 [95% CI, 1.211~4.199, p = 0.010] for mild and 2.498 [95% CI, 1.301~4.799, p = 0.006] for moderate to severe; when screened with the NRS-2002, the OR was 2.266 [95% CI, 1.259~4.076, p = 0.006].
 |
Table 3 Multivariate Logistic Analysis of the Association Between at of Malnutrition Risk (Screened by NRS-2002 and GNRI) and Mortality |
Nutritional Risk and secondary Outcomes
During the postdischarge follow-up, 140 (29.2%) patients had a poor prognosis within three months after discharge, while 172 (47.3%) patients had a poor prognosis within three years after discharge (Table 4).
 |
Table 4 Multivariate Logistic Analysis of the Association Between the Poor Prognosis and Nutritional Risk at Admission Screened by the GNRI |
At 3 months after discharge, when the GNRI was applied, the ORs of nutritional risks for poor prognosis (mRS ≥3) were 1.947 [95% CI, 1.030~3.680, p = 0.040] for mild and 2.213 [95% CI, 1.144~4.279, p = 0.018] for moderate to severe; when the NRS-2002 was applied, the OR was 2.748 [95% CI, 1.518~4.972, p = 0.001]. However, when the follow-up time was 3 years, there were no significant differences in the correlation between malnutritional risk and poor functional outcome as evaluated by either the NRS-2002 (p = 0.07) or the GNRI (p>0.1). In contrast to all-cause death, nutritional risk was only independently associated with poor prognosis at 3 months (Table 5).
 |
Table 5 Multivariate Logistic Analysis of the Association Between at of Malnutrition Risk (Screened by NRS-2002 and GNRI) and Prognosis |
Comparison of the Effects of Malnutritional Risk Screened by the GNRI and NRS-2002 on Mortality and Poor Prognosis
In the ROC analysis (Figure 2), based on the area under the curve, the GNRI and NRS-2002 performed similarly in predicting 3-month (0.848 vs 0.827) and 3-year (0.727 vs 0.731) mortality and 3-month functional outcome (0.870 vs 0.876) (p>0.05).
Discussion
To explore the association between malnutritional risk and short-term and long-term outcomes in elderly stroke patients, we conducted this prospective, multicentre study. Attributed to different screening times, ages and stroke subtypes, nutritional risk in patients with acute stroke varies widely.15,26 Sato et al and Siotto et al reported that the scores of nutritional risk changed after rehabilitation.27,28 The results of our study demonstrated that nutritional risk was associated with age (GNRI: p < 0.010, NRS-2002: p < 0.010), which deserves clinical attention. In hospitalized AIS patients of all ages, the prevalence of nutritional risk ranged from 35.0–50.0%,29–31 while the prevalence in patients aged 65 and older ranged from 17.2~53.8%.8,9,32–34 In our study, the percentages of individuals at risk of malnutrition screened by the GNRI were 66.3% (mild malnutrition: 36.7%, moderate and severe malnutrition: 29.6%), and the percentages screened by the NRS-2002 were basically equal (66.3% vs 66.2%, p > 0.05).The prevalence of nutritional risk in the sample population of this study paralleled findings from previous studies.35
The main prognostic indicators in this study were all-cause death at 3 months and 3 years. Previous studies focused on the predictive value of malnutritional risk for poor functional outcomes in stroke patients, and the duration of the studies was usually short. In our previous study, the risk of malnutrition was possibly predictive of poor outcomes at 3 months in AIS and acute haemorrhagic stroke (AHS).36,37 Recent studies have demonstrated that nutritional risk assessed by the NRS-2002 is independently associated with in-hospital mortality in hospitalized patients.38 The results of a Korean single-centre prospective registry study that enrolled 1906 patients with stroke suggested that severe nutritional risk was associated with poor 3-month outcomes. The results of a large-scale Chinese study involving 15,166 patients with AIS also supported the proposition that patients with moderate to severe nutritional risk were more likely to have adverse 1-year outcomes.8 However, the association between nutritional risk and long-term all-cause death in elderly stroke patients has been reported on in only a few studies. A previous study illustrated that nutritional risk was associated with four-year mortality in older adults with acute ischaemic stroke.9 Our study and the results of that study complement each other to further verify that the risk of malnutrition at admission is related to the long-term mortality of elderly patients with stroke.
Our secondary outcome was poor outcomes defined as mRS score ≥3. We found that malnutritional risk showed a good predictive value for 3-month functional outcomes, which was consistent with most studies.8,39,40 However, the association between the risk of malnutrition and poor prognosis diminished at 3 years after discharge. Possible reasons are described below. In our study, an mRS of ≥3 was considered an indicator of poor outcomes, and a score of 3 denoted “moderate disability”, that is, represented by an individual who prefers some assistance but is able to walk by himself.41,42 In other words, mRS focuses on the evaluation of walking ability. However, in practice, many stroke patients choose to participate in postdischarge rehabilitation training, which reduces disability after stroke.43,44 The neuronal plasticity processes may be modified and boosted by rehabilitative training, which results in the spontaneous recovery of patients.45 Therefore, persistent rehabilitation training after acute stroke may lead to less influence of nutritional risk on long-term prognosis. Thus, the correlation between nutritional risk and the long-term prognosis of elderly stroke patients needs to be confirmed by further studies. Additionally, a cross-sectional comparison to explore the relationship between functional changes and nutritional risk in patients without stroke is warranted.
Two nutritional screening tools were used in our study. The NRS-2002 is an ESPEN-recommended screening tool for hospitalized patients.46 An NRS-2002 score ≥3 was linked to stroke-related infections during hospitalization, high requirements for nutritional support and low ADL scores at discharge.47 The association between NRS-2002 scores and mRS was also confirmed in stroke patients with dysphagia.40 Although the NRS-2002 is reliable, its use has considerable limitations in clinical neurology, especially in elderly stroke patients. First, many elderly people do not pay attention to their weight changes before the onset of the disease. Second, the aphasia and loss of consciousness of stroke patients makes it difficult to obtain information about weight loss and disease severity.
A large amount of literature has confirmed that the GNRI has a good screening effect on the malnutritional risk of elderly patients.32,34,48–50 It is calculated by laboratory and physical indicators that can be easily collected. In the modern medical system of information expansion, the GNRI score is much more convenient and constant than NRS 2002. In our study, the comparison of the ROC curves showed that the GNRI and NRS-2002 performed with fair accuracy in all-cause death, both at 3 months (0.848 vs 0.827) and 3 years (0.727 vs 0.731) post discharge. The GNRI and NRS-2002 also performed fairly well in predicting the 3-month functional outcome (0.870 vs 0.876) (p>0.05). Of course, more representative, larger sample long-term studies are warranted to verify the accuracy and predictive performance of the 2 malnutrition scores for predicting poor outcomes in elderly stroke patients.
The strengths of our research are described below. First, our study is both prospective and multicentre. Second, the relatively long duration of this study provided an opportunity for our design of short-term and long-term observation endpoints, which can better reflect the predictive value of malnutritional risk in prognosis. Third, both ischaemic stroke and haemorrhagic stroke patients were enrolled in our study; in contrast, past studies always focused on people with ischaemic strokes only. Fourth, there were multiple indicators of observation. Not only all-cause death but also poor prognostic indicators were observed, reflecting the overall adverse effects of malnutritional risk more comprehensively.
We acknowledge several limitations to our study. First, some patients in the study were lost to follow-up, which may result in follow-up bias. Second, we did not pay attention to nutritional status and rehabilitation training after discharge. If we did, we may have been able to provide a more comprehensive picture of the interaction between nutrition and functional recovery in elderly patients with acute stroke. Third, we investigated the effects of malnutritional risk by screening tools only, and no diagnostic tools were used to further verify the results. Fourth, nutritional intervention was not performed in this study, and further research is needed on the impact of nutritional support on patients with nutritional risk.
Conclusions
Nutritional risk increases the risk of poor short-term and long-term outcomes in elderly patients with acute stroke. The GNRI may be a more suitable tool to screen nutritional risk in elderly stroke patients based on the convenience of the operation. We recommend initiating complete nutritional screenings to help with individualized nutritional care management in those with a GNRI score≤98 or an NRS-2002 score ≥3 to improve the overall prognosis of elderly stroke patients.
Acknowledgments
We thank all participating hospitals, physicians, nurses and the science committee in Wenzhou, China (Project number: Y20190561).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Feigin VL, Stark BA, Johnson CO. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20:795–820. doi:10.1016/S1474-4422(21)00252-0
2. Chen RL, Balami JS, Esiri MM, et al. Ischemic stroke in the elderly: an overview of evidence. Nat Rev Neurol. 2010;6:256–265. doi:10.1038/nrneurol.2010.36
3. Kaiser MJ, Bauer JM, Rämsch C, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58:1734–1738. doi:10.1111/j.1532-5415.2010.03016.x
4. Bullock AF, Greenley SL, McKenzie GAG, et al. Relationship between markers of malnutrition and clinical outcomes in older adults with cancer: systematic review, narrative synthesis and meta-analysis. Eur J Clin Nutr. 2020;74:1519–1535. doi:10.1038/s41430-020-0629-0
5. Feng MC, Lin YC, Chang YH, et al. The mortality and the risk of aspiration pneumonia related with dysphagia in stroke patients. J Strok Cerebrovas Dis. 2019;28:1381–1387. doi:10.1016/j.jstrokecerebrovasdis.2019.02.011
6. Cederholm T, Jensen GL, Correia MITD, et al. GLIM criteria for the diagnosis of malnutrition - A consensus report from the global clinical nutrition community. Clin Nutr. 2019;38:1–9. doi:10.1016/j.clnu.2018.08.002
7. Fluck D, Fry CH, Gulli G, et al. Association of risk of malnutrition with adverse outcomes and early support on discharge in acute stroke patients without prestroke disability: a multicenter, registry-based cohort study. Nutrit Clin Pract. 2022;37:1233–1241. doi:10.1002/ncp.10790
8. Zhang G, Pan Y, Zhang R, et al. Prevalence and prognostic significance of malnutrition risk in patients with acute ischemic stroke: results from the third china national stroke registry. Stroke. 2022;53:111–119. doi:10.1161/STROKEAHA.121.034366
9. Yuan K, Zhu S, Wang H, et al. Association between malnutrition and long-term mortality in older adults with ischemic stroke. Clin Nut. 2021;40:2535–2542. doi:10.1016/j.clnu.2021.04.018
10. Burgos R, Bretón I, Cereda E, et al. ESPEN guideline clinical nutrition in neurology. Clin Nutr. 2018;37:354–396. doi:10.1016/j.clnu.2017.09.003
11. Aquilani R, Sessarego P, Iadarola P, et al. Nutrition for brain recovery after ischemic stroke: an added value to rehabilitation. Nutr Clin Pract. 2011;26:339–345. doi:10.1177/0884533611405793
12. Yoshimura Y, Bise T, Shimazu S, et al. Effects of a leucine-enriched amino acid supplement on muscle mass, muscle strength, and physical function in post-stroke patients with sarcopenia: a randomized controlled trial. Nutrition. 2019;58:1–6. doi:10.1016/j.nut.2018.05.028
13. Power L, Mullally D, Gibney ER, et al. A review of the validity of malnutrition screening tools used in older adults in community and healthcare settings - A MaNuEL study. Clin Nutr ESPEN. 2018;24:1–13. doi:10.1016/j.clnesp.2018.02.005
14. Skipper A, Ferguson M, Thompson K, et al. Nutrition screening tools: an analysis of the evidence. JPEN J Parenter Enteral Nutr. 2012;36:292–298. doi:10.1177/0148607111414023
15. Sabbouh T, Torbey MT. Malnutrition in stroke patients: risk factors, assessment, and management. Neurocritical Care. 2018;29:374–384. doi:10.1007/s12028-017-0436-1
16. Özkaya I, Gürbüz M. Malnourishment in the overweight and obese elderly. Nutricion hospitalaria. 2019;36:39–42. doi:10.20960/nh.02062
17. van Bokhorst-de van der Schueren MA, Guaitoli PR, Jansma EP, et al. Nutrition screening tools: does one size fit all? A systematic review of screening tools for the hospital setting. Clin Nut. 2014;33:39–58. doi:10.1016/j.clnu.2013.04.008
18. Kondrup J, Allison SP, Elia M, et al. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–421. doi:10.1016/S0261-5614(03)00098-0
19. Kondrup J, Rasmussen HH, Hamberg O, et al. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–336. doi:10.1016/S0261-5614(02)00214-5
20. Bouillanne O, Morineau G, Dupont C, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutrit. 2005;82:777–783. doi:10.1093/ajcn/82.4.777
21. Fan Y, He L, Zhou Y, et al. Predictive value of geriatric nutritional risk index in patients with coronary artery disease: a meta-analysis. Frontiers in Nutrition. 2021;8:736884. doi:10.3389/fnut.2021.736884
22. Donnan GA, Fisher M, Macleod M, et al. Stroke. Lancet. 2008;371:1612–1623. doi:10.1016/S0140-6736(08)60694-7
23. Brott T, Adams HP, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20:864–870. doi:10.1161/01.STR.20.7.864
24. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42:703–709. doi:10.1016/0895-4356(89)90065-6
25. Anthony PS. Nutrition screening tools for hospitalized patients. Nutrit Clin Pract. 2008;23:373–382. doi:10.1177/0884533608321130
26. Foley NC, Martin RE, Salter KL, et al. A review of the relationship between dysphagia and malnutrition following stroke. J Rehabilit Med. 2009;41:707–713. doi:10.2340/16501977-0415
27. Sato M, Ido Y, Yoshimura Y, et al. Relationship of malnutrition during hospitalization with functional recovery and postdischarge destination in elderly stroke patients. J Strok Cerebrovas Dis. 2019;28:1866–1872. doi:10.1016/j.jstrokecerebrovasdis.2019.04.012
28. Siotto M, Germanotta M, Guerrini A, et al. Relationship between nutritional status, food consumption and sarcopenia in post-stroke rehabilitation: preliminary data. Nutrients. 2022;14:4825. doi:10.3390/nu14224825
29. Chen X, Li D, Liu Y, et al. Nutritional risk screening 2002 scale and subsequent risk of stroke-associated infection in ischemic stroke: the REMISE study. Frontiers in Nutrition. 2022;9:895803. doi:10.3389/fnut.2022.895803
30. Zhang M, Ye S, Huang X, et al. Comparing the prognostic significance of nutritional screening tools and ESPEN-DCM on 3-month and 12-month outcomes in stroke patients. Clin Nutr. 2021;40(5):3346–3353. doi:10.1016/j.clnu.2020.11.001
31. Çoban E. Malnutrition rate in stroke patients on admission. Sisli Etfal Hastanesi tip bulteni. 2019;53:272–275. doi:10.14744/SEMB.2018.81994
32. Chen Y, Yang X, Zhu Y, et al. Malnutrition defined by geriatric nutritional risk index predicts outcomes in severe stroke patients: a propensity score-matched analysis. Nutrients. 2022;14:4786. doi:10.3390/nu14224786
33. Hua J, Lu J, Tang X, et al. Association between geriatric nutritional risk index and depression after ischemic stroke. Nutrients. 2022;14:2698. doi:10.3390/nu14132698
34. Lee M, Lim JS, Kim Y, et al. Association between geriatric nutritional risk index and post-stroke cognitive outcomes. Nutrients. 2021;13:1.
35. Di Vincenzo O, Pagano E, Cervone M, et al. High nutritional risk is associated with poor functional status and prognostic biomarkers in stroke patients at admission to a rehabilitation unit. Nutrients. 2023;15:4144. doi:10.3390/nu15194144
36. Zhu BL, Wu YZ, Cai ZM, et al. A prospective epidemiological analysis of controlling nutritional status score with the poor functional outcomes in Chinese patients with haemorrhagic stroke. Br J Nutr. 2022;128:192–199. doi:10.1017/S0007114521003184
37. Cai ZM, Wu YZ, Chen HM, et al. Being at risk of malnutrition predicts poor outcomes at 3 months in acute ischemic stroke patients. Eur J Clin Nutr. 2020;74:796–805. doi:10.1038/s41430-020-0605-8
38. Bakkaloglu OK, Bektas M, Ince B, et al. Malnutrition risk in hospitalized patients measured with nutrition risk screening 2002 tool and its association with in-hospital mortality. Eur Rev Med Pharmacol Sci. 2023;27:5812–5821. doi:10.26355/eurrev_202306_32820
39. Hu J, Chen T, Wang Z, et al. Geriatric nutritional risk index and the prognosis of patients with stroke: a meta-analysis. Horm Metab Res. 2022;54:736–746. doi:10.1055/a-1886-4276
40. Liu T, Wu LY, Yang XM, et al. Influence of nutritional status on prognosis of stroke patients with dysphagia. Altern Ther Health Med. 2022;28:26–33.
41. van Swieten JC, Koudstaal PJ, Visser MC, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–607. doi:10.1161/01.STR.19.5.604
42. Broderick JP, Adeoye O, Elm J. Evolution of the modified rankin scale and its use in future stroke trials. Stroke. 2017;48:2007–2012. doi:10.1161/STROKEAHA.117.017866
43. Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet. 2011;377:1693–1702. doi:10.1016/S0140-6736(11)60325-5
44. Seidel G, Röttinger A, Lorenzen J, et al. Quality of life and disability after severe stroke and early neurological rehabilitation. Nervenarzt. 2019;90:1031–1036. doi:10.1007/s00115-019-0740-4
45. Hara Y. Brain plasticity and rehabilitation in stroke patients. J Nippon Med Sch. 2015;82:4–13. doi:10.1272/jnms.82.4
46. Serón-Arbeloa C, Labarta-Monzón L, Puzo-Foncillas J, et al. Malnutrition screening and assessment. Nutrients. 2022;14:2392. doi:10.3390/nu14122392
47. Di Vincenzo O, Luisi MLE, Alicante P, et al. The assessment of the risk of malnutrition (undernutrition) in stroke patients. Nutrients. 2023;15:683. doi:10.3390/nu15030683
48. Akimoto T, Hara M, Morita A, et al. Relationship between nutritional scales and prognosis in elderly patients after acute ischemic stroke: comparison of controlling nutritional status score and geriatric nutritional risk index. Ann Nutr Metab. 2021;77:116–123. doi:10.1159/000515212
49. Bao Y, Zhang Y, Du C, et al. Malnutrition and the risk of early neurological deterioration in elderly patients with acute ischemic stroke. Neuropsychiatr Dis Treat. 2022;18:1779–1787. doi:10.2147/NDT.S366851
50. Kakehi S, Wakabayashi H, Inuma H, et al. Rehabilitation nutrition and exercise therapy for sarcopenia. World J Mens Health. 2022;40:1–10. doi:10.5534/wjmh.200190
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.