Back to Journals » Cancer Management and Research » Volume 15
Real-World Data Analysis of Survival Outcomes and Central Nervous System Relapses in Testicular Diffuse Large B Cell Lymphoma
Authors Lee YP, Yoon SE, Cho J, Ko YH, Oh D , Ahn YC , Kim WS, Kim SJ
Received 9 February 2023
Accepted for publication 10 May 2023
Published 5 June 2023 Volume 2023:15 Pages 463—474
DOI https://doi.org/10.2147/CMAR.S407837
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Kattesh Katti
Yong-Pyo Lee,1,* Sang Eun Yoon,2,* Junhun Cho,3 Young Hyeh Ko,3 Dongryul Oh,4 Yong Chan Ahn,4 Won Seog Kim,2,5 Seok Jin Kim2,5
1Division of Hematology-Oncology, Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea; 2Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 4Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea; 5Department of Health Sciences and Technology, Samsung Advanced Institute for Health Sciences and Technology, Sungkyunkwan University, Seoul, Korea
*These authors contributed equally to this work
Correspondence: Seok Jin Kim, Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro Gangnam-gu, Seoul, 06351, Korea, Tel +82-2-3410-1766, Fax +82-2-3410-1754, Email [email protected]
Background: Primary testicular lymphoma is a rare type of non-Hodgkin lymphoma, mostly of the diffuse large B cell lymphoma (DLBCL). Although a consensus on standard treatment has been established, unresolved issues remain, such as recurrence in the central nervous system (CNS).
Methods: We retrospectively analyzed the clinical characteristics and survival outcomes of 65 testicular DLBCL patients according to clinical settings and treatment modalities.
Results: The median age of the patients in our study was 65 years, and two-thirds of them had disease limited to one testis. There was no right or left lateralization of testicular involvement. Over a median follow-up of 53.9 months (95% confidence interval 34.0– 73.7 months), patients with stage I disease and a low international prognostic index score showed better survival outcomes than those in other categories. Orchiectomy, six cycles of chemotherapy, and radiation therapy (RT) to the contralateral testis demonstrated survival benefits, whereas CNS prophylaxis therapy did not reduce CNS recurrence. During the follow-up period, the survival curves showed continuous decline, mostly due to disease progression. CNS recurrence was observed in 15% of patients, and parenchymal involvement was dominant. However, no factors were associated with CNS recurrence in our analyses. Although our molecular analyses were performed in a small number of patients, MYD88, CD79B, and PIM1 mutations were frequent.
Conclusion: In our study, treatment with orchiectomy, six cycles of immunochemotherapy, and contralateral RT was effective. However, because CNS prophylaxis is an essential part of testicular DLBCL management, better treatment strategies than intrathecal therapy are required.
Keywords: testis, diffuse large B cell lymphoma, central nervous system, survival outcome
Introduction
Primary testicular lymphoma, which accounts for less than 2% of non-Hodgkin lymphoma (NHL) cases, has similarities to extra-nodal NHL that occurs in immune-privileged sites, such as the eye and central nervous system (CNS).1 Pathologically, 80–90% of primary testicular lymphoma cases demonstrate diffuse large B-cell lymphoma (DLBCL) with non-germinal center/activated B-cell (ABC) subtype.2,3 At diagnosis, most cases of testicular DLBCL show localized disease described as stage I/II. However, distinction between stage III/IV testicular DLBCL and systemic DLBCL with secondary testicular involvement is somewhat arbitrary. The rate of advanced testicular DLBCL is less than 20%.4
Due to the rarity of testicular DLBCL, treatment strategies have been adopted based on small-scale, non-randomized, Phase 2 studies or retrospective studies.3,5–7 Currently, the standard treatment scheme is orchiectomy of the disease-involved testis, immunochemotherapy combined with rituximab, contralateral testicular radiation therapy (RT), and CNS prophylaxis with intrathecal (IT) or intravenous (IV) methotrexate (MTX).8–10 Although the ability of rituximab to penetrate immune-privileged sites, including CNS, is uncertain, previous studies have demonstrated improved survivals in testicular DLBCL when rituximab is added to the CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) regimen.8,11–14 Therefore, the standard systemic treatment for testicular DLBCL is RCHOP, as for other systemic DLBCL. However, previous results have shown that RCHOP did not mitigate CNS recurrence, and that patients who experienced CNS recurrence had dismal survival outcomes.15,16 IT or IV MTX is commonly recommended for testicular DLBCL to prevent CNS recurrence. In the IELSG-10 study, the CNS recurrence rate was 6% among stage I/II testicular DLBCL patients treated with IT MTX at a 12mg total dose, weekly for four weeks.9 In the IELGS-30 study, CNS prophylaxis consisted of four doses of IT liposomal cytarabine and two courses of IV MTX (1.5g/m2). Those researchers reported no CNS recurrences during five years of follow-up.17 However, given that the median age of testicular lymphoma patients at diagnosis is older than 65 years, the dosage and route of administration of MTX required to provide effective CNS prophylaxis remain unclear in terms of safety and efficacy.5
Therefore, we recognize the needs for research to consider novel treatment schemes, but such studies are difficult to perform due to the small number of patients. In this retrospective study, we classify the clinical features and survival outcomes of testicular DLBCL patients according to the clinical characteristics and treatment modalities. Based on our analyses, we discuss the optimal treatment modalities for resolving CNS recurrence and improving dismal survival outcomes. We also consider the prognostic factors that influence survival and CNS recurrence.
Methods
Study Analysis and Patient Collection
We collected 65 Korean patients with testicular DLBCL from two prospective observational cohort studies (NCT #01877109 and NCT #03117036) and the lymphoma registry of Samsung Medical Center between 1996 and 2021. Although the main subjects of this study were patients with primary testicular DLBCL, patients with DLBCL in other extra-nodal sites were also included. Among the 65 patients, 63 received orchiectomy for biopsy confirmation and treatment aim, and two were diagnosed with DLBCL by biopsy of a site other than the testis. Pathologic diagnosis was conducted by lymphoid malignancy pathology experts (J.C. and Y.H.K.). The cell of origin (COO) of lymphoma was determined according to the Hans algorithm.18,19 The immunohistochemistry for Bcl-2 and c-Myc was performed for the diagnosis of double-expressor type whereas we did a fluorescence in situ hybridization (FISH) using the probe for MYC, BCL2 and BCL6 to identify cases having double-hit/triple-hit lymphomas.20 We retrospectively reviewed the medical records of the patients, who were all registered in the cohorts or the lymphoma registry, after receiving approval of the Institutional Review Board of Samsung Medical Center (approval number. 2022-01-120). This study was conducted under the ethical principles of the Declaration of Helsinki and the Korea Good Clinical Practice guidelines, and written informed consent was waived due to the retrospective study nature. In this study, all data of patients accessed complied with relevant data protection and privacy regulations. The last update of survival and disease status occurred in February 2022.
We collected the following clinical and laboratory information from medical records at the time of diagnosis and during treatment and follow-up: age, complete blood count, lactate dehydrogenase (LDH), beta-2 microglobulin, Eastern Cooperative Oncology Group performance status (ECOG-PS), presence of extra-nodal site involvement, Ann Arbor stage, international prognostic index (IPI), and CNS-IPI. After reviewing the imaging results, we defined a limited stage of testicular DLBCL as cases involving one or both testes without nodal or extra-nodal involvement, and we defined the advanced stage as cases involving the testes and lymph nodes or extra-nodal sites. In addition, we analyzed the archived results of next-generation sequencing (NGS) conducted in clinical practice at diagnosis, although that analysis included only patients with tumor tissue available for targeted sequencing using HemaSCAN, which contains 425 genes associated with hematological malignancies, as previously described.21,22 Mean sequencing coverage was greater than 700x, and somatic alterations were called using a previously described pipeline.22–24
Treatment Modalities
We collected the following treatment-related information: unilateral or bilateral orchiectomy, chemotherapy, prophylactic contralateral testicular RT, and CNS prophylaxis. All patients were recommended to receive four to six cycles of chemotherapy (CHOP or RCHOP). The institute advocated for prophylactic contralateral testicular RT on patients who completed primary treatment. Irradiation was performed using a single anterior field of 12-MeV electrons or single to multiple fields of X-rays with 4–10 MV. A total dose of 30 grays in 10–15 fractions was delivered over two to three weeks. CNS prophylaxis was also recommended for all patients at a fixed dose of 15mg of MTX for IT treatment or 1.0 g/m2 MTX for IV treatment. The response rates were estimated after completion of the planned treatment modalities and were assessed by the Lugano classification for lymphoma using computed tomography scans, brain magnetic resonance imaging, and [18F] 2-fluoro-2-deoxy-D-glucose positron emission tomography in cases with measurable nodal or extra-nodal lesions.25 A small number of patients with suspected or confirmed CNS involvement underwent cerebrospinal fluid (CSF) studies before, during, or after treatment.
Statistical Analysis
Descriptive statistics are given as percentages and medians, and intergroup comparisons of categorical variables were conducted using the χ2 test or Fisher’s exact test. The Kaplan–Meier method was used to estimate overall survival (OS), progression-free survival (PFS), and event-free survival (EFS) for CNS recurrence. The OS was assessed from diagnosis to death or the last follow-up date; PFS was estimated from diagnosis to disease progression or death from any cause; and EFS was calculated from the end of treatment to the confirmation date of CNS recurrence. To elucidate factors associated with CNS recurrence and survival following the diagnosis of testicular DLBCL, we performed univariate and multivariate analyses using Cox proportional hazard models. All data were analyzed using the Statistical Package for Social Sciences software, version 24.0 (IBM Corp., Armonk, NY, USA).
Results
Patient Characteristics
The median age of patients at diagnosis was 65 years (33–83 years). More than 60% of the patients were older than 60 years, and approximately 30% of the patients were older than 70 years (Table 1). Most patients presented ECOG-PS of 0 or 1 (n = 62, 95.3%). Of the 53 (81.5%) patients who had identifiable COO, 16 (24.6%) manifested the germinal center B cell (GCB) type, and 37 (56.9%) exhibited the non-GCB type. Forty-three (66.2%) patients presented limited stage testicular DLBCL. Six patients with stage II disease having multiple intraabdominal lymph node involvement were classified as advanced disease. Three patients (4.6%) had DLBCL with bone marrow involvement, and another three (4.6%) showed kidney or adrenal gland involvement. The number of patients with elevated LDH was 25 (38.4%). Forty-two patients (64.6%) had a low-risk IPI (score 0 or 1) whereas 23 patients (35.4%) had two or more than two IPI scores. Ten (15.3%) patients had a high CNS-IPI score due to adrenal gland or kidney involvement, old age, and high LDH level (Table 1).
 |
Table 1 Baseline Demographics and Disease Characteristics at Diagnosis (n = 65) |
Treatments
Most patients were diagnosed with testicular DLBCL after orchiectomy. Although the treatment strategy after orchiectomy was systemic chemotherapy plus CNS prophylaxis followed by contralateral testicular RT, not all patients received the same treatment due to various reasons including patients’ refusal and physicians’ decision based on patients’ condition (Figure 1A). Out of 65 patients, six patients only underwent orchiectomy because they refused systemic chemotherapy whereas 59 patients received chemotherapy after orchiectomy. Most patients received RCHOP (n = 52) but seven patients who were diagnosed before 2003 received CHOP because rituximab was not used in Korea before 2003. Among 59 patients receiving chemotherapy, 49 patients received six cycles of chemotherapy. However, the remaining 10 patients received less than 4 cycles because they were elderly and frail patients including six patients older than 75 years receiving one or two cycles of chemotherapy. Basically, IT MTX injection for CNS prophylaxis was recommended in all patients, however, 30 patients received IT MTX because it was difficult to be done in elderly or uncooperative patients. Only two patients received IV administration of MTX for CNS prophylaxis based on physicians’ decision. After completion of planned chemotherapy and CNS prophylaxis, 39 patients received contralateral testicular RT at a median dose of 2750 centigrays (cGy) (range, 750–3750 cGy) in 15 fractions (range, 7–22). Of the 43 patients with limited disease, five (11.6%) received orchiectomy alone, two of whom had systemic disease progression and eventually died. The remaining 38 patients received orchiectomy and chemotherapy as primary treatment. Twenty-nine (67.4%) patients received contralateral testicular RT after primary treatment, and 20 (46.5%) received CNS prophylaxis. Seventeen patients (39.5%) received tri-modality treatment of orchiectomy, chemotherapy, and contralateral testicular RT (Figure 1A). Of the 22 patients with advanced disease, six had stage II disease, and 16 had stage IV testicular DLBCL. One patient was diagnosed with lymphoma through orchiectomy, but no further treatment was performed due to his old age and poor performance status. In addition, two patients received systemic chemotherapy immediately after diagnosis without removal of the lymphoma-involved testis due to their severe disease status. Thus, in 19 advanced-stage patients (excluding those three patients), 10 (45.5%) and 12 (54.5%) received contralateral testicular RT and CNS prophylaxis, respectively (Figure 1A).
Clinical Outcomes According to Patient Characteristics and Treatment
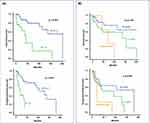
With a median follow-up duration of 53.9 months (95% confidence interval [CI] 34.0–73.7 months), the median OS and PFS for primary treatment were 138.0 months (95% CI: 86.4–189.6 months) and 92.9 months (95% CI: 25.3–160.4 months), respectively (Figure 1B). Thus, the 5-year OS and PFS were 68.2% and 55.7%, respectively. The patients diagnosed with limited-stage disease had significantly better OS (P = 0.025) and PFS (P = 0.005) than those diagnosed with advanced-stage disease (Figure 1C). In addition, patients with IPI score 0 or 1 presented better survival outcomes than patients with IPI score ≥2 (OS: P < 0.001 and PFS: P < 0.001; Figure 2A). However, the survival outcomes did not differ according to lateralization of testicular involvement (OS: P = 0.140 and PFS: P = 0.049, Figure 2B) or COO (OS: P = 0.176 and PFS: P = 0.703; Supplementary Figure 1). Moreover, we assessed PFS according to CNS-IPI and showed that it was similar among the 10 patients (15%) with high CNS-IPI score and others (P = 0.220, data not shown).
The OS of patients who received six cycles of chemotherapy showed better than that of patients receiving only one to four cycles of chemotherapy regardless of stage (Figure 3A). Although the numbers were relatively small, the OS of patients receiving CHOP was worse than that of patients receiving RCHOP (data not shown). Radiotherapy to the contralateral testis after primary treatment significantly affected OS, resulting in longer OS even in patients with advanced-stage disease (Figure 3B). However, CNS recurrence did not differ significantly between patients who received CNS prophylaxis and those who did not although late CNS relapses were observed in stage I patients who did not receive CNS prophylaxis (Figure 3C). Regardless of disease stage, patients who received tri-modality treatment, with or without CNS prophylaxis, showed better clinical outcomes than those who received bi- or mono-modality treatment (Figure 3D).
Patients with Relapsed or Progressive Disease
During the follow-up period, 22 (33.8%) patients experienced disease progression or recurrence. The clinical features and treatment course of those patients are summarized in Figure 4. Among those patients, 13 had stage I disease, and the remaining nine had advanced stage disease at the time of diagnosis. Among patients with disease progression or recurrence, 20 (91.0%) experienced distant disease relapse, and two had regional lymph node recurrence (Figure 4). Although no patient experienced disease relapse in the contralateral testis, CNS recurrence occurred in 10 patients (15.4%, Figure 4). The median time to CNS recurrence was 30.9 months (6.6–181.3 months). Among them, seven presented parenchymal CNS involvement, one showed leptomeningeal seeding, and two had both parenchymal and leptomeningeal involvement. Out of 10 (15.3%) patients having a high CNS-IPI score at diagnosis, only one patient experienced CNS relapse (Patient 19, Figure 4), thus, CNS-IPI at diagnosis was not related with CNS relapse in this study. Likewise, the CNS recurrence rate did not differ significantly according to disease stage [stage I: 16.2% (7/43) vs stage II, III, IV: 13.6% (3/22)]. Through univariate and multivariate analyses, we found prognostic variables that affected OS and PFS (Table 2). Contralateral testicular RT and good performance status (ECOG-PS 0–1) offered significant benefit to both OS and PFS. However, no variables predicted CNS recurrence (data not shown).
 |
Table 2 Univariate and Multivariate Analyses |
Mutation Profiles of Testicular DLBCL
We obtained mutation profiles of eight patients using tumor tissue samples at diagnosis (Figure 5A). The MYD88 and PIM1 mutations, commonly observed somatic mutations in primary testicular lymphoma, were found in all eight patients. In addition, CD79B, CDKN2A, HIST1H1E, PCLO, and EIF3A mutations were found in six patients (75.0%). As the number of analyzed cases was too, the impact of mutation profiles on survival could not be evaluated (Figure 5A). Out of eight patients, only one case (patient 3) died due to disease progression whereas the remaining seven patients survived without relapse at the time of analysis (Figure 5B). Patient 3 experienced repeated disease recurrence and a short first PFS of 10.1 months even though he had stage I disease and received tri-modality treatment. He showed disease recurrence in distant extra-nodal sites including bone and nasal cavity.
 |
Figure 5 Paired analysis of mutation profiles in eight patients (A) and their swimmer plot (B). |
Discussion
We retrospectively analyzed clinical characteristics of patients with primary testicular DLBCL who were histologically proven and compared survival outcomes according to their disease status and treatment modalities with the median follow-up of 53.9 months (95% CI: 34.0–73.7 months). In this study, stage I or II accounted for more than 65% and the elevation of serum LDH was observed in less than 40% of patients (Table 1). Accordingly, most patients (n = 42, 64.6%) belonged to a low-risk IPI (score 0 or 1). Nevertheless, more than 60% of patients were older than 60 years including around 30% of patients older than 70 years (Table 1). This finding suggested aggressive treatment strategies might not be possible for this disease entity. Indeed, out of 65 patients, six patients did not receive chemotherapy and 10 patients received less than 4 cycles of chemotherapy because they were elderly and frail patients. Likewise, IT MTX injection for CNS prophylaxis only could be done in less than a half of patients.
Thus, the basic treatment protocol for primary testicular DLBCL consisting of orchiectomy, chemotherapy with CNS prophylaxis, and prophylactic contralateral testicular RT might not always be feasible in clinical practice. However, the histological and genetic features of primary testicular DLBCL were unfavorable because our study showed more than 50% of cases with non-GCB type (Table 1), and frequent mutations of MYD88, PIM1, and CD79B (Figure 5A) consistent with a previous study reporting unfavorable mutation profiles of primary testicular DLBCL.26 Considering these unfavorable characteristics, the active application of treatment might be important for improving the prognosis of primary testicular DLBCL. Indeed, the OS of patients who received six cycles of chemotherapy was better than that of patients receiving only one to four cycles of chemotherapy regardless of stage (Figure 3A). Likewise, the survival outcome of patients who completed the planned treatment protocol consisting of tri-modality treatment was better than that of patients who did not (Figure 3D).
Previous studies also reported improved survival outcome of patients receiving chemotherapy and contralateral testicular RT.3,13,27 In our study, patients who received radiotherapy to the contralateral testis also had longer OS even in patients with advanced stage (Figure 3B). However, disease relapse involving the contralateral testis was not documented in patients who did not receive RT to contralateral testis in our study. This finding might not support the role of additional RT to contralateral testis in patients with primary testicular DLBCL. However, disease relapses in distant sites might be related to microscopic involvement of contralateral testis that was not be detected by radiologically. Thus, the current treatment protocol including contralateral testicular RT should be done in patients with primary testicular DLBCL.
CNS recurrence is another important factor influencing the prognosis of primary testicular DLBCL because CNS recurrence was observed in 6–23% of patients.8,9,13,28 In our study, CNS recurrence occurred in 10 patients including late relapse in CNS (Figure 4) consistent with previous studies reporting that CNS recurrence could occur as late relapse.29,30 However, there was no association between CNS relapse and CNS prophylaxis (Figure 3C). Out of 10 patients who had CNS recurrence, nine patients had brain parenchyma involvement including two cases with simultaneous leptomeningeal involvement in our study. Indeed, it has been reported that CNS recurrence in primary testicular DLBCL mainly occurs in the brain parenchyma rather than the leptomeninges.31 Therefore, currently used combined modality therapy might be insufficient to effectively reduce CNS recurrence due to low intra-CSF level of rituximab32 and the limitations of IT chemotherapy.31,33 In several studies, IV administration of MTX as part of combined modality treatment showed survival benefits and reduced CNS recurrence.17,34 However, given that primary testicular DLBCL most commonly occurs in elderly people, intensified CNS prophylaxis with IV chemotherapy should be selectively performed in patients with high risk and generally good condition. Therefore, it is important to identify patients at risk of CNS relapse requiring active CNS prophylaxis. A recent study reported that lymphoma involvement in the kidney/adrenal gland appears to predict CNS recurrence, and rearrangement of PDL or BCL6 increases the risk of CNS recurrence in testicular DLBCL.35 However, out of ten patients with a high CNS-IPI score due to adrenal gland or kidney involvement, only one patient experienced CNS relapse in our study implying the limited value of CNS-IPI in patients with primary testicular DLBCL. Although our study failed to show the impact of CNS prophylaxis on the occurrence of CNS relapse, our results should be cautiously interpreted because this study retrospectively analyzed the patients with testicular DLBCL who were treated in clinical practice. As not all patients received CNS prophylaxis and there were no established criteria for CNS prophylaxis, our results might be influenced by selection bias.
Although our study has some limitations, such as being a retrospective study based on clinical information for a small number of patients, it does reinforce the benefits of tri-modality treatment (orchiectomy, immunochemotherapy with RCHOP, and RT to contralateral testis). However, CNS recurrence remains an unresolved issue, thus, further research to prevent CNS recurrence is needed. Currently, few biomarkers can predict the prognosis and CNS recurrence of primary testicular DLBCL, and therapies targeted for specific molecular abnormalities. For example, novel agents such as Bruton’s tyrosine kinase (BTK) inhibitors can cross the blood–brain barrier and act on immune-privileged site diseases.36 In addition, BTK inhibition may be an attractive treatment strategy in testicular lymphoma, given its biology of harboring frequent mutations such as CD79B and MYD88.30 Taken together, treatment with orchiectomy, six cycles of immunochemotherapy, and contralateral RT was effective in this study. However, further studies should be warranted to explore more effective CNS-directed prophylaxis and improve outcome of patients with primary testicular DLBCL, especially in case of advanced disease.
Data Sharing Statement
All data are available upon request to the corresponding authors.
Ethics Approval
This study was approved by the Institutional Review Board of Samsung Medical Center (approval number: 2022-01-120).
Acknowledgments
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI22C0999).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors are fully responsible for the contents of this manuscript, and the views and opinions described in the publication are solely those of the authors. The authors report no conflicts of interest in this work.
References
1. King RL, Goodlad JR, Calaminici M, et al. Lymphomas arising in immune-privileged sites: insights into biology, diagnosis, and pathogenesis. Virchows Archiv. 2020;476(5):647–665. doi:10.1007/s00428-019-02698-3
2. Møller MB, d’Amore F, Christensen BE, Group DLS. Testicular lymphoma: a population-based study of incidence, clinicopathological correlations and prognosis. EUR J Cancer. 1994;30(12):1760–1764.
3. Zucca E, Conconi A, Mughal TI, et al. Patterns of outcome and prognostic factors in primary large-cell lymphoma of the testis in a survey by the International Extranodal Lymphoma Study Group. J Clin Oncol. 2003;21(1):20–27. doi:10.1200/JCO.2003.11.141
4. Cheah CY, Wirth A, Seymour JF. Primary testicular lymphoma. Blood. 2014;123(4):486–493. doi:10.1182/blood-2013-10-530659
5. Gundrum JD, Mathiason MA, Moore DB, Go RS. Primary testicular diffuse large B-cell lymphoma: a population-based study on the incidence, natural history, and survival comparison with primary nodal counterpart before and after the introduction of rituximab. J Clin Oncol. 2009;27(31):5227–5232. doi:10.1200/JCO.2009.22.5896
6. Verma N, Lazarchick J, Gudena V, Turner J, Chaudhary UB. Testicular lymphoma: an update for clinicians. Am J Med Sci. 2008;336(4):336–341. doi:10.1097/MAJ.0b013e31817242bc
7. Visco C, Medeiros LJ, Mesina OM, et al. Non-Hodgkin’s lymphoma affecting the testis: is it curable with doxorubicin-based therapy? Clin Lymphoma. 2001;2(1):40–46. doi:10.3816/CLM.2001.n.010
8. Kridel R, Telio D, Villa D, et al. Diffuse large B-cell lymphoma with testicular involvement: outcome and risk of CNS relapse in the rituximab era. Br J Haematol. 2017;176(2):210–221. doi:10.1111/bjh.14392
9. Vitolo U, Chiappella A, Ferreri AJ, et al. First-line treatment for primary testicular diffuse large B-cell lymphoma with rituximab-CHOP, CNS prophylaxis, and contralateral testis irradiation: final results of an international Phase II trial. J Clin Oncol. 2011;29(20):2766–2772. doi:10.1200/JCO.2010.31.4187
10. Linassier C, Desablens B, Lefrancq T, et al. Stage I-IIE primary non-Hodgkin’s lymphoma of the testis: results of a prospective trial by the GOELAMS Study Group. Clin Lymphoma. 2002;3(3):167–172. doi:10.3816/CLM.2002.n.023
11. Seymour JF, Solomon B, Wolf MM, Janusczewicz EH, Wirth A, Prince HM. Primary large-cell non-Hodgkin’s lymphoma of the testis: a retrospective analysis of patterns of failure and prognostic factors. Clin Lymphoma. 2001;2(2):109–115. doi:10.3816/CLM.2001.n.016
12. Lantz AG, Power N, Hutton B, Gupta R. Malignant lymphoma of the testis: a study of 12 cases. Can Urol Assoc J. 2009;3(5):393–398. doi:10.5489/cuaj.1153
13. Mazloom A, Fowler N, Medeiros LJ, Iyengar P, Horace P, Dabaja BS. Outcome of patients with diffuse large B-cell lymphoma of the testis by era of treatment: the M. D. Anderson Cancer Center experience. Leuk Lymphoma. 2010;51(7):1217–1224. doi:10.3109/10428191003793358
14. Telio D, Villa D, Shenkier T, et al. Diffuse large B-cell lymphoma with testicular involvement: outcome and risk of CNS relapse in the rituximab era. Blood. 2011;118(21):780. doi:10.1182/blood.V118.21.780.780
15. Mazloom A, Fowler N, Iyengar P, Dabaja BS. Primary testicular diffuse large B-cell lymphoma, M.D. Anderson Cancer Center experience. Blood. 2009;114(22):2697. doi:10.1182/blood.V114.22.2697.2697
16. Deng L, Xu-Monette Z, Loghavi S, et al. Primary testicular diffuse large B-cell lymphoma displays distinct clinical and biological features for treatment failure in rituximab era: a report from the International PTL Consortium. Leukemia. 2016;30(2):361–372. doi:10.1038/leu.2015.237
17. Conconi A, Chiappella A, Orsucci L, et al. Intensified (Intravenous and Intrathecal) CNS prophylaxis in primary testicular diffuse large B-cell lymphoma: 5-year results of the IELSG30 trial. Hematol Oncol. 2021;39(S2). doi:10.1002/hon.48_2879
18. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–2390. doi:10.1182/blood-2016-01-643569
19. Hans CP, Weisenburger DD, Greiner TC, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103(1):275–282. doi:10.1182/blood-2003-05-1545
20. Riedell PA, Smith SM. Double hit and double expressors in lymphoma: definition and treatment. Cancer. 2018;124(24):4622–4632. doi:10.1002/cncr.31646
21. Hyeon J, Lee B, Shin SH, et al. Targeted deep sequencing of gastric marginal zone lymphoma identified alterations of TRAF3 and TNFAIP3 that were mutually exclusive for MALT1 rearrangement. Modern Pathol. 2018;31(9):1418–1428. doi:10.1038/s41379-018-0064-0
22. Shin HT, Choi YL, Yun JW, et al. Prevalence and detection of low-allele-fraction variants in clinical cancer samples. Nat Commun. 2017;8(1):1377. doi:10.1038/s41467-017-01470-y
23. Wilm A, Aw PP, Bertrand D, et al. LoFreq: a sequence-quality aware, ultra-sensitive variant caller for uncovering cell-population heterogeneity from high-throughput sequencing datasets. Nucleic Acids Res. 2012;40(22):11189–11201. doi:10.1093/nar/gks918
24. Cibulskis K, Lawrence MS, Carter SL, et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat Biotechnol. 2013;31(3):213–219. doi:10.1038/nbt.2514
25. Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059–3068. doi:10.1200/JCO.2013.54.8800
26. Chapuy B, Roemer MG, Stewart C, et al. Targetable genetic features of primary testicular and primary central nervous system lymphomas. Blood. 2016;127(7):869–881. doi:10.1182/blood-2015-10-673236
27. Ho JC, Dabaja BS, Milgrom SA, et al. Radiation therapy improves survival in patients with testicular diffuse large B-cell lymphoma. Leuk Lymphoma. 2017;58(12):2833–2844. doi:10.1080/10428194.2017.1312381
28. Park BB, Kim JG, Sohn SK, et al. Consideration of aggressive therapeutic strategies for primary testicular lymphoma. Am J Hematol. 2007;82(9):840–845. doi:10.1002/ajh.20973
29. Fonseca R, Habermann TM, Colgan JP, et al. Testicular lymphoma is associated with a high incidence of extranodal recurrence. Cancer. 2000;88(1):154–161. doi:10.1002/(SICI)1097-0142(20000101)88:1<154::AID-CNCR21>3.0.CO;2-T
30. Yan Z, Yao S, Wang Y, Liu Y, Yao Z. Primary testicular lymphoma with central nervous system relapse was successfully treated by a chemo-free regimen: a case report and literature review. Cancer Manag Res. 2021;13:9489–9500. doi:10.2147/CMAR.S341342
31. Balis FM, Blaney SM, McCully CL, Bacher JD, Murphy RF, Poplack DG. Methotrexate distribution within the subarachnoid space after intraventricular and intravenous administration. Cancer Chemother Pharmacol. 2000;45(3):259–264. doi:10.1007/s002800050038
32. Rubenstein JL, Fridlyand J, Abrey L, et al. Phase I study of intraventricular administration of rituximab in patients with recurrent CNS and intraocular lymphoma. J Clin Oncol. 2007;25(11):1350–1356. doi:10.1200/JCO.2006.09.7311
33. Batchelor T, Leahy N, Kaufman D. High-dose methotrexate for isolated central nervous system relapse in patients with testicular non-Hodgkin’s lymphoma. Clin Lymphoma. 2001;2(2):
34. Avilés A, Nambo MJ, Cleto S, Neri N, Huerta-Guzmán J. Rituximab and dose-dense chemotherapy in primary testicular lymphoma. Clin Lymphoma Myeloma. 2009;9(5):386–389. doi:10.3816/CLM.2009.n.075
35. Twa DDW, Lee DG, Tan KL, et al. Genomic predictors of central nervous system relapse in primary testicular diffuse large B-cell lymphoma. Blood. 2021;137(9):1256–1259. doi:10.1182/blood.2020006338
36. Wilson WH, Young RM, Schmitz R, et al. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Nat Med. 2015;21(8):922–926. doi:10.1038/nm.3884
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.