Back to Journals » International Journal of Women's Health » Volume 16
Same-Day Discharge is Safe, Feasible Following Vaginal Hysterectomy with Apical Suspension
Authors Ray MM , Yeung J, Hoehn J, Valenti M, Lewis KE, Pauls RN, Crisp CC
Received 23 November 2023
Accepted for publication 20 March 2024
Published 17 April 2024 Volume 2024:16 Pages 655—661
DOI https://doi.org/10.2147/IJWH.S451435
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Marlana M Ray,1 Jennifer Yeung,1 Jonathan Hoehn,2 Matthew Valenti,3 Kelsey E Lewis,1 Rachel N Pauls,1 Catrina C Crisp1
1Urogynecology Division, TriHealth, Cincinnati, OH, USA; 2Hatton Research Institute, TriHealth, Cincinnati, OH, USA; 3OB/GYN Department, University of Cincinnati, Cincinnati, OH, USA
Correspondence: Marlana M Ray, TriHealth, Urogynecology Division, 3219 Clifton Ave, Medical Office Building Suite 100, Cincinnati, OH, 45220, USA, Email [email protected]
Purpose: Studies involving minimally invasive hysterectomy and robotic sacrocolpopexy have demonstrated safety and feasibility of same-day discharge. There are limited data, however, on same-day discharge outcomes for vaginal hysterectomy and pelvic reconstruction. This study aimed to compare 30 and 90-day surgical outcomes between same-day discharge versus overnight stay following vaginal hysterectomy and apical suspension.
Patients and Methods: This retrospective study evaluated surgeries performed over two time periods. Overnight stay was standard between December 2018 and February 2020. Same-day discharge was standard from December 2020 to February 2022. All patients who underwent vaginal hysterectomy with apical suspension were included. The primary outcome was to determine if there was an increase in 30-day readmission rates. Secondary outcomes included emergency department visits and reoperations within 30 days, the previous variables at 90 days, and the rate for successful same-day discharge.
Results: A total of 324 patients were analyzed over the 30 months: 149 (46%) in the overnight stay group and 175 (54%) in the same-day discharge group. At 30 days, no difference was found between groups for readmissions (2.7% vs 4.0%, p = 0.56), emergency department visits (14.8% vs 14.9%, p = 1.0), or reoperations (2.0% vs.1.7%, p = 1.0). At 90 days, outcomes were also similar. Same-day discharge as standard practice was successful in 80% of patients.
Conclusion: In this retrospective two cohort study, the safety of same-day discharge following vaginal hysterectomy with apical suspension was demonstrated with no increased risk of 30 or 90-day readmissions, emergency visits, or reoperation rates. The majority (80%) of patients were discharged on the day of surgery, suggesting feasibility of this model.
Keywords: female pelvic reconstructive surgery, urogynecology, vaginal prolapse repair, pelvic floor surgery
Introduction
Approximately 600,000 hysterectomies are performed annually, making this procedure one of the most common major gynecologic procedures.1 Of the various approaches, vaginal hysterectomy has been shown to have fewer complications, shorter hospital stays, and faster recovery.2,3 Recently, same-day discharge (SDD) following minimally invasive vaginal hysterectomy has gained acceptance.4 When compared to inpatient vaginal hysterectomy, SDD has shown to be safe and feasible with similar or lower rates of postoperative complications.5–7 Studies have also demonstrated success of SDD upwards of 96% with low rates of readmission and estimated blood loss (EBL).6,7
There is now a growing body of evidence evaluating SDD after major urogynecologic procedures.8–13 Results are conflicting regarding rates of readmission after SDD compared to overnight stay (OS), with one study reporting higher rates of readmission and others reporting no difference.8,9 The majority of studies, however, have reviewed laparoscopic or robotic procedures.10–12 Outcomes following vaginal hysterectomy and pelvic reconstruction with apical suspension are limited in number and sample size.14,15 The objective of this study was to determine if SDD is safe and feasible for patients undergoing vaginal hysterectomy with pelvic reconstruction, including apical suspension. We also chose to extend the evaluation period by including outcomes up to 90 days postoperatively.
Materials and Methods
In this TriHealth Institutional Review Board-approved retrospective, two cohort study, we evaluated outcomes following vaginal hysterectomy and pelvic reconstruction with apical suspension. Surgeries were performed over two time periods by three fellowship-trained, board-certified Urogynecologic surgeons at two Institution-affiliated hospitals. Time periods were chosen based on a shift in standard discharge practice due to the COVID-19 pandemic. Planned OS was standard prior to March 2020, at which time all elective procedures were halted. In order to resume elective surgeries, hospital policy required SDD to ensure hospital beds remained available to those requiring COVID-19 treatment. This requirement shifted standard discharge practice to SDD. Similar 15-month intervals during each period were selected for comparison. The study population included female patients, 18 years or older, who underwent vaginal hysterectomy and vaginal apical reconstruction for pelvic organ prolapse. Apical reconstruction was performed via high uterosacral ligament suspension utilizing two 0-polydioxanone suture (0-PDS, Ethicon, Johnson & Johnson) on each side. Concomitant vaginal reconstructive procedures were performed based on compartmental prolapse, including anterior and posterior colporrhaphy via midline plication, enterocele repair via internal McCall culdoplasty, or midurethral sling procedures for stress urinary incontinence. All patients underwent cystoscopy to evaluate for bladder injury and ureteral patency. As this was a retrospective chart review involving no more than minimal risk, the TriHealth Institutional Review Board did not require patient consent to review medical records. This study was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All data was anonymized and maintained using a password-protected computer.
We compared OS as standard practice between December 2018 and February 2020 with SDD as standard practice between December 2020 and February 2022. If an overnight stay was necessary during the SDD period, patients remained included in the SDD group as that was standard practice. Successful SDD was defined as discharge home on postoperative day (POD) 0. Standard office follow-up visits also shifted due to the COVID-19 pandemic. In the OS group, office visits occurred at both 2 and 6 weeks postoperatively. In the SDD group, patients had one visit between 3 and 5 weeks. All patients were seen in the office at 12 weeks.
All demographic, operative, and postoperative data were collected from the electronic medical record from the baseline preoperative appointment until 90 days postoperatively. The primary outcome was unanticipated readmissions within 30 days of surgery. Secondary outcomes analyzed Emergency Department (ED) visits and reoperations within 30 days and the same three variables within 90 days postoperatively. Other outcomes of interest included the rate of successful SDD and comparison of postoperative urinary retention (POUR) and EBL. In the OS group, patients had a voiding trial on the morning of POD1. The SDD group underwent a voiding trial prior to discharge. POUR was defined as a post-void residual of >150mL. Patients with POUR were discharged home with an indwelling Foley catheter for 3–7 days. Estimated blood loss was categorized as normal or high. The definition of “high” EBL (>200mL) was selected based on our group’s average blood loss of less than 100mL for vaginal hysterectomy with pelvic reconstruction. For all readmissions, ED visits, and reoperations, the principal diagnosis was obtained. We also evaluated for differences in postoperative patient communication, via phone calls and electronic messages, and office visits at both 30 and 90-days. All phone calls were documented in the medical record, including calls initiated by the patient or by office staff.
We hypothesized that there would be no difference in postoperative readmissions, ED visits, or reoperations between the SDD and the OS group. Statistical analysis was performed with Mann–Whitney U-test for continuous variables and Fisher’s Exact test for categorical variables. A multivariable regression model was built using age, BMI, race, ethnicity, stage of prolapse, unsuccessful voiding trial, EBL, surgical end time, and surgical duration to determine any relationship with ED visits within 30 days. A similar model with the same variables was used to determine any relationship with unsuccessful SDD during that time period.
Results
We identified a total of 324 patients who underwent vaginal hysterectomy and pelvic reconstruction with apical suspension. Of those, 149 (46%) were in the OS as standard practice group and 175 (54%) were in the SDD as standard practice group. Table 1 demonstrates the demographics. The OS group was younger with a median age of 62 years compared to 65 years in the SDD group (p = 0.02). There was no difference in median BMI (27.62 vs 27.44, p = 0.15). There was no difference in race or ethnicity, while the majority of all patients were White (87.2% vs 94.3%, p = 0.27). All patients underwent total vaginal hysterectomy with vaginal vault suspension via uterosacral ligament suspension (Table 2). All but one patient in each group received an anterior repair as well as a posterior repair. There was no difference in rates of mid-urethral slings between groups (32.9% vs 42.3%, p = 0.09).
 |
Table 1 Demographics of Subjects by Time Period |
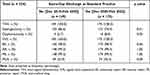 |
Table 2 Procedures of Subjects by Time Period |
Table 3 demonstrates no difference in 30-day readmission between the OS and SDD groups (2.7% vs 4.0%, respectively; p = 0.56). Of the 11 total patients readmitted, 4 were in the OS group and 7 in the SDD group. The OS group included one readmission for each of the following, constipation, small bowel obstruction, nausea and vomiting, and weakness. The SDD group included two patients with sepsis and one readmission for each of the following, constipation, pelvic hematoma, pelvic abscess, myocardial infarction, and electrolyte abnormalities.
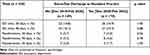 |
Table 3 Outcomes by Time Period |
Within 30 days after surgery, there were no differences in ED visits (Table 3). In the OS group, 22 visits (14.8%) occurred compared to 26 visits (14.9%) in the SDD group (p = 1.0). ED visits were most commonly due to urinary retention, accounting for 38% of visits. Similarly, there was no difference in patients requiring reoperation, with 3 in each cohort (2.0% vs 1.7%, p = 1.0; Table 3). In the OS group, one patient had unilateral vaginal vault sutures removed due to nerve entrapment. One patient in this group was taken for reoperation due to increased bleeding after removal of vaginal packing on the evening of surgery. One patient in this group suffered a small bowel obstruction and underwent resection and reanastomosis. In the SDD group, two patients had removal of unilateral vaginal vault sutures due to nerve entrapment. One patient in this group was not successfully discharged on POD0 due to prolonged recovery and was taken for reoperation the next morning after increased bleeding with removal of vaginal packing.
The same outcomes were also evaluated at 90-days postoperatively (Table 3). Readmissions were not different between groups (OS 3.4% vs SDD 4.6%, p = 0.78). Between 31 and 90 days postoperative, atrial fibrillation prompted one additional readmission in the OS group. In the SDD group, opioid withdrawal prompted one additional readmission. Similarly, emergency room visits were not different (OS 16.1% vs SDD 15.4%, p = 0.88). There were no additional reoperations after the first 30 days.
Rates of POUR and intraoperative high-volume blood loss were not different between groups (Table 1). In the OS group, 73.2% of patients were discharged home with a catheter as compared to 75.4% of patients in the SDD group (p = 0.70). There were 16 patients (10.7%) in the OS group with an EBL > 200mL compared to 9 patients (5.1%) in the SDD group (p = 0.09). Notably, only 5 total patients had an EBL > 500mL.
Among the 149 patients in the period where OS was standard, 145 (97.3%) patients were discharged on POD1, and 4 (2.7%) were discharged on POD2. When SDD was standard, 80% (140/175) of patients were successfully discharged on POD0. Of those who were not discharged on POD0, all were subsequently discharged on POD1. Multivariable regression was performed on the 175 patients in the SDD as standard practice group. The independent variable was successful SDD. Age, BMI, race, ethnicity, EBL, surgical end time, and surgical duration were not significantly associated with the need for overnight stay.
Postoperative office visits, patient phone calls, and electronic messaging were also analyzed (Table 4). As per the pre-COVID-19 standard, there were twice as many office visits for the OS group, with two median visits within 30 days and four within 90 days. During the pandemic, there was one median visit within 30 days and two within 90 days in the SDD group. There were more patient phone calls in the OS group interquartile range (IQR) at 30 days (OS 3 [IQR 2–5] vs SDD 3 [IQR 2–4], p = 0.03) and no difference at 90 days (OS 4 [IQR 2–6] vs SDD 3 [IQR 2–6], p = 0.09). Alternatively, more electronic messaging occurred for the SDD group within 30 days (OS 0 [IQR 0–0] vs SDD 0 [IQR 0–1], p < 0.01) and 90 days (OS 0 [IQR 0–0] vs 0 [IQR 0–3], p < 0.01). When phone calls and electronic messaging were combined and evaluated as “total patient communication”, no difference was observed between the two groups within 30 days (OS 3 [IQR 2–6] vs SDD 3 [IQR 2–6], p = 0.95) or 90 days (OS 4 [IQR 3–7] vs SDD 5 [IQR 3–8], p = 0.12).
 |
Table 4 Office Visits, Office Calls, Electronic Messages, Communications |
Discussion
This study was designed to evaluate the safety and feasibility of SDD after vaginal hysterectomy and pelvic reconstructive surgery with apical suspension. When comparing two 15-month time periods of differing discharge practices, we found similar rates of readmissions, ED visits, and reoperations within 30 and 90 days after surgery. Additionally, 80% of patients were successfully discharged on the day of surgery.
These findings expand on existing Urogynecology SDD literature. Prior studies, however, included a multitude of surgical approaches for prolapse repair, including obliterative procedures and laparoscopic, robotic, and vaginal apical suspension.8–14 These studies also included laparoscopic or robotic hysterectomy as well as procedures without hysterectomy, which may be considered the highest risk procedure. This broad inclusion of procedures results in a heterogenous study population, making it difficult to draw specific conclusions regarding SDD for patients undergoing vaginal hysterectomy and pelvic reconstruction with apical suspension via high uterosacral ligament fixation. While one study by Liu et al did evaluate vaginal hysterectomy with apical suspension, the specific approach for apical suspension is unclear, and the findings are limited due to a small population size of 55 patients.15 Our study expands on this pilot study by including a larger population of 324 patients over a total of 30 months.
Few studies have evaluated the success rate of SDD after urogynecologic surgery. Data is limited to one study following minimally invasive sacrocolpopexy and one study by Carter-Brooks et al, which noted a 91.7% success rate among those who underwent various prolapse repair approaches, while nearly half of patients did not have concurrent hysterectomy.9,12 These studies prove difficult to extrapolate success of SDD in our specific surgical population. Though Liu et al’s pilot study on vaginal hysterectomy and pelvic reconstruction noted successful SDD of 63.9%, the patients were able to self-select their discharge cohort, introducing selection bias.15 Our study demonstrated a rate of 80% successful SDD in a cohort of 175 patients, suggesting feasibility of SDD after vaginal hysterectomy and pelvic reconstruction with apical suspension.
Few studies have evaluated for differences in EBL or POUR between groups. Carter-Brooks et al reported no difference in total EBL, yet an increased rate of POUR in patients discharged same day.9 Again, this study population included a variety of prolapse procedures and hysterectomy was not performed in nearly half of patients, making these results difficult to generalize to our population. In our study, we focused on rates of “high” EBL (>200mL) and found no difference between OS and SDD. There were also no differences in rates of POUR between the groups. While our overall POUR rate is notably high, we attribute this to our strict post-void residual criteria. A residual volume of 150mL or greater was considered retention and patients were sent home with a catheter.
Our study also adds to the literature by extending the evaluation of outcomes to 90 days postoperatively. Apart from two studies on SDD after minimally invasive sacrocolpopexy, which evaluated outcomes up to 6 weeks postoperatively, all other studies on SDD after urogynecologic procedures only evaluated outcomes within 30 days of surgery.8–15
Due to the COVID-19 pandemic, our office practices regarding postoperative visits also changed. During the OS period, which occurred prior to the pandemic, standard visits were at 2 and 6 weeks. During the SDD period, the standard decreased to one visit between 3 and 5 weeks. Therefore, we expected a decrease in visits after this practice change and can be reassured that SDD is not associated with an increase in office visits. There were more phone calls during the OS period, yet more electronic messaging during the SDD period. When these were combined into “general patient communication”, however, no differences were noted. This suggests that overall postoperative patient communication was not increased with SDD, and merely the form of communication shifted from phone calls to electronic messaging.
Strengths of our study included a detailed comparison of two 15-month time periods where the standard for discharge timing shifted from OS to SDD. While this shift in discharge practice was due to a new hospital policy secondary to the COVID-19 pandemic, vaginal surgery remained vital for patient care and had reduced risk of transmission compared to other approaches for hysterectomy.16 In order to reduce confounders from the various surgical approaches to prolapse repair, we limited our study to only include vaginal hysterectomy and vaginal reconstruction with apical suspension. We also collected data on postoperative outcomes including the principal diagnosis for readmissions, ED visits, and reoperations up to 90 days postoperatively. Therefore, our study provides strong reassurance and a unique insight into the safety and feasibility of same-day discharge as standard of practice in this surgical population.
Our study is limited by its retrospective, observational design. The decision to shift the standard practice of discharge timing across the two time periods occurred as a result of the COVID-19 pandemic. Therefore, there may be social and societal factors that influence the success rates of SDD as well as postoperative visits, phone calls, and electronic messaging as the COVID-19 pandemic was still ongoing at the conclusion of the SDD period. To attempt to control for this, we used all patients across two matched 15-month time periods, and the overall similar demographics between the two groups demonstrate an appropriate comparison.
Additionally, our study is limited in comparing the details of postoperative office visits, phone calls, and electronic messages. We did not identify the primary diagnosis or reason for each interaction, therefore some of the data may not accurately reflect total time spent with the patient. While we recognize the importance of content in patient communication in the postoperative period, a full analysis of these qualitative data was beyond the scope of this manuscript. We look forward to future publications regarding this data.
Conclusion
Same-day discharge as the standard practice after vaginal hysterectomy with pelvic reconstruction, including apical suspension, is both safe and feasible. We found that patients and surgeons are willing to adopt this model as 80% were successfully discharged the same day.
Funding
Funding for publication was provided by the TriHealth Medical Education Research Fund.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110(5):1091–1095. doi:10.1097/01.AOG.0000285997.38553.4b
2. Aarts JW, Nieboer TE, Johnson N, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2015;8:CD003677.
3. Kaya C, Yıldız Ş, Alay İ, et al. Comparison of Surgical Outcomes of Total Laparoscopic Hysterectomy and vNOTES Hysterectomy for Undescended-Enlarged Uteri. J Invest Surg. 2022;35(4):918–923. doi:10.1080/08941939.2021.1958111
4. Moawad G, Liu E, Song C, Fu AZ. Movement to outpatient hysterectomy for benign indications in the United States, 2008–2014. PLoS One. 2017;12(11):1–15. doi:10.1371/journal.pone.0188812
5. Levy BS, Luciano DE, Emery LL. Outpatient vaginal hysterectomy is safe for patients and reduces institutional cost. J Minimally Invasive Gynecol. 2005;12(6):494–501. doi:10.1016/j.jmig.2005.06.015
6. Zakaria MA, Levy BS, Zakaria MA, Levy BS. Outpatient vaginal hysterectomy: optimizing perioperative management for same-day discharge. Obstetrics Gynecol. 2012;120(6):1355–1361. doi:10.1097/AOG.0b013e3182732ece
7. Ellinides A, Manolopoulos PP, Hajymiri M, Sergentanis TN, Trompoukis P, Ntourakis D. Outpatient Hysterectomy versus Inpatient Hysterectomy: a Systematic Review and Meta-analysis. J Minimally Invasive Gynecol. 2022;29(1):23–40. doi:10.1016/j.jmig.2021.06.012
8. Romanova AL, Carter-Brooks C, Ruppert KM, Zyczynski HM. 30-Day unanticipated healthcare encounters after prolapse surgery: impact of same day discharge. Am J Clin Exp Obstet Gynecol. 2020;222(5):482. doi:10.1016/j.ajog.2019.11.1249
9. Carter-Brooks CM, Du AL, Ruppert KM, Romanova AL, Zyczynski HM. Implementation of a urogynecology-specific enhanced recovery after surgery (ERAS) pathway. Am J Clin Exp Obstet Gynecol. 2018;219(5):495. doi:10.1016/j.ajog.2018.06.009
10. Kisby CK, Polin MR, Visco AG, Siddiqui NY. Same-Day Discharge After Robotic-Assisted Sacrocolpopexy. Female Pelvic Med Reconstructive Surgery. 2019;25(5):337–341. doi:10.1097/SPV.0000000000000573
11. Guérin S, Nyangoh Timoh K, Khene Z-E, et al. Outpatient laparoscopic sacrocolpopexy: feasibility and patient satisfaction. J Gynecol Obstetrics Human Reproduction. 2021;50(7):102118. doi:10.1016/j.jogoh.2021.102118
12. Hickman LC, Paraiso MFR, Goldman HB, Propst K, Ferrando CA. Same-Day Discharge After Minimally Invasive Sacrocolpopexy Is Feasible, Safe, and Associated With High Patient Satisfaction. Female Pelvic Med Reconstructive Surgery. 2021;27(8):e614–e619. doi:10.1097/SPV.0000000000000998
13. Robison EH, Smith PE, Pandya LK, Nekkanti S, Hundley AF, Hudson CO. Readmissions and perioperative outcomes for same-day versus next-day discharge after prolapse surgery. Int Urogynecology J. 2021;1–9.
14. Berger AA, Tan-Kim J, Menefee SA, Tan-Kim J. Comparison of 30-Day Readmission After Same-Day Compared With Next-Day Discharge in Minimally Invasive Pelvic Organ Prolapse Surgery. Obstetrics Gynecol. 2020;135(6):1327–1337. doi:10.1097/AOG.0000000000003871
15. Liu L, Yi J, Cornella J, Butterfield R, Buras M, Wasson M. Same-Day Discharge after Vaginal Hysterectomy with Pelvic Floor Reconstruction: pilot Study. J Minimally Invasive Gynecol. 2020;27(2):498–503. doi:10.1016/j.jmig.2019.04.010
16. Kaya C. The Importance of Vaginal Natural Orifice Surgeries in the Era of COVID-19 Pandemic. J Minim Invasive Gynecol. 2020;27(6):1429. doi:10.1016/j.jmig.2020.06.003
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
