Back to Journals » International Medical Case Reports Journal » Volume 17
Solitary Glomus Tumor on the Base of the Right Thumb: A Rare Case Report and a Literature Review from Saudi Arabia
Authors Arkoubi AY
Received 14 January 2024
Accepted for publication 9 April 2024
Published 23 April 2024 Volume 2024:17 Pages 371—380
DOI https://doi.org/10.2147/IMCRJ.S456808
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Vinay Kumar
Amr Youssef Arkoubi
Department of Anesthesia and Surgery, College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh, Saudi Arabia
Correspondence: Amr Youssef Arkoubi, Department of Anesthesia and Surgery, College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh, Saudi Arabia, Email [email protected]
Abstract: A glomus tumor (GT) is a rare and usually benign tumor that originates from the glomus body, which is involved in thermoregulation in the skin. Solitary or multiple, digital or extra-digital, these cutaneous tumors can be benign or malignant. This report describes the diagnosis and surgical management of a solitary glomus tumor at the base of the right thumb in a young Sudanese woman. The diagnosis of glomus tumor was confirmed by medical history, sonographic findings and histopathological report. The lesion was excised via direct complete excision under local anesthesia, resulting in a complete resolution of symptoms. Owing to its high sensitivity level, the use of ultrasound is appropriate to evaluate a lesion suspected to be a glomus tumor. A clinician needs to take into consideration the likelihood of glomus tumors when assessing a patient who has a skin lesion on fingers, toes, or extra-digital area, with pain triggered by temperature changes, pressure, or touch. Additionally, this report includes a review of recent globally reported cases of glomus tumor in the hand to highlight the distinctiveness of this report in context to its atypical location in the area of the thenar eminence and underscoring it as a unique report of its kind from Saudi Arabia.
Keywords: glomus, digital, extra digital, hand, thumb, solitary, benign
Introduction
Glomus tumor usually appears as a painful dermal lesion consisting of glomus cells.1 The most common occurrence is underneath the nail plate which is termed a subungual glomus tumor (SGT).2 A glomus tumor may, however, also develop at other sites; in these cases, it is called a glomus extra-digital tumor (GET). Most often, extra-digital glomus tumors present as painful nodules on the arms, legs, trunk, head or any internal organs.3
The absence of the typical GT-related cold sensitivity along with atypical location of the lesion can often delay its diagnosis.4,5 Though most glomus tumors are benign, malignant ones can typically measure over 2 centimeters and affect the visceral organs.6,7 Female patients are more likely to have glomus tumors,8 while there is no established gender predisposition for these tumors.9,10 Considering the limited effectiveness of anti-inflammatory drugs,11 a full excision of the lesion is the only option to relieve pain. As a bloody field may prevent complete excision and lead to recurrence,12 tumor removal is performed in a bloodless field under loupe magnification, with tourniquet application.13,14
Other painful tumors such as neuroma, leiomyoma, hemangioma, and conditions such as gouty arthritis should be considered as a part of a differential diagnosis while assessing solitary glomus tumors.15 A neuroma may produce similar pain symptoms and have a trigger zone, but it will not exhibit hypersensitivity to cold.16 On the other hand, melanoma would not cause pain and would be visible beneath the skin.17 It is crucial to carefully distinguish multiple glomus tumors, which may be painless, from cavernous hemangioma18 and blue rubber nevus syndrome.19 Both ultrasound and magnetic resonance imaging (MRI) have a comparably high sensitivity and are preferred in confirming the tumor diagnosis of a skin lesion. With established high sensitivity level, ultrasound modality can be an economic and time-saving alternative for the patients. Although the diagnosis of a glomus tumor can be suspected based on clinical features and radiographic examination, a microscopic evaluation of the lesion is required to establish the diagnosis.20 Due to the uncertain nature of the clinical presentations and unusual anatomical locations, it is very important to report any atypical cases of GT to support earlier diagnosis and thus effective relief of symptoms. The current case report is elaborated and reported in this study with this purpose.
Case Presentation
A 36-year-old woman presented herself for evaluation of a tender area beneath the skin on the base of her right thumb that had been symptomatic for about 6 months. The patient did not recall any history of trauma to the site of lesion. Upon cold exposure, the lesion was very painful with worsening pain and tenderness.
Investigations
On physical examination, the right thumb of the patient showed a 3 millimeter raised erythematous patch surrounded by a flat-topped papule with diameter of 2 millimeters that had a slight central depression (Figure 1a). Standard clinical tests were applied which consisted of the Love’s test, Hildreth test and a cold sensitivity test.12 Love’s test showed an amplified pain with an application of pressure on the location. Hildreth test was deemed positive as there was reduction in tenderness in the area of the lesion when the area was exsanguinated. Cold sensitivity test was positive as the area elicited pain on exposure to cold water. Ultrasound imaging revealed a small nodule beneath the skin which was well defined and hypoechoic along with a prominent vascularity. This was an important finding which was consistent with the glomus tumor diagnosis in this case (Figure 1b).
The tissue specimen from the lesion site on microscopic examination showed large nodular clusters of benign cells in the dermis along with compact hyperkeratosis and mild acanthosis that correlated with the typical thickness of the skin at this location (Figure 1d), The basophilic tumor appeared as solid sheets of uniform-appearing glomus cells with sparse smooth muscle and thus identifying it as glomus tumor, classified as the solid type.
Differential Diagnosis
A mucous cyst or a foreign body presence, along with other possible hand tumors were included among the preliminary considerations in the clinical differential diagnosis. Correlated with the patient’s symptoms, ultrasound findings and the lesion morphology, a diagnosis of a glomus tumor was established.
Treatment and Follow Up
A direct complete excisional biopsy under local anesthesia was performed using a 4-millimeter elliptical excisional biopsy tool and the wound was closed with 4–0 absorbable braided sutures (Figure 1c). The histopathological images (Figure 1d) showed round to ovoid glomus cells scattered with fibroblast, myxoid stroma with fine vasculature, with no evidence of necrosis, mycosis, and atypia.
Sutures were removed after 2 weeks of the biopsy and the biopsy site had completely healed on examination. No pain was reported at the site of lesion at the 2 weeks follow-up visit. On telephonic follow up during the subsequent 12 months, there was no report of any recurrence of symptoms.
Discussion
An updated prevalence and incidence context is provided here by a comprehensive literature review from a PubMed search of case reports/series from 2019–2023 on glomus tumor on hand among adult patients. Studies report that the incidence of subungual glomus tumor is about 1–6% of all soft tissue tumors in the upper limb, with hand accounting for about 50–75%.21 To provide the context of the current case report, this review focused on glomus tumor of the hand, though it can occur on various locations in the human body.22
An electronic literature search was undertaken with key words such as “glomangioma”, “glomus tumor”, “Saudi Arabia”, “glomangiomyoma”, and “case”. A total of 101 patients were identified from 2019 to January 2024. Tumor topography across the literature included is described in Table 1 and the patient/sample demographics and characteristics are described in Table 2.
 |
Table 1 Tumor Topography from the Reviewed Literature |
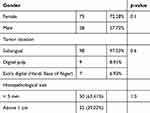 |
Table 2 Patient Demography and Tumor Variables from the Reviewed Literature |
A total of 101 patients with glomus tumor in the hand were assessed in the literature review included in this case report. As observed from the literature reviewed, GT on the subungual region was the most widely reported with 98 (97.03%), while the digital pulp GTs were 9 (8.91%) and GTs on other parts of the hand were only 7 (6.93%). On assessing the presentation of the size of the GTs reported, tumors smaller than 5 mm were reported among 16 (32.0%) patients and tumors ranging between 5 mm to 1 cm in 29 (58.0%), while 5 (10.0%) had tumor size reports between 1–2 cm. Within the sample from the included literature, there were 4 reports (3.96%) of recurrence of the tumor.
Female gender was the most predominant of all the cases as seen from Table 2. No statistical correlation with the recurrences of the tumor could be derived from the variables such as gender and age reported across the literature, which is observable from Table 2. As ethnicity cannot be considered as a variable for correlation just based on the region of reporting and publishing, it was not practical to report a reliable conclusion on the ethnic presentation of this case. However it can be mentioned 85.14% (86) of all the cases were reported from India, Pakistan and Bangladesh. It is recommended to undertake future cross-sectional studies examining the association between ethnicity and the incidence of GT to provide clinically relevant insights about this condition. Table 2 is descriptive of the statistical correlation analysis of these observations. The information from the case reports (Table 3) and case series (Table 4) reviewed are described in Table 1 which illustrates the rarity of the anatomical location of the present case.
 |
Table 3 Literature Review Summary from Case Reports of Glomus Tumors on Hand |
 |
Table 4 Literature Review Summary from Case Series and Retrospective Studies of Glomus Tumors on Hand |
Though the first clinical description of a glomus tumor was reported in 1812 by Wood, as a painful subcutaneous tubercle,40 the histopathological features of the glomus tumor and its emergence from the glomus body were not described until 1924 by Barre and Masson.41 There is no clear understanding of the factors influencing the pathogenesis of glomus tumors and their etiology, including age at onset, gender, family predisposition, and history of trauma to the site.42 Most cases of delayed diagnosis of GT, which could be between 3–15 years,43–45 were due to a lack of awareness about the disease among the general practitioners who usually receive the patients initially, its anatomical presentation and visibility. Most cases go undiagnosed or misdiagnosed for a long period, even with the typical clinical symptoms of pain, pinpoint tenderness, and cold sensitiveness.46,47
It was deemed necessary to report this case, particularly in light of its rarely reported anatomical location (the base of the thumb) and geographical location (Saudi Arabia). An emphasis on the importance in the early diagnosis and management of such cases and the necessity of vigilance in monitoring painful skin lesions is underscored here. There is a need for further investigation of the pathogenesis of this tumor formation and reoccurrence in light of this case report. Ultimately, this case report provides valuable information to the medical community, highlighting the need for continuous research on differential diagnosis and the right diagnostic protocols to follow. A review of previous publications indicates that this is the first case of glomus tumor of the thumb reported from Saudi Arabia.
Conclusion
The present study is a case history with a comprehensive literature review, which points to the disadvantage of proposing causal hypotheses based on the results. It is noted in this study that future research should be designed to appraise genetic factors, bone and tendon involvement, and histological features of hand tumors with an objective to understand and identify possible predictors of reoccurrence of these tumors.
Though MRI is an extremely important tool to help in the diagnosis of glomus tumors,48,49 ultrasound is also deemed efficient enough to confirm the diagnosis as the tumor can be seen as well-defined small hypoechoic nodule/s beneath the affected area.50–52 This present case was early and easily diagnosed with confirmation as glomus tumor from the initial ultrasound scan itself. The direct complete excision offered a greater chance of a cure and thus a better functional outcome.53,54
Documenting occurrence of glomus tumor cases in unusual locations in the literature raises awareness of this condition and reduces the time needed for diagnosis, which could be very long and contribute to severe morbidity to the patient. In order to completely remove glomus tumors and prevent recurrence, accurate preoperative localization is essential.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the College of Medicine, Imam Mohammed Ibn Saud Islamic University (RC12.12.12) in human studies.
Informed Consent Statement
Informed consent was obtained from all the subjects involved in the study. It is confirmed that the patient’s informed consent for the case details to be published including the publication of the images has been obtained.
Data Sharing Statement
All data underlying the results are available as part of the article and no additional source data are required.
Funding
This study did not receive any external funding.
Disclosure
The author declares no conflicts of interest in this work.
References
1. Álvarez‐salafranca M, Bañuls J, Thomas L, et al. Dermoscopy of glomus tumour: a cross‐sectional study of 86 cases. J Eur Acad Dermatol Venereol. 2022;36(11):2016–2024. doi:10.1111/jdv.18432
2. Hamm H, Stolze I. Diseases of nails. In: Braun-Falco´ s Dermatology. Berlin, Heidelberg: Springer Berlin Heidelberg; 2022:1373–1398.
3. Haneen A, Osman GMA, Ibraheam A. Extra digital glomus tumor: a rare cause for undiagnosed chronic pain in unusual sites. Plas Surg Case Stud. 2019;5:2513826X19828796.
4. Poornima K, Sigamani K, Harke AB. Clinicopathological study of glomus tumors in a tertiary care hospital. Indian J Dermatol. 2022;67.4:480.
5. Sbai MA, Benzarti S, Gharbi W, et al. Glomus tumor of the leg: a case report. Pan Afr Med J. 2018;31(1). doi:10.11604/pamj.2018.31.186.9706
6. Xiao A, Ahlers M, Dry SM, et al. Rare malignant glomus tumor of the esophagus with pulmonary metastasis: a case report. AME Case Rep. 2022;2022:6.
7. Sbaraglia M, Businello G, Bellan E, et al. Mesenchymal tumours of the gastrointestinal tract. Pathologica. 2021;113.3:230. doi:10.32074/1591-951X-309
8. Grover C, Jayasree P, Kaliyadan F. Clinical and onychoscopic characteristics of subungual glomus tumor: a cross‐sectional study. Int J Dermatol. 2021;60:693–702. doi:10.1111/ijd.15358
9. Xie Y, Zhang F, Lineaweaver WC, et al. Risk factors associated with misdiagnosis of digital glomus tumor: a retrospective cohort study. Ann Plast Surg. 2022;89(4):376–379. doi:10.1097/SAP.0000000000003263
10. Guedes GVC, Jácome DT, Alves GF, et al. Epidemiological analysis of glomus tumors of the hand and association with recurrence rate. Revista Iberoam De Cirugía De la Mano. 2022;50(01):e27–e33. doi:10.1055/s-0042-1744466
11. Irojah B, Mullner DL, Moores C, et al. Tumors. Tip Trick Plast Surg. 2022;2022:763–780.
12. Falcone M-O, Asmar G, Chassat R. Subungual Glomus Tumor. Hand Surg Rehabilit. 2023;101607. doi:10.1016/j.hansur.2023.10.001
13. Kim YJ, Kim DH, Park JS, et al. Factors affecting surgical outcomes of digital glomus tumour: a multicentre study. J Hand Surg Europ Vol. 2018;43(6):652–658. doi:10.1177/1753193418774176
14. Faruquee SR, Kumar Saha M. Glomus tumour excision by nail sparing. J Bangl Orthop Soc. 2016; 31(2): 146–149.
15. Gong JH, Mehrzad R, Bhatt RA. Practical management of lumps and bumps of the fingers, hand, and wrist. J Am Board Family Med. 2022;35(6):1194–1203. doi:10.3122/jabfm.2022.220028R2
16. Causeret A, Lapègue F, Bruneau B, et al. Painful traumatic neuromas in subcutaneous fat: visibility and morphologic features with ultrasound. J Ultrasound Med. 2019;38(9):2457–2467. doi:10.1002/jum.14944
17. Rutkowski P, Wysocki PJ, Nasierowska-Guttmejer A, et al. Cutaneous melanoma. Oncol Clin Pract. 2020;16(4):163–182. doi:10.5603/OCP.2020.0021
18. Gharbi A, Abayed A, Abid L, et al. Cavernous hemangioma of the forearm muscles: three case reports and literature review. J Orthop Case Rep. 2023;13(10):157. doi:10.13107/jocr.2023.v13.i10.3974
19. Andrade FAL, Cadena Arteaga JA, Echeverry Morillo VL, et al. Blue rubber bleb nevus syndrome: presentation of a case and review of the literature. Radiol Case Rep. 2021;16(8):2003–2006. doi:10.1016/j.radcr.2021.04.086
20. Akyurek M, Hafiz G. Retrospective analysis of clinical findings and radiologic diagnostic methods of subungual glomus tumor: a single-center study. Eur J Plastic Surg. 2023;46(6):1247–1253. doi:10.1007/s00238-023-02123-8
21. Lee WQ, Yihan L, Eng Meng Yeo N. Glomus tumour: an institutional experience of 31 cases. J Orthopaedic Surg Res. 2023;18.1:741. doi:10.1186/s13018-023-04234-1
22. Pansa A, Samà L, Ruspi L, et al. Glomus tumor of the stomach: a systematic review and illustrative case report. Dig Dis. 2023;41(1):17–33. doi:10.1159/000525513
23. Rahbari K, Farzan M, Saffar H, et al. Glomus tumor of uncertain malignant potential in thumb: a case report and review of literature. Arch Bone Joint Surg. 2020;8(1):117. doi:10.22038/abjs.2019.35225.1928
24. Ardeleanu V, Jecan CR, Tatu AL, et al. A recurrent solitary glomus tumor of the forearm. Rom J Morphol Embryol. 2019;60:1019–1023.
25. Bordianu A, Zamfirescu D. The hidden cause of chronic finger pain: glomus tumor–a case report. J Med Life. 2019;12(1):30. doi:10.25122/jml-2018-0060
26. Rashid T, Altaf J, Husain M, et al. Glomus tumor in two non-adjacent finger tips of the same hand: a case report with literature review. Int J Med Rev Case Rep. 2021;5(8):30.
27. Saba M, Moser A, Rosenberg J, et al. Rare glomus tumor formation following trauma to the first digit. Internat J Surg Case Rep. 2021;86:106324. doi:10.1016/j.ijscr.2021.106324
28. Kumar S, Tiwary S, More R, et al. Digital glomus tumor: an experience of 57 cases over 20 years. J Fam Med Prim Car. 2020;9(7):3514. doi:10.4103/jfmpc.jfmpc_446_20
29. Hatan M, AlRabah R, Kattan AE. Unusual location of pulp glomus tumor: a case study and literature review. Plastic Reconst Surg Global Open. 2022;10:3.
30. Patel J, Vaish A, Vaishya R, et al. Reappearance of a glomus tumor of the finger after nine years-A rare case report and literature review. J Orthop Rep. 2022;1(1):38–41. doi:10.1016/j.jorep.2022.03.014
31. Rahman M, Akhter N, Iqbal A, et al. Glomus tumor of finger pulp-A Case Report. J Bangl Coll Physic Surg. 2022;40:4.
32. Dhingra M, Niraula B, Regmi A, et al. Glomus tumour of hand––A commonly misdiagnosed pathology: a case series. J West Af Coll Surg. 2022;12(4):39. doi:10.4103/jwas.jwas_171_22
33. Prashant K, Ariwala D, Mohanty SS. The glomus tumor of finger–a case series. J Orthop Case Rep. 2023;13(3):17. doi:10.13107/jocr.2023.v13.i03.3568
34. Abidin MA, Kitta MI, Nong I, et al. ”Diagnosis and surgical approach in treating glomus tumor distal phalanx left middle finger: a case report. Internat J Surg Case Rep;2023. 108426. doi:10.1016/j.ijscr.2023.108426
35. Cohen PR. Glomus extradigital tumor: a case report of an extradigital glomus tumor on the wrist and comprehensive review of glomus tumors. Cureus. 2023;15:5.
36. Santoshi JA, Kumar Kori V, Khurana U. Glomus tumor of the fingertips: a frequently missed diagnosis. J Fam Med Prim Car. 2019;8(3):904. doi:10.4103/jfmpc.jfmpc_88_19
37. Saaiq M. Presentation and management outcome of glomus tumors of the hand. Arch Bone Joint Surg. 2021;9(3):312. doi:10.22038/abjs.2020.47878.2367
38. Perţea M, Poroch V, Velenciuc N, et al. Clinical, histopathological and immunohistochemical features of glomus tumor of the nail bed. Rom J Morphol Embryol. 2021;62:233. doi:10.47162/RJME.62.1.23
39. Nikhil CS, Davis J, Muraleedharan K, et al. Glomus tumor: a case series study of 30 cases and review of the literature. J Orthop Assoc South Indian Stat. 2022;19(1):39–43. doi:10.4103/joasis.joasis_37_21
40. Hernández V, Lena T, Camacho E, et al. Digital glomus tumor: bibliographic review of the studies published over the past 10 years. Revista Iberoam De Cirugía De la Mano. 2021;49.01:046–055.
41. Mohamed WT, Jahagirdar V, Jaber F, et al. Glomus tumor of the stomach presenting with upper gastrointestinal bleeding: a case report. J Investig Med High Imp Case Rep. 2023;11:23247096231192891. doi:10.1177/23247096231192891
42. Reinders EFH, Klaassen KMG, Pasch MC. Transungual excision of glomus tumors: a treatment and quality of life study. Dermatologic Surg. 2020;46(1):103–112. doi:10.1097/DSS.0000000000002006
43. Obeid AE, Al-Nasheet H, Alsharakat AH, Yousif W, Alhassan MA. Clinical and Histopathological diagnosis of glomus tumor: a 6 year institutional retrospective study. Int J Orthopaed Sci. 2020;6:285–288. doi:10.22271/ortho.2020.v6.i4e.2352
44. Wang Y, Xiang Y, Bian Y, et al. Glomus tumors associated with the bone and joints: a review of 91 cases. Ann Translat Med. 2020;8(21):1460. doi:10.21037/atm-20-6998
45. Singal A, Bisherwal K, Agrawal S, et al. Clinico-epidemiological profile and management outcome of subungual digital glomus tumor—Indian experience. Dermatologic Therapy. 2022;35(10):e15745. doi:10.1111/dth.15745
46. Sun Y, Qi R, Wu Z, et al. The clinicopathologic and immunohistochemical features of 60 cutaneous glomus tumor: a retrospective case series study. Anais Brasil De Dermatol. 2023;99:238–243. doi:10.1016/j.abd.2023.03.005
47. Nthumba PM, Naguria Oundoh L. Glomus tumors: a systematic review of the sub-saharan Africa experience. Plast Reconst Surg. 2024;12:e5564. doi:10.1097/GOX.0000000000005564
48. Bargon CA, Mohamadi A, Talaei-Khoei M, et al. Factors associated with requesting magnetic resonance imaging during the management of glomus tumors. Arch Bone Joint Surg. 2019;7(5):422.
49. Patel T, Meena V, Meena P. Hand and foot glomus tumors: significance of MRI diagnosis followed by histopathological assessment. Cureus. 2022;14:10.
50. Chen L, Nikolić N, Mildner M, et al. Diagnosis of subungual glomus tumors with 18 MHz ultrasound and CDFI. Sci Rep. 2020;10(1):1–6. doi:10.1038/s41598-019-56847-4
51. de Almeida CA. High-frequency ultrasonography for subungual glomus tumor evaluation–imaging findings. Skell Radiol. 2023;2023:1–8.
52. Kim YB, Choi IC, Park JH, et al. High-resolution ultrasonography is a more useful primary diagnostic tool than magnetic resonance imaging for subungual glomus tumors: a single-center retrospective study. Arch Hand Microsurg. 2023;28(1):33–38. doi:10.12790/ahm.22.0060
53. Lim P, Yue B, Cavallo A. Surgical treatment of benign subungual tumours—a systematic review and case series. Austral J Plast Surg. 2023;6:1–8.
54. Pertea M, Grosu OM, Filip A, et al. Rare benign tumors and tumor-like lesions of the hand without skin damage—clinical, imagistic and histopathological diagnosis, retrospective study. Diagnostics. 2023;13(6):1204. doi:10.3390/diagnostics13061204
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

