Back to Journals » Infection and Drug Resistance » Volume 17
Study on mNGS Technique in Diagnosing Pneumocystis jirovecii Pneumonia in Non-HIV-Infected Patients
Authors Li S, Han X, Ma J, Huang GH, Yang ST, Wang CM
Received 20 November 2023
Accepted for publication 7 February 2024
Published 11 April 2024 Volume 2024:17 Pages 1397—1405
DOI https://doi.org/10.2147/IDR.S450878
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Shuai Li, Xue Han, Jing Ma, Guo-Hong Huang, Shu-Ting Yang, Chang-Min Wang
Clinical Laboratory Center, People’s Hospital of Xinjiang Uygur Autonomous Region, Urumqi, Xinjiang, 830001, People’s Republic of China
Correspondence: Chang-Min Wang, Department of Clinical Laboratory Center, People’s Hospital of Xinjiang Uygur Autonomous Region, No. 91 Tianchi Street, Tianshan District, Urumqi, Xinjiang, 830001, People’s Republic of China, Tel +86 13609992616, Fax +86− 9918564168, Email [email protected]
Objective: To investigate the value of metagenomic Next-Generation Sequencing (mNGS) in diagnosing Pneumocystis jirovecii pneumonia (PJP) in non-human immunodeficiency virus (HIV)-infected patients.
Methods: In this retrospective study, non-HIV-infected patients with PJP and those diagnosed with non-PJP from August 2022 to December 2024 were selected as subjects. The presence of Pneumocystis jirovecii (PJ) and other co-pathogens in bronchoalveolar lavage fluid (BALF) was analyzed, and the diagnostic efficacy of NGS, polymerase chain reaction (PCR) and serum 1,3-β-D-glucan (BDG) in PJP was compared with the reference standard of clinical compound diagnosis.
Results: Eighty-nine non-HIV-infected patients were recruited, with dyspnea as the primary symptom (69.66%) and solid malignant tumor as the most common underlying disease (20.22%). Taking clinical compound diagnosis as the reference standard, the sensitivity, specificity, negative predictive value and positive predictive value of mNGS were higher than those detected by PCR and serum BDG. Among 42 non-HIV-infected patients with PJP who underwent mNGS and conventional pathogen detection of BALF, 6 had simple PJ infection and 36 had combined PJ infection. The detection rate of mNGS in mixed infections was significantly higher than that of conventional pathogen detection (85.71 vs 61.70%, P = 0.012). A total of 127 pathogens were detected in BALF using mNGS, among which fungi had the highest detection rate (46.46%). The fungi, viruses and bacteria detected were mainly Pneumocystis jirovecii, human gammaherpesvirus 4 and Acinetobacter baumannii.
Conclusion: mNGS is highly effective in diagnosing non-HIV-infected patients with PJP and exhibits ideal performance in the detection of co-pathogens. In addition, it has certain value for clinical diagnosis and guidance of targeted anti-infective drug treatment.
Keywords: metagenomic next-generation sequencing, Pneumocystis jirovecii pneumonia, polymerase chain reaction, non-HIV infection
Introduction
Pneumocystis jirovecii pneumonia (PJP) is an acute or subacute pneumonia resulting from infection with Pneumocystis jirovecii (PJ). It may initially cause dyspnea, fever, and dry cough, and in severe cases, death.1 As an opportunistic infection, it occurs in immunocompromised or compromised hosts and is one of the most common complications of human immunodeficiency virus (HIV). It also frequently makes inroads on non-HIV immunocompromised people with hematological malignancies, hematopoietic stem cell transplantation, autoimmune diseases, inflammatory diseases, and immunosuppressive therapy.2 Recent decades have witnessed a decrease in the incidence and mortality of PJP in HIV-infected patients due to routine use of chemoprophylaxis and antiretroviral therapy.3 In contrast, the incidence of PJP in non-HIV-infected patients increased significantly.4 Studies have shown that the mortality rate of PJP in HIV-infected patients is less than 10%, while it is as high as 25% to 55% in non-HIV-infected patients.5 Delayed diagnosis and treatment of PJP will affect the prognosis of patients and bring a huge economic burden to families and society. Therefore, pathogen identification and clinical intervention of PJP should be carried out at an early stage, which is crucial to reduce mortality and improve the prognosis of patients.
In the previous practice, the diagnosis of PJP depended on observing respiratory specimens under a microscope after routine or immunofluorescence staining. However, the low fungal load and low sensitivity of routine staining resulted in negative reports that were far from sufficient to rule out a diagnosis of PJP. In addition, immunofluorescence staining is not routinely performed in many hospitals.6 1,3-β-D-glucan (BDG) is currently a common serological biomarker for auxiliary diagnosis of PJP, but it lacks specificity.7 Polymerase chain reaction (PCR) is widely used to detect PJ because of its good sensitivity and specificity, but it has limited value in single detection of mixed infection.8 Therefore, there is an urgent need to explore a more accurate and efficient microbial diagnostic tool for detecting PJP in non-HIV populations.
With the advent of the metagenomic Next-Generation Sequencing (mNGS) technique, pathogen detection approaches are increasingly diverse. mNGS refers to the use of high-throughput sequencing and bioinformatics analysis technology for gene sequencing of all microbial nucleic acids extracted from different types of clinical samples. It can be used to obtain all microbial information in samples in an efficient, objective and accurate way and provide a new means for identifying pathogenic infection.9 At present, the vast majority of studies on mNGS focus on the diagnosis and treatment of bacterial infections, but rarely on the diagnosis and treatment of fungal infections, especially non-HIV-infected PJP. To this end, we specifically designed this study to investigate the value of mNGS in the diagnosis and treatment of non-HIV-infected patients with PJP.
Materials and Methods
Subjects
This retrospective study selected non-HIV-infected PJP patients and non-PJP patients diagnosed in the People’s Hospital of Xinjiang Uygur Autonomous Region from August 2022 to December 2024 as the research objects. Forty-two PJP patients without HIV infection were selected as the case group, and 46 patients with pulmonary infection who were admitted to the hospital during the same period and subsequently diagnosed as non-PJP were selected as the control group. Inclusion criteria for non-HIV-infected PJP patients: (1) Pneumocystis jirovecii was detected in lower respiratory tract specimens;10 (2) Immunocompromised patients, including but not limited to hematological diseases, rheumatic connective tissue diseases, long-term use of corticosteroids or immunosuppressants, solid organ transplantation, solid tumors, etc.; (3) The patient was definitely diagnosed as non-HIV-infected person; (4) Those with PJ nucleic acid positively detected by PCR or PJ gene sequence detected by mNGS. A clinical compound diagnosis of PJP or non-PJP was made jointly by two experienced clinicians. Inclusion criteria for non-PJP patients: (1) Patients with fever, dyspnea, cough, expectoration and other respiratory symptoms; (2) The patient’s imaging findings were pale patchy shadows with increased density with blurred edges, which could also be manifested as patchy consolidation shadows or ground glass shadows; (3) PCR detection of PJ nucleic acid was negative, and mNGS detection of PJ gene sequence was negative; (4) Sputum culture or bronchoalveolar lavage fluid specimens produced a clear pathogen. The exclusion criteria were as follows: (1) Patients with missing important case data; (2) Those with infection in other sites; (3) Those aged <18 years old; (4) Those co-infected with HIV. This study was approved by the Ethics Committee of our hospital. All patients or family members have signed an informed consent form, this was conducted in accordance with the Declaration of Istanbul, and all organs were donated voluntarily with written informed consent.
Study Methods
All patients underwent fiberoptic bronchoscopy, and their bronchoalveolar lavage fluid (BALF) samples were collected. Subsequently, each BALF sample was divided into aliquots for routine microbial tests (including PCR detection and traditional culture) and mNGS, and blood samples were sent for related tests.
Sample Processing and DNA Extraction for mNGS Detection
Enzyme and 100 g of 0.5 mm glass beads were added to the 600 μL sample taken and vortexed for 30 min [(1200–1500) × g]; Then, 300 μL of the shaken supernatant was transferred to a 1.5 mL centrifuge tube for nucleic acid extraction. Three to five milliliters of anticoagulated venous blood samples were centrifuged for 10 min at 4°C and 1600 g, and the plasma was transferred to a 2 mL centrifuge tube for DNA extraction. DNA was extracted using the Huada Nucleic Acid Extraction Kit.
DNA Library Construction and Sequencing
MGIEasy Cell-free DNA Library Prep Set (batch No.: 108420230) was utilized to construct the DNA library by DNA fragmentation, end repair and PCR amplification. This technique transforms double-stranded DNA into single-stranded circular DNA via DNA degradation and cyclization and then loads the qualified DNA onto the chip. DNA library nanospheres were prepared by using the MGISP-100 automated sample preparation system. After preparation, the concentration was determined for quality control, which was required to be ≥8ng/ul. The nanospheres with qualified concentration, nanospheres loading buffer and nanospheres polymerase mixed solution were configured into a loading system and were put into the MGISEQ-2000 platform for gene sequencing together with sequencing slides.
Bioinformatics Analysis
The results of gene sequencing were preliminary data, which need to be further processed. First, high-quality data were obtained by removing low-quality data and data with reads of length less than 35bp.9 The high-quality data were aligned to the human genome (hg19) by using the Burrows-Wheeler Aligner software (BWA: http://bio-bwa.sourceforge.net/), and then the data containing the host human nucleic acid sequence were removed. The remaining data were compared with a dedicated microbial database after removing low-complexity sequences, and the sequenced data were classified and arranged according to viruses, bacteria, fungi and parasites. The classification reference database can be downloaded from NCBI (ftp://ftp.ncbi.nlm.nih.gov/genomes/). As to the threshold criteria for interpretation of mNG, the microbial species-specific read number (SSRN) method was used to interpret the sequencing results. For Pneumocystis jirovecii, SSRN, that is, Pj reads ≥1, was used as the positive criterion in this study to ensure sensitivity.
Data Collection
The basic information (demographics, clinical symptoms, underlying diseases, etc.), laboratory indicators, BALFmNGS, PCR, serum BDG, etc. of the patients were collected.
Statistical Analysis
All data collected in this study were statistically analyzed using SPSS 26.0 software and plotted by GraphPad 8.0. Measurement data conforming to normal distribution were presented as mean ± standard deviation (x±s), and the independent sample t-test was used for comparison between the two groups. Non-normally distributed measurement data were expressed as median (interquartile interval) [M (P25, P75)], and the Mann⁃Whitney U-test was used for comparison between the two groups. Count data were expressed as frequency (%), and χ2 test or Fisher’s exact test was used for comparison between groups. Taking the clinical compound diagnosis (whether Pneumocystis jirovecii was detected in lower respiratory tract specimens) as the reference standard,10 the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated, and P < 0.05 was considered a statistically significant difference.
Results
Clinical Data
Eighty-nine non-HIV-infected patients were recruited in this study, including 57 males (64.04%) and 32 females (35.96%), aged from 22 to 83, with an average age of 58.34 ± 17.44. Most patients had dyspnea as the primary symptom (69.66%) and solid malignant tumor (20.22%) as the most common underlying disease. Laboratory examination showed that the absolute value of the median lymphocyte count was 0.41×109/L, and the median CD4+T lymphocyte count was 117.0/L, both of which were lower than the lower limit of the normal reference range. See Table 1 for details.
 |
Table 1 Clinical Data of Non-HIV Patients |
Diagnostic Efficacy of MNGS, PCR and Serum BDG Detection in PJP
Taking clinical compound diagnosis as the reference standard, the sensitivity, specificity, negative predictive value and positive predictive value of mNGS were all 100%, those of PCR detection were 90.48%, 91.49%, 90.48% and 91.49%, respectively, and those of BDG detection were 73.81%, 80.85%, 77.50% and 77.55%, respectively. It can be seen that the diagnostic efficiency of mNGS is significantly higher than that of PCR detection and serum BDG detection (Table 2).
 |
Table 2 Diagnostic Efficacy of mNGS, PCR and Serum BDG Detection in Non-HIV-Infected PJP |
Detection of Mixed Infections by mNGS and Conventional Pathogen Detection Technologies
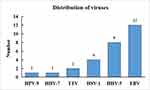
Among 42 non-HIV-infected patients with PJP who underwent mNGS and conventional pathogen detection of BALF, 6 (14.29%) had simple PJ infection and 36 (85.71%) had combined PJ infection. The detection rate of mNGS in mixed infections was significantly higher than that of conventional pathogen detection (85.71 vs 61.70%, P = 0.012) (Table 3). Among mixed infections, fungi combined with bacteria and viruses were the most common (20 cases) (Figure 1).
 |
Table 3 Comparison Between mNGS and Traditional Detection of Infection |
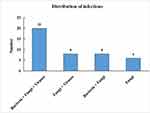 |
Figure 1 Distribution of mixed infections in patients with PJP. Abbreviation: PJP, Pneumocystis jirovecii pneumonia. |
Distribution of Pathogens of MNGS in Non-HIV-Infected Patients with PJP
In 42 non-HIV-infected patients with PJP, 127 pathogens were detected by mNGS in alveolar lavage fluid, among which the detection rate of fungi was the highest (46.46%). The fungi detected were mainly Pneumocystis jirovecii (42 cases) and Streptococcus albicans (8 cases) (Figure 2). The main bacteria detected were Acinetobacter baumannii (6 cases) and Staphylococcus aureus (4 cases) (Figure 3). The viruses detected are mainly human gammaherpesvirus 4 (12 cases) and human betaherpesvirus 5 (8 cases) (Figure 4).
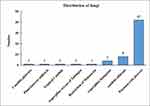 |
Figure 2 Distribution of fungi in non-HIV-infected patients with PJP. Abbreviations: PJP, Pneumocystis jirovecii pneumonia; HIV, human immunodeficiency virus. |
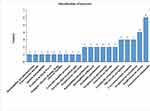 |
Figure 4 Distribution of bacteria in non-HIV-infected patients with PJP. Abbreviations: PJP, Pneumocystis jirovecii pneumonia; HIV, human immunodeficiency virus. |
Discussion
Pneumocystis jirovecii is an opportunistic pathogenic fungus that enters the lungs through the respiratory tract, mostly presenting as an asymptomatic infection. If left untreated on time, it will easily develop into acute respiratory distress syndrome, which is also one of the primary causes of death among AIDS patients.11 Given the possible variation in the host immune response to PJ, PJP is a relatively inert process in HIV-infected patients, which usually develops into a subacute or chronic course. In contrast, PJP in non-HIV-infected patients is mostly acute, with rapid progress of lung lesions, high risk of respiratory failure and high mortality.12 Ko et al13 found that delayed initiation of specific anti-infective therapy or initially unsuccessful antimicrobial therapy resulted in acute respiratory failure with poor prognosis in non-HIV-infected patients with PJP. Rapid diagnosis and early initiation of treatment for PJP yields a better prognosis.
PJ has difficulty in being diagnosed due to a low inoculation amount in the respiratory tract of patients, which is usually negative by direct microscopic examination of smears.14 In the current microbiological diagnosis of PJP, two detection technologies, PCR and serum BDG, are preferred. In particular, PCR technology can quantitatively detect PJ in respiratory secretions. It was found in the present study that PCR has high sensitivity (90.48%) and specificity (91.49%). Salzer et al15 concluded that the sensitivity of PJ in BALF detected by PCR was 94%-99%, and the specificity was 89%–91%, which was consistent with the results of this study. However, PCR has limitations in the diagnosis of PJP. Contamination, colonization, etc. may cause false-positive results. Studies have shown that quantitative PCR (qPCR) seems to improve diagnostic efficiency, but there is controversy regarding the threshold required to distinguish PJ colonization from infection.16 Furthermore, PCR has limited value in the single detection of mixed infections, despite its higher detection value in single infections. In contrast, mNGS has higher diagnostic efficiency in PJP and higher diagnostic value in mixed infections. mNGS is a good choice when the conventional anti-infection treatment is not effective and mixed infection is considered. BDG is a structural polysaccharide produced in the process of cell wall synthesis of many pathogenic fungi. At present, it is primarily used in the auxiliary diagnosis of pulmonary invasive aspergillosis and invasive candidiasis.17 Several observational studies in recent years have described the use of BDG detection for the presumptive diagnosis of PJP. Studies have shown that BDG detection can be used as a minimally invasive screening test for the presumed diagnosis of PJP without invasive fibrobronchi.18 However, BDG is prone to false-positive results in the diagnosis of PJP, resulting in the termination of the diagnosis (in the case of positive results, the diagnosis is generally not terminated), especially in critically ill patients. Therefore, further confirmatory testing is required when performing BDG detection.19 mNGS is superior to BDG in that it has better diagnostic performance and can identify pathogenic microorganisms quickly, objectively and without bias.
MNGS is a novel microbial detection and identification technique that can identify pathogenic microorganisms quickly, impartially and objectively compared with conventional detection techniques. It has obvious advantages in the early diagnosis of unknown pathogens, pathogens that are difficult to culture, conditional pathogens, mixed pathogen infections and difficult infections, and provides a new means for accurate anti-infection treatment.20 However, there is currently no complete knowledge of the diagnostic performance of mNGS in PJP. In this study, the sensitivity and specificity of mNGS in non-HIV-infected patients with PJP were both 100%, which was significantly better than that of serum BDG and PCR detection. These results show that early application of mNGS is beneficial to promote the rapid and accurate diagnosis of PJP. Besides, the detection rate of mixed infection in BALF using mNGS was significantly higher than that of conventional pathogen detection, suggesting that mNGS has advantages in identifying co-pathogens in patients with PJP mixed infection. This is consistent with the results by Duan et al.21 More studies by Li et al10 explored the diagnostic value of mNGS in AIDS patients complicated with PJ infection, and the results showed that the coincidence rate of mNGS detection was 100%. This is consistent with the results of this study. In the present study, the mNGS technique was used to detect not only the target pathogen but also the mixed infection of other pathogens, among which mixed infections with herpes viruses were the most common. Meanwhile, the infection of bacteria, viruses and fungi is also common, which can provide guidance for effective anti-infection treatment.
There are still certain limitations in this study: this is a single-center study with bias in patient group selection; Besides, this is also a retrospective study with limited sample size. In response to this, further prospective study is needed to confirm the application value of mNGS in the diagnosis and treatment of PJP infection in non-HIV patients.
Conclusion
To sum up, compared with serum BDG and PCR detection, mNGS has obvious advantages in the diagnosis of non-HIV-infected PJP, with its rapid detection speed, short reporting time, high sensitivity and specificity, and high detection rate of mixed infection. It has a certain value for early clinical diagnosis and guiding targeted treatment.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of People’s Hospital of Xinjiang Uygur Autonomous Region. Due to the nature of retrospective study and anonymized patient's information, informed consent is waived with the approval of Ethics Committee of People’s Hospital of Xinjiang Uygur Autonomous Region. All methods were carried out in accordance with relevant guidelines and regulations.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Study on NGS technique for diagnosis of Pneumocystis yerbii pneumonia in non-HIV infected patients (20220104).
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately.
References
1. Apostolopoulou A, Fishman JA. The pathogenesis and diagnosis of Pneumocystis jiroveci Pneumonia. J Fungi. 2022;8(11):1167. PMID: 36354934; PMCID: PMC9696632. doi:10.3390/jof8111167
2. Bateman M, Oladele R, Kolls JK. Diagnosing pneumocystis jirovecii pneumonia: a review of current methods and novel approaches. Med Mycol. 2020;58(8):1015–1028. PMID: 32400869; PMCID: PMC7657095. doi:10.1093/mmy/myaa024
3. Huang YS, Yang JJ, Lee NY, et al. Treatment of Pneumocystis jirovecii pneumonia in HIV-infected patients: a review. Expert Rev Anti Infect Ther. 2017;15(9):873–892. PMID: 28782390. doi:10.1080/14787210.2017.1364991
4. Tang G, Tong S, Yuan X, et al. Using routine laboratory markers and immunological indicators for predicting Pneumocystis jiroveci Pneumonia in immunocompromised patients. Front Immunol. 2021;12:652383. PMID: 33912176; PMCID: PMC8071988. doi:10.3389/fimmu.2021.652383
5. Yang L, Xia P, Zhou Y, et al. Characteristics and risk factors for Pneumocystis jirovecii pneumonia in patients with idiopathic membranous nephropathy. Eur J Clin Microbiol Infect Dis. 2021;40(11):2305–2314. PMID: 34047874. doi:10.1007/s10096-021-04227-0
6. Weyant RB, Kabbani D, Doucette K, et al. Pneumocystis jirovecii: a review with a focus on prevention and treatment. Expert Opin Pharmacother. 2021;22(12):1579–1592. PMID: 33870843. doi:10.1080/14656566.2021.1915989
7. Zhou S, Linder KA, Kauffman CA, et al. Diagnostic performance of bronchoalveolar lavage (1,3)-β-d-glucan assay for Pneumocystis jirovecii Pneumonia. J Fungi. 2020;6(4):200. PMID: 33019729; PMCID: PMC7712134. doi:10.3390/jof6040200
8. Lussac-Sorton F, Fleur T, Voisin T, et al. Interest of a commercialized Pneumocystis jirovecii quantitative PCR to discriminate colonization from Pneumocystis Pneumonia according to the revised EORTC/MSGERC criteria. J Clin Med. 2022;12(1):316. PMID: 36615116; PMCID: PMC9821677. doi:10.3390/jcm12010316
9. Wu X, Li Y, Zhang M, et al. Etiology of severe community-acquired Pneumonia in adults based on metagenomic next-generation sequencing: a Prospective Multicenter Study. Infect Dis Ther. 2020;9(4):1003–1015. PMID: 33170499; PMCID: PMC7652912. doi:10.1007/s40121-020-00353-y
10. Li XQ, Yang CL, Mao YH, et al. The diagnostic value of metagenomic next-generation sequencing in AIDS patients complicated with Pneumocystis jirovecii infection. Chin J Lab Med. 2023;46(2):169–175. doi:10.3760/cma.j.cn114452-20220408-00207
11. Cillóniz C, Dominedò C, Álvarez-Martínez MJ, et al. Pneumocystis pneumonia in the twenty-first century: HIV-infected versus HIV-uninfected patients. Expert Rev Anti Infect Ther. 2019;17(10):787–801. PMID: 31550942. doi:10.1080/14787210.2019.1671823
12. Wang Y, Zhou X, Saimi M, et al. Risk factors of mortality from Pneumocystis Pneumonia in non-HIV patients: a meta-analysis. Front Public Health. 2021;9:680108. PMID: 34222179; PMCID: PMC8244732. doi:10.3389/fpubh.2021.680108
13. Ko Y, Jeong BH, Park HY, et al. Outcomes of Pneumocystis pneumonia with respiratory failure in HIV-negative patients. J Crit Care. 2014;29(3):356–361. PMID: 24440053. doi:10.1016/j.jcrc.2013.12.005
14. Zakrzewska M, Roszkowska R, Zakrzewski M, et al. Pneumocystis Pneumonia: still a serious disease in children. J Mother Child. 2021;23(3):159–162. PMID: 33759428; PMCID: PMC8522405. doi:10.34763/devperiodmed.20192303.159162
15. Salzer HJF, Schäfer G, Hoenigl M, et al. Clinical, diagnostic, and treatment disparities between HIV-infected and non-HIV-infected immunocompromised patients with Pneumocystis jirovecii Pneumonia. Respiration. 2018;96(1):52–65. PMID: 29635251. doi:10.1159/000487713
16. Chagas OJ, Nagatomo PP, Pereira-Chioccola VL, et al. Performance of a real time PCR for Pneumocystis jirovecii identification in induced sputum of AIDS patients: differentiation between Pneumonia and colonization. J Fungi. 2022;8(3):222. PMID: 35330224; PMCID: PMC8950466. doi:10.3390/jof8030222
17. Pan T, Tan R, Qu H, et al. Next-generation sequencing of the BALF in the diagnosis of community-acquired pneumonia in immunocompromised patients. J Infect. 2019;79(1):61–74. PMID: 30476493; PMCID: PMC7133759. doi:10.1016/j.jinf.2018.11.005
18. Yoshida M. Development of a method of measuring β-D-glucan and its use in preemptive therapy for invasive fungal infections. Int J Mol Sci. 2021;22(17):9265. PMID: 34502174; PMCID: PMC8431658. doi:10.3390/ijms22179265
19. Szvalb AD, Malek AE, Jiang Y, et al. Serum (1,3)-Beta-d-glucan has suboptimal performance for the diagnosis of Pneumocystis jirovecii pneumonia in cancer patients and correlates poorly with respiratory burden as measured by quantitative PCR. J Infect. 2020;81(3):443–451. PMID: 32650108. doi:10.1016/j.jinf.2020.07.003
20. Zhang P, Chen Y, Li S, et al. Metagenomic next-generation sequencing for the clinical diagnosis and prognosis of acute respiratory distress syndrome caused by severe pneumonia: a retrospective study. PeerJ. 2020;8:e9623. PMID: 32821543; PMCID: PMC7395598. doi:10.7717/peerj.9623
21. Duan J, Gao J, Liu Q, et al. Characteristics and prognostic factors of non-HIV immunocompromised patients with Pneumocystis Pneumonia diagnosed by metagenomics next-generation sequencing. Front Med Lausanne. 2022;9:812698. PMID: 35308503; PMCID: PMC8928194. doi:10.3389/fmed.2022.812698
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.