Back to Journals » Journal of Blood Medicine » Volume 14
Systematic Workup of Transfusion Reactions Reveals Passive Co-Reporting of Handling Errors
Authors Nitsche E, Dreßler J, Henschler R
Received 5 March 2023
Accepted for publication 19 June 2023
Published 8 August 2023 Volume 2023:14 Pages 435—443
DOI https://doi.org/10.2147/JBM.S411188
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Martin H Bluth
Elisabeth Nitsche,1,2 Jan Dreßler,2,* Reinhard Henschler1,*
1Department of Forensic Medicine, Institute of Legal Medicine, University of Leipzig, Leipzig, Saxony, Germany; 2Department of Quality Control, Institute of Transfusion Medicine, University Hospital Leipzig, Leipzig, Saxony, Germany
*These authors contributed equally to this work
Correspondence: Reinhard Henschler, Institute of Transfusion Medicine, University Hospital Leipzig, Johannisallee 32, Leipzig, Saxony, 04103, Germany, Tel +49 341 97 25300, Email [email protected]
Introduction: Reporting of transfusion reactions is good practice and required by many guidelines. Errors in the transfusion chain can also lead to severe patient reactions and depend on active error reporting. We aimed to characterize transfusion incidents and asked whether workup of transfusion reactions may also contribute to revealing logistical errors.
Methods: Transfusion medical records from 2011 to 2019 at our tertiary medical centre, as well as forensic autopsy reports, digitized sections, and court records from 1990 to 2019 were analysed. A total of 230,845 components were transfused between 2011 and 2019 at our own institution.
Results: Overall, 322 transfusion incidents were reported. Of these, 279 were from our own institution, corresponding to a frequency of 0.12% of all transfusions. The distribution of reaction types is consistent with the literature, with allergic reactions (55.9%), febrile-non-hemolytic reactions (FNHTR, 24.2%), hemolytic reactions (3.4%) and other types at smaller frequencies (< 3%). Twenty-nine (10.4%) of the 279 reports revealed logistical errors, including hemoglobin above guideline threshold (4.3%), incorrect or non-performed bedside tests (3.2%), inadequate patient identification (2.5%), laboratory and issuing errors, missed product checks or failure to follow recommendations (1.1% each). Eight of 29 (27.5%) of the logistical errors were detected by serendipity during workup of incident reports. In addition, 8/932 autopsy cases under code A14 (medical treatment errors) were found to be transfusion-associated (0.9%).
Conclusion: Systematic workup of transfusion incidents can identify previously undetected errors in the transfusion chain. Passive reporting of errors through the recording of side effects may serve as a tool to assess more closely assess the frequency and quality of handling errors in real life, and thus serve to improve patient safety.
Keywords: adverse transfusion reactions, near miss, hemovigilance, allergic transfusion reaction
Introduction
Blood transfusions rank among the most frequently performed procedures in clinical practice.1 Despite multiple precautious measures, transfusion-related adverse effects still cause significant morbidity in patients and may also lead to death.2–5 Transfusion reactions have been classified into several main types by international consensus criteria such as by the International Haemovigilance Network.6–8 The term “transfusion incident” includes, in addition to transfusion reactions, any unintended effect in the patient and/or deviation from established rules and guidelines that occurs before, during or after a transfusion,6,9 whereas “near miss” refers to any error that, if not noticed, may lead to faults such as incorrect determination of the blood group or transfusion of the wrong blood product but has been noticed before administration.9–11 The recording of handling errors, logistical difficulties and uncertainties as well as near miss events have not been regulated uniformly worldwide and currently lack international standardisation.
The aim of our study was to explore adverse transfusion reactions using a retrospective observational analysis and to identify handling errors and other logistical deficiencies by potential co-reporting in incident reports. This would allow improving patient safety and provide learning material to further sensitize transfusion staff to the handling of blood products.
Materials and Methods
At our institution, an active error reporting system is in place, with obligatory reporting of all suspected and obvious transfusion incidences. These are discussed with the transfusion officer of the respective department and with the head of the immune hematology laboratory. The reports are finalized and submitted to the supervisory authority by a designated person for pharmaceutical alerts. A total of 322 transfusion incidents, 314 of which had been reported in the Paul Ehrlich Institute documentation form (Langen, Germany, www.pei.de/haemovigilanz-formulare) between January 1, 2011 and December 31, 2019 to the Institute of Transfusion Medicine Leipzig were included in the study. Of these, 279 occurred at the University Hospital Leipzig covering a total of 230,845 transfusions comprising 150,775 erythrocyte concentrates (RCC), 43,247 platelet concentrates (PC) and 36,823 units of frozen fresh plasma (FFP). Another 35 cases were reported by external hospitals and medical practices supplied with blood products from the Institute of Transfusion Medicine Leipzig. Incompletely documented cases (2.8%) were recognized by absence of documented symptoms and excluded from evaluation. Forensic autopsy reports were available for a period from 1990 until 2019 and reported an additional 8 cases related to transfusions in an extended period (in total: 322 cases). Furthermore, all files with the code A14 (medical treatment errors) from 1990 to 2019 at the Institute of Legal Medicine of Leipzig University were consulted (n = 932), and a selection of medical records from the years 2010 to 2019 at the Institute of Legal Medicine of the University of Dresden and the Public Prosecutor’s Office in the City of Chemnitz were made available by personal communication. Inclusion criteria were documented occurrence or suspicion of a transfusion reaction in the course of the hospital or outpatient unit stay or the presence of a documented transfusion incident evaluated as contributing to the course of the disease. The study protocol was approved by the institutional ethics committee. For statistical analysis, SPSS statistics was used (JMP Statistical Discovery LLC, D- 69188 Heidelberg). Cramér’s V calculations were used to measure the effect strength for chi-square tests. Values are between 0 and 1, with higher values indicating a stronger relationship between two nominally scaled variables. Statistical significance was assumed if p < 0.05.12
Results
Between January 1, 2011 and December 31, 2019, 314 cases of transfusion incidents were reported and filed. A total of 279 cases were reported from the University Hospital, and 35 from other institutions to which blood components were delivered, including other hospitals and external medical practices. At the Institutes of Legal Medicine, 8 autopsy cases were reported as associated with transfusions between 1990 and 2019. Three additional cases in the hospital cohort were associated with death (total, 11). The patients’ age ranged from 0 to 92 years (M = 53.0 years, median = 60.0, SD = 24.4 years). The disease reports originated mainly from hematology (34.4%), from surgical departments (21.5%), or other departments of internal medicine (17.1%; Figure 1A and B). The highest proportion of transfusion incidents was reported in standard care wards (78.9%) and intensive/intermediate care wards (13.4%). Other documented locations were outpatient units (3.4%), accident and emergency department (1.6%) and operating theatres (0.9%). In 1.8%, information on the site was missing.
In 80.4% of cases, treating physicians followed the guidelines of the Federal Medical Association13 for the workup of transfusion incidents and provided answers to all items. This included laboratory diagnostic parameters, immunohematology and microbiology. In 19.6% of the cases, only partial or no information was provided. As shown in Table 1, indications for transfusions were described most frequently as anemia, thrombocytopenia, and decreased hemoglobin (84.1% of cases). No information on the indication was given in 27 cases (8.4%). Multiple nominations were possible. Clinical symptoms of a reaction after administration of the blood product were documented in 96.3% of incidents. The most common causes were discomfort, increased temperature, chills and urticaria/itching (Figure 2).
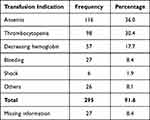 |
Table 1 Distribution of Transfusion Indications in the Study Period |
Transfusion reactions were recorded most frequently in the departments of Surgery (19.9%), Internal Medicine (13%) and Intensive Care (11.8%). About 98.4% of all cases were reported as incidents. Three of the incidents were falsely reported as “near miss” events (0.9%), ie they were found to be adverse events, but the report classified them as a near miss. Incidents were noticed by clinical symptoms in 89.4% of the cases. Table 2 shows a breakdown of the types of reaction. The most commonly classified type of incident was allergic reaction (55.9%), followed by FNHTR (24.2%) and hemolytic reactions (3.4%). Incompletely documented cases resulted in non-classified reactions and occurred in 2.8%. Other types of reactions represented reactions upon suspected causative factors including immunohematological reactions, incompatible cross-matches and bacterial contamination.
 |
Table 2 Distribution of Transfusion Incidents by Type of Reaction |
Severe reactions were defined when they were either fatal or life-threatening, or accompanied by disability, or when resulting in an extended hospital stay.8 Transfusion reactions were classified as non-severe in 49.4% of cases (n = 159) and severe in 24.5% (Table 2). Allergic reactions and FNHTR were the most commonly reported. This was followed by hemolytic events and TACO/TRALI. Information on severity was missing in 26.1% of cases (n = 84). If the patient showed symptoms, but they did not meet the criteria for a transfusion reaction, a transfusion incident was documented as non-causative or unlikely.
Operational errors by staff were found in 29 (10.4%) of the 279 incidents reported from the University Hospital where a total of 230,845 components were transfused, resembling a rate of 1.26 per 10,000 transfusions (0.12%; Table 3). These included transfusion above the upper limit of the hemoglobin threshold (4.3%), omission or incorrect performance of the bedside test (3.2%), insufficient identity control of the blood product and the patient resulting in transfusing the blood product to the wrong patient (2.5%), lab errors, con-compliance with transfusion recommendation (eg warm transfusion) or omitted product quality check (eg expired product; 1.1% each). Operational errors were classified as serious incidents, except for hemoglobin values exceeding the upper guideline limit.
 |
Table 3 Distribution of Errors and Relative Frequencies |
In addition to the cases identified through the hemovigilance system, we analyzed autopsy reports to search for transfusion errors that may have contributed to fatal outcome. Eight cases were identified in the Legal Medicine institutions as associated with a transfusion from a total of 932 section reports between 1990 and 2019. Table 4 shows the diagnoses, symptoms and their potential relation to the transfusion. In one case, transfusion of ABO incompatible RCC was considered a major contributing cause.
 |
Table 4 Legal Medicine Cases Associated with Blood Transfusions and Nature of Reported Transfusion Incidents (Observation Period from 1990 to 2019) |
Clinical consequences were derived or recommended in 23.3% of the cases. In 14.7%, the conclusions addressed the organisation of the transfusion chain. These included inspections by the transfusion officer and audits (2.7%), enforcement of close patient monitoring during transfusion (6.7%), references to instructions (8.0%), recommendations for training modules for transfusion staff (5.3%) and case review conferences (2.7%, multiple nominations were possible).
The indication for a red cell transfusion is defined via the pretransfusion hemoglobin value and the patient’s hypoxia risk status.13,14 In patients without risk factors, a hemoglobin threshold of <7 g/dL (4.3mmol/L) is considered restrictive. If there are risk factors, it is set between 7 and 10 g/dL (4.3–6.2mmol/L). The indication for an RCC transfusion according to hemoglobin value <6.2 mmol/L was given in 88/92 (95.7%) of the analysed RCC transfusions studied (Table 5). In 4.3% (4/92 cases with available pretransfusion hemoglobin values), RCC transfusions were not indicated according to the guidelines, representing too high hemoglobin as the most frequent transfusion error.
 |
Table 5 Available Hemoglobin Values of Patients Before RCC Transfusion |
Statistical analysis explored potential associations between types of component administered, types of reaction, clinical symptoms, severity of symptoms and patients age. Only a moderate effect size (Cramér’s V = 0.427, p < 0.001) was found for the association between RCC administration and the type of transfusion incident, or type of transfusion reaction and administration of FFPs (Cramér’s V = 0.232, p = 0.040) or PCs (Cramér’s V = 0.384, p < 0.001). All other associations were not significant except for the clinical symptoms with FFP (Cramér’s V = 0.176, p = 0.002), incident type and clinical symptoms (Cramér’s V = 0.739, p < 0.001) and severity of the transfusion reaction and RCCs.
Discussion/Conclusions
In this study, we report on a total of 322 transfusion incidents, of which 279 were from our University Hospital representing a total of 230,845 transfusions which allowed frequency calculations. The most frequently reported types of incident were allergic reactions and FNHTR.
Clinical symptoms were reported in 96.3% of the patients and were mostly discomfort (44.1%) or an increase in temperature (34.2%). No symptoms were reported in 3.1% of cases, and in 0.6% documentation was missing. The comparative study by Hatayama et al 20182 reported that clinical symptoms were present in 99.9% of the cases. Here, the largest group was allergic symptoms (urticaria, pruritus, rash) with 68.1%. These figures indicate that the recognition of transfusion incidents might rely on subjective observation and interpretation of symptoms and relating them to the transfusion.
The distribution of the types of adverse transfusion reactions corresponds to internationally reported data, including Serious Hazards of Transfusion (SHOT) reports from the United Kingdom and reports from the International Haemovigilance Network (IHN).8,10 For example, allergic reactions and FNHTR were reported in a total of 80.1% of all incidents in our study. Similarly, Saha et al 2020,15 Goel et al 201916 and Moncharmont et al 201817 also identified these two types of incident as the largest groups. The observed frequency of incidents of 0.12% in our study is at the lower end of the frequencies described by other authors, which ranked from 0.13% to 2.6%.2,15,17–19
In addition to adverse events, we found actively reported administrative and logistic errors in about 13% of the reports, corresponding to a rate of 1.26/10.000 transfusions (0.12%). Vossoughi et al18 report an error rate of about 0.15% of all transfusions by active reporting. Similarly, the British SHOT system in the 2021 report20 summarized 2569 errors, which corresponds to a reported error rate of approximately 0.1%. However, SHOT reported a total of 15 cases of ABO incompatible RCC transfusions during the 2018–2021 period, corresponding to about 0.0001% (one per million), whereas our study based on a “passive” co-reporting in cases of transfusion adverse events found three ABO incompatible RCC transfusions in 230,845 transfusions, corresponding to 0.001% (ten per million). Although the numbers are low, this suggests a trend towards a higher rate of ABO incompatible transfusions compared with current SHOT data, and it corresponds to the rate of ABO incompatible RCC transfusions that were measured in the UK SHOT systems in the late 1990s and early 2000s.20
The results of the workup of transfusion adverse event files yielded 8 accidentally detected errors within the 279 reports (2.7%; see Table 3) or of 0.003% (1:28.800) per 230,845 transfusions. This indicates that active reporting of near miss events can be further developed in our hospital, in order to improve patient safety.
Interestingly, we found that staff errors were involved in 29/279 (10.4%) of the reported incidents. Of these, 8 (about one-third; 2.9% of all reported incidents from the University Hospital) were not the cause of the report but were instead detected by serendipity during the workup of the reported incidents. If this rate is applied to all transfusions, this would amount to 6619 errors per 230,845 transfusions. These data point to the substantial potential of systematic workup of transfusion incident reports to detect logistical errors. It demonstrates that the workup of transfusion incidents may reveal information of logistical errors by a “passive” reporting more efficiently than an “active” reporting. Standardized and detailed workup of transfusion reactions can therefore be employed to detect abnormalities and errors and may yield additional detection of incidents reported by an active error reporting.
The second most frequent passively detected error after too high hemoglobin values was the incorrect execution or omission of the bedside test (3.2% of all reported incidents). The bedside test is mandatory in Germany before all RCC transfusions, including emergency transfusions.21 This points to deficits in compliance with the written operating procedures and provides a strong basis for additional training of the transfusing personnel.
The limitations of this observational study were that not all reactions were reported in the same way and that some cases were incompletely documented. Transfusion medical files were often lacking at least one parameter (n = 222) or were completed in handwritten form. This problem did not occur in the sectional files of the forensic institutes, which were always based on a schema with a defined sequence of documentation and which was available digitally. Reports from the UK SHOT cohort20 describe the benefits of a standardized collection of thematic data. Cases are centrally recorded and evaluated, facilitating comparability with other registries.8,20,22 As a consequence at our University Hospital, we therefore introduced a digital documentation instead of hand-written records in order to improve the quality of documentation.
As a conclusion for clinicians, the importance of careful documentation of peri-transfusional data such as hemoglobin value, bedside test and other irregularities should be highlighted in transfusion educational sessions, in the transfusion committee, in audits and in case workups.
The reported transfusion incidents contained 4 actively reported “near miss” events, ie errors noticed before blood products were administered and 8 more detected by serendipity. Here, regulated and efficiency-controlled staff training using teaching examples can raise awareness that valuable clinical conclusions can be drawn from near misses to improve patient safety.10,22
In summary, the results of the present study show the importance of implementing systematic and standardized data acquisition in the context of hemovigilance systems to further expand the understanding of transfusion reactions and thus increase the safety of patients during hemotherapy. Further studies could shed light on the advantages of this approach in an international comparison or collect data beyond the nominal level in order to make even more differentiated statements about patient groups and the relationship between transfusion and transfusion response.
Data Sharing Statement
The data that support the findings of this study are not publicly available because they contain information that could compromise the privacy of research participants but are available from the corresponding author (R.H.).
Statement of Ethics
The research was reviewed for compliance with the guidelines for human studies in accordance with the Declaration of Helsinki of the World Medical Association. A positive ethical vote was obtained from the Ethics Committee of the Medical Faculty of the University of Leipzig (reference: 499/20-ek). Written informed consent was not required, but anonymity was granted.
Author Contributions
E.N. developed the concept of the study, carried out the data collection, analysed the results, wrote the manuscript and created the figures and tables. She agreed on the journal to which the article was submitted. R.H. developed the concept of the study, helped with the acquisition and interpretation of the data, corrected and reviewed the manuscript critically. He agreed on the journal to which the article was submitted. J.D. initiated the study, developed the study design, helped with the acquisition of data and critically reviewed the manuscript. He agreed on the journal to which the article was submitted. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Supported by the Open Access Publishing Fund of Leipzig University.
Disclosure
The authors have no conflicts of interest to declare for this work.
References
1. Murphy MF, Stanworth SJ, Yazer M. Transfusion practice and safety: current status and possibilities for improvement. Vox Sang. 2011;100:46–59. doi:10.1111/j.1423-0410.2010.01366.x
2. Hatayama Y, Matsumoto S, Hamada E, et al. Analysis of acute transfusion reactions and their occurrence times. Yonago Acta Med. 2018;61:087–090. doi:10.33160/yam.2018.03.013
3. Delaney M, Wendel S, Bercovitz RS, et al. Transfusion reactions: prevention, diagnosis, and treatment. Lancet. 2016;388:2825–2836. doi:10.1016/S0140-6736(15)01313-6
4. Pfuntner A, Wier LM, Stocks C. Most frequent conditions in U.S. hospitals, 2011: statistical brief #162; 2021. Available from: https://europepmc.org/article/NBK/nbk169248#free-full-text.
5. Aubron C, Aries P, Le niger C, et al. How clinicians can minimize transfusion-related adverse events? Transfus Clin Biol. 2018;25:257–261. doi:10.1016/j.tracli.2018.08.158
6. de Vries RRP, Faber JC, Strengers PFW, et al. Haemovigilance: an effective tool for improving transfusion practice. Vox Sang. 2011;100:60–67. doi:10.1111/j.1423-0410.2010.01442.x
7. Land KJ, Whitaker BI, Uhl L. National hemovigilance: the current state. In: Cohn CS, Delaney M, Johnson ST, Katz L, editors. Technical Manual.
8. Politis C, Wiersum JC, Richardson C, et al. The international haemovigilance network database for the surveillance of adverse reactions and events in donors and recipients of blood components: technical issues and results. Vox Sang. 2016;111:409–417. doi:10.1111/vox.12447
9. Nuttall GA, Stubbs JR, Wc O. Transfusion errors: causes, incidence, and strategies for prevention. Curr Opin Anaesthesiol. 2014;27:657–659. doi:10.1097/aco.0000000000000136
10. Narayan S, Poles D; on behalf of the Serious Hazards of Transfusion (SHOT) Steering Group. The 2019 annual SHOT report (2020); 2021. Available from: https://www.shotuk.org/wp-content/uploads/myimages/SHOT-REPORT-2019-Final-Bookmarked-v2.pdf.
11. Maskens C, Downie H, Wendt A, et al. Hospital- based transfusion error tracking from 2005 to 2010: identifying the key errors threatening patient transfusion safety. Transfusion. 2014;54:66–73. doi:10.1111/trf.12240
12. Cohen J. Statistical power analysis for the behavioral sciences, New York/ San Francisco/ London, Academic Press (1977); 2021. Available from: https://books.google.de/books?hl=de&lr=&id=rEe0BQAAQBAJ&oi=fnd&pg=PP1&ots=swWRMsURo5&sig=ezonSWt_I9-_XCEke7o60vbGMzo#v=onepage&q&f=false.
13. Bundesärztekammer. Querschnitts-Leitlinien (BÄK) zur Therapie mit Blutkomponenten und Plasmaderivaten – gesamtnovelle 2020; 2022 Available from: https://www.bundesaerztekammer.de/fileadmin/user_upload/_old-files/downloads/pdf-Ordner/MuE/Querschnitts-Leitlinien_BAEK_zur_Therapie_mit_Blutkomponenten_und_Plasmaderivaten-Gesamtnovelle_2020.pdf.
14. Kotzerke D, Walter Costa M, Voigt J, et al. Novelle QLL 2020 – welche Auswirkungen haben die neu empfohlenen Hämoglobin – transfusionstrigger auf die klinische Versorgung? Transfusionsmedizin. 2022;12(01):26–36. doi:10.1055/a-1669-3918
15. Saha S, Krishna D, Prasath R, et al. Incidence and analysis of 7 years adverse transfusion reaction: a retrospective analysis. Indian J Hematol Blo. 2020;36:149–155. doi:10.1007/s12288-019-01174-x
16. Goel R, Tobian AA, Shaz BH. Noninfectious transfusion-associated adverse events and their mitigation strategies. Blood. 2019;133:1831–1839. doi:10.1182/blood-2018-10-833988
17. Moncharmont P, Barday G, Odent- Malaure H, et al. Adverse transfusion reactions in recipients transfused in out-of-hospital. Transfus Clin Biol. 2018;25:105–108. doi:10.1016/j.tracli.2018.02.003
18. Vossoughi S, Perez G, Whitaker BI, et al. Safety incident reports associated with blood transfusions. Transfusion. 2019;59:2827–2832. doi:10.1111/trf.15429
19. Sousa Neto AL, Barbosa MH. Analysis of immediate transfusion incidents reported in a regional blood bank. Rev Bras Hematol Hemoter. 2011;33:337–341. doi:10.5581/1516-8484.20110095
20. Narayan S, Poles D; on behalf of the Serious Hazards of Transfusion (SHOT) Steering Group. The 2021 annual SHOT report (2022); 2022. Available from: https://www.shotuk.org/wp-content/uploads/myimages/SHOT-REPORT-2021-FINAL-bookmarked-V2-September.pdf.
21. Bundesärztekammer. Richtlinie zur Gewinnung von Blut und Blutbestandteilen und zur Anwendung von Blutprodukten (2017); 2021. Available from: https://www.bundesaerztekammer.de/fileadmin/user_upload/downloads/pdf-Ordner/RL/RiliH_Lese.pdf.
22. Wood EM, Ang AL, Bisht A, et al. International haemovigilance: what have we learned and what do we need to do next? Transfus Med. 2019;29:221–230. doi:10.1111/tme.12582
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.