Back to Journals » Clinical Interventions in Aging » Volume 19
The Association of Intraindividual Difference Between Cystatin- and Creatinine-Based Estimated GFR and Contrast-Associated Acute Kidney Injury
Authors Zhang LW, Luo MQ, Zeng JL, You ZB, Chen LC, Chen JH, Lin KY, Guo YS
Received 28 October 2023
Accepted for publication 27 February 2024
Published 8 March 2024 Volume 2024:19 Pages 411—420
DOI https://doi.org/10.2147/CIA.S447042
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Li-Wei Zhang,1– 3,* Man-Qing Luo,4,* Ji-Lang Zeng,1– 3,* Zhe-Bin You,2,3,5 Li-Chuan Chen,1– 3 Jun-Han Chen,1– 3 Kai-Yang Lin,1– 3 Yan-Song Guo1– 3
1Department of Cardiology, Shengli Clinical Medical College of Fujian Medical University, Fujian Provincial Hospital, Fuzhou, People’s Republic of China; 2Fujian Provincial Key Laboratory of Cardiovascular Disease, Fujian Provincial Center for Geriatrics, Fujian Provincial Clinical Research Center for Severe Acute Cardiovascular Diseases, Fuzhou, People’s Republic of China; 3Fujian Heart Failure Center Alliance, Fuzhou, People’s Republic of China; 4Department of Cardiology, Fuwai Hospital, National Clinical Research Center for Cardiovascular Diseases, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People’s Republic of China; 5Department of Geriatric Medicine, Fujian Key Laboratory of Geriatrics, Fujian Provincial Hospital, Fujian Provincial Center for Geriatrics, Fujian Medical University, Fuzhou, Fujian, 350001, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kai-Yang Lin; Yan-Song Guo, Tel +86-13559355708 ; +86-059188217410, Email [email protected]; [email protected]
Purpose: The estimated glomerular filtration rate (eGFR) based on creatinine is crucial for the risk assessment of contrast-associated acute kidney injury (CA-AKI). In recent, the difference between cystatin C-based eGFR (eGFRcys) and creatinine-based eGFR (eGFRcr) has been widely documented. We aimed to explore whether intraindividual differences between eGFRcys and eGFRcr had potential value for CA-AKI risk assessment in patients undergoing elective percutaneous coronary intervention (PCI).
Patients and Methods: From January 2012 to December 2018, we retrospectively observed 5049 patients receiving elective PCI. To determine eGFR, serum creatinine and cystatin C levels were measured. CA-AKI was defined as serum creatinine being increased ≥ 50% or 0.3 mg/dL within 48 h after contrast agents exposure. Chronic kidney disease (CKD) was defined as the eGFR < 60 mL/min/1.73 m2.
Results: Approximately half of the participants (2479, 49.1%) had a baseline eGFRdiff (eGFRcys-eGFRcr) between − 15 and 15 mL/min/1.73 m2. Restricted cubic splines analysis revealed a nonlinear relationship between eGFRdiff and CA-AKI. Multivariable logistic regression analysis indicated that compared with the reference group (− 15 to 15 mL/min/1.73 m2), the negative-eGFRdiff group (less than − 15 mL/min/1.73 m2) had a higher risk of CA-AKI (OR, 3.44; 95% CI, 2.57– 4.64). Furthermore, patients were divided into four groups based on CKD identified by eGFRcys or eGFRcr. Multivariable logistic analysis revealed that patients with either CKDcys (OR, 2.94; 95% CI, 2.19– 3.95, P < 0.001) or CKDcr (OR, 2.44; 95% CI, 1.19– 4.63, P < 0.001) had an elevated risk of CA-AKI compared to those without CKDcys and CKDcr.
Conclusion: There are frequent intraindividual differences between eGFRcys and eGFRcr, and these differences can be used to forecast the risk of CA-AKI.
Keywords: estimated glomerular filtration rate, contrast-associated acute kidney injury, cystatin C, percutaneous coronary intervention
Introduction
In patients with coronary heart disease, percutaneous coronary intervention (PCI) is one technique for revascularization that restores coronary blood flow. During the procedure, contrast agent is used to make the coronary arteries visible. As one of the major postoperative complications in patients undergoing elective PCI, contrast-associated acute kidney injury (CA-AKI) closely related to dialysis risk,1 an extended hospital stay, increased costs, and even a poor prognosis.2,3 Additionally, the population of individuals at CA-AKI risk is particularly vast due to the substantial burden of coronary heart disease.4 It’s important to find predictors to forecast the CA-AKI occurrences. One of the most well-known risk factors in clinical practice currently is lower creatinine-based eGFR (eGFRcr),5 which is usually adopted in risk-scoring systems for CA-AKI prediction.6 However, it is possible that people with extremes of protein intake, or muscle mass may have creatinine values that do not necessarily reflect the true GFR.7 Therefore, when eGFR is solely assessed by creatinine, the number of patients at risk for CA-AKI may be ambiguous. Nevertheless, eGFRcr remains the most widely utilized indicator in the clinical context due to its low price and availability. In comparison, cystatin C is less sensitive to muscle mass and independent of dietary protein intake.8 Some scholars have proposed cystatin C as a diagnostic and evaluable index of CA-AKI.9 With the increasing clinical application of cystatin C-based eGFR (eGFRcys), it has been extensively noted that there are often differences between eGFRcys and eGFRcr. This difference contains expected information that has been linked to frailty,10 heart failure,11 and poor outcomes.12 One study13 showed that this difference is common in patients with heart failure, is considered a manifestation of frailty, and is associated with a poor short-term prognosis.
In addition to heart failure, cardiovascular specialists are highly worried about renal function in patients undergoing percutaneous coronary intervention (PCI), since it is directly associated with CA-AKI. Additionally, the Chronic kidney disease (CKD) stage determined by eGFR may differ according to the use of various markers, increasing the uncertainty surrounding the risk of CA-AKI. This study aimed to explore the predictive value of intraindividual differences between eGFRcys and eGFRcr for CA-AKI in patients undergoing elective percutaneous coronary intervention (PCI).
Methods
Study Population
This study included all patients who received elective PCI and detected creatinine as well as cystatin C in Fujian Provincial Hospital from 2012 to 2018. The exclusion criteria were as follows: (1). concomitant diseases (thyroid disease, malignant tumors with life expectancy less than 1 year, eGFR less than 15 mL/min/1.73m2 or dialysis (n=30); (2). use of steroid hormones (n=3); (3). died within 72 hours after admission (n=4). Finally, 5049 patients were enrolled in this analysis (Figure 1).
 |
Figure 1 Information on the selection of study participants. |
Percutaneous Coronary Intervention
PCI is performed by experienced interventional cardiologists according to ACC/AHA/SCAI guidelines for coronary artery revascularization. A nonionic and low-osmolarity contrast medium (CM) was administered to all the patients during all procedures (either ultravist or iopamiron, both 370 mgI/mL). Hydration is one of the effective methods to preventing CA-AKI in revascularization guidelines. In addition, intravenous infusion of 0.9% normal saline at a rate of 1 mL/kg/h (or 0.5 mL/kg/h for those who were intolerant) for 12 hours constituted hydration treatment.
Exposure
Serum creatinine (Scr) was detected at baseline and 2 consecutive days after the operation, and cystatin was only detected before the operation by using the COBAS automatic biochemical analyser (Roche Diagnostics, Basel, Switzerland). The eGFRcys and eGFRcr were calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) cystatin C equation (2012)14 and CKD-EPI creatinine equation (2012),15 respectively (Table S1). The eGFRdiff was defined as eGFRcys - eGFRcr, and categorized as < −15 mL/min/1.73 m2 (negative-eGFRdiff group), −15 to 15 mL/min/1.73 m2 (reference group), and ≥ 15 mL/min/1.73 m2 (positive-eGFRdiff group). A difference of 15 mL/min/1.73 m2 in eGFR was chosen to be the cut-point because it is clinically meaningful and capable of distinguishing CKD stages.15 CKDcys and CKDcr were defined as the eGFRcys < 60 mL/min/1.73 m2 and eGFRcr < 60 mL/min/1.73 m2, respectively. This definition has clinical value, and is widely used by many studies.15,16
Outcomes
The primary outcome was CA-AKI which was diagnosed as an absolute SCr increase ≥ 26.4 µmol/L or a relative increase in SCr ≥ 50% within 48 h after CM exposure.
Covariates
All covariate data were obtained, including demographic characteristics, medical history, medical therapy during hospitalization, laboratory measurements, clinical presentation and procedure details. Biochemical tests including blood routine, coagulation function, liver function, kidney function, electrolytes, blood lipid profile, glycated hemoglobin, etc. were obtained on admission or after overnight fasting of 8–12 h.
Statistical Analysis
We summarized baseline characteristics according to three eGFRdiff (mL/min/1.73 m2) groups. Numbers and percentages were shown for categorical variables, while means and standard deviations (normally distributed) or median and interquartile range (nonnormally distributed) were shown for continuous variables. By using the Wilcoxon rank-sum test or Student’s t-test, the difference between the groups was determined.
For the evaluation of the linear or nonlinear association between eGFRdiff and CA-AKI, restricted cubic splines (RCS) were used. Multivariable logistic regression analyses were conducted on the factors that were significant in the univariable analysis (P < 0.05) or were of great clinical significance. Adjusted logistic regression models were constructed in the following ways: Model 1 adjusted for age, sex; Model 2 included adjustments for Model 1 variables as well as smoking and morbidities (hypertension, diabetes, atrial fibrillation, anemia, eGFRcr < 60 mL/min/1.73m2); Model 3 further adjusted for acute myocardial infarction, congestive heart failure and contrast volume > 150mL. A fully adjusted logistic regression model was used for the subgroup and interaction analyses, subgroup ORs and 95% confidence intervals were calculated along with interactions P values. The results were presented in the form of forest plots. Another manifestation of the intraindividual difference between eGFRcys and eGFRcr is the different CKD definitions derived from them. To further evaluate the effects of different CKD definitions on predicting CA-AKI, patients were categorized into four groups according to with or without CKDcys and CKDcr. Statistical analyses were performed by R (version 4.1.2; R Foundation, Vienna, Austria). A value of P < 0.05 (two-tailed) was considered statistically significant.
Results
Baseline Characteristics
Of 5049 eligible patients, 324 (6.42%) patients developed CA-AKI. Approximately half of the participants had eGFRdiff between −15 and 15 mL/min/1.73 m2 (2478, 49.1%). Basic demographic and procedural characteristics were presented in Table 1. Since we choose patients with elective PCI, the great majority of patients had stable hemodynamics and patients requiring intra-aortic balloon pump (IABP) support were very few in our study (only 2 patients). Compared with the other two eGFRdiff groups, participants in the negative-eGFRdiff group were generally older and tended to have higher cystatin C and D-dimer levels while having lower serum creatinine and hemoglobin levels. They presented with a higher rate of acute myocardial infarction incidence, had elevated levels of N-terminal pro-brain natriuretic peptide, and were more frequently treated with diuretics. There were no significant differences in sex, body mass index, hypertension and atrial fibrillation among the three groups. The baseline characteristics of patients with and without CA-AKI were shown in Table S2.
 |
Table 1 Baseline Variables Among Different eGFRdiff Groups (mL/Min/1.73 m2) |
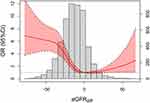
Predictive Value of the eGFRdiff on CA-AKI
RCS in logistic regression analysis revealed a nonlinear relationship between eGFRdiff and CA-AKI risk (P for non-linearity < 0.001, Figure 2). Univariable logistic regression analysis indicated that compared with reference group, negative-eGFRdiff group had a higher risk of CA-AKI (odds ratio [OR], 3.43; 95% CI, 2.66–4.46, Table 2). These differences persisted after adjustment for potential confounding factors (Model 1: OR, 3.35; 95% CI, 2.60–4.36; Model 2: OR, 3.53; 95% CI, 2.67–4.70; Model 3: OR, 3.44; 95% CI, 2.57–4.64). Subgroup analysis showed that none of the different subgroups had any discernible interaction effects (Figure 3). Negative eGFRdiff was associated with an increased CA-AKI risk irrespective of with or without CKDcr (P for interaction = 0.528).
 |
Table 2 Logistic Regression for the Relationship of eGFRdiff and CA-AKI |
 |
Figure 3 Subgroup analysis stratified by CA-AKI risk factors. |
The Effect of Different CKD Definitions on CA-AKI
Multivariable logistic analysis indicated that CKD was an independent risk factor of CA-AKI. Compared to non-CKD patients, patients with either CKDcys (OR, 2.94; 95% CI 2.19–3.95) or CKDcr (OR, 2.44; 95% CI,1.19–4.63) were prone to CA-AKI development (Table 3). Interestingly, the risk of CA-AKI in patients with both CKDcys and CKDcr was similar to those with either CKDcys or CKDcr (CKDcys and CKDcr vs CKDcys and non-CKDcr, OR, 0.999; 95% CI, 0.661–1.491; CKDcys and CKDcr vs non-CKDcys and CKDcr, OR, 1.207; 95% CI, 0.604–2.568).
 |
Table 3 CA-AKI Risk Among Different CKD Groups |
Sensitivity Analysis
The eGFRcr derived from other formulae, such as CKD-EPI (2021) and Modification of Diet in Renal Disease (MDRD), may affect the value of eGFRdiff and the population of CKD. To deeper evaluate the robustness of the results, we conducted a series of sensitivity analyses. Overall, the results obtained from sensitivity analyses were consistent with our main findings and were presented in Tables S3 and S4. Negative-eGFRdiff maintained a strong association with CA-AKI regardless of the use of eGFR equations. After excluding patients with eGFR < 30mL/min/1.73m2 (n=36), the results remained consistent with the main analysis (Table S5).
Discussion
As far as we are aware, this is the first study to investigate the association of intraindividual differences between eGFRcys and eGFRcr and CA-AKI in patients undergoing elective PCI. The main finding of this study was that not only the differences in the absolute value of eGFRcys versus eGFRcr but also the differences in CKD status were associated with the risk of CA-AKI. Despite being a retrospective study conducted at a single institution, our investigation included a large sample size and thorough available factors.
Although creatinine is currently the most commonly used biomarker to estimate GFR, its susceptibility to non-glomerular filtration rate has been concerned. Therefore, cystatin C as an alternative predictor was discussed in previous studies.17 In recent years, the National Kidney Foundation (NKF) and the American Society of Nephrology (ASN) have strongly recommended the promotion of routine and dynamic detection of cystatin C, especially to confirm eGFR in those who are at risk of or with chronic kidney disease.18 Individual differences between eGFRcys and eGFRcr have not received attention for a long time before. At present, it is the mainstream trend to comprehensively evaluate renal function and the risk of kidney disease by using both indicators simultaneously.12,13,19 A close relationship between eGFRdiff and heart failure was observed in previous studies. A Cohort Analysis of Chronic Renal Insufficiency Cohort (CRIC) Study found that patients in the eGFRdiff < −15 group had a 2-fold increased risk of heart failure hospitalization,11 a 1.37-fold increased risk of developing into end-stage Kidney Disease (ESKD), and a 2.73-fold increased risk of death12 compared with patients in the eGFRdiff ≥ 15 group. Besides, eGFRdiff is also closely associated with frailty and poor prognosis. In the Systolic Blood Pressure Intervention Trial (SPRINT), fully adjusted model showed that each unit standard deviation decrease in eGFRdiff was associated with 24% increased odds of prevalent frailty (OR,1.32; 95% CI,1.23–1.41), with a higher incidence rate of injurious falls (HR, 1.19; 95% CI, 1.09–1.30), cardiovascular events (HR, 1.12; 95% CI, 1.03–1.23), and all-cause mortality (HR, 1.41; 95% CI, 1.22–1.59).10 Our research expands the clinical applications of eGFRdiff and highlights its significance in the prediction of CA-AKI.
As a potential substitute for creatinine, cystatin C has been proved to be a biomarker in the prevention20,21 and diagnostic criterion of CA-AKI.9,22,23 Since cystatin C and creatinine were often analysed separately, the roles they played concurrently in CA-AKI have been still unclear. What’s more, the significance of eGFRdiff for CA-AKI is still a blank. This study is the first to observe a relationship between eGFRdiff and CA-AKI. Our study showed that patients with eGFRdiff less than −15 mL/min/1.73 m2 had a more than 3-fold higher risk of CA-AKI than those without, which was proved to be independent of eGFRcr. There are some reasons for this result. Firstly, one of the main contributing factors to the onset of frailty is sarcopenia, which is defined as the loss of skeletal muscle mass and decrease in muscle strength that is directly linked to aging.24 eGFRdiff is associated with sarcopenia and frailty,10,25 which have proved to be the risk factors for CA-AKI.26 Non-GFR factors such as sarcopenia and malnutrition can interfere with the estimation of eGFRcr, resulting in an overestimation of that and a lower eGFRdiff. Negative eGFRdiff may be a bridge between frailty and CA-AKI. Furthermore, negative eGFRdiff may be a novel and particular type of renal dysfunction and result in susceptibility to CA-AKI. Previous studies have shown that a significantly lower eGFRcys than eGFRcr may also be a manifestation of kidney disease,27–29 which is mainly manifested in glomerular filtration dysfunction of medium-sized molecules,27,30 such as cystatin C. And, eGFRdiff is negatively correlated with the severity of this novel kidney disease.31 Moreover, this disease may cause the decline of the resistance and defense of the kidneys32 and lead to a tendency of CA-AKI when hit by the contrast agent.
Besides, patients with either CKDcys or CKDcr were found to be associated with CA-AKI development in this study. Current ACC/AHA/SCAI guidelines only recommended routine hydration in patients with CKD defined by eGFRcr. However, we have found that the differences between eGFRcys and eGFRcr were very common and about 20% of the patients (1031 / 5049) had CKDcys but not CKDcr. These patients may be underestimated in the initial CA-AKI risk assessment and were likely to miss the only prevention measure due to the insufficient clinical use of cystatin C. Therefore, we suggest that it is necessary to detect cystatin C routinely and even evaluate eGFRdiff and CKDcys in patients undergoing PCI to enhance the sensitivity of CA-AKI risk assessment during current clinical practice. Combining other risk factors such as age, gender, diabetes mellitus to promote the precision of risk assessment of CA-AKI.33 The categorization based on eGFRcr and eGFRcys makes it feasible to correctly identify the groups at risk for CA-AKI, and clinicians may then apply more aggressive intervention methods in response, including active hydration, reduced contrast use and active adoption of acute kidney injury care bundles.34
Limitations
There are several limitations in our study. First of all, the design of this study is a single-center, observational study, which has inherent limitations. It is thus necessary to confirm these results in a multicenter, large-scale, international study. The presence of residual confounding cannot be included despite adjusting for potential confounders as far as possible. In addition, GFR was estimated from serum biomarkers and not able to be compared with the real situation.
Conclusion
Our study demonstrated that intraindividual differences between eGFRcys and eGFRcr could provide more predictive utility on the risk stratification of CA-AKI in patients undergoing elective PCI. First, eGFRdiff less than −15 mL/min/1.73 m2 is associated with a higher risk of CA-AKI. Second, both CKD determined by eGFRcys or eGFRcr can markedly predict the occurrence of CA-AKI. Future research is required to investigate the underlying mechanisms of eGFRdiff and to determine whether it is associated with other disorders. It is also necessary to raise public awareness of eGFRdiff.
Abbreviations
PCI, percutaneous coronary intervention; CA-AKI, contrast-associated acute kidney injury; eGFRcr, creatinine-based eGFR; eGFR, estimated glomerular filtration rate; eGFRcys, cystatin C-based eGFR; CM, contrast medium; CKD-EPI, Chronic Kidney Disease Epidemiology Collaboration; MDRD, Modification of Diet in Renal Disease.
Data Sharing Statement
The datasets generated during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
A review and approval of the study were performed by the Fujian Provincial Hospital Ethics Committee (Ethical approval number: K2019-07-011). Our research conformed to the Declaration of Helsinki. Due to the retrospective nature of the study, informed written consent was waived. Personal information and data remained confidential and anonymous.
Author Contributions
LW Z, MQ L and JL Z contributed equally to this work. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by a grant from the National Natural Science Foundation of China General Program (Grant number: 81873495, 82171569), Heart Failure Center Research Foundation of Fujian Provincial Hospital (supported by Fujian Provincial Department of Finance), National Key Clinical Specialty Construction Project of China (Cardiovascular Medicine 2021). The grants played no roles in the design of the study, collection of data, follow-up of the patients, interpretation of data and writing the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mohebi R, Karimi Galougahi K, Garcia JJ, et al. Long-Term Clinical Impact of Contrast-Associated Acute Kidney Injury Following PCI: an ADAPT-DES Substudy. JACC: Cardiovasc Interv. 2022;15(7):753–766. doi:10.1016/j.jcin.2021.11.026
2. Gruberg L, Mintz GS, Mehran R, et al. The prognostic implications of further renal function deterioration within 48 h of interventional coronary procedures in patients with pre-existent chronic renal insufficiency. J Am Coll Cardiol. 2000;36(5):1542–1548. doi:10.1016/S0735-1097(00)00917-7
3. Rihal CS, Textor SC, Grill DE, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105(19):2259–2264. doi:10.1161/01.CIR.0000016043.87291.33
4. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: a Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(2):e21–e129. doi:10.1016/j.jacc.2021.09.006
5. Davenport MS, Perazella MA, Yee J, et al. Use of Intravenous Iodinated Contrast Media in Patients with Kidney Disease: consensus Statements from the American College of Radiology and the National Kidney Foundation. Radiology. 2020;294(3):660–668. doi:10.1148/radiol.2019192094
6. Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44(7):1393–1399. doi:10.1016/j.jacc.2004.06.068
7. Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015;313(8):837–846. doi:10.1001/jama.2015.0602
8. Fan L, Inker LA, Rossert J, et al. Glomerular filtration rate estimation using cystatin C alone or combined with creatinine as a confirmatory test. Nephrol Dial Transplant. 2014;29(6):1195–1203. doi:10.1093/ndt/gft509
9. Droppa M, Desch S, Blase P, et al. Impact of N-acetylcysteine on contrast-induced nephropathy defined by cystatin C in patients with ST-elevation myocardial infarction undergoing primary angioplasty. Clin Res Cardiol. 2011;100(11):1037–1043. doi:10.1007/s00392-011-0338-8
10. Potok OA, Ix JH, Shlipak MG, et al. The Difference Between Cystatin C- and Creatinine-Based Estimated GFR and Associations With Frailty and Adverse Outcomes: a Cohort Analysis of the Systolic Blood Pressure Intervention Trial (SPRINT). Am J Kidney Dis. 2020;76(6):765–774. doi:10.1053/j.ajkd.2020.05.017
11. Chen DC, Shlipak MG, Scherzer R, et al. Association of Intra-individual Differences in Estimated GFR by Creatinine Versus Cystatin C With Incident Heart Failure. Am J Kidney Dis. 2022;80(6):762–772.e1. doi:10.1053/j.ajkd.2022.05.011
12. Chen DC, Shlipak MG, Scherzer R, et al. Association of Intraindividual Difference in Estimated Glomerular Filtration Rate by Creatinine vs Cystatin C and End-stage Kidney Disease and Mortality. JAMA Network Open. 2022;5(2):e2148940. doi:10.1001/jamanetworkopen.2021.48940
13. Pinsino A, Fabbri M, Braghieri L, et al. The difference between cystatin C- and creatinine-based assessment of kidney function in acute heart failure. ESC Heart Fail. 2022;9(5):3139–3148. doi:10.1002/ehf2.13975
14. Inker LA, Schmid CH, Tighiouart H, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367(1):20–29. doi:10.1056/NEJMoa1114248
15. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi:10.7326/0003-4819-150-9-200905050-00006
16. Mehran R, Owen R, Chiarito M, et al. A contemporary simple risk score for prediction of contrast-associated acute kidney injury after percutaneous coronary intervention: derivation and validation from an observational registry. Lancet. 2021;398(10315):1974–1983. doi:10.1016/S0140-6736(21)02326-6
17. Hsu CY, Yang W, Parikh RV, et al. Race, Genetic Ancestry, and Estimating Kidney Function in CKD. N Engl J Med. 2021;385(19):1750–1760. doi:10.1056/NEJMoa2103753
18. Delgado C, Baweja M, Crews DC, et al. A Unifying Approach for GFR Estimation: recommendations of the NKF-ASN Task Force on Reassessing the Inclusion of Race in Diagnosing Kidney Disease. Am J Kidney Dis. 2022;79(2):268–288.e1. doi:10.1053/j.ajkd.2021.08.003
19. Lin YL, Chang IC, Liou HH, et al. Serum indices based on creatinine and cystatin C predict mortality in patients with non-dialysis chronic kidney disease. Sci Rep. 2021;11(1):16863. doi:10.1038/s41598-021-96447-9
20. Duan SB, Liu GL, Yu ZQ, Pan P. Urinary KIM-1, IL-18 and Cys-c as early predictive biomarkers in gadolinium-based contrast-induced nephropathy in the elderly patients. Clin Nephrol. 2013;80(5):349–354. doi:10.5414/CN107829
21. Andreucci M, Faga T, Riccio E, Sabbatini M, Pisani A, Michael A. The potential use of biomarkers in predicting contrast-induced acute kidney injury. Int J Nephrol Renovasc Dis. 2016;9:205–221. doi:10.2147/IJNRD.S105124
22. Ribichini F, Gambaro G, Graziani MS, et al. Comparison of serum creatinine and cystatin C for early diagnosis of contrast-induced nephropathy after coronary angiography and interventions. Clin Chem. 2012;58(2):458–464. doi:10.1373/clinchem.2011.170464
23. Liu YH, Xue JH, Wu DX, et al. A novel simple experimental model for low-osmolar contrast-induced acute kidney injury using different definitions based on the levels of serum creatinine and cystatin C. BMC Nephrol. 2019;20(1):243. doi:10.1186/s12882-019-1436-5
24. Nishiguchi S, Yamada M, Fukutani N, et al. Differential association of frailty with cognitive decline and sarcopenia in community-dwelling older adults. J Am Med Dir Assoc. 2015;16(2):120–124. doi:10.1016/j.jamda.2014.07.010
25. Wang S, Xie L, Xu J, et al. Predictive value of serum creatinine/cystatin C in neurocritically ill patients. Brain Behav. 2019;9(12):e01462. doi:10.1002/brb3.1462
26. Jiesisibieke ZL, Tung TH, Xu QY, et al. Association of acute kidney injury with frailty in elderly population: a systematic review and meta-analysis. Ren Fail. 2019;41(1):1021–1027. doi:10.1080/0886022X.2019.1679644
27. Almén MS, Björk J, Nyman U, et al. Shrunken Pore Syndrome Is Associated With Increased Levels of Atherosclerosis-Promoting Proteins. Kidney Int Rep. 2019;4(1):67–79. doi:10.1016/j.ekir.2018.09.002
28. Grubb A. Shrunken pore syndrome - a common kidney disorder with high mortality. Diagnosis, prevalence, pathophysiology and treatment options. Clin Biochem. 2020;83:12–20. doi:10.1016/j.clinbiochem.2020.06.002
29. Zhang LW, Luo MQ, Xie XW, et al. Shrunken Pore Syndrome: a New and More Powerful Phenotype of Renal Dysfunction Than Chronic Kidney Disease for Predicting Contrast-Associated Acute Kidney Injury. J Am Heart Assoc. 2023;12(1):e027980. doi:10.1161/JAHA.122.027980
30. Xhakollari L, Jujic A, Molvin J, et al. Proteins linked to atherosclerosis and cell proliferation are associated with the shrunken pore syndrome in heart failure patients: shrunken pore syndrome and proteomic associations. Proteomics Clin Appl. 2021;15(4):e2000089. doi:10.1002/prca.202000089
31. Öberg CM, Lindström M, Grubb A, Christensson A. Potential relationship between eGFR(cystatin C) /eGFR(creatinine) -ratio and glomerular basement membrane thickness in diabetic kidney disease. Physiol Rep. 2021;9(13):e14939. doi:10.14814/phy2.14939
32. Wu Z, Wang L, Li Y, Yao Y, Zeng R. Shrunken Pore Syndrome Is Associated with Renal Function Decline in Female Patients with Kidney Diseases. Biomed Res Int. 2022;2022:2177991. doi:10.1155/2022/2177991
33. Frydman S, Freund O, Banai A, Zornitzki L, Banai S, Shacham Y. Relation of Gender to the Occurrence of AKI in STEMI Patients. J Clin Med. 2022;11(21):6565. doi:10.3390/jcm11216565
34. Khoury S, Frydman S, Abu-Katash H, et al. Impact of care bundles on the occurrence and outcomes of acute kidney injury among patients with ST-segment elevation myocardial infarction. J Nephrol. 2023;36(9):2491–2497. doi:10.1007/s40620-023-01652-6
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.