Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
The Effectiveness of Multidisciplinary Team Huddles in Healthcare Hospital-Based Setting
Authors Lin SP, Chang CW, Wu CY , Chin CS , Lin CH, Shiu SI, Chen YW , Yen TH, Chen HC, Lai YH, Hou SC, Wu MJ , Chen HH
Received 2 August 2022
Accepted for publication 23 September 2022
Published 6 October 2022 Volume 2022:15 Pages 2241—2247
DOI https://doi.org/10.2147/JMDH.S384554
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Shih Ping Lin,1– 3 Ching-Wein Chang,4 Chun-Yi Wu,1,5 Chun-Shih Chin,1,6 Cheng-Hsien Lin,1,7 Sz-Iuan Shiu,1,8 Yun-Wen Chen,1,9 Tsai-Hung Yen,1,9 Hui-Chi Chen,4 Yi-Hung Lai,4 Shu-Chin Hou,4 Ming-Ju Wu,3,5 Hsin-Hua Chen1,3,9– 11
1Division of General Medicine, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan; 2Division of Infection, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan; 3Department of Post-Baccalaureate Medicine, College of Medicine, National Chung Hsing University, Taichung, Taiwan; 4Department of Nursing, Taichung Veterans General Hospital, Taichung, Taiwan; 5Division of Nephrology, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan; 6Division of Chest Medicine, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan; 7Division of Hematology and Oncology, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan; 8Gastroenterology and Hepatology, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan; 9Division of Allergy, Immunology and Rheumatology, Department of Internal Medicine, Taichung Veterans General Hospital, Taichung, Taiwan; 10Institute of Biomedical Science and Rong Hsing Research Centre for Translational Medicine, Big Data Center, Chung Hsing University, Taichung, Taiwan; 11School of Medicine, National Yang Ming Chiao Tung University, Taipei, Taiwan
Correspondence: Hsin-Hua Chen, Division of General Medicine, Department of Internal Medicine, Taichung Veterans General Hospital, 1650 Taiwan Boulevard Sect. 4, Taichung, 40705, Taiwan, Email [email protected]
Objective: Huddles are short, regular debriefings that are designed to provide frontline staff and bedside caregivers environments to share problems and identify solutions. Daily huddle implementation could improve medical safety work, problem identification and improvement, situation awareness and teamwork enhancement, the collaboration and communication between professionals and departments, and patient safety. This study aimed evaluated the effectiveness of a hospital-based huddle at a general medical ward in Taiwan.
Methods: A Continuous Integration team was conducted by combining multidisciplinary frontline staff to huddle at a 74-bed general medical ward. Team Huddles started twice a week. A physical huddle run board was created, which contained four parts, including idea submitted, idea approved, working on an idea and standardizing. Problems were submitted to the board to be identified, and the solutions were evaluated through huddle discussion. We divided the problems into two groups: quick hits (resolved within 24– 48hrs) and complex issues (resolved > 48hrs). An anonymous questionnaire was designed to evaluate the huddle response.
Results: A total of 44 huddles occurred from September 9th, 2020, to September 30th, 2021, and 81 issues were identified and resolved. The majority issues were policy documentation (n=23; 28.4%). Sixty-seven (82.7%) issues were defined as quick hits, and the other fourteen (17.3%) issues were complex. The mean hours to the resolution of quick hits was 5.17 hours, median 3.5 hours, and range from 0.01– 15.4 hours. The mean days to resolve completion issues were 19.73 days, median 7.5 days, and range 3.57– 26.14 days. An overwhelming 92.9% of staff responded that huddles help to expedite the process to reach treatment goals, reduce clinical mistakes, near misses, reduce patient incidences, and help teamwork enhancement, with rating of 4.52 (on a 5-point Likert scale).
Conclusion: Implementing of multidisciplinary team huddle improved the accountability of issue identification, problem-solving and teamwork enhancement.
Keywords: huddle run, safety culture, teamwork, patient safety
Introduction
To increase the quality of healthcare for hospitalized patients in a ward, it is crucial to identify issues regarding patient safety with subsequent problem-solving through multidisciplinary teamwork. Huddles are short, regular debriefings that are designed to provide frontline staff and bedside caregivers environments to share problems and identify solutions.1 Through these daily quick meetings, team members can stay informed, review events, and make and share plans for ensuring well-coordinated patient care. The institute for health care improvement recommends using huddles as part of a quality management system.2
Observational studies showed that daily huddle implementation could improve medical safety work,3 problem identification and improvement,4 situation awareness and teamwork enhancement,5 the collaboration and communication between professionals and departments,6,7 and patient safety and organizational quality improvement.8 Two controlled prospective studies showed that high fidelity huddles, which were identified as high frequency huddle runs (≥75% working days) and monthly reporting ≥ median issues, reduce the excess length of patient’s stay,9 and reduce alarm rates of individual patients.10 The implementation of hospital-based huddles or safety briefings can improve patient safety, not only through the process of constructive intervention, but also as a result of continuous improvement and safety culture.11
The Taiwan Patient-Safety Reporting (TPR) System was introduced by the Joint Commission of Taiwan in 2003 to enhance patient safety and promote reporting. This reporting system has 13 different event categories in this reporting system, including falls, medication errors, violence/suicide, tubing-related incidents, security, accident, surgery-related incidents, anesthesia-related incidents, blood transfusion-associated incidents, unexpected cardiac arrest, medical practice-related, laboratory-related incidents, and others. Promoting TPR can detect errors, analyze the nature and cause of errors, and establish a mechanism to prevent the mistakes from occurring and repeatedly occurring in different organizations and individuals. In addition, since 2004, the Joint Commission of Taiwan has set annual patient safety goals for healthcare organizations to improve the quality of patient care. Primary goals were medication safety, infection control in hospitals, mistake prevention in surgery, effective communication among healthcare workers, and the encouragement of reporting medical errors, adverse events, sentinel events, etc.
Evidence of for daily huddle implementation in patient safety and medical care quality remains sparse in Taiwan. Furthermore, to our knowledge, multidisciplinary team huddles interventions have never been tested in enhancing teamwork and communication in Taiwan. In this study, we conducted a hospital-based huddle at a general medical ward in Taiwan to evaluate the effectiveness as measuring by time to resolution of problems and staff huddle response survey.
Methods
Establish a Team Huddle Routine
In sport, a huddle is the action of a team gathering together and to strategize before each play. For health care implementation, a huddle is a short, stand-up meeting — 10 minutes or less — that is typically used once at the start of each workday in a clinical setting. To transform the leadership and frontline staff relationship, we created time and space for meaningful conversations to enhance relationships and strengthen safety culture. We conducted a CI team to huddle at a 74-bed general medical ward at Taichung Veterans General Hospital, which was a 1500-bed medical centre in central Taiwan. The team members included 7 clinical physicians, 9 resident doctors, 63 nurses, 2 medical assistants, 2 front desk personnel, and one hospital cleaning staff. Team Huddles started twice a week (every Wednesday and Friday) in the ward conference room on September 9th, 2020. The meeting began at 8:08 am, lasting around 15–20 minutes before morning clinic hours. We always started and ended the team huddles on time to ensure reliability and consistency.
Develop Relationships and Identify Roles
The ward director was the huddle leader initially, and then we rotated the leader to different physicians in the general ward to make everyone feel more involved. The meeting followed a standardized process so that various people could run it. Every staff member could submit an issue to the idea card. The primary responsibility of the huddle leader was to control the meeting time, direct the conversation according to the submitted issues, make short and quick communication cycles up to and down the chain, and make the final conclusion. The medical assistants helped to record the decision-making of every issue or project and followed up on the unsolved problems. The role of the head nurse was to ensure the team members’ awareness and the processing of medical care issues. The chief resident used very consistent messaging of continuous improvement and a safety culture for the orientation of new residents monthly. All team members would review any items requiring action from the previous day and capture action items for solving problems.
Huddle Run Board
We created a physical huddle run board, which was posted in the ward conference room, to allow every project team member to see, know, and act as a group. The board contained four parts: idea submitted, idea approved, working on a picture and standardizing. In addition, we created an idea card as a sticky note to post on the huddle board. The purpose of the idea card was to record the problem. Every team member could write down what the target condition is? What is the actual situation now? And the why to improve. Issues were submitted to the board to be identified, and the solutions were evaluated through huddle discussion.
Identification of Problems
We divided the problems into two groups: quick hits and complex issues.12 Quick Hits are issues anticipated to be resolved within a short period (24–48hrs) and do not require large amounts of problem analysis or project management. The examples of quick hits are issues of communications between doctors and nurses, the setting of medical order bundles for joint fluid and cerebrospinal fluid studies. Complex Issues are identified problems that often will take a more extended time and would benefit from a higher level of project management. Complex Issues usually contain equipment/safe environment problems, changes in information technology systems, and clinical care pathways. Time to resolution of problems was defined as the first time of issue discussion to the time of problems resolved. For example, the setting down of medical orders bundles and the completeization of information technology systems were denied as problems resolved.
Questionnaire for Huddle Response Survey
A published questionnaire, which was designed to evaluate the improvement of the quality of team care after the intervention of medical team resource management (TRM), was used in our study.13 Total of 10 questions were designed and the Likert five-point scale was adopted. Higher scores indicate more positive teamwork satisfaction. The overall scale content validity was 95.3%. Internal consistency Cronbach’s test was 90. This survey was an electronic structured questionnaire and was done one year after the huddle began. The questionnaire was distributed via email to all team members of the huddle. Survey responses were categorized as positive or negative with respect to the huddles. The Ethics Committee of Taichung Veterans General Hospital approved this study.
Results
Issues Category
A total of 44 huddles occurred from September 9th, 2020, to September 30th, 2021. Huddle runs were held from May 8th to August 10th 2021, because of the pandemic of coronavirus disease 2019 (COVID-19) in Taiwan. Among each huddle, 7 fixed physicians, one chief resident, 8 resident doctors, 2 medical assistants, and 5–10 nurses participated in huddle discussion. For other team members, they would attend huddles if they submit an issue to the idea card. The attendance rate was around 30%. Eighty-one issues were identified and resolved, among them 46 (57%) issues were identified by clinical doctors, 33 (41%) by nurses and medical assistants, and 2 (2%) by front desk personnel, and hospital cleaning staff. The category and percentage were summarized in Table 1. The majority issues were policy documentation (n=23; 28.4%), followed by drug safety (n=18; 22.2%), communication (n=9, 11.1%), information technology systems (n=9, 11.1%), equipment/safe environment (n=9, 11.1%), clinical care pathway (n=8, 9.9%), and others issues (n=5, 6.2%). Issue example for policy documentation was we orientated the risk priority for inter-hospital transport for critical patients. Example for drug safety was the antibiotic administration time for hemodialysis patients. For communication issues, we orientated the blood draw time to avoid multiple blood draws for a patient and strengthen the importance of double-check between doctor and nurse for emergency blood draw.
 |
Table 1 Issues Category and Percentage |
Time to Resolution of Problems
Among 81 issues, 67 (82.7%) issues were defined as quick hits, and the other 14 (17.3%) issues were complex. The mean days to resolve all problems was 3.59 days, the median 0.24 days and range from 0–90 days. The mean hours to the resolution of quick hits was 5.17 hours, the median 3.5 hours, and the range from 0.01–15.4 hours. The mean days to resolve completion issues were 19.73 days, a median of 7.5 days, and a range of 3.57–26.14 days. The details of the processing time are shown in Table 2. Problems about equipment/safe environment took the longest time for resolution, with a mean of 47.33 days and a median of 45 days.
 |
Table 2 Huddle Run Classification Number and Processing Time Analysis |
Huddle Response Survey
Table 3 shows the huddle responses survey using the Likert scale. Table 4 shows huddle responses survey categorized by different huddle team members. A total of 85 huddle team members completed the anonymous questionnaire for the huddle response survey. Team members included 17 (20.0%) clinical physicians and residents, 65 (76.5%) nurses and medical assistants, and 3 (3.5%) front desk personnel and hospital cleaning staff. After one year of huddles implantation, the average rating of all survey items was 4.49 (on a 5-point Likert scale). An overwhelming 92.9% of staff responded that huddles help expedite the process to reach treatment goals, reduce clinical mistakes and near misses, reduce patient incidences, and help enhance teamwork, with a rating of 4.52.
 |
Table 3 Huddle Responses Survey Using Likert Scale |
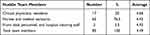 |
Table 4 Huddle Responses Survey Categorized by Different Huddle Team Members |
Discussion
In this prospective study, we implemented a multidisciplinary team huddle at a general medical ward. We noticed that after the intervention, 81 issues were identified and resolved. The major issues were policy documentation (28.4%). Quick hits accounted for 82.7% of issues. Problems about equipment/safe environment took the longest time for resolution. Team huddles also brought closer relationships between physician leaders and hospital-side managers. Implementing multidisciplinary team huddles improved the accountability of issue identification, problem-solving and teamwork enhancement.
In health care, team huddles have been used to increase patient safety and facilitate problem identification and solving efficiency.4,14 Through team huddles, clinical mistakes or near misses were discussed. The team was encouraged to become engaged and involved in developing solutions. Donnelly et al reported that a daily readiness huddle is a framework to identify issues and foster problem-solving rapidly. Huddles brought both visibility and accountability to the process of project completion.4 Burr et al also demonstrated that the implementation of huddles in a respiratory care department allowed the identification of process improvement opportunities, with 88% of opportunities resolved within one week.15 An observational study of addressing weekly physicians’ safety huddles at a rehabilitation hospital showed an average of 3.3 ±1.8 actions were taken in response per huddle to improve patient safety.8 Similar to the previous study, after the intervention of scheduled multidisciplinary team huddles at our general medical ward, a total of 81 issues were identified and resolved. The mean days for problems resolving in our study was 3.59 days. Huddles allow problem-solving transparency and direct and practical communication with department associates. In addition, huddles enable groups to plan for contingencies, express concerns, address conflicts, and reassign resources. As a result, discipline-based problems are quickly resolved.
Most of our staff responded positively to our study’s huddle response survey. An overwhelming 92.9% of our team responded that huddles help to expedite the process to reach treatment goals, reduce clinical mistakes and near misses, reduce patient incidences, and help enhance teamwork. In addition, many studies demonstrated the improvement of safety culture after the implantation of huddles. For example, Pannick et al conducted a non-randomized controlled trial at two hospitals in the UK. The teamwork and safety scores were significantly higher after daily huddles intervention.9 Interprofessional huddles could also improve effective communication in a multidisciplinary team,16 and make their work more efficient.17 A cluster-randomized trial also demonstrated that leadership training for facilitating daily huddles, team coordination, credibility, team learning, and knowledge creation all improved compared with less engaged teams.18 In the review article, huddles implementation leads to quality information sharing, increased levels of accountability, empowerment, and a sense of community.1,19–21 Altogether, create a culture of collaboration and collegiality that improves the staff’s quality of collective awareness and enhanced capacity for eliminating patient harm.
There are limitations in our studies, and caution is needed in the interpretation of our findings. First of all, this study was a retrospective study. We did not compare the huddle response before and after the intervention. We further controlled pre-post study designed research is needed. Second, the attendance rate was around 30%. Not all staff attend the huddles, because some doctors and nurses were not on duty at huddles time. We provided idea cards for issue submission to provide voice opportunities for those not attending. Doctors and nurses’ voices were mostly heard in the huddles. Third, there were positively bias in our huddle response survey, because we comparing it to no huddles. Some downsides may be missed from our huddles survey. The patient satisfaction surveys from discharged patients were improved after huddle intervention, especially in terms of “Ward environment equipment”, “Health care givers are more willing to discuss with me about my condition”. Finally, we conducted a non-daily but twice-A-week huddle. However, most huddles were conducted daily and focused on the clinical process and patient outcome. Our study created a brief discussion following a standard agenda targeted at specific safety objects. The majority of issues were policy documentation and drug safety, and an overwhelming number of staff had positively responded at huddles. Our study concluded that implementing a non-daily huddle can also get positive results in safety culture. Our study encouraged starting a huddle run, especially in a hospital ward setting, which could begin from twice a week to a daily huddle run.
While the positive benefits of huddles in hospital settings were discussed in many studies, high quality pre and post intervention comparison studies were still rare. Most studies were uncontrolled pre–post studies, substantially descriptive in nature, and implemented in a single unit. Multi-factors are associated with patient safety outcomes. Further rigorous research, especially focusing on one specific category issue, more clarify outcome definitions are warranted to analyze the benefit of huddles.
In conclusion, our study was a pilot study of huddles run in a hospital-based setting in Taiwan. Implementing a multidisciplinary team huddle improved the accountability of issue identification, problem-solving and teamwork enhancement.
Acknowledgments
The authors would like to thank for team members participating in this study in Taichung Veterans General hospital.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Goldenhar LM, Brady PW, Sutcliffe KM, Muething SE. Huddling for high reliability and situation awareness. BMJ Qual Saf. 2013;22(11):899–906. doi:10.1136/bmjqs-2012-001467
2. Institute for Healthcare Improvement. Tools: Huddles. Available from: ihi.org/resources/Pages/Tools/Huddles.aspx.
3. Ore S, Rosvold EO, Helleso R. Lessons learned from introducing huddle boards to involve nursing staff in targeted observation and reporting of medication effect in a nursing home. J Multidiscip Healthc. 2019;12:43–50. doi:10.2147/JMDH.S182872
4. Donnelly LF, Cherian SS, Chua KB, et al. The daily readiness huddle: a process to rapidly identify issues and foster improvement through problem-solving accountability. Pediatr Radiol. 2017;47(1):22–30. doi:10.1007/s00247-016-3712-x
5. Chapman LR, Molloy L, Wright F, et al. Implementation of situational awareness in the pediatric oncology setting. does a “huddle” work and is it sustainable? J Pediatr Nurs. 2020;50:75–80. doi:10.1016/j.pedn.2019.10.016
6. McBeth CL, Durbin-Johnson B, Siegel EO. Interprofessional huddle: one children’s hospital’s approach to improving patient flow. Pediatr Nurs. 2017;43(2):71–76.
7. Zhu J, Stadeli KM, Pandit K, et al. Standardizing nightly huddles with surgical residents and nurses to improve interdisciplinary communication and teamwork. Am J Surg. 2020;219(5):769–775. doi:10.1016/j.amjsurg.2020.03.002
8. Guo M, Tardif G, Bayley M. Medical safety huddles in rehabilitation: a novel patient safety strategy. Arch Phys Med Rehabil. 2018;99(6):1217–1219. doi:10.1016/j.apmr.2017.09.113
9. Pannick S, Athanasiou T, Long SJ, Beveridge I, Sevdalis N. Translating staff experience into organisational improvement: the HEADS-UP stepped wedge, cluster controlled, non-randomised trial. BMJ Open. 2017;7(7):e014333. doi:10.1136/bmjopen-2016-014333
10. Bonafide CP, Localio AR, Sternler S, et al. Safety huddle intervention for reducing physiologic monitor alarms: a hybrid effectiveness-implementation cluster randomized trial. J Hosp Med. 2018;13(9):609–615. doi:10.12788/jhm.2956
11. Ryan S, Ward M, Vaughan D, et al. Do safety briefings improve patient safety in the acute hospital setting? A systematic review. J Adv Nurs. 2019;75(10):2085–2098. doi:10.1111/jan.13984
12. LP D. The daily readiness huddle – a key component to a system of care. Health Syst Policy Res. 2016;3:1.
13. Available from: https://tpl.ncl.edu.tw/NclService/JournalContentDetail?SysId=A20016530.
14. Hills L. The art of the morning huddle: how to use this simple tool to build your team. J Med Pract Manage. 2016;32(3):202–206.
15. Burr KL, Stump AA, Bladen RC, et al. Twice-daily huddles improves collaborative problem solving in the respiratory care department. Respir Care. 2021;66(5):822–828. doi:10.4187/respcare.07717
16. Newman RE, Bingler MA, Bauer PN, Lee BR, Mann KJ. Rates of ICU transfers after a scheduled night-shift interprofessional huddle. Hosp Pediatr. 2016;6(4):234–242. doi:10.1542/hpeds.2015-0173
17. Tielbur BR, Rice Cella DE, Currie A, et al. Discharge huddle outfitted with mobile technology improves efficiency of transitioning stroke patients into follow-up care. Am J Med Qual. 2015;30(1):36–44. doi:10.1177/1062860613510964
18. Lampman MA, Chandrasekaran A, Branda ME, et al. Optimizing huddle engagement through leadership and problem solving within primary care: results from a cluster-randomized trial. J Gen Intern Med. 2021;36(8):2292–2299. doi:10.1007/s11606-020-06487-6
19. Stapley E, Sharples E, Lachman P, Lakhanpaul M, Wolpert M, Deighton J. Factors to consider in the introduction of huddles on clinical wards: perceptions of staff on the SAFE programme. Int J Qual Health Care. 2018;30(1):44–49. doi:10.1093/intqhc/mzx162
20. Franklin BJ, Gandhi TK, Bates DW, et al. Impact of multidisciplinary team huddles on patient safety: a systematic review and proposed taxonomy. BMJ Qual Saf. 2020;29(10):1–2. doi:10.1136/bmjqs-2019-009911
21. Pimentel CB, Snow AL, Carnes SL, et al. Huddles and their effectiveness at the frontlines of clinical care: a scoping review. J Gen Intern Med. 2021;36(9):2772–2783. doi:10.1007/s11606-021-06632-9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
