Back to Journals » Research and Reports in Urology » Volume 16
The Outcome of the Miniaturized Percutaneous Nephrolithotomy in Lateral Position with Guidance of Non-Rotational C-Arm
Authors Pham NH, Hoang VT , Bui CLK , Nguyen VQA , Truong VC , Hampton LJ
Received 3 October 2023
Accepted for publication 20 January 2024
Published 22 February 2024 Volume 2024:16 Pages 45—56
DOI https://doi.org/10.2147/RRU.S442145
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Guglielmo Mantica
Ngoc Hung Pham,1 Vuong Thang Hoang,1 Cong Le Kha Bui,1 Van Quoc Anh Nguyen,1 Van Can Truong,1 Lance J Hampton2
1Department of Urology, Hue Central Hospital, Hue, Vietnam; 2Division of Urology, Massey Cancer Center, VCU Health, Richmond, VA, USA
Correspondence: Ngoc Hung Pham, Department of Urology, Hue Central Hospital, 16 Le Loi street, Vinh Ninh ward, Hue City, Thua Thien Hue Province, Vietnam, Email [email protected]
Objective: Evaluation of the outcome of the miniaturized percutaneous nephrolithotomy in the treatment of nephrolithiasis with a lateral position based on the principle of a right triangle under the guidance of a C-Arm without contrast fluid.
Materials and Methods: Sixty-nine cases of Mini-PCNL with the assistance of a vacuum-assisted sheath in the lateral position were performed at Central Hospital from March 2021 to August 2022. Percutaneous renal access was under the guidance of a non-rotational C-arm without contrast medium, and we determined the puncture location and depth of the needle based on the principle of right triangles.
Results: The median age was 51.6 ± 12.5 years, and males accounted for 68.1% of the cases. 60.9% of all patients had normal weight. The median stone surface area was 361.1mm2, and 59.4% of all cases were graded as 2 regarding Guy’s stone score. The successful renal access rate was 100%. The tunnel access from the middle and lower calyx accounted for 94.2%. The median access duration, fluoroscopy duration, and hospital length of stay were 271.7 seconds, 14.79 seconds, and 6.3 days, respectively. The complete stone clearance rate was 78.3%. Bleeding complications occurred in 2 patients without mortality. Three patients required an additional procedure.
Conclusion: The puncture technique into the renal calyxes based on the principle of the right triangle under the guidance of a non-rotational C-Arm without contrast medium in PCNL is a fast, exact, and safe technique.
Keywords: MiniPCNL, percutaneous renal access, non-rotational C-arm, flank position, vacuum-assisted sheath
Introduction
Percutaneous nephrolithotomy (PCNL) was first invented in 1976, and since then, it has been widely accepted as a safe and highly efficient minimally invasive technique for the treatment of nephrolithiasis.1 PCNL has even been highly recommended by international guidelines, such as the European Association of Urology, as the first-line treatment for nephrolithiasis larger than 20mm in size.2 Initially, the conventional patient position for PCNL was prone. However, there is increasing research evidence to suggest that the prone position is not suitable for the majority of patients, especially those who are obese or have compromised respiratory and cardiovascular function. To ameliorate this limitation, diverse patient positioning methods for PCNL, such as the supine, supine-oblique, and flank positions, have been employed, yielding variable outcomes.3 Since its first use in 1994 by Kerbl et al, the lateral position has become a common posture.4 This position is often utilized in open or laparoscopic renal surgery, so urologists are familiar with it. Moreover, within the elevation of the waist is achieved through the use of a waist bridge, extended flank workspace will be completely exposed and the position of kidney will be lower than 12th rib. This not only mitigates the inherent risks associated with general anesthesia but also facilitates the manipulation of creating an access tract and surgical steps during operation without resistance of iliac crest and ribs.
However, it is a relatively complex technique, with reported complication rates ranging from 2% to 17.1%.5 Among these complications, bleeding is the most significant and can occur during or after the procedure. One of the direct factors affecting bleeding complications and the risk of transfusion in percutaneous nephrolithotomy is the size of the access tract.6 Moving through the kidney calyces with standard manipulation channels to access stones can be difficult and may cause rupture and bleeding of the renal calyces.7 In recent years, with the continual development of technology and the improvement in urologists’ skills, there has been an increase in the utilization of smaller sheaths for PCNL, from Standard-PCNL to Mini-PCNL. Keeping up with this trend, Mini-PCNL has become more and more popular in Vietnam. Creating a tunnel through the skin is the most important step in the surgical process, and if done properly, it can achieve optimal results with a low complication rate.
The advantage of ultrasound-guided puncture is that there is less exposure to radiation and the ability to identify neighboring organs. However, ultrasound depends on the surgeon and is limited in delineating small details of renal anatomy, especially in cases where the renal calyces system is not dilated or in obese patients. On the other hand, C-arm-guided puncture can show the shape of the stone and the direction of the stone from the renal pelvis to the renal calyces, allowing the appropriate puncture position to be chosen for accessing and removing the stone. Moreover, in the process of locating and removing stones that are located in other groups of calyces or stones that move after fragmentation, the C-arm helps to locate the position of the stone.8 Therefore, C-arm guidance is used more widely by surgeons than ultrasound. Even when using ultrasound-guided puncture, many authors still combine it with C-arm during the surgical process.
Although there have been many improvements in the C-arm-guided puncture technique, it is still a difficult technique to perform, partly because it is difficult to imagine the three-dimensional spatial image of the renal calyces system on a two-dimensional fluoroscopic image like the Bull’s eye and triangulation technique. Therefore, we conducted this study to introduce a new method, which helps urologists approach kidney stones more easily based on the right triangle theorem.
Material and Methods
This retrospective study included 69 patients with primary and recurrent kidney stones of 1–3 cm in size, from March 2021 to August 2022 at Hue Central Hospital, Vietnam. Here, the cases of recurrent nephrolithiasis were reported following previous treatment with extracorporeal shock wave lithotripsy (ESWL), endoscopic nephrolithotripsy, open or previous PCNL procedures. We excluded those suffered specific conditions including pregnancy, severe urinary tract infections, uncontrolled diabetes, bleeding disorders, abdominal aortic aneurysm, renal artery stenosis/ aneurysm, ureteral structures, ureteropelvic junction obstructions, congenital anomalies of kidney and urinary tract. This study was examined and approved by the Research Ethics Committee of Hue Central Hospital and informed consent was obtained from the patients. In our research involving human participants, we adhered to the ethical guidelines outlined in the 1964 Helsinki Declaration, as well as the ethical standards set by the national research association during procedural stages.
The procedure was performed under general anesthesia and experienced 2 stages:
Stage 1: The patient was placed in the supine decubitus position. An ureteral catheter was placed upstream from the bladder to the kidney to evaluate the urinary deformity, the circulation of urine in ureter, the position and shape of the kidney stone and the morphology of the renal calyx. After that, a Double-J stent was placed simultaneously with ureteral catheter (Figure 1). If there was a condition of ureter stricture, we would have placed antegrade Double-J stent during or accomplishing lithotomy process. Afterwards, the urethral Foley catheter was inserted and fixed with the ureteral catheter. The patient was changed to lateral position. Both surgeons and surgical assistants stand on the side of the targeting kidney, while the screen of the endoscope, C-arm machine were placed on opposite site (Figure 2).
 |
Figure 1 The Double-J stent (White) was placed simultaneously with ureteral catheter (Blue). |
 |
Figure 2 The patient was in lateral position. |
Stage 2: “Bull’s eye” and “triangulation” method have been used commonly with favourable assistance of C-arm machine to determine the site of skin puncture and the angle of puncture. In this study, however, we introduce a new technique to create optimal puncture with the non-rotational C-arm machine thank to the principle of right triangle. The technique is described below (Figure 3).
- Determination of Needle Entry Point: (Point A coincides with Point B). Identify Point A by projecting the position of the renal stone on the C-arm and cross-referencing it with CT scan images or by injecting contrast agent into the renal pelvis to locate Point A (Point A represents an empty space within the renal pelvis).
- Determination of Puncture Direction: From the renal pelvis into the renal calyx, typically at an angle of approximately 50–60 degrees to facilitate the procedure. Identification of Puncture Landmarks:
- Point A: Based on the C-arm when positioned perpendicular to the operational plane.
- Measure the length of AB on the CT film (Figure 4).
- Determine Point C based on the length of AB and the angle C of the right-angled triangle ABC. Similarly, calculate the length of CA.
After determining the puncture points, angles, and lengths, we proceed to determine the length of the needle and puncture into the renal pelvis. Determination of the successful procedure by injecting normal saline into the ureteral catheter flowing out through the needle tip. After confirming that the needle has been inserted into the renal pelvis, we insert the guide wire (preferably by guiding the wire down the ureter or passing it through another group of calyces to prevent it from slipping out). Renal tunnel dilation started from 8 Fr to 18 Fr diameter using a single-step dilator. The process of tunneling is controlled by the C-arm to determine the direction and depth of the tunneling needle and insertion of an 18 Fr vacuum-assisted sheath (Figure 5).
 |
Figure 4 The way to determine (A, B and C) on CTScan based on the principle of right triangles. |
 |
Figure 5 The vacuum-assisted sheath. |
 |
Figure 6 The continuous renal irrigation pump system. |
We collected the data related to demographic information such as age, gender, body mass index (BMI), underlying health conditions, submission date, surgical procedure, and discharge details were recorded. Prior to the surgery, pre-operative investigations were conducted, including a complete blood count, serum creatinine and blood urea levels, and coagulation profile evaluation. The size, location, and number of stones were determined through computed tomography (CT) scans and kidney, ureter, and bladder (KUB) X-rays. During the surgery, assessments were made regarding stone clearance, operation duration, puncture techniques guided by fluoroscopy, lithotripter and puncture site, complications, usage of nephrostomy, and placement of Double J stent. Post-operative evaluations included hospitalization duration, complications, decrease in hemoglobin levels, and secondary procedures for residual fragments. Post-operative complications were monitored for a period of 30 days. In the post-operative follow-up, patients were assessed for stone clearance using KUB X-rays, and stents were removed if they had been deployed. Patients are considered stone-free when the KUB X-rays are completely clear of stones or there are still stone fragments ≤ 4mm. Statistical analysis: Data analysis was performed using IBM SPSS version 26.0 Software (IBM, Armonk, NY, USA).
Results
Median age was 51.6 ± 12.5 years and the rate of males is almost 68%. Most had normal weight with 42 cases (69%), 23 (33.3%) overweight patients and no one was obese. There were 48 cases (69.6%) without a history of previous kidney surgery, while 21 patients (30.4%) had undergone previous interventions, of which open surgery was the most common, accounting for 23.2% (16/69 cases). One patient may have multiple symptoms, with pain in flank and back being the most common in the majority of patients, accounting for 56.5%. Most cases were renal pelvis calyx stones (47.8%). 50/69 cases (72.5%) had stones in two or more stones, while 19 cases (27.5%) had a single stone. Median stone surface area was 446.9 ± 328.7 mm2. Most of the patients were graded as 2 regarding the Guy’s stone score (59.4%) while grade 3 accounted for 17.4%. Forty-one patients (59.4%) had hydronephrosis while the rest of patients had no hydronephrosis. 62/69 cases (89.9%) had normal serum creatinine levels, while 7 cases (10.1%) had elevated levels. Thirty-eight cases (55.1%) had positive urinary leukocyte and 9 cases (13.0%) had positive nitrite. Five patients had positive urine cultures, with E. coli being the most common pathogen in 60.0% of these cases (Table 1).
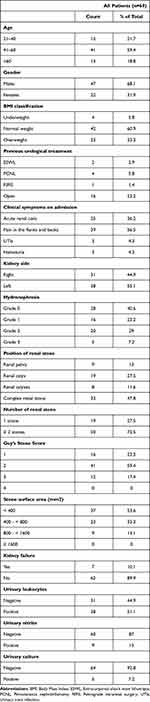 |
Table 1 Demographic and Clinical Characteristics |
Table 2 demonstrates the intraoperative characteristics. Sixty of patients were performed with only one puncture into the renal pelvis, seven patients underwent 2-times punctures (10.1%) and two those with 3-times punctures (2.9%). The upper, middle, and lower calyx were the sites of puncture access in 4 (5.8%), 42 (60.9%), and 23 (33.3%) cases, respectively. Intraoperative parameters were recorded that percutaneous puncture duration was 271.70±433.11 seconds, dilation time was 3.18±2.91 minutes, fluoroscopy duration time was 14.79±24.32 seconds and total operative duration was 143.26±33.94 minutes. The average length of hospital stay after surgery is 6.30 days. The shortest treatment time is 2 days, and the longest is 22 days. The average duration of nephrostomy after surgery is 2.39 days, with 71.0% of cases removed catheter for 1–2 days, the shortest being 1 day and the longest being 8 days.
 |
Table 2 Intraoperative Characteristics |
Out of 69 patients, 44 (63.8%) had no residual stones after surgery, while the remaining 25 (36.2%) had no residual stones ≥ 4mm, which had no clinical significance. The average number of red blood cells and hemoglobin decreased significantly after surgery (p<0.05). 7/69 patients experienced fever during the postoperative period, accounting for 10.1%. There were 3 cases of bleeding that required blood transfusion during the postoperative period (Table 3).
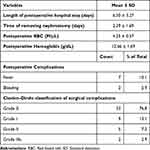 |
Table 3 Postoperative Characteristics |
At the one-month follow-up examination after surgery, 3 patients had symptoms of flank pain, accounting for 4.3%. One patient reported hematuria and one patient reported dysuria. The stone-free rate at the one-month follow-up examination was 78.3%. All cases were examined by ultrasonography, and hydronephrosis with a Grade 1 on ultrasonography was found in almost all cases, accounting for 96.5% (Table 4).
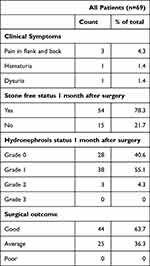 |
Table 4 Follow-Up Characteristics |
Discussion
PCNL is the preferred treatment for large renal stones and is commonly used in clinical treatments.2 Despite technological advancements, complications still occured. To improve safety and effectiveness, Mini-PCNL technology was developed, allowing for the use of smaller sheaths.5 There is no major distinction between PCNL procedures guided by fluoroscopy and those guided by ultrasound. The decision to use either method is typically based on the surgeon’s familiarity with a specific technique and the characteristics of the patient and their kidney stone. Both approaches are equally reliable and secure in the hands of an experienced practitioner. It is essential to note that the use of one technique does not preclude the use of the other, and they can sometimes be utilized in conjunction with each other,9 but currently C-arm is the most widely used method. The “Bull’s Eye” technique and the “triangulation” technique are two classic techniques described. Both techniques require the C-arm to rotate. In 2007, Mues presented a non-rotational C-arm puncture technique, which describes how to puncture the lower, upper, and middle calyxes.10 When using rotational C-arm techniques, through clinical practice, we found that it requires a longer exposure time and multiple rotations, making the surgery more complex. Mues’s non-rotational C-arm puncture technique can be applied, but contrast agents are needed to locate the calyces. The use of contrast agents is performed under C-arm guidance during puncture. The advantage of using contrast agents is that the calyces can be identified easily, but in difficult cases where multiple punctures are required, the risk of contrast agents spilling out is high, which can blur the surgical field and make it more difficult to locate the position of the calyces and stones. According to the classic technique, the direction to puncture the kidney is 20–30 degrees from the back, and puncturing the lower pole of the posterior surface of the kidney makes it easy to reach the renal pelvis or even the upper pole. However, we have observed limitations during the procedure due to the endoscope touching the iliac bone, especially when reaching the upper part of the kidney, and in some cases, the endoscope may slip out of the kidney due to the patient’s strong breathing. Based on this, we have improved and applied a non-rotational C-arm puncture method based on the length and angle of the needle inserted into the renal pelvis, with an angle of about 50–60 degrees, as described above, and we do not use contrast agents. The decision to not use contrast agents is based on our calculation of the necessary length and angle of the needle, and in practice, the stone is an important landmark for determining the location of the renal pelvis. We only use contrast agents in cases where the stone is located in a different position than where we need to puncture, and we also use them sparingly to determine the C point in the calculated triangle.
The results indicated that our average fluoroscopy time was 271.70 seconds (about 4.5 minutes), with the fastest being 10 seconds and the slowest being 45 minutes. Compared to previous studies that used C-arm support like Mohamed M. Abdallah11 and Abdel-Mohsen Essam12 with an average fluoroscopy time of 8.3 and 6.5 minutes respectively, our time was probably faster due to the pre-calculated position and depth of the needle based on CTscan. As a result, both the surgical and radiation exposure times were significantly reduced. On the other hand, a shorter probing time also means less exposure to X-rays, which is an important factor in protecting the health of surgeons, operating room staff, and patients, as well as speeding up the surgical process. In our study, we did not use contrast agents in 100% of cases. Cases with no or mild (grade 1) hydronephrosis accounted for 63.8% of the study population. With mild hydronephrosis, the process of probing becomes more difficult, so accurate probing is necessary for optimal results. Therefore, not using contrast agents on patients with mild hydronephrosis still yields fast results, indicating that the estimation and probing methods are reasonable. We did not use contrast agents due to several unfavorable factors, such as the drugs overflowing into the kidney and making it difficult to locate and remove stones, some patients having allergic reactions to the drugs, and reduced surgical costs. We chose to probe the middle calyx the most (60.9%), followed by the lower calyx (33.3%). Probing the upper calyx carries a higher risk of puncturing the lung membrane, so authors often avoid it. However, in reality, the type, shape, location, and degree of hydronephrosis of the stones, as well as the surgeon’s experience, all determine the choice of a reasonable probing route that creates conditions for clean stone removal with fewer complications. The stone clearance rate was 78.3%, equivalent to that of other authors. The Clavien-Dindo scoring system is currently used by many authors to evaluate complications of surgeries, including PCNL.13 In the study being referred to, out of 69 cases, two had postoperative complications, accounting for a 2.9% rate. One case experienced bleeding that required intervention to block the artery, while seven cases had fever (which subsided after 2–5 days of antibiotic treatment). According to Celik H., the rate of fever after PCNL is usually between 2.8% and 32.1%,14 with a low incidence of sepsis, but he recommends testing urine and culturing the urine prior to performing PCNL. The majority of complications and adverse events in PCNL are related to the steps of puncturing and dilating the kidney. The method used in the study was found to be rapid and associated with insignificant complications or adverse events, which the authors view as an advantage. Another advantage is that the method does not require the use of contrast agents. However, the authors suggest that larger studies are needed to further evaluate the advantages and limitations of the method, in order to provide surgeons with more options in clinical practice.
Conclusion
The technique of puncturing the renal pelvis based on the right triangle principle in percutaneous nephrolithotomy results in fast, accurate, and safe outcomes for the initial step in kidney stone removal through the skin. It does not use any contrast medium. The stone clearance rate is high, and there were no complications during the puncture and tract dilation.
Acknowledgments
The study received approval for publication from the Research Ethics Committee of Hue Central Hospital.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Reddy S, Shaik AB. Outcome and complications of percutaneous nephrolithotomy as primary versus secondary procedure for renal calculi. Int Braz J urol. 2016;42(2):262–269. doi:10.1590/S1677-5538.IBJU.2014.0619
2. Geraghty RM, Davis NF, Tzelves L, et al. Best practice in interventional management of urolithiasis: an update from the European Association of Urology Guidelines Panel for Urolithiasis 2022. Euro Urol Focus. 2023;9(1):199–208. doi:10.1016/j.euf.2022.06.014
3. Mourmouris P. Patient positioning during percutaneous nephrolithotomy: what is the current best practice? Res Rep Urol. 2018:189–193. doi:10.2147/RRU.S174396
4. Kerbl K, Clayman RV, Chandhoke PS, et al. Percutaneous stone removal with the patient in a flank position. J Urol. 1994;151(3):686–688. doi:10.1016/S0022-5347(17)35048-6
5. ElSheemy MS, Elmarakbi AA, Hytham M, et al. Mini vs standard percutaneous nephrolithotomy for renal stones: a comparative study. Urolithiasis. 2019;47(2):207–214. doi:10.1007/s00240-018-1055-9
6. Wollin DA, Preminger GM. Percutaneous nephrolithotomy: complications and how to deal with them. Urolithiasis. 2018;46(1):87–97. doi:10.1007/s00240-017-1022-x
7. Khadgi S, EL-Nahas AR, Darrad M, et al. Safety and efficacy of a single middle calyx access (MCA) in mini-PCNL. Urolithiasis. 2020;48(6):541–546. doi:10.1007/s00240-019-01176-4
8. Kim BS. Recent advancement or less invasive treatment of percutaneous nephrolithotomy. Korean J Urol. 2015;56(9):614–623. doi:10.4111/kju.2015.56.9.614
9. Corrales M, Doizi S, Barghouthy Y, et al. Ultrasound or fluoroscopy for percutaneous nephrolithotomy access, is there really a difference? A review of literature. J Endourol. 2021;35(3):241–248. doi:10.1089/end.2020.0672
10. Mues E, Gutierrez J, Loske AM. Percutaneous renal access: a simplified approach. J Endourol. 2007;21(11):1271–1276. doi:10.1089/end.2007.9887
11. Abdallah MM, Salem SM, Badreldin MR, et al. The use of a biological model for comparing two techniques of fluoroscopy-guided percutaneous puncture: a randomised cross-over study. Arab J Urol. 2013;11(1):79–84. doi:10.1016/j.aju.2012.12.001
12. Abdel-Mohsen E, Kamel M, Zayed A-L, et al. Free-flank modified supine vs. prone position in percutaneous nephrolithotomy: a prospective randomised trial. Arab J Urol. 2013;11(1):74–78. doi:10.1016/j.aju.2012.11.002
13. Zhang X-J, Zhu Z-J, Wu -J-J, Abdulhay E. Application of Clavien–Dindo classification system for complications of minimally invasive percutaneous nephrolithotomy. J Healthcare Eng. 2021;2021:1–5. doi:10.1155/2021/5361415
14. Celik H, Tasdemir C, Altintas R. An overview of percutaneous nephrolithotomy. EMJ Urol. 2015;3(1):46–52. doi:10.33590/emjurol/10313975
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

