Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
The Prevalence of Complementary and Alternative Medications Use Among Dermatology Patients in Aseer Region, Saudi Arabia
Authors Al-Atif HM, AL-Ghamdi HS, Alzubaidi WA, Alnaem NM, Qahtani SH
Received 10 July 2022
Accepted for publication 17 November 2022
Published 6 December 2022 Volume 2022:15 Pages 2607—2615
DOI https://doi.org/10.2147/CCID.S381199
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Hend M Al-Atif,1 Hasan S AL-Ghamdi,2 Waad Abdulaziz Alzubaidi,3 Nejad Mubasher Alnaem,3 Saad Hussain Qahtani3
1Department of Internal Medicine, College of Medicine, King Khalid University, Abha City, Kingdom of Saudi Arabia; 2Internal Medicine Department, Division of Dermatology, Faculty of medicine, Albaha University, Albaha City, Kingdom of Saudi Arabia; 3College of Medicine, King Khalid University, Abha City, Kingdom of Saudi Arabia
Correspondence: Hend M Al-Atif, Tel +966556464612, Email [email protected]
Purpose: The utilization rate of complementary and alternative medication (CAM) is on the rise, especially for the general population. Despite the lack of scientific support, CAM has been used for decades and is more often used among chronic patients. This research examines the prevalence of CAM use in dermatology patients in the area of Aseer, Saudi Arabia.
Materials and Methods: This research was done using a descriptive hospital-based cross-sectional survey among adults who attended the dermatological clinics at the major hospitals in the Aseer area of Southern Saudi Arabia. The dermatology outpatients were approached individually and were asked to fill out a survey about their usage of CAM therapies in the preceding year. The questionnaire included questions on patients’ socio-demographic data and clinical data on their dermatological condition, including duration and the effect on their daily life. The occurrence and pattern of CAM use and the type of CAM utilized were also examined.
Results: 353 dermatological patients filled out the study questionnaire. Patients varied in age from 18 to above 60 years, with an average of 26.1 ± 12.9 years. 203 (57.5%) patients were females. 120 (34%) of the study patients reported using folk medicine with doctor medication for their dermatological disorder, 84 (23.8%) used folk medicine and stopped using medications prescribed by a doctor, while 149 (42.2%) never used folk medicine. The most used CAM was olive oil (22%), followed by sidr (21%), honey (19%), cactus (15%), henna (14%), and garlic (13%).
Conclusion: More than half of the participants in this study used CAM, with nearly 1 out of 5 patients not using the medications prescribed by their physicians. Females with long-lasting diseases were the main users who reported using a variety of CAMs. Satisfactory results were experienced by nearly half of the patients.
Keywords: complementary or alternative medications, dermatology, use, prevalence, knowledge, effect, Saudi Arabia
Introduction
Dermatological diseases have high variability in treatment procedures, which may draw people toward complementary or alternative medications (CAMs) and treatments.1 Even though CAM often lacks scientific evidence to support it,2,3 it has been used for decades4 and has been demonstrated to be used more often by patients with chronic conditions.5 Throughout the previous few decades, CAM has attained more attention and has been more frequently used by patients worldwide.6,7 The rate of alternative medicine utilization differs across regions and ranges from 5 to 74.8% in the overall population.6 Among the reported reasons by CAM consumers are lack of efficacy from other treatments, medical drugs’ associated side effects, prolonged conditions, and the high cost of conventional medications.8,9
CAM use is frequently reported by patients with the dermatological disease with many diseases, including psoriasis, acne, and atopic dermatitis.10,11 In dermatology, CAM users have been mainly recognized as older females.12,13 Most related studies have been interested in determining which CAM therapies are utilized and their effectiveness, but little knowledge has been reported on what represents the users of CAM among dermatology patients.14,15
There is a tremendous number of people who use traditional medicine in Saudi Arabia. Research has revealed an encouraging perception and attitude toward using CAM with growing requests among the population. However, their knowledge is unsatisfactory regarding modalities and their associated consequences.8,16 The aim of this research was to investigate the prevalence of CAM use in dermatology among individuals in the Aseer region of Saudi Arabia.
Methodology
This research utilized a descriptive hospital-based cross-sectional survey among adults who attended the dermatological clinics at the leading hospitals in the Aseer province in the southern area of the Kingdom of Saudi Arabia (KSA). The research was carried out from October to December 2021. A major tertiary care facility, Aseer Central Hospital, was the primary setting.
To create the final version of the survey, a pilot study of 25 patients was conducted to obtain the participants’ feedback on the questions’ clarity and comprehension. Dermatology outpatients were contacted physically and asked to fill out a survey on how they had been using CAM therapies during the previous year. The researchers developed the questionnaire Supplementary Material after a comprehensive expert consultation and literature review. The questionnaire included questions on patients’ socio-demographic data and clinical data about their dermatological diseases, including duration and effects on daily life. The pattern and occurrence of CAM use among participants were also assessed along with the type of CAM used.
Data Analysis
After obtaining data, it was reviewed, coded, and analyzed using the statistical software IBM SPSS version 22 (SPSS, Inc. Chicago, IL). All the analyses were conducted using two-tailed tests. Statistical significance was determined using P values less than 0.05. Univariate analyses were first done using the characteristics of study patients regarding the dermatological disease, clinical data, prevalence of CAM usage, types of alternative medication used, and pattern of use. Cross-tabulation was utilized to assess the parameters associated with folk medicine usage. An exact probability test and Pearson’s chi-squared test for small dispersion were effective in assessing the importance of all relationships.
Results
A total of 353 dermatological patients answered the study questionnaire. Patients’ ages varied from 18 to above 60 years with a mean of 26.1 ± 12.9 years. 203 (57.5%) patients were females, 189 (53.5%) were single, and 158 (44.8%) were married. Regarding educational level, 226 (64%) had a university level of education/diploma, while 104 (29.5%) had a secondary level of education or below. A total of 148 (41.9%) were students, 96 (27.2%) were employed in the governmental sector, and 86 (24.4%) were not employed. Regarding monthly income, 102 (28.9%) earned 5000–10,000 SR per month, while 96 (27.2%) earned more than 15,000 SR per month, as shown in Table 1.
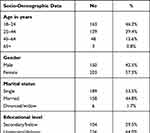 |
Table 1 Socio-Demographic Data of Sampled Patients in Aseer Region, Saudi Arabia |
Table 2 shows the dermatological disease data of the study patients. 140 (39.7%) participants had a dermatological disorder for more than 7 years, and 101 (28.6%) had one for 1–3 years. Only 56 (15.9%) patients had the disease for less than 1 year. A total of 152 (43.1%) patients reported that the disease did not affect their quality of life at work. 130 (36.8%) reported low effects, while 21 (5.9%) had significant to tremendous effects. 144 (40.8%) patients reported that they regularly use medications prescribed by their doctor, while 112 (31.7%) use them infrequently, and 97 (27.5%) had no medications at all.
 |
Table 2 Dermatological Diseases Data Among Study Patients in Aseer Region, Saudi Arabia |
Figure 1 shows the prevalence of CAM use. 120 (34%) patients reported using folk medicine with doctor-prescribed medication for their dermatological disorder, 84 (23.8%) used folk medicine while stopping prescribed medications, while 149 (42.2%) never used folk medicine. Figure 2 shows the types of folk medicine used. The most used was olive oil (22%), followed by sidr (21%), honey (19%), cactus (15%), henna (14%), garlic (13%), bitter (13%), castor oil (12%), and ginger (10%). The least used folk medicines were milk (3%), cinnamon (3%), and argan oil (1%).
 |
Figure 2 Types of used folk medicine among dermatology patients in Aseer region, Saudi Arabia. |
Table 3 shows the pattern of use of folk medicine. A total of 101 (50.2%) individuals reported that they experienced positive results after using folk medicine for their dermatological disease, but 13 (6.5%) had negative results, and 87 (43.3%) had no effect. Using folk medicine specifically to treat skin problems was reported among 124 (60.8%) patients. The most reported reasons for using folk medicine were a lack of benefit from medical drugs (47.7%), better results with folk medicine (28.6%), price of medical drugs (25.6%), side effects of medical drugs (21.1%), and religious or cultural beliefs (15.1%). Regarding sources of advice to use folk medicine, 48% reported family and friends, followed by social media (27.9%), internet sites (13.2%), physicians (6.9%), and previous experience of using folk medicine (3.9%).
 |
Table 3 Pattern of Use of Folk Medicine Among Dermatology Patients in Aseer Region, Saudi Arabia |
Table 4 shows various factors associated with folk medicine use. 63.5% of female patients used folk medicine for their dermatological disease compared to 50% of male patients, and the difference was statistically significant (P=0.011). Also, 72.1% of unemployed patients used folk medicine versus 51.4% of students (P=0.018). Folk medicine was used by 63.6% of patients with dermatological disease for more than 7 years in comparison to 46.4% of those with newly diagnosed disease (< 1 year; P=0.033). 80% of patients who experienced a tremendous effect of their dermatological disease on their daily life used folk medicine compared to 48.7% who experienced no effect (P=0.024).
 |
Table 4 Factors Associated with Folk Medicine Use Among Dermatology Patients in Aseer Region, Saudi Arabia |
Discussion
There is an increasing trend of using alternative medication for various illnesses as a component of CAM, which has long been utilized in the Middle East region.8,17 However, CAM usage by dermatology patients is rare. Clarke et al estimated that 40 to 60% of Americans had utilized CAM over a 1-year period.18 In Europe, 23% of people utilized CAM in 1 year in Denmark, while 46% had used it in Germany, and 49% had used it in France.19 Factors influencing the use of CAM include demographics,20 herbs in the area, and variation in CAM terminology. One example is bloodletting, which is considered a type of CAM in Saudi Arabia and constituted about 19% of all CAM used by the Saudi population. Conversely, none of the other nations mentioned classified bloodletting as a CAM.
The study results showed that more than half of the dermatology patients used CAM, with doctor-prescribed medications used by one-third of them. One-fifth of the patients used CAM alone after stopping prescribed medications. The most used CAMs were olive oil, sidr, honey, cactus, henna, and garlic. Factors associated with CAM use included female gender, employed patients, duration of the skin disease, and effect of disease on patients’ life quality at work.
In the USA, Sihamoni et al21 reported that only 13.4% and 39.2% of the dermatology patients used CAM for problems connected to the skin and those unrelated to skin. Herbal alternatives were the most frequently used CAM for skin issues (58.6%) and non-skin-related problems (51.8%). In Iran, Dastgheib et al22 found that 31.3% of dermatology patients had used a single CAM method. Herbal medicines were the most commonly reported therapies (89.9%).
When a comparison was made between CAM users and nonusers, the average duration of the skin problem was high among CAM consumers. Demirci and Altunay23 estimated that the illness duration was significantly associated with CAM use, which is consistent with the results of our study. This means that individuals with long-term illnesses may look for other methods to improve their health. Also, one of the factors influencing CAM was gender. The research showed that women were more likely to utilize CAM than men, which matches the current findings.24
In Singapore, a study revealed that 25.7% of dermatology patients utilized CAM.25 Patients with a greater level of education and white-collar employment had longer illness timelines and reported a higher prevalence of CAM. More than 60% of patients wanted dermatologists to give them basic advice about CAM, and 75% of the patients were willing to disclose their CAM use. In Saudi Arabia, AlGhamdi et al26 estimated that 40% of dermatology outpatients used CAM, and most of them were women (55.1%), with a mean age of 31.6 ± 12 years. Most were knowledgeable (71.2%), and just over half were married (51.9%).
Patients with acute skin disorders were observed to be more prone to CAM. According to the survey, frequently used CAM therapies included vitamins, natural products, prayers, and herbs. About 47% of CAM users did not seek medical advice from their doctors before using it, and 30% did not obtain enough information from their specialists on how to use CAM.
The present study indicates that patients employ different kinds of CAM. A previous study in the UAE reported that herbal therapies were frequently used CAMs by individuals who attended a primary health center.27 Other investigations in the Middle East concluded that herbal preparations are the most frequent CAM therapies.28,29
Regarding the effects and benefits of CAM use, the present study revealed that half of the patients reported positive effects, while the other half had nearly no change. The most reported reasons for using CMA were a lack of benefit from medical drugs, experiencing satisfactory results with CAM use, and high cost of medications. These findings are consistent with those of Sivamani21 and Dastgheib et al.22 Also, Demirci and Altunay8 estimated that 18.2% had negative consequences, but the nature of those consequences was similar and were usually allergic responses to herbal medicines used for the skin. Moreover, most patients use herbal therapists and are well aware that the items might be combined with conventional treatments. Lack of a previous study in the same region of Saudi Arabia and time constraints represent the possible limitations in this study.
Conclusions and Recommendations
In conclusion, more than half of the individuals in the present study with skin diseases used CAM. Nearly 1 out of 5 patients stopped using medications prescribed by their physicians. Females with long-lasting diseases were the main users, and a variety of CAM modalities were reported. Satisfactory results were experienced by nearly half of the patients who used CAM, who mainly used them due to a lack of benefits from medical drugs and their high cost. The vast majority of CAM users were motivated by their family/friends and social media, while dermatologists had a meager role in prescribing these modalities. More effort should be made by physicians and primarily dermatologists to discuss with their patients about these alternative therapies to guarantee safe practice.
Data Sharing Statement
On request, the corresponding author will provide access to the data sets that were utilized to support the study’s outcomes.
Participant Consent and Ethical Approval
The Declaration of Helsinki’s guiding principles were followed in the conduct of this work. The King Khalid University Research Ethics Committee approved the research (HAPO-06-B-001) and informed consent was taken from the participants.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lee J, Bielory L. Complementary and alternative interventions in atopic dermatitis. Immunol Allergy Clin North Am. 2010;30(3):411–424. doi:10.1016/j.iac.2010.06.006
2. Vieira BL, Lim NR, Lohman ME, Lio PA. Complementary and alternative medicine for atopic dermatitis: an evidence-based review. Am J Clin Dermatol. 2016;17(6):557–581. doi:10.1007/s40257-016-0209-1
3. Thandar Y, Gray A, Botha J, Mosam A. Topical herbal medicines for atopic eczema: a systematic review of randomized controlled trials. Br J Dermatol. 2017;176(2):330–343. doi:10.1111/bjd.14840
4. Eisenberg DM. Advising patients who seek alternative medical therapies. Ann Intern Med. 1997;127(1):61–69. doi:10.7326/0003-4819-127-1-199707010-00010
5. Italia S, Brüske I, Heinrich J, et al. Complementary and alternative medicine use among chronically ill adolescents from 2 german birth cohorts. Forsch Komplement Med. 2016;23(4):246–252.
6. Frass M, Strassl RP, Friehs H, Müllner M, Kundi M, Kaye AD. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: a systematic review. Ochsner J. 2012;12:45–56.
7. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi:10.1001/jama.280.18.1569
8. Abolhassani H, Naseri M, Mahmoudzadeh S. A survey of complementary and alternative medicine in Iran. Chin J Integr Med. 2012;18:409–416. doi:10.1007/s11655-012-1124-9
9. Sharples FM, van Haselen R, Fisher P. NHS patients’ perspective on complementary medicine: a survey. Complement Ther Med. 2003;11:243–248. doi:10.1016/S0965-2299(03)00107-9
10. Ernst E, Pittler MH, Stevinson C. Complementary/alternative medicine in dermatology: evidence-assessed efficacy of two diseases and two treatments. Am J Clin Dermatol. 2002;3(5):341–348. doi:10.2165/00128071-200203050-00006
11. Magin PJ, Adams J, Heading GS, Pond DC, Smith W. Complementary and alternative medicine therapies in acne, psoriasis, and atopic eczema: results of a qualitative study of patients’ experiences and perceptions. J Altern Complement Med. 2006;12(5):451–457. doi:10.1089/acm.2006.12.451
12. Landis ET, Davis SA, Feldman SR, Taylor S. Complementary and alternative medicine use in dermatology in the United States. J Altern Complement Med. 2014;20(5):392–398. doi:10.1089/acm.2013.0327
13. Noiesen E, Munk MD, Larsen K, Høyen M, Agner T. Use of complementary and alternative treatment for allergic contact dermatitis. Br J Dermatol. 2007;157(2):301–305. doi:10.1111/j.1365-2133.2007.08015.x
14. Kim GW, Park JM, Chin HW, et al. Comparative analysis of the use of complementary and alternative medicine by Korean patients with androgenetic alopecia, atopic dermatitis and psoriasis. J Eur Acad Dermatol Venereol. 2013;27(7):827–835. doi:10.1111/j.1468-3083.2012.04583.x
15. Silverberg JI, Lee-Wong M, Silverberg NB. Complementary and alternative medicines and childhood eczema: a US population-based study. Dermatitis. 2014;25(5):246–254. doi:10.1097/DER.0000000000000072
16. Adib-Hajbaghery M, Hoseinian M. Knowledge, attitude and practice toward complementary and traditional medicine among Kashan health care staff, 2012. Complement Ther Med. 2014;22:126–132. doi:10.1016/j.ctim.2013.11.009
17. Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548–1553. doi:10.1001/jama.279.19.1548
18. Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: united States, 2002–2012. Natl Health Stat Report. 2015;10(79):1.
19. Fisher P, Ward A. Medicine in Europe: complementary medicine in Europe. BMJ. 1994;309(6947):107–111. doi:10.1136/bmj.309.6947.107
20. Williams AM, Kitchen P, Eby J. Alternative health care consultations in Ontario, Canada: a geographic and socio-demographic analysis. BMC Complement Altern Med. 2011;11(1):1–3. doi:10.1186/1472-6882-11-47
21. Sivamani RK, Morley JE, Rehal B, Armstrong AW. Comparative prevalence of complementary and alternative medicine use among outpatients in dermatology and primary care clinics. JAMA Dermatol. 2014;150(12):1363–1365. doi:10.1001/jamadermatol.2014.2274
22. Dastgheib L, Farahangiz S, Adelpour Z, Salehi A. The prevalence of complementary and alternative medicine use among dermatology outpatients in Shiraz, Iran. J Evid Based Complementary Altern Med. 2017;22(4):731–735. doi:10.1177/2156587217705054
23. Tukenmez Demirci G, Altunay IK. Use of complementary and alternative medicine and assessment of dermatology quality of life index among dermatology outpatients: a cross-sectional comparative study. Br J Med Med Res. 2014;4:1812–1820. doi:10.9734/BJMMR/2014/6924
24. Barnes PM, Powell-Griner E, McFann K. Complementary and alternative medicine use among adults: united States, 2002. Adv Data. 2004;27:1–19.
25. See A, Teo B, Kwan R, et al. Use of complementary and alternative medicine among dermatology outpatients in Singapore. Aust J Dermatol. 2011;52(1):7–13. doi:10.1111/j.1440-0960.2010.00709.x
26. AlGhamdi KM, Khurrum H, Al-Natour SH, et al. Use of complementary and alternative medicine among dermatology outpatients: results from a national survey. J Cutan Med Surg. 2015;19(6):570–579. doi:10.1177/1203475415584867
27. Johnston G, Bilbao R, Graham-Brown R. The use of complementary medicine in children with atopic dermatitis in secondary care in Leicester. Br J Dermatol. 2003;149:566–571. doi:10.1046/j.1365-2133.2003.05471.x
28. Ali-Shtayeh MS, Jamous RM, Jamous RM. Herbal preparation use by patients suffering from cancer in Palestine. Complement Ther Clin Pract. 2011;17(4):235–240. doi:10.1016/j.ctcp.2011.06.002
29. Omeish AF, Abbadi W, Ghanma IM, et al. Hospital-based study on the use of herbal medicine in patients with coronary artery disease in Jordan. JPMA. 2011;61(7):683.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

