Back to Journals » Clinical Interventions in Aging » Volume 19
Trajectory Groups of 72-Hour Heart Rate After Mechanical Thrombectomy and Outcomes
Authors Wang H, Zhang C, Xu L, Xu J, Xiao G
Received 14 November 2023
Accepted for publication 6 February 2024
Published 12 February 2024 Volume 2024:19 Pages 229—236
DOI https://doi.org/10.2147/CIA.S449897
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Huaishun Wang,1,* Chi Zhang,2,* Longdong Xu,3,* Jiaping Xu,1,* Guodong Xiao1,*
1Department of Neurology and Suzhou Clinical Research Center of Neurological Disease, The Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu, 215004, People’s Republic of China; 2Department of Neurology, The Affiliated Jiangsu Shengze Hospital of Nanjing Medical University, Suzhou, Jiangsu, 215000, People’s Republic of China; 3Department of Neurology, The Fifth People’s Hospital of Changshu, Changshu, Jiangsu, 215500, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Guodong Xiao; Jiaping Xu, Department of Neurology and Suzhou Clinical Research Center of Neurological Disease, The Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu, 215004, People’s Republic of China, Email [email protected]; [email protected]
Background and Purpose: Elevated heart rate (HR) after mechanical thrombectomy (MT) was associated with an increased risk of adverse outcomes. However, optimal HR management after MT remains unclear. This study aimed to identify patient subgroups with distinct HR trajectories after MT and explore their association with outcomes.
Methods: Acute ischemic stroke patients undergoing MT therapy were prospectively recruited from July 2020 to December 2022. Their heart rate indicators were collected every hour for 72 hours after MT procedure. Latent variable mixture modeling was used to separate subjects into five groups with distinct HR trajectories. The primary outcome was poor functional outcome (mRS score > 2) at 3 months. Additional outcome was all-cause mortality (mRS score = 6) at 3 months.
Results: A total of 224 patients with large vessel occlusion were enrolled, with a mean age of 65.2+14.0 years. Eighty-seven patients had a good functional outcome, and 137 patients had a poor functional outcome. Five distinct HR trajectories were observed: low (19.2%), moderate (33.0%), rapidly stabilized HR group (20.5%), persistently high HR group (21.0%), and very high HR group (6.3%). After adjusting for potential confounders, the HR trajectory group was independently associated with poor functional outcome at 3 months (P for interaction = 0.022). The risk of having poor functional outcome was increased in the rapidly stabilized HR group (odds ratio, 3.18 [95% confidence interval, 1.10– 9.19]), the persistently high HR group (odds ratio, 5.55 [95% confidence interval, 1.72– 17.87]) and very high HR group (odds ratio, 18.32 [95% confidence interval, 2.20– 95.52]) but not in the moderate group (odds ratio, 1.50 [95% confidence interval, 0.61– 3.69]), when compared with the low HR group. No significant association was found between trajectory group and 3-month all-cause mortality.
Conclusion: HR during the first 72 hours after MT may be categorized into distinct trajectory groups, which differ in relation to poor functional outcome event risks. The findings may help to recognize potential candidates for future HR control trials.
Key words: ischemic stroke, heart rate trajectory, mechanical thrombectomy, outcome
Introduction
Cardioembolic stroke and atherothrombotic stroke are the subtypes of ischemic infarct with the highest in-hospital mortality.1 Autonomic nervous function is often impaired during a stroke, particularly in a stroke with massive infarct, and associated with worsening of functional outcome and increased risk of mortality.2,3 Heart rate (HR) represents the balance between the sympathetic and parasympathetic nervous systems, can reflect the overall stress acting on the body, and is easy to record.4–6 Many studies have showed that admission heart rate was associated with functional outcomes after ischemic stroke onset.7,8 Furthermore, other studies also provided the evidence that the mean HR was related to worse prognosis.9,10 HR variability could predict the risk of presence of myocardial ischemia in patients without known coronary artery disease or poor outcome in those with cardiovascular disease.11,12 However, these indicators do not show the direction and magnitude of HR changes. HR trajectory is a dynamic index that shows the change in HR over time, which has a lot of potential.
In recent years, the incidence of acute ischemic stroke with large vessel occlusion (LVO) has increased significantly.13,14 Mechanical thrombectomy (MT) has gradually changed the post-stroke treatment means. In recent years, it remained unclear what treatment would be used for patients with acute ischemic stroke (AIS) presenting with low National Institutes of Health Stroke Scale (NIHSS) or presenting with distal vessel occlusions.15,16 Several risk factors, such as the age, stroke severity, timing recanalization, the collateral status, blood pressure or blood pressure variability, etc., are known to have an adverse effect on their outcome.17–20 However, evidence on the impact of HR trajectory, as direct indicators of autonomic nervous system dysfunction, on the outcome in patients with large vessel strokes has remained unclear.
The purpose of this study was to explore the association between HRtrajectories within 72 hours after MT therapy and 3-month poor outcome (all-cause mortality and functional outcome).
Methods
Study Population and Setting
We prospectively analyzed data of AIS patients with large cerebral artery occlusion who underwent MT therapy in the Second Affiliated Hospital of Soochow University from July 2020 to December 2022. The exclusion criteria are as follows: (1) without the complete 72 hours heart rate records or baseline information, (2) patients died within 72 hours after MT procedure, (3) known prestroke mRS >1, (4) intracranial hemorrhage or arteriovenous malformations were confirmed by CT, (5) terminal medical diagnoses such as a stage IV cancer, (6) the ASPECT score obtained by preoperative CT is less than 6 points or (7) 3-month follow-up data is missing. All methods were carried out in accordance with relevant guidelines and regulations. After excluding 75 patients who were lost to follow-up or with incomplete baseline information or 72 hours heart rate records, 224 patients were entered into the final analysis of this study.
Data Collection and Assessment of Heart Rate Measures
Baseline information included demographic information, medical history, clinical features, time from onset to admission time, puncture to reperfusion time, onset to reperfusion time and imaging features. Medical history included history of hypertension, diabetes mellitus, prior stroke, prior coronary heart disease, atrial fibrillation, current smoking, drinking, β blocker use during the first 72 hours after MT. Clinical features included blood pressure and heart rate profile on admission, baseline NIHSS score, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and tPA administered. Imaging features included the site of the occluded brain artery (ICA with or without MCA/ACA), isolated MCA or ACA, and vertebrobasilar or other locations, the collateral status before procedure and reperfusion status after procedure. Collateral status was assessed using the American Society of Interventional and Therapeutic Neuroradiology/Society of Interventional Radiology (ASITN/SIR) grading by DSA.21 The etiologic subtypes of stroke were defined according to the Trial of ORG 10172 in acute stroke treatment (TOAST).22 The cerebral tissue reperfusion was evaluated by modified Thrombolysis in Cerebral Infarction (mTICI) scale and classified as no perfusion (grade 0), minimal perfusion (Grade 1), partial perfusion (Grade 2: a<2⁄3 of the entire vascular territory; b complete filling but slowly) and complete perfusion. The state of grade 2b/3 was generally regarded as successful reperfusion.23
Outcome Assessment
Follow-up was conducted by trained neurologists who had no knowledge of the patient’s baseline information through telephone or face-to-face visit. The primary outcome was poor functional outcome (mRS score >2) at 3 months. Additional outcome was all-cause mortality (mRS score = 6) at 3 months.
Trajectory Group Modeling
We adopted a group-based trajectory modeling approach using the TRAJ procedure in SAS software to identify HR trajectories during the first 72 hours after admission.24 This is a specialized form of finite mixture modeling, and the longitudinal HR data were fitted by a maximum likelihood method as a mixture of multiple latent trajectories in a censored normal model with a polynomial function of time. We used the Bayesian Information Criterion to determine the optimal number of strata and the highest significant order of individual trajectory groups through the modeling process. We assign a descriptive label to each group based on the visual pattern of HR over time.
Statistical Analysis
Continuous variables were appropriately expressed as means with standard deviation (SD) or medians with interquartile range (IQR) and were analyzed by 1-way ANOVA or Kruskal–Wallis test according to their normality of distribution. Categorical variables were presented as proportions and analyzed by the χ2 or Fisher exact tests. Binary logistic regression was used to estimate the risk of poor prognosis. Odds ratios (OR) and 95% confidence intervals (CI) were calculated for each group. Cox proportional hazards regression was used to analyze all-cause mortality. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated for each group. The effects of HR trajectory on mRS shift were analyzed using multivariable ordinal logistic regression model adjusted for the same variables as for the mortality analyses. Two-sided P values of 0.05 were considered statistically significant. All statistics were conducted with SAS 9.4 software (SAS Institute Inc., Cary, NC). Figures were drawn by R software (R Development Core Team 2014, www.r-project.org).
Results
A total of 224 LVO patients were finally included with the mean age of 65.2+14.0 years old. One hundred and thirty-seven (61.2%) patients had a poor functional outcome and 31 (13.8%) patients died at 3 months (Figure 1). The main causes of death were postoperative cerebral edema, cerebral hemorrhage and pulmonary infection caused by massive infarction. Among them, 42.9% were women, and median National Institutes of Health stroke scale score at arrival was 16 (13–19). Successful recanalization of large vessel occlusion was achieved in 194 patients (Table 1).
 |
Table 1 Baseline Characteristics of Mechanical Thrombectomy Treated Acute Ischemic Stroke Patients |
 |
Figure 1 Functional outcomes at 90 days among all patients. |
Trajectory Groups Based on HR
During the First 72 Hours
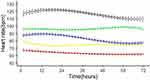
The study subjects were classified into 5 groups based on his/her HR trajectory during the first 72 hours after MT as follows (Figure 2): group 1 (a low HR group, 19.2%) indicates those who had lower-than-average HR profiles; group 2 (a moderate HR group, 33.0%) had stable HR measurements around 70 to 80 beats per minute; group 3 (a rapidly stabilized HR group, 20.5%) had moderate HR at initial presentation but gradually decreased over a few hours thereafter; group 4 (a persistently highHR group, 21.0%) represents patients having HR levels around 90 to 100 beats per minute; and group 5 (a very high HR group, 6.3%) represents patients having very high HR levels during the first 72 hours after MT.
Patients in these 5 HR trajectory groups had distinct clinical profiles (Table 1). The low HR group had lowest proportion of female (27.9%), lowest admission HR level (68.6 ± 14.5), admission glucose level and admission NIHSS score. This group had the highest proportion of cardioembolic stroke (30.2%) and lowest proportion of β blocker use (4.7%). The moderate HR group had lowest proportion of prevalence of atrial fibrillation (27.0%) and lowest admission DBP level.
Trajectory Groups and Outcome Events
In Table 2, HR trajectory groups during the first 72 hours of admission showed differential associations with poor functional outcome (mRS >2) in MT-treated acute ischemic stroke patients. The association between trajectory groups and poor functional outcome was statistically significant (P for interaction = 0.009). After adjusting for covariates, the associations still exist in Model 2 (P for interaction = 0.047) and Model 3 (P for interaction = 0.022). The risk of having poor functional outcome was increased in the rapidly stabilized HR group (odds ratio, 3.18 [95% confidence interval, 1.10–9.19]), the persistently high HR group (odds ratio, 5.55 [95% confidence interval, 1.72–17.87]) and very high HR group (odds ratio, 18.32 [95% confidence interval, 2.20–95.52]) but not in the moderate group (odds ratio, 1.50 [95% confidence interval, 0.61–3.69]), when compared with the low HR group. We did not find a statistical association between the HR groups and all-cause mortality in Table 3. In addition, we explore the association between Groups and 3-month worse functional outcome (mRS shift) in Supplement Table. But we did not find a correlation.
 |
Table 2 The Association Between Groups and 3-Month Poor Functional Outcome (mRS >2) in MT-Treated Acute Ischemic Stroke Patients |
 |
Table 3 The Association Between Groups and 3-Month All-Caused Mortality (mRS = 6) in MT-Treated Acute Ischemic Stroke Patients |
Discussion
This study focused on the analysis of acute phase HR trajectory in patients with acute ischemic stroke after MT. We found there are distinct subgroups of HR trajectories during the first 72 hours in patients with AIS afterMT. We identified 5 unique HR trajectories, namely, low, moderate, rapidly stabilized, high, very high HR. These trajectory groups have different clinical profiles and were significantly different in relation to risk for poor functional outcome.
The initial rise in BP is common in the early phase of ischemic stroke. Previous studies have found that different BP trajectories are associated with poor outcomes in stroke patients.25 A multicenter study by Petersen et al further found that patients with acute ischemic stroke demonstrate distinct SBP trajectories during the first 72 hours after MT that have differing associations with functional outcome.26
However, the studies related to HR or HR trajectory after MT are gone unreported in stroke patients after MT. For analysis of the outcome, most previous studies used baseline HR, mean and HR variability.10,27,28 Above measures did not reflect individual changes in HR over time. Some high-risk groups may be mistaken for low-risk groups. Using trajectory may help to avoid this mistake. Two recent studies evaluated the relationship between resting HR trajectories and cardio-cerebrovascular events.29,30 The results showed that elevated trajectories were associated with an increased risk of myocardial infarction and all-cause mortality. However, these associations had not been demonstrated in stroke patients receiving MT. Our study provided evidence that AIS patients with persistently high HR after MT had a higher risk of poor functional outcomes at 3 months.
The imbalance between sympathetic and parasympathetic systems often occurs in the acute phase of stroke and represents an abnormal autonomic function in response to the severity of disease. HR trajectory may reflect individual response of the autonomic nervous system to a perceived catastrophic stimulus. For patients with acute stroke, HR change and trajectory patterns after ischemic stroke would be consequences of short-term autonomic neuroregulation mechanisms encompassing external stimuli, such as psychological stress, to emergent transfer to hospital or unfamiliar environment and internal stimuli, including ischemic stroke, increased intracranial pressure, or psychological response, to perceived neural deficit.31 Given the association between increased sympathetic tone and cardiovascular disease, understanding the impact of temporal changes in HR may be important for risk stratification and individual prediction of adverse outcome.
Previous studies have linked high heart rates to worse cardiovascular outcomes, possibly due to prolonged hemodynamic strain on the artery wall, leading to stiffness in the tube wall and increased sympathetic tone, which leads to increased pressure on the artery wall and endothelial damage.32,33 Bayés syndrome is a clinical condition characterized by advanced interatrial block that can act as a predictor of atrial fibrillation, further causing an increase in HR level.34 Elevated HR is also associated with pre-thrombotic status, platelet activation and increased risk of hypertension.35 Conversely, HR reduction has been shown to prevent endothelium-dependent vascular relaxation.36 After adjusting for relevant confounders, we found that HR trajectory remained an independent risk factor for adverse functional outcome in AIS patients. This means that patients with high HR for a long period of time may develop vasoconstriction and thrombosis, leading to a poor functional outcome. The clinical significance of heart rate and blood pressure trajectories remains unclear. Compared with blood pressure, HR has been studied less. We hope that more researchers will pay attention to the importance of HR in stroke patients.
First, it was a single-center, small sample size observational study. The generalization of our results to other clinical practices is inconclusive. Multicenter, large-scale cohort studies are needed to confirm our findings. Second, the study did not collect information inflammation or general anesthesia, which may HR measurement. Third, HR indicators were collected every hour for 72 hours. Further long-term continuous dynamic HR recording was worth exploring.
Conclusion
This study provides a longitudinal profile of HR in the first 72 hours after EVT. Stroke patients exhibit five distinct HR trajectories that are associated with poor 3-month outcomes. Patients with stroke demonstrate 5 unique HR trajectories that differ in their association with functional outcome. The HR trajectory of stroke patients, especially those with persistently high HR, should be paid attention to. Future studies should focus more on the relationship between individual HR changes over time and prognosis rather than just HRV and prognosis.
Data Sharing Statement
The datasets generated and/or analysed during the current study are not publicly available due to the datasets are owned by the institution only but are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The informed consent to participate was obtained from all participants and written informed consent in accordance with the Declaration of Helsinki. This study was performed in accordance with the appropriate guidelines and regulations. The study protocols were approved by the ethics committees of Second Affiliated Hospital of Soochow University, Soochow University.
Acknowledgments
Huaishun Wang, ChiZhang and LongdongXu are co-first authors for this study. Jiaping Xu and Guodong Xiao are co-correspondence authors for this study.
We thank the study participants, their relatives, and the clinical staff for their support and contribution to this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by a grant from the National Natural Science Foundation of China (grant: 82071310), Jiangsu Provincial Medical Key Discipline Project (grant: ZDXKB2016022), Suzhou Clinical Research Center of Neurological Disease (grant: Szzx201503), Discipline Construction Program of the Second Affiliated Hospital Soochow University (grant: XKTJ-XK202001).
Disclosure
The authors declare that they have no competing interests and the research was conducted in the absence of any commercial or financial relationships that could be constructed as a potential conflict of interest.
References
1. Arboix A, Oliveres M, Massons J, Pujades R, Garcia-Eroles L. Early differentiation of cardioembolic from atherothrombotic cerebral infarction: a multivariate analysis. Eur J Neurol. 1999;6(6):677–683. doi:10.1046/j.1468-1331.1999.660677.x
2. Xiong L, Tian G, Leung H, et al. Autonomic dysfunction predicts clinical outcomes after acute ischemic stroke: a prospective observational study. Stroke. 2018;49(1):215–218. doi:10.1161/STROKEAHA.117.019312
3. Zhao M, Guan L, Collet J, Wang Y. Relationship between ischemic stroke locations, etiology subtypes, neurological outcomes, and autonomic cardiac function. Neurological Res. 2020;42(8):630–639. doi:10.1080/01616412.2020.1782103
4. He L, Wang J, Zhang L, Zhang X, Dong W, Yang H. Decreased fractal dimension of heart rate variability is associated with early neurological deterioration and recurrent ischemic stroke after acute ischemic stroke. J Neurol Sci. 2019;396:42–47. doi:10.1016/j.jns.2018.11.006
5. Xu Y, Wang X, Yang J, Zhou L, Pan Y. Changes of deceleration and acceleration capacity of heart rate in patients with acute hemispheric ischemic stroke. Clin Interventions Aging. 2016;11:293–298. doi:10.2147/CIA.S99542
6. Wei C, Shyu K, Chien K. Association of heart rate trajectory patterns with the risk of adverse outcomes for acute heart failure in a heart failure cohort in Taiwan. Acta Cardiologica Sinica. 2020;36(5):439–447. doi:10.6515/ACS.202009_36(5).20200519A
7. Jeong H, Ko S, Kim C, et al. Tachycardia burden in stroke unit is associated with functional outcome after ischemic stroke. Int J Stroke. 2016;11(3):313–320. doi:10.1177/1747493016631357
8. Nolte C, Erdur H, Grittner U, et al. Impact of heart rate on admission on mortality and morbidity in acute ischaemic stroke patients - results from Vista. Eur J Neurol. 2016;23(12):1750–1756. doi:10.1111/ene.13115
9. Tomii Y, Toyoda K, Nakashima T, et al. Effects of hyperacute blood pressure and heart rate on stroke outcomes after intravenous tissue plasminogen activator. J Hyperten. 2011;29(10):1980–1987. doi:10.1097/HJH.0b013e32834a764e
10. Lee K, Kim B, Han M, et al. Effect of heart rate on stroke recurrence and mortality in acute ischemic stroke with atrial fibrillation. Stroke. 2020;51(1):162–169. doi:10.1161/STROKEAHA.119.026847
11. Goldenberg I, Goldkorn R, Shlomo N, et al. Heart rate variability for risk assessment of myocardial ischemia in patients without known coronary artery disease: the hrv-detect (heart rate variability for the detection of myocardial ischemia) study. J Am Heart Assoc. 2019;8:e014540.
12. Fang S, Wu Y, Tsai P. Heart rate variability and risk of all-cause death and cardiovascular events in patients with cardiovascular disease: a meta-analysis of cohort studies. Biol Res Nurs. 2020;22(1):45–56. doi:10.1177/1099800419877442
13. Renú A, Millán M, San Román L, et al. Effect of intra-arterial alteplase vs placebo following successful thrombectomy on functional outcomes in patients with large vessel occlusion acute ischemic stroke: the choice randomized clinical trial. JAMA. 2022;327(9):826–835. doi:10.1001/jama.2022.1645
14. Yoshimura S, Sakai N, Yamagami H, et al. Endovascular therapy for acute stroke with a large ischemic region. New Engl J Med. 2022;386(14):1303–1313. doi:10.1056/NEJMoa2118191
15. Alexandre A, Colò F, Brunetti V, et al. Mechanical thrombectomy in minor stroke due to isolated m2 occlusion: a multicenter retrospective matched analysis. J Neurointervent Surg. 2023;15(e2):e198–e203. doi:10.1136/jnis-2022-019557
16. Radu R, Costalat V, Fahed R, et al. First pass effect as an independent predictor of functional outcomes in medium vessel occlusions: an analysis of an international multicenter study. Eur Stroke J;2023. 23969873231208276. doi:10.1177/23969873231208276
17. Wollenweber F, Tiedt S, Alegiani A, et al. Functional outcome following stroke thrombectomy in clinical practice. Stroke. 2019;50(9):2500–2506. doi:10.1161/STROKEAHA.119.026005
18. Ravindran A, Killingsworth M, Bhaskar S. Cerebral collaterals in acute ischaemia: implications for acute ischaemic stroke patients receiving reperfusion therapy. Euro J Neurosci. 2021;53(4):1238–1261. doi:10.1111/ejn.14955
19. Alawieh A, Vargas J, Fargen K, et al. Impact of procedure time on outcomes of thrombectomy for stroke. J Am College Cardiol. 2019;73(8):879–890. doi:10.1016/j.jacc.2018.11.052
20. Mistry E, Mehta T, Mistry A, et al. Blood pressure variability and neurologic outcome after endovascular thrombectomy: a secondary analysis of the best study. Stroke. 2020;51(2):511–518. doi:10.1161/STROKEAHA.119.027549
21. Liu L, Ding J, Leng X, et al. Guidelines for evaluation and management of cerebral collateral circulation in ischaemic stroke 2017. Stroke Vascul Neurol. 2018;3(3):117–130. doi:10.1136/svn-2017-000135
22. Adams H, Bendixen B, Kappelle L, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. Toast. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41. doi:10.1161/01.STR.24.1.35
23. Zaidat O, Yoo A, Khatri P, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44(9):2650–2663. doi:10.1161/STROKEAHA.113.001972
24. Nagin D, Odgers C. Group-based trajectory modeling in clinical research. Ann Rev Clin Psychol. 2010;6(1):109–138. doi:10.1146/annurev.clinpsy.121208.131413
25. Kim B, Cho Y, Hong K, et al. Trajectory groups of 24-hour systolic blood pressure after acute ischemic stroke and recurrent vascular events. Stroke. 2018;49(8):1836–1842. doi:10.1161/STROKEAHA.118.021117
26. Petersen N, Kodali S, Meng C, et al. Blood pressure trajectory groups and outcome after endovascular thrombectomy: a multicenter study. Stroke. 2022;53(4):1216–1225. doi:10.1161/STROKEAHA.121.034408
27. Cooney M, Vartiainen E, Laatikainen T, Juolevi A, Dudina A, Graham I. Elevated resting heart rate is an independent risk factor for cardiovascular disease in healthy men and women. Am Heart J. 2010;159(4):612–619.e613. doi:10.1016/j.ahj.2009.12.029
28. Tang S, Xiong L, Fan Y, Mok V, Wong K, Leung T. Stroke outcome prediction by blood pressure variability, heart rate variability, and baroreflex sensitivity. Stroke. 2020;51(4):1317–1320. doi:10.1161/STROKEAHA.119.027981
29. Wei C, Chen P, Hsu H, et al. Association of heart rate trajectories with the risk of adverse outcomes in a community-based cohort in Taiwan. PeerJ. 2020;8:e8987.
30. Feng Z, Qin H, Zhang Y, et al. Acute-phase heart rate trajectories and functional outcomes in acute ischemic stroke. J Clin Hypertens. 2022;24(4):457–464. doi:10.1111/jch.14441
31. Salman I. Major autonomic neuroregulatory pathways underlying short- and long-term control of cardiovascular function. Curr Hypertens Rep. 2016;18(3):18. doi:10.1007/s11906-016-0625-x
32. Cavalcante J, Lima J, Redheuil A, Al-Mallah M. Aortic stiffness: current understanding and future directions. Journal of the American College of Cardiology. 2011;57(14):1511–1522. doi:10.1016/j.jacc.2010.12.017
33. Chen S, Li W, Jin C, et al. Resting heart rate trajectory pattern predicts arterial stiffness in a community-based Chinese cohort. Arteriosclerosis Thrombosis Vasc Biol. 2017;37(2):359–364. doi:10.1161/ATVBAHA.116.308674
34. Arboix A, Martí L, Dorison S, Sánchez M. Bayés syndrome and acute cardioembolic ischemic stroke. World J Clin Cases. 2017;5(3):93–101. doi:10.12998/wjcc.v5.i3.93
35. Sharashova E, Wilsgaard T, Løchen M, Mathiesen E, Njølstad I, Brenn T. Resting heart rate trajectories and myocardial infarction, atrial fibrillation, ischaemic stroke and death in the general population: the tromsø study. Euro J Prevent Cardiol. 2017;24(7):748–759. doi:10.1177/2047487316688983
36. Custodis F, Schirmer S, Baumhäkel M, Heusch G, Böhm M, Laufs U. Vascular pathophysiology in response to increased heart rate. Journal of the American College of Cardiology. 2010;56(24):1973–1983. doi:10.1016/j.jacc.2010.09.014
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.