Back to Journals » Vascular Health and Risk Management » Volume 20
Trends in AAA Repair in Australia Over Twenty Years
Authors Anthony L, Gillies M, Goh D
Received 11 November 2023
Accepted for publication 31 January 2024
Published 28 February 2024 Volume 2024:20 Pages 69—75
DOI https://doi.org/10.2147/VHRM.S449375
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Lakmali Anthony,1 Madeline Gillies,2 David Goh1
1Department of Vascular Surgery, Northern Health, Epping, Victoria, Australia; 2Department of Surgery, Western Health, Footscray, Victoria, Australia
Correspondence: Lakmali Anthony, Email [email protected]
Background: The advent of endovascular techniques has revolutionised the treatment of abdominal aortic aneurysms (AAA). Many countries have seen a transition from open AAA repair (OAR) to endovascular AAA repair (EVAR) over the past 25 years. The only study done in Australia that describes this change was done in the private sector. Majority of healthcare in Australia is delivered through the public, universal healthcare system. The aim of this study was to evaluate the trends in AAA repair in the Australian public sector over the past two decades.
Methods: The Australian Institute of Health and Welfare (AIHW) Procedures Data Cubes from the National Hospitals Data Collection was used to extract data pertaining to AAA repairs from 2000 to 2021. Population data from the Australian Bureau of Statistics was used to calculate incidence of each type of repair per 100,000 population.
Results: There were 65,529 AAA repairs performed in the Australian public sector from 2000 to 2021. EVARs accounted for 64.4% (42,205) and OARs accounted for 35.6% (23, 324) of them. EVAR surpassed OAR as the preferred method of AAA repair in 2006. This trend was observed in both males and females and across all age groups.
Conclusion: There was a consistent and steady transition from OAR to EVAR over the 21 year period with EVAR surpassing OAR as the preferred method of AAA repair relatively early in Australia compared to other countries. Further research that investigates medium- and long-term outcomes of newer stent grafts is needed to further ascertain the continued viability and effectiveness of this trend in AAA treatment.
Keywords: abdominal aortic aneurysm, AAA, endovascular aneurysm repair, EVAR, open surgical repair
Introduction
An abdominal aortic aneurysm (AAA) is a pathological dilatation of the aorta that is more than 50% of its usual diameter. An infra-renal aorta that is greater than 3cm is generally considered to be aneurysmal. Prevalence of AAA is estimated to be 4.8% in the general population with variations between genders, standing at 6% for males and 1.6% for females.1 Each year in Australia, AAAs lead to more than 3100 hospital admissions and are responsible for over 1000 deaths annually, highlighting the critical nature of AAAs that require hospital care.2
The current treatment options for AAA include open AAA repair (OAR) and endovascular AAA repair (EVAR). Open repair was first described in 1951 by Dubost.3 Until 1990’s, this was the only method of treatment of AAAs and it carried a high perioperative morbidity and mortality. In the 1990s, the advent of EVAR introduced a less invasive approach, significantly reducing perioperative morbidity and mortality compared to open repair.4 The first commercial EVAR was successfully deployed in Australia in 1993.5 Since this milestone, Australia has not only been pioneering early adoption of such technology but has also significantly contributed to the innovation in stent graft technology with the first bifurcated graft in 1994 and first fenestrated graft in 1998.5
Since the introduction of EVAR in 1990’s, many developed countries in Asia, Europe and North America have reported national trends showing a shift from open to endovascular repair of AAA over time.6–8 These countries include Korea, Japan, Denmark, Finland, Hungary, Italy, Norway, Sweden, Switzerland, United Kingdom and North America. This likely reflects a change in management of AAAs that occurred after the positive results of two large randomised controlled trials that were published in 2005 that compared outcomes of open repair to endovascular repair of AAAs.9,10 However, the adoption rate of new and costly technologies varies among healthcare systems. For instance, in Canada, EVARs represented a minority of AAA treatments until well into 2008.11 Published data pertaining to these trends within the Australian context is lacking. Existing studies have primarily focused on the private healthcare sector, and to the best of our knowledge, none has explored trends within the Australian public healthcare system thus far. Majority of medical care in Australia, including elective surgery, is delivered through the public, universal healthcare system. Accordingly, the aim of this study was to examine national trends in AAA repair in the Australian public sector to determine if similar trends occurred in the public system in the early 21st century.
Methods
This study used data from the Australian Institute of Health and Welfare (AIHW) Procedures Data Cubes from the National Hospitals Data Collection. Data were extracted from procedure chapter VIII “Procedures on the cardiovascular system”, for open infrarenal AAA repair (MBS codes 33,115, 33,118, 33,121), open infrarenal repair of ruptured AAA (MBS codes 33,154, 33,157, 33,160) and infrarenal EVAR (MBS codes 33,116, 33,119). These data can only distinguish ruptured and elective repair for open approach. The Australian Institute of Health and Welfare (AIHW) Ethics Committee has provided ethical approval for AIHW data collection and use of such publicly available data in research publications. As such, local hospital ethics committee ethical approval was not required.
Statistical Analysis
The unadjusted incidence of AAA operations and selected subcategories are presented with descriptive statistics. The population-adjusted incidence was calculated per 100,000 population using annual Australian Bureau of Statistics (ABS) data for each age and sex group. Simple linear regression was performed to quantify the change in population-adjusted incidence of each operation with year as the independent variable. This was expressed as a change per year per 100,000 people (β) with 95% confidence intervals. A p-value less than 0.05 was considered statistically significant. All statistical analyses were performed in the statistics package R (R Core Team, 2023), and figures were generated using GraphPad Prism 8 (Dotmatics, Boston, Massachusetts, United States).
Results
There were 65,529 AAA repairs performed during the study period. Among these, 82.6% were in male patients and 17.4% in female patients (Table 1). The majority were aged 70–79 years (43.9%). Approximately two-thirds of the procedures were endovascular (64.4%), and one-third were open (35.6%) (Table 1).
 |
Table 1 Cumulative Population Characteristics and Simple Linear Regression of Incidence with Year as the Independent Variable |
In the initial year of this study, 2000, OARs were the preferred method of AAA repair and accounted for 70.6% (n = 2082) of all repairs, whereas EVARs only accounted for 29.4% (n = 865). Since then, there has been a consistent shift towards EVAR over OAR over time (Figure 1). The proportion of EVARs surpassed OARs as the preferred method of AAA repair in 2006 (Figure 1). By 2021, EVARs accounted for 84.5% (n = 2564) of all AAA repairs, while OARs only accounted for 15.5% (n = 469).
 |
Figure 1 Incidence of AAA interventions per Australian standard population. |
A significant shift from OAR to EVAR was noted in both male and female patients (Figure 2). Regression analysis demonstrated a significant decrease in OAR (β = −0.77, p < 0.001 for males; β = −0.21, p < 0.001 for females) and a concurrent significant increase in EVAR (β = 0.53, p < 0.001 for males; β = 0.15, p < 0.001 for females) (Table 2).
 |
Table 2 Cumulative Incidence and Simple Linear Regression of OAR and EVAR Performed Over the Study Period by Age, Sex and Type of Presentation |
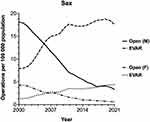 |
Figure 2 Incidence of AAA interventions in males and females per 100,000 population. |
The trend was consistent across different age groups, with all demographics exhibiting a significant uptick in EVAR procedures and a decline in OAR interventions (Table 2 and Figure 3). Notably, the most pronounced shift towards EVAR was observed in patients over the age of 80 (β = 1.63, p < 0.001) (Table 2). A discernible trend across the age spectrum reflected a move away from OAR, with the 70–79 age group exhibiting a particularly marked decrease (β = −4.29, p < 0.001) (Table 2). The EVAR:OAR ratio increased steadily over the study period for both males and females and for all age groups (Figure 4).
 |
Figure 3 Incidence of AAA interventions by age group per 100,000 population. |
 |
Figure 4 EVAR to OAR ratio during the study period by age and sex. |
In examining the types of AAA presentations, there was a notable decrease in elective OARs (β = −0.38, p < 0.001) and OARs for ruptured aneurysms (β = −0.06, p < 0.001) over the study period (Table 2).
Discussion
Abdominal aortic aneurysm is a key pathology in vascular surgery that has seen significant advancements in management over the last 20 years. This study presents an extensive analysis of 65,529 AAA repairs, unveiling a substantial shift from OAR to EVAR in the public sector of Australia over a 21-year period.
This study showed a steady increase in uptake of EVAR in Australia; however, it also highlighted that the overall incidence of AAA repairs has not experienced a corresponding increase. This suggests that the integration of EVAR into clinical practice has not resulted in an increase in total volume of AAA repairs but has prompted a definitive shift from OAR to EVAR as the preferred treatment modality. Furthermore, this data implies that the advent of minimally invasive surgical options has not relaxed the stringent patient selection criteria employed by surgeons in the management of AAA, underlining a continued commitment to judicious surgical decision-making. A similar trend was observed in a study conducted in the Australian private sector, reflecting consistency in surgical decision-making across the public and private sectors in Australia.5 Comparable transitions to minimally invasive approaches have been noted in the realm of general surgery with the introduction of laparoscopic inguinal hernia repair without an overall increase in the volume of hernia repairs.12
Emerging trends from continents like Asia, Europe, and America depict a parallel surge in the adoption of EVAR in comparison to OAR. In this study of the Australian public sector, EVAR surpassed OAR as the preferred method of AAA repair in 2006. In the Australian private sector, the trend was slightly ahead, with EVAR overtaking OAR as early as 2005.5 When positioned against an international backdrop, Australia demonstrated an earlier transition to and widespread adoption of EVAR. To the best of our knowledge, the United States was the earliest to document EVAR overtaking OAR in 2006.8 Many other nations reached this pivotal moment considerably later. For instance, this shift was observed in Sweden, Italy, and the United Kingdom in 2009, followed by France and Spain in 2010.6,13–15 New Zealand noted a similar transition in 2011, five years after Australia.16 Additionally, Japan and Finland joined this trend in 2013.17,18 This early uptake and proliferation of EVAR in Australia can likely be attributed to the pioneering role that Australian vascular surgeons played in the innovation of stent graft technology. Conversely, the delay in uptake of EVAR in Europe is likely attributable to organisations such as National Institute for Health Care and Excellence (NICE) in the United Kingdom advising against overuse of EVAR. Current NICE guidelines advise against the use of EVAR if the patient is suitable for open surgical repair.19 They recommend EVAR or conservative management if the patient is unsuitable for open repair due to abdominal co-pathology, anaesthetic or medical risk factors. This is based on studies evaluating the medium to long-term outcomes of EVAR when compared to open surgery.20–23 Several landmark studies have indeed reported that the early survival benefit of EVAR is lost in the medium to long term and that EVAR is associated with a higher rate of reintervention and rupture.20–23 These guidelines do raise concern about a rapid increase in EVAR among younger and generally healthier patient populations, and rapid proliferation of EVAR in Australia is likely not in accordance with these guidelines. Australia, however, does not have such national guidelines and therefore surgeons have the capacity to apply more personal judgement, taking into account their clinical expertise and patient preferences. Although the rapid proliferation of EVAR in Australia is not in keeping with NICE guidelines, the rise in incidence over time was least pronounced in younger patient demographics, exhibiting a gradual escalation corresponding with advancing age groups. Furthermore, trials that found medium to long-term disadvantages of EVAR were conducted between 1999 and 2008. Stent graft technology has evolved rapidly during, and since that time and modern grafts may demonstrate comparable longevity to open surgical repair.
The decline in the frequency of open repairs, however, carries important ramifications for the education and skill retention of vascular surgeons. Numerous studies have established a link between surgeon volume of open aortic surgery and improved patient outcomes.24–27 Geiger et al, in a recent analysis, identified that performing a minimum of seven open aortic procedures annually was a standalone predictor of better outcomes following OAR.27 Our study demonstrated a significant decline in open procedures over the past two decades. This evolving landscape of AAA management presents a distinctive challenge to vascular surgeons and surgical units across Australia. It necessitates the formulation of strategic approaches to preserve and hone the essential skills required for open aortic operations, a critical competency within the vascular surgeon’s repertoire. This shift underscores the need for innovative training and practice models to ensure the continued proficiency in these fundamental surgical techniques amidst the rising predominance of endovascular procedures.
Strengths and Limitations
The main strength of this study is the large sample size and the study time span of the 21 years. This allowed for a national population analysis of AAA repairs as well as associated patient demographics such as age and sex. As such, this is the largest and most comprehensive analysis of AAA repairs over the last two decades in Australia in the public sector.
One limitation of the study though was that the AIHW data only capture the procedural and demographic information. Details of perioperative outcomes such as complications, need for reintervention or death, were not available for analysis. Another limitation of this study was that while the Medical Benefits Schedule (MBS) codes distinctly categorised ruptured and non-ruptured OARs, such distinction was not applied to EVARs. As a result, our analysis could not compare the trends in ruptured and non-ruptured AAA repairs.
Another limitation of the use of AIHW data is potential inaccuracies in coding. While AIHW conducts regular quality checks to minimise these errors, inaccuracies can occur due to human error and as such cannot be completely eliminated.
Conclusion
Over the past two decades, there has been a notable paradigm shift in the management of AAAs in Australia. EVAR has progressively superseded OAR as the preferred treatment method for AAAs, a shift that Australia witnessed relatively earlier than many other nations. This transition towards EVAR, in preference over OAR, has been observed consistently in both males and females and across all age groups, with a particularly marked increase among octogenarians. Given these developments, it becomes essential to conduct further research into the medium- and long-term outcomes of EVAR, especially those performed with new technological advancements over the past 20 years. Such investigations are crucial to ascertain the continued viability and effectiveness of this trend in AAA treatment.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li X, Zhao G, Zhang J, et al. Prevalence and trends of the abdominal aortic aneurysms epidemic in general population—a meta-analysis. PLoS One. 2013;8(12):e81260. doi:10.1371/journal.pone.0081260
2. Australian Institute of Health and Welfare. Principal Diagnosis Data Cubes 2021-2022; 2023.
3. Dubost C, Allary M, Oeconomos N. Treatment of aortic aneurysms; removal of the aneurysm; re-establishment of continuity by grafts of preserved human aorta. Mem Acad Chir. 1951;77:381–383.
4. Yei K, Mathlouthi A, Naazie I, Elsayed N, Clary B, Malas M. Long-term outcomes associated with open vs endovascular abdominal aortic aneurysm repair in a Medicare-matched database. JAMA Network Open. 2022;5(5):e2212081. doi:10.1001/jamanetworkopen.2022.12081
5. Qin KR, Perera M, Papa N, Mitchell D, Chuen J. Open versus Endovascular Abdominal Aortic Aneurysm Repair in the Australian Private Sector Over Twenty Years. J Endovasc Ther. 2021;28(6):844–851. doi:10.1177/15266028211028215
6. Mani K, Lees T, Beiles B, et al. Treatment of abdominal aortic aneurysm in nine countries 2005-2009: a vascunet report. Eur J Vasc Endovasc Surg. 2011;42(5):598–607. doi:10.1016/j.ejvs.2011.06.043
7. Joh JH, Park YY, Cho SS, Park HC. National trends for open and endovascular repair of aneurysms in Korea: 2004-2013. Exp Ther Med. 2016;12(5):3333–3338. doi:10.3892/etm.2016.3781
8. Suckow BD, Goodney PP, Columbo JA, et al. National trends in open surgical, endovascular, and branched-fenestrated endovascular aortic aneurysm repair in Medicare patients. J Vasc Surg. 2018;67(6):1690–1697.e1. doi:10.1016/j.jvs.2017.09.046
9. EVAR Trial Participants. Endovascular aneurysm repair versus open repair in patients with abdominal aortic aneurysm (EVAR trial 1): randomised controlled trial. Lancet. 2005;365:9478.
10. Blankensteijn JD, de Jong SE, Prinssen M, et al. Two-year outcomes after conventional or endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2005;352(23):2398–2405.
11. Chadi SA, Rowe BW, Vogt KN, et al. Trends in management of abdominal aortic aneurysms. J Vasc Surg. 2012;55(4):924–928. doi:10.1016/j.jvs.2011.10.094
12. Kevric J, Papa N, Toshniwal S, et al. Fifteen-year groin hernia trends in Australia: the era of minimally invasive surgeons. ANZ J Surg. 2018;88(7–8):E298–E302. doi:10.1111/ans.14466
13. Mani K, Björck M, Wanhainen A. Changes in the management of infrarenal abdominal aortic aneurysm disease in Sweden. Br J Surg. 2013;100(5):638–644. doi:10.1002/bjs.9046
14. Salomon du Mont L, Rinckenbach S, Besch G, Steinmetz E, Kretz B. Evolution of Practices in Treatment of Abdominal Aortic Aneurysm in France between 2006 and 2015. Ann Vasc Surg. 2019;58:38–44. doi:10.1016/j.avsg.2018.12.063
15. Lopez-de-Andrés A, Jiménez-Trujillo I, Jiménez-García R, et al. National trends in incidence and outcomes of abdominal aortic aneurysm among elderly type 2 diabetic and non-diabetic patients in Spain (2003-2012). Cardiovasc Diabetol. 2015;14:48. doi:10.1186/s12933-015-0216-1
16. Gormley S, Bernau O, Xu W, Sandiford P, Khashram M. Incidence and Outcomes of Abdominal Aortic Aneurysm Repair in New Zealand from 2001 to 2021. J Clin Med. 2023;12(6):2331. doi:10.3390/jcm12062331
17. Hoshina K, Ishimaru S, Sasabuchi Y, Yasunaga H, Komori K. Japan Committee for Stentgraft Management (JACSM). Outcomes of Endovascular Repair for Abdominal Aortic Aneurysms: a Nationwide Survey in Japan. Ann Surg. 2019;269(3):564–573. doi:10.1097/SLA.0000000000002508
18. Laine MT, Laukontaus SJ, Sund R, et al. A Population-Based Study of Abdominal Aortic Aneurysm Treatment in Finland 2000 to 2014. Circulation. 2017;136(18):1726–1734. doi:10.1161/CIRCULATIONAHA.117.028259
19. National Institute for Health and Care Excellence (NICE) UK. Abdominal aortic aneurysm: diagnosis and management. Available from: https://www.nice.org.uk/guidance/ng156/chapter/Recommendations#repairing-unruptured-aneurysms.
20. EVAR trial participants. Endovascular aneurysm repair versus open repair in patients with abdominal aortic aneurysm (EVAR trial 1): randomised controlled trial. Lancet. 2005;365(9478):2179–2186. doi:10.1016/S0140-6736(05)66627-5
21. Lederle FA, Freischlag JA, Kyriakides TC, et al. Long-term comparison of endovascular and open repair of abdominal aortic aneurysm. N Engl J Med. 2012;367(21):1988–1997. doi:10.1056/NEJMoa1207481
22. De Bruin JL, Baas AF, Buth J, et al. Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med. 2010;362(20):1881–1889. doi:10.1056/NEJMoa0909499
23. Becquemin JP. The ACE trial: a randomized comparison of open versus endovascular repair in good risk patients with abdominal aortic aneurysm. J Vasc Surg. 2009;50(1):222–224. doi:10.1016/j.jvs.2009.04.074
24. Young EL, Holt PJ, Poloniecki JD, et al. Meta-analysis and systematic review of the relationship between surgeon annual caseload and mortality for elective open abdominal aortic aneurysm repairs. J Vasc Surg. 2007;46(6):1287–1294. doi:10.1016/j.jvs.2007.08.058
25. Sawang M, Paravastu SCV, Liu Z, et al. The relationship between aortic aneurysm surgery volume and peri-operative mortality in Australia. Eur J Vasc Endovasc Surg. 2019;57(4):510–519. doi:10.1016/j.ejvs.2018.10.028
26. Sawang M, Paravastu SCV, Liu Z, et al. The relationship between operative volume and peri-operative mortality after non-elective aortic aneurysm repair in Australia. Eur J Vasc Endovasc Surg. 2020;60(5):519–530. doi:10.1016/j.ejvs.2020.07.043
27. Geiger JT, Fleming FJ, Stoner M, Doyle A. Surgeon volume and established hospital perioperative mortality rate together predict for superior outcomes after open abdominal aortic aneurysm repair. J Vasc Surg. 2022;75(2):504–513.e3. doi:10.1016/j.jvs.2021.08.077
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
