Back to Journals » Advances in Medical Education and Practice » Volume 14
University Pre-Professional Program: A Transitional Phase from Didactic to PBL Pedagogy
Authors Memon I , Alrayani YH, Akhund S, Feroz Z, Rohra DK, Alkushi A, Alrashid AA , Anjum I
Received 13 May 2023
Accepted for publication 17 September 2023
Published 17 November 2023 Volume 2023:14 Pages 1299—1307
DOI https://doi.org/10.2147/AMEP.S421180
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Ismail Memon,1– 3 Yazeed H Alrayani,4 Shahid Akhund,5 Zeeshan Feroz,2,3 Dileep Kumar Rohra,6 Abdulmohsen Alkushi,2,3 Azzam A Alrashid,4 Irfan Anjum7
1Human Body Structure and Function Department, Saba University, School of Medicine The Bottom Saba, Dutch Caribbean the Netherlands; 2Basic Sciences Department, College of Science and Health Professions, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; 3King Abdullah International Medical Research Center, Riyadh, Saudi Arabia; 4College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia; 5Anatomy and Medical Education Department, College of Medicine, Alfaisal University, Riyadh, Saudi Arabia; 6Pharmacology Department, College of Medicine, Alfaisal University, Riyadh, Saudi Arabia; 7Clinical Psychology, General Manchester Mental Health Foundation Trust, London, UK
Correspondence: Ismail Memon, Anatomy, Saba University School of Medicine, Church Street, The Bottom, Saba Caribbean, the Netherlands, Tel +599 416 7795, Email [email protected]
Purpose: The College of Science and Health Professions offers the University Pre-Professional Program (UPPP) to newly enrolled students. This study aimed to evaluate the effectiveness of the program in preparing students to become self-directed learners and to seek students’ perceptions about student-centered teaching.
Methods: A quantitative quasi-experimental study that used a pre and post-test survey in two stages, before and after semester-4. A self-developed questionnaire was distributed online.
Results: The t-test showed students (n=701) after semester-4 had a significant increase in the understanding of Problem-Based Learning (PBL) (t (699) = − 8.27, p < 0.01), PBL dynamics (t (699) = − 5.12, p < 0.01), learning and dynamics of Case-Based Learning (CBL) and Self-Directed Learning (SDL) (t (699) = − 6.48, p < 0.01), and facilitators’ role in such curriculum (t (699) = − 3.41, p < 0.01). The ANOVA showed students attending various courses perceived the program variables differently (Learning in PBL p = 0.08, PBL dynamics p < 0.01, CBL and SDL dynamics p < 0.01, role of facilitator in PBL p < 0.01). Regarding the resources used by students during the basic medical sciences courses, no significant difference was observed between the study groups (p = 0.06). However, the only significant difference observed was in their satisfaction with the question related to assessment and course (p < 0.01).
Conclusion: The UPPP improved students’ understanding of student-centered teaching and learning approaches, especially the PBL. Thus, UPPP helps students shift their learning habits from didactic to student-centered modern learning approaches. Variation among different students’ groups could be attributed to their previous academic background and change in learning medium to English. This study suggests that preparatory teaching programs like UPPP are helpful for students interested in joining the bachelor’s programs in countries like Saudi Arabia where English is not a native language.
Keywords: university pre-professional program, student-centered learnings, curriculum, didactic
Introduction
Many universities worldwide offer pre-professional, preparatory, or mentorship programs to school graduates/newcomers to support their entry into the undergraduate programs accompanied by the transition to university life.1–3 The preparatory year programs help students transition from the high school system (didactic teaching/learning) to that of a university (student-centered teaching/learning methods).3 Additionally, they familiarize students with basic medical sciences in an integrated manner and enable them to pursue an appropriate healthcare profession.4 In Saudi Arabia, where English is not a native language and the medium of primary and high school education is the local language, offering such preparatory programs is an essential part of Bachelor’s programs.
The College of Science and Health Professions (COSHP) at King Saud bin Abdulaziz University for Health Sciences (KSAU-HS), Riyadh, Saudi Arabia, offers the University Pre-Professional Program (UPPP) to high school graduates before they pursue bachelor degree programs. The UPPP aims to provide these students with the necessary knowledge, skills, and expertise required to succeed in their prospective professional courses. In the UPPP, over the course of four semesters (two academic years), the students take multiple courses related to the English language, basic sciences, and basic medical sciences (Table 1). English language courses main objective is to prepare students for studying all subjects in an English medium while basic sciences (eg chemistry and biology) and basic medical sciences (eg anatomy and pharmacology) courses aim to consolidate and enhance the students’ prior knowledge and introduce them to the fundamental medical concepts necessary for pursuing higher-level education in the health sciences.5 Another critical role that the UPPP plays is shifting the students’ learning habits from passive didactic learning to student-centered learning approaches. In student-centered learning approach, students take the majority of the responsibility for their learning and proactively participate in teaching.6–10
 |
Table 1 Courses Offered in the UPPP at COSHP |
Upon completing the first year of the UPPP, students enter a matching process to be allocated to their desired colleges based on their cumulative Grade Point Average (GPA) of the first two semesters. From the third semester, each student will join a particular pre-professional group, the pre-medical (PMED), the pre-dental (PDNT), the pre-pharmacy (PPHR), the pre-applied medical sciences (PAMS), and the pre-health informatics (PHIS). During the second year of the UPPP, students will continue taking the remaining English language courses; however, the focus of the second year, especially semester-4, is more towards the basic sciences and basic medical sciences courses. After completing the second year of the UPPP, students will proceed with their undergraduate programs in their respective colleges.
Similar to KSAU-HS, many other universities in Saudi Arabia, such as King Abdulaziz University, Alfaisal University, King Faisal University of Petroleum, and Batterjee Medical College, offer preparatory courses to enhance the English language and Science skills of newcomers in graduate programs. The main objectives of these preparatory programs are to enable students to continue their education in the English medium and strengthen their knowledge in related science disciplines.11–14 However, in contrast to our study, Aldarmahi (2022) conducted a recent study in Saudi Arabia and did not find an effective impact of preparatory programs on students in healthcare professions colleges.3
College of Medicine (COM) at KSAU-HS in its professional program offers an integrated Problem-Based Learning (PBL) curriculum. The PBL sessions and the Patient & Doctor sessions are central features of the educational process in the first 2 years at COM. All other teaching strategies (conceptual lectures, practicals, images, models, slides, museum, and dissected specimens) revolve around themes.15,16 The COM curriculum is organized in three phases. The first phase is the UPPP conducted in COSHP and is a transitional phase to prepare students and adjust their learning habits.6 The second, pre-clinical phase (basic science), and the third, clinical phase, are conducted in the COM.15
Before starting the second and third phases in the COM and commencing with PBL sessions, students are introduced to the topic of PBL and many other related concepts within the Health Professions Education (HPE) course in the UPPP. The HPE course teaches students about group dynamics and behavior principles, PBL, and Case-Based Learning (CBL) processes. Students also learn about effective leadership skills, presentation and delivery skills, basics of research, and literature review. Furthermore, they become familiar with E-learning, the relationship between cognitive skills and behavior in the health environment. Also, the Anatomy & Physiology course introduces students to 3–5 CBL sessions aimed to familiarize them with such learning approach.
This study aims to evaluate the effectiveness of the UPPP in preparing students to become self-learners and in shifting their learning style from teacher-centered to student-centered approaches. Furthermore, the study also aims to seek students’ perceptions of student-centered teaching/learning methods.
Materials and Methods
Study Design and Participants
This is a quantitative quasi-experimental study that used a pre and post-test survey. A questionnaire was used to collect data from all pre-professional health science students (male and female) in the COSHP who were enrolled in semester-4 of the UPPP. The study was conducted in two stages; the first stage was at the beginning of semester-4, and the second stage was after the students completed the UPPP. This research project was approved by the Institutional Review Board (IRB) of King Abdullah International Medical Research Center (study no.RC20/071/R vide approval memo ref no IRBC/0367/20). This study was conducted following the international guidelines for human studies.17 At the time of data collection, every participant gave their consent.
Estimated Sample Size
The total number of students enrolled before and after semester-4 of the UPPP was 907 and 881, respectively. All enrolled students were invited to participate in the study. The students re-taking the semester-4 were excluded afterward. The sample size 263 was determined using formula suggested by Daniel.18 A simple random sampling given the standard variable of the normal distribution corresponding to 95% confidence level (z = 1.96), the anticipated population proportion of knowledge (P = 0.5), the absolute statistical precision on either side of the anticipated population proportion (e = 0.05). Based on the population of students registered in UPPP before and after semester 4, a sample of 270 and 268 respondents were needed for before and after semester analysis. This study collected the data of 431 and 270 respondents before and after semester-4.
Development of the Questionnaire
A self-developed questionnaire was used to collect the data. The questionnaire was validated by face validity from biostatistics, health professions experts, and some participants. A pilot study was carried out on 10% of the total expected responses to check for the clarity of the questions and calculate Cronbach’s alpha for reliability. Some wordings of the questionnaire items were modified to make items unambiguous according to the feedback from the pilot testing. A language expert checked the Arabic translation. The questionnaire consisted of three parts: Part 1 focused on the demographic characteristics of the students and their family backgrounds. Part 2 assessed students’ knowledge about student-centered learning methods, PBL, CBL, and Self-Directed Learning (SDL), before and after the completion of semester-4. This part included 24 statements with “Yes”, “No”, and “Don’t know” options. Part 3 assessed students’ perception of the curriculum, teaching approaches, and available facilities after completing semester-4. This part of the questionnaire consisted of 18 items with “Don’t agree”, “Agree”, “Strongly agree”, and “Don’t know” options.
Data Collection
The questionnaire (Supplementary Material) and a consent form explaining the research purpose were distributed to the targeted students, and the confidentiality of their responses was assured. During the first stage of the study, the questionnaire was distributed using an online link given to students through a QR code that was displayed in the lecture halls. Similarly, the data in the second stage were also collected online, but this time via a link shared on WhatsApp group chats due to the pandemic. In both phases, members of the research team were available to answer all student queries about the research.
Data Analysis
The data were analyzed using the software SPSS IBM V27. The survey comprises 42 items related to the UPPP curriculum, content, and delivery. Initial 24 items were included in both pre and post-semester-4 surveys, while the last 18 items were only included in the post-semester-4 survey. These items were factor analyzed using a principal component with Varimax (orthogonal) rotation. The analysis yielded four factors for each pre-semester-4 course stage I and post-semester-4 course stage II surveys, explaining 43.08% and 49.20% respectively of the variables for the entire set of variables. The scores of different survey items factoring together were merged for further analysis. Most of the data were normally distributed and met the assumption for employing the appropriate statistical tests.
Results
The survey was sent to 907 eligible students enrolled before and 881 after semester-4 in the UPPP program. A total of 431 (47.51%) and 270 (30.64%) students responded to the survey at stages 1 and 2 of the study conducted before and after semester-4, respectively. Table 2 shows the demographics of the respondents. The majority of the respondents were males (60.3%). The age difference between the two genders was insignificant (t = 0.45, df = 699, p = 0.65). Most of the participants were enrolled in PMED group (42.5%), and the least were in Pre-Health Informatics (PHIS) group (2.7%).
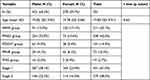 |
Table 2 Demographics of the Respondents |
Factor analysis of the survey identified four different response factors in each pre and post-semester-4 course. For pre-semester-4, the following factors were identified: Learning in PBL, PBL dynamics, CBL and SDL dynamics, and the role of the facilitator in PBL (Table 3). For post-semester-4, the following four factors were identified: Learning support, satisfaction with assessment and course, perception of HPE course, and resources for learning basic sciences and developing new skills. The mean scores with standard deviation (SD) of four factors, considered as latent variables, in pre and post-semester-4 stages, ie, stage 1 and stage 2, were compared. A statistically significant difference exists between students in stage 1 and stage 2 of the study. After attending semester-4, the students have shown an increased understanding of UPPP curriculum delivery, including PBL, CBL, and SDL, learning and dynamics of these strategies, and the role of facilitators in the curriculum.
 |
Table 3 Comparison of Latent Variables Found by Factor Analysis of the Pre and Post-Semester-4 |
Table 4 shows the students’ perception of the UPPP curriculum. Students enrolled in different courses had significantly different perceptions of the UPPP curriculum except for “learning in PBL”. Among the five student groups, the PMED group showed lower mean scores than students in other groups. To highlight the difference between students enrolled in different courses, the two largest groups, PAMS and PMED, are reported in a separate column (Table 4). These two groups consistently showed a significant difference in their mean scores.
 |
Table 4 Students Perception About PBL, CBL, SDL (UPPP Curriculum) |
To further investigate the students’ perception of basic medical science courses in the UPPP, additional items were added to the stage 2 survey. Table 5 shows the mean scores of students on different variables reflecting the understanding of basic medical sciences courses. Regarding the perception of basic medical sciences courses, students of PPHR and PHIS courses generally showed a lower understanding, as indicated by lower scores on UPPP course delivery and support. However, the only significant difference among students of various groups was their satisfaction with the assessment. The PAMS and PPHR group students were less satisfied than PMED and PDENT students.
 |
Table 5 Comparison of Latent Variables Found by Factor Analysis of the Post-Semester-4 Course Survey Among Different Student Groups |
Discussion
The preparatory programs in the educational institutes help to alleviate the barriers for school graduates seeking entry in health sciences professions.2 On the other hand, increased stress levels have been observed among students in such programs.19 COSHP offers the UPPP to all newly enrolled students in KSAU-HS. The curriculum in the UPPP is based on traditional learning/teaching strategies, with the additional courses and learning strategies related to the modern curriculum that students will be exposed to in their professional colleges. Any change in curriculum delivery from traditional to modern methods needs alteration in the pre-clinical phase, including content, teaching methodology, and assessment.20 In this study, we aimed to evaluate the effectiveness of the UPPP in preparing students to become self-learners and investigate the students’ perceptions about student-centered teaching/learning methods.
At COSHP, though male and female students are separated into different buildings, they experience the same curriculum, teaching strategies, and assessment tools. In this study, the response rate from the groups was different. The possible reasons for the higher response rate from male PMED and PAMS groups (Table 2) could be the greater number of seats available for male candidates for PMED and PAMS groups than other groups in the UPPP. Additionally, similar to the medical students,21 the PMED students in the UPPP are usually more motivated to participate in research activities.
The stage 2 of this study showed that the UPPP positively impacts students’ understanding of the PBL, CBL, and SDL, learning and dynamics strategies, and the role of lecturers in curriculum delivery (Table 3). In contrast to a recent study conducted in the Saudi Arabia, the students’ responses in this study reflected that after attending semester-4, their knowledge of the basics of student-centered teaching and learning strategies has increased.3 So, it will not be a new strategy for them when they practically practice the PBL at COM.
All the students’ groups in stage 2 of the study had almost a uniform understanding of learning in PBL; however, some students’ groups had a different perception about the dynamics of PBL, CBL, and SDL, and the role of lecturers in PBL. The SDL sessions are allocated for all groups; whereas CBL sessions are only conducted with PMED, PDNT, and PPHR groups, which could be a reason for the differences in perception. Generally, the lower mean scores of the PMED students compared to other groups indicate a critical approach of PMED students to the questionnaire. Similar to the observation of Campos-Sanchez et al,22 in this study, PMED students have higher GPAs and comparatively more motivated attitudes towards teaching, learning, and research activities than other students.
In the UPPP courses at COSHP, KSAU-HS, most PAMS, PPHR, and PHIS students do not usually achieve higher grades, and their motivation level for different learning activities is also lower.23 Though the university provides equal learning facilities and the same learning environment to all groups, the differences in their perception of the UPPP could be because of their previous academic background and lesser level of motivation. The lower mean scores of the PMED group compared to other students’ groups could be attributed to their higher level of critical analysis of UPPP courses, curriculum, and teaching strategies like PBL. The PMED and PAMS are two large groups; their merit-wise selection in the programs is from highest to lowest levels, respectively; hence, these two groups consistently showed a significant difference in mean scores (Table 4).
In Saudi Arabia, primary education is delivered in the native language in most public sector schools.24 The students face difficulties when teaching/learning medium changes from their native language to another language like English, as in the COSHP. The UPPP has three dedicated semesters, out of the four (Table 1), for teaching mainly the English language. Despite that, weaknesses in communication in English language are still observed among the students, especially PPHR, PHIS, and PAMS groups. So, the language barrier could also be a reason for the lower understanding of basic medical sciences and lower level of satisfaction by the PPHR, PHIS, and PAMS groups. The PMED group students are more fluent in English and interactive in the learning activities, and their academic performances and achievements are also better. Some PMED students also have international schooling backgrounds where the teaching medium is English, which is also advantageous.
Conclusion
The UPPP improved students’ understanding of student-centered teaching and learning approaches, especially the PBL. Thus, UPPP helps students shift their teaching/learning habits from didactic to student-centered moderns learning approaches. Variation among different students’ groups could be attributed to their previous academic background and change in learning medium to English. This study suggests that preparatory teaching programs like UPPP are helpful for students interested in joining the bachelor’s programs in countries like Saudi Arabia where English is not a native language. Moreover, the initial schooling in English medium or inclusion of English language as a major subject in school courses will help Saudi students pursue their professional careers in medicine and other professional programs with more ease. To strengthen our findings, further studies should be conducted to evaluate the effectiveness of UPPP. This can be achieved by comparing the characteristics and performance of students who underwent UPPP with those who did not undergo the procedure.
Acknowledgments
The authors thank Nabeel Qamar, Lecturer anatomy at College of Science and Health Professions, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia, for his assistance in formatting the tables and reviewing the text.
Funding
The work was not supported by any funding agency.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lewis CL. A state university’s model program to increase the number of its disadvantaged students who matriculate into health professions schools. Acad Med. 1996;71(10):1050–1057. doi:10.1097/00001888-199610000-00010
2. Patel SI, Rodríguez P, Gonzales RJ. The implementation of an innovative high school mentoring program designed to enhance diversity and provide a pathway for future careers in healthcare related fields. J Racial Ethn Health Disparities. 2015;2(3):395–402. doi:10.1007/s40615-015-0086-y
3. Aldarmahi A, Al-Rabia M, Alserhani F, et al. Impact of a preparatory year programme on the students of health professions education colleges: perception of students and faculty members. Sultan Qaboos Univ Med J. 2022;22(1):65–73. doi:10.18295/squmj.5.2021.094
4. Adelman C The toolbox revisited: paths to degree completion from high school through college. Available from: http://www2.ed.gov/rschstat/research/pubs/toolboxrevisit/toolbox.pdf.
5. Memon I, Alkushi A, Shewar DE, Anjum I, Feroz Z. Approaches used for teaching anatomy and physiology in the university pre-professional program at King Saud bin Abdulaziz University for Health Sciences. Adv Physiol Educ. 2020;44(2):188–191. doi:10.1152/advan.00167.2019
6. Funk PE, Knott P, Burdick L, Roberts M. Development of a novel pathways program for pre-health students by a private four-year university and a private health professions university. J Physician Assist Educ. 2018;29(3):150–153. doi:10.1097/JPA.0000000000000218
7. Lockspeiser TM, O’Sullivan P, Teherani A, Muller J. Understanding the experience of being taught by peers: the value of social and cognitive congruence. Adv Health Sci Educ Theory Pract. 2008;13(3):361–372. doi:10.1007/s10459-006-9049-8
8. Rodrigues J, Sengupta A, Mitchell A, et al. The Southeast Scotland Foundation Doctor Teaching Programme--is “near-peer” teaching feasible, efficacious and sustainable on a regional scale? Med Teach. 2009;31(2):e51–7. doi:10.1080/01421590802520915
9. Thomas JS, Hashim Z, Fahim N. Foundation doctor-led clinical teaching: a new innovation in the undergraduate curriculum. Int J Collab Res Intern Med Public Health. 2012;4(12):2065–2074.
10. Jacobs JCG, Wilschut J, van der Vleuten C, Scheele F, Croiset G, Kusurkar RA. An international study on teachers’ conceptions of learning and teaching and corresponding teacher profiles. Med Teach. 2020;42(9):1000–1004. doi:10.1080/0142159x.2020.1772465
11. University preparatory program. Available from: https://cos.alfaisal.edu/en/upp.
12. Preparatory year program. Available from: http://www.kfupm.edu.sa/departments/pyp/default.aspx.
13. Preparatory year English language program. Available from: https://eli.kau.edu.sa/Pages-preparatory-year-program-en.aspx.
14. Preparatory year. Available from: https://bmc.edu.sa/Academics/Preparatory-Year.
15. Academics, Phase II. Available from: https://www.ksau-hs.edu.sa/English/Colleges/com/Riyadh/Pages/Academics/Medical%20Program/PhaseII.aspx.
16. Abed SS, Al-Mansour M, Ahmed SN, et al. Evaluation of problem-based learning in college of medicine: an indicator of quality education in a hybrid curriculum. Educ Res Int. 2023:9. Article ID 9955409. doi:10.1155/2023/9955409
17. Kottow Lang MH. Critical analysis of the Council for International Organizations of Medical Sciences 2016 International Guidelines for health-related research involving humans. Medwave. 2017;17(4):e6956. doi:10.5867/medwave.2017.04.6956
18. Daniel WW. Biostatistics: A Foundation for Analysis in the Health Sciences.
19. Alsulami S, Al Omar Z, Binnwejim MS, et al. Perception of academic stress among health science preparatory program students in two Saudi universities. Adv Med Educ Pract. 2018;9:159. doi:10.2147/amep.s143151
20. Marinović D, Hren D, Sambunjak D, et al. Transition from longitudinal to block structure of preclinical courses: outcomes and experiences. Croat Med J. 2009;50(5):492–506. doi:10.3325/cmj.2009.50.492
21. Tempski P, Arantes-Costa FM, Kobayasi R, et al. Medical students’ perceptions and motivations during the COVID-19 pandemic. PLoS One. 2021;16(3):e0248627. doi:10.1371/journal.pone.0248627
22. Campos-Sánchez A, López-Núñez JA, Carriel V, Martín-Piedra MÁ, Sola T, Alaminos M. Motivational component profiles in university students learning histology: a comparative study between genders and different health science curricula. BMC Med Educ. 2014;14(1):1–3. doi:10.1186/1472-6920-14-46
23. Memon I, Feroz Z, Alkushi A, Qamar N, Ismail F. Switching from face-to-face to an online teaching strategy: how anatomy and physiology teaching transformed post-COVID-19 for a university preprofessional program. Adv Physiol Educ. 2021;45(3):481–485. doi:10.1152/advan.00233.2020
24. Ashraf TA. Teaching English as a foreign language in Saudi Arabia: struggles and strategies. IJELE. 2018;6(1):133–154. doi:10.5296/ijele.v6i1.13148
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
