Back to Journals » Journal of Pain Research » Volume 17
Update on Treating Painful Diabetic Peripheral Neuropathy: A Review of Current US Guidelines with a Focus on the Most Recently Approved Management Options
Authors Mallick-Searle T , Adler JA
Received 29 September 2023
Accepted for publication 26 February 2024
Published 13 March 2024 Volume 2024:17 Pages 1005—1028
DOI https://doi.org/10.2147/JPR.S442595
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Michael A Ueberall
Theresa Mallick-Searle,1,* Jeremy A Adler2,*
1Division Pain Medicine, Stanford Health Care, Redwood City, CA, USA; 2Pacific Pain Medicine Consultants, Encinitas, CA, USA
*These authors contributed equally to this work
Correspondence: Jeremy A Adler, Pacific Pain Medicine Consultants, 477 N El Camino Real, Suite B301, Encinitas, CA, 92024, USA, Tel +1 760 753 1104, Fax +1 760 943 6494, Email [email protected]
Abstract: Painful diabetic peripheral neuropathy (DPN) is a highly prevalent and disabling complication of diabetes that is often misdiagnosed and undertreated. The management of painful DPN involves treating its underlying cause via lifestyle modifications and intensive glucose control, targeting its pathogenesis, and providing symptomatic pain relief, thereby improving patient function and health-related quality of life. Four pharmacologic options are currently approved by the US Food and Drug Administration (FDA) to treat painful DPN. These include three oral medications (duloxetine, pregabalin, and tapentadol extended release) and one topical agent (capsaicin 8% topical system). More recently, the FDA approved several spinal cord stimulation (SCS) devices to treat refractory painful DPN. Although not FDA-approved specifically to treat painful DPN, tricyclic antidepressants, serotonin/norepinephrine reuptake inhibitors, gabapentinoids, and sodium channel blockers are common first-line oral options in clinical practice. Other strategies may be used as part of individualized comprehensive pain management plans. This article provides an overview of the most recent US guidelines for managing painful DPN, with a focus on the two most recently approved treatment options (SCS and capsaicin 8% topical system), as well as evidence for using FDA-approved and guideline-supported drugs and devices. Also discussed are unmet needs for this patient population, and evidence for potential future treatments for painful DPN, including drugs with novel mechanisms of action, electrical stimulation devices, and nutraceuticals.
Keywords: neuropathic, pain, painful diabetic peripheral neuropathy, treatment, guidelines, diabetic nerve pain
Introduction
Diabetic peripheral neuropathy (DPN) is among the most common complications of type 1 diabetes (T1D) and type 2 diabetes (T2D)1,2 in the United States (US), approximately 37 million individuals have diabetes, predominantly (90–95%) T2D, with an additional 96 million adults having prediabetes.3 An estimated 50% of diabetic patients and 10‒30% of prediabetic patients will develop neuropathy.4,5 Neuropathy is accompanied by pain in approximately 20–40% of afflicted patients, many of whom continue to have unresolved pain even with treatment.2,6–10 Diabetic neuropathic pain is associated with a high prevalence of anxiety, depression and sleep disorders which can amplify the disease burden and increase the complexity of management,11 particularly with respect to treatment selection and potential for drug–drug interactions (DDIs) and adverse drug reactions (ADRs) in the presence of polypharmacy.
Major risk factors for DPN are hyperglycemia in T1D and metabolic syndrome in T2D.12 Although glycemic control helps to prevent DPN in patients with T1D, it provides modest or no benefits in preventing DPN in patients with T2D, likely due to the presence of co-morbidities.12 The development of painful DPN has been associated with numerous factors including poorly controlled glucose levels, worsening glucose tolerance, T2D (relative to T1D), insulin resistance, tobacco smoking, excessive alcohol consumption, advanced age and duration of diabetes, diabetic vessel disease, abdominal obesity, hypertension, elevated triglyceride levels, and low high-density lipoprotein levels.8,10
Typically, DPN presents initially as distal neuropathy without pain in the feet, followed by a gradual and symmetric progression of predominantly sensory symptoms including, paradoxically, numbness with exquisite sensitivity, allodynia and hyperalgesia.6,13,14 Neuropathy symptoms arise from damage to the peripheral sensory nerves, accompanied by a gradual decrease in epidermal nerve fiber density, resulting in a worsening of sensory loss and an increase in responsiveness to painful stimuli.15 The pathophysiological processes involved in the development of painful DPN are complex and appear to involve sustained hyperglycemia, dyslipidemia, and altered insulin signaling.8,16 These lead to several possible pathological alterations (eg, DNA and macrophage activation damage, endoplasmic reticulum stress, mitochondrial dysfunction, neurodegeneration, and loss of neurotrophic signaling) in neurons and other cells critical to normal functioning. Disruptions to the intracellular processes of neurons, some of which are directly related to the effects of the metabolic syndrome, may lead to nerve dysfunction and, ultimately, neuropathy.8
The pathogenesis of pain related to DPN is not fully understood, although several theories have been proposed.17 These include changes in blood vessels that supply the peripheral nerves; metabolic and autoimmune disorders accompanied by glial cell activation; alterations in sodium and calcium channel expression; and, more recently, central pain mechanisms, such as increased thalamic vascularity and imbalance of the facilitatory/inhibitory descending pathways.17
The management of painful DPN involves treating the underlying causes via lifestyle modifications and pharmacological control of risk factors, targeting its pathogenesis, and providing symptomatic pain relief, thereby improving patient function and health-related quality of life (HR-QoL).8–10,18–24 Despite the substantial morbidity of painful DPN, its negative impact on HR-QoL, and immense healthcare burden, the condition is often misdiagnosed and inadequately treated.8,14,25
Since 2020, the US Food and Drug Administration (FDA) has approved two novel options to manage painful DPN, namely the capsaicin 8% topical system and spinal cord stimulation devices. As such, we considered it timely to examine the evidence supporting the use of these newer options and their positioning within current US guidelines. We also present evidence for three FDA-approved oral pharmacological treatments and other guideline-supported oral treatments commonly used as first-line options in clinical practice; explore potential future options to manage painful DPN; and discuss the unmet needs of this increasingly complex and rapidly growing patient population.
Guidelines for Managing Painful Diabetic Peripheral Neuropathy (DPN)
The management of painful DPN involves controlling the underlying diabetic condition and symptomatically treating the associated pain, as recommended in multiple clinical practice guidelines and expert reviews.8–10,18–24,26–29 Given their influence and importance in determining recommendations in other relevant expert opinions and reviews,8–10,22–24,28,29 we have focused on evidence-based guidelines and recommended treatment algorithms from the following US organizations:
- American Academy of Neurology (AAN): Published in December 2021, the Oral and Topical Treatment of Painful Diabetic Neuropathy: Practice Guideline Update Summary18 provides updated recommendations on the treatment of painful DPN. Graded recommendations for the use of numerous drug classes and individual agents are based on a systematic and statistical analysis of the results of 133 relevant peer-reviewed randomized, controlled trials (RCTs).
- American Diabetes Association (ADA): Three publications guiding the treatment of painful DPN are available from the ADA. Diabetic Neuropathy: A Position Statement19 was published in 2017 and provides graded recommendations on all aspects of DPN management—including prevention, diagnosis, and treatment—based on several technical reviews and associated supporting references. The clinical compendium on the Diagnosis and Treatment of Painful Diabetic Peripheral Neuropathy20 and Standards of Medical Care in Diabetes‒202226,27 were published in 2022. The clinical compendium focuses on the screening, diagnosis and treatment of painful DPN in routine clinical practice, and summarizes the latest guidance on effective therapies, including pharmacological agents, nutraceutical products, and non-pharmacological therapies.20 Guidance on treating painful DPN is also provided in Chapter 12: Retinopathy, Neuropathy, and Foot Care27 of the updated Standard of Medical Care in Diabetes ‒2022.26
- American Association of Clinical Endocrinology (AACE). Published in 2022, the AACE Clinical Practice Guideline: Developing a Diabetes Mellitus Comprehensive Care Plan‒2022 Update21 provides graded recommendations for the care of diabetic patients, including diagnosis and management of DPN, based on a comprehensive search and appraisal of the current literature.
Several other international and national clinical practice guidelines on the management of neuropathy are available, including those from the Neuropathic Pain Special Interest Group of the International Association for the Study of Pain,30,31 the European Federation of Neurological Societies,32 the European Association for the Study of Diabetes,33 the UK National Institute for Health and Care Excellence,34 the Canadian Pain Society,35 the German Society for Neurology,36 and the German National Disease Management Guideline for Diabetic Neuropathy.37 However, in light of their publication date (before 2016)30–35,37 and/or focus on the management of neuropathic pain in general,30,32,34–36 any guidance specific to painful DPN may be incomplete, especially as it relates to newer treatment options.
Key AAN, ADA, and AACE recommendations for managing painful DPN are summarized in Table 1.18–21 All three organizations advocate a customized stepwise approach, with the choice of pharmacological agent guided by factors such as comorbidities, cost, and potential for DDIs and ADRs.18–21
 |
Table 1 Summary of Current American Academy of Neurology,18 American Diabetes Association,19,20 and American Association of Clinical Endocrinology21 Guidelines for the Management of Diabetic Peripheral Neuropathy |
Guideline-recommended (although not necessarily FDA-approved) first-line oral options to treat painful DPN include tricyclic antidepressants (TCAs), gabapentinoids, and serotonin-norepinephrine reuptake inhibitors (SNRIs); the AAN guideline also includes sodium channel blockers.18 Based on the results of a meta-analysis of Class I and II trials showing comparable estimated effect sizes, the AAN states that it is difficult to recommend any one drug class over another.18 Later-line therapy involves switching first-line agents or using combinations of pharmacological agents from different classes or pharmacological plus non-pharmacological options.18,20,21
Capsaicin 8% topical system, the only FDA approved non-oral pharmaceutical to treat painful DPN, is a first-line treatment option in the AACE guidelines21 and is recommended in the ADA compendium.20 The German Diabetes Association (Deutsche Diabetes Gesellschaft, DDG) also positions capsaicin 8% topical system as a first-line treatment for painful DPN,22 whereas an international expert consensus group considers it a third line analgesic treatment for painful DPN in clinical practice.29
FDA-Approved Treatments for Painful DPN
Five treatments are currently approved by the FDA to treat painful DPN based on their efficacy and safety in RCTs in this patient population. These include three oral medications (duloxetine, pregabalin, and tapentadol extended release [ER]); one topical agent (capsaicin 8% topical system); and low- and high-frequency spinal cord stimulation (SCS) devices indicated for the treatment of chronic intractable painful DPN, which is defined as constant moderate to severe pain that has no known cure and requires daily medical treatment.
Table 2 summarizes the year of approval, indication, contraindications, and most common adverse events reported with the use of FDA-approved options to treat DPN.38–44 Although pain-related endpoints among RCTs differed to some extent, all treatments were associated with significant improvements from baseline in pain scores relative to placebo or standard therapy, as well as increases in the proportion of patients achieving a clinically meaningful pain response (ie, a ≥30% or ≥50% improvement in pain score).
 |
Table 2 Current FDA-Approved Options for the Management of Painful Diabetic Peripheral Neuropathy (Trade name; Year of FDA Approval for Painful DPN) |
In reverse chronological order of their FDA approval, the efficacy and safety of these treatments in their pivotal RCTs are examined, with emphasis on the two most recently approved options (ie, SCS devices and the capsaicin 8% topical system).
Spinal Cord Stimulation (SCS) for Intractable Painful DPN
SCS therapy involves placing wire leads within the epidural space of the spinal canal accompanied by implantation of an internal pulse generator device in the superficial tissue, usually the back or buttock.38,39 SCS requires minor outpatient surgery and, for decades, has been a component of the management of intractable pain of the torso and limbs. Use in painful DPN was only recently added to its indications. Conventional tonic SCS devices use low-frequency (40–100 Hz) SCS to induce paresthesia in painful anatomic regions.45 High-frequency (10 kHz) SCS induces minimal to no paresthesia and is thought to act by modulating axonal activity in the superficial dorsal horn, thereby regulating chronic pain pathways.45
In 2022, the FDA approved the Medtronic Vanta™ and Intellis™ implantable neurostimulation systems to aid in the management of chronic intractable unilateral or bilateral pain of the lower limbs associated with DPN (Table 2).38 These devices have options to personalize patient therapy and allow patients to adjust the intensity of the electric current as required.38 The Vanta™ SCS device provides low-frequency SCS and does not require recharging (the battery is estimated to last 11 years). The Intellis™ SCS device provides high-frequency SCS and is transcutaneously recharged within 1 hour using a recharge antenna.
Nevro’s Senza®, Senza II™ and Senza Omnia™ neuromodulation systems were approved in 2021 to treat chronic intractable unilateral or bilateral pain of the lower limbs associated with DPN (Table 2).39 When used in this indication, the devices are preprogrammed to deliver high-frequency (10 kHz) paresthesia-free electrical pulses.39 The batteries in the devices are transcutaneously recharged using hand-held portable chargers, via a schedule that fits with the patient’s lifestyle and maintains a sufficient charge to deliver the desired level of stimulation. The battery has an expected life of at least 10 years using a typical 10 kHz program stimulation setting.39
Before implantation of SCS devices, patients undergo trial stimulation for approximately 1 week to determine whether implantation is appropriate.38,39 If pain relief, functional enhancement, and tolerability goals are satisfied, a complete SCS system (neurostimulator and leads) is implanted. Adverse events are generally associated with the implantation procedure (Table 2). Although the minimally invasive implantation procedure is usually well tolerated, adverse events and complications, such as wound-related issues, may be more frequent and severe in diabetic patients, especially those with poor glucose control.38,39
At the time of manuscript development, SCS devices manufactured by Nevro and Medtronic were approved for painful DPN, but the authors have since become aware of FDA approval of devices from Abbott (Proclaim™ Plus and Proclaim™ XR) and Boston Scientific (WaveWriter Alpha™). As this therapeutic area is evolving rapidly, we might anticipate the approval of more devices in future.
Evidence for the Efficacy of SCS in Refractory Painful DPN
FDA approvals of the Medtronic and Nevro SCS devices were based on the results of three open-label multicenter RCTs of low-frequency46,47 or high-frequency48 SCS. To be eligible for enrollment in these RCTs, patients were required to have painful DPN for ≥1 year that was refractory to conventional pharmacological therapy.46–48 Patients were randomized to receive open-label SCS treatment plus best/conventional medical management (CMM) or CMM alone for 6 months. Patients in the SCS plus CMM group underwent temporary trial stimulation for 5–7 days, and those who achieved a ≥50% pain reduction were eligible for device implantation.
According to an analysis conducted by Medtronic, low-frequency SCS46,47 and high-frequency SCS48 had similar adjusted ≥50% responder rates (55% vs 55%).49 The findings are supported by results from a recent network meta-analysis of SCS RCTs for painful DPN.50 In addition, a systematic review and meta-analysis of individual patient and aggregate data showed that SCS is an effective therapeutic adjunct to best medical therapy in reducing pain intensity and improving HR-QoL in patients with painful DPN.51
Low-Frequency SCS
In the larger (n = 60) of two clinical trials of low-frequency SCS for intractable painful DPN, trial stimulation was successful (ie, ≥50% pain reduction) in 93% of the low-frequency SCS plus CMM group.46 This group had a significant reduction in mean visual analog score (VAS) scores at 6 months (from 7.3 cm at baseline to 3.1 cm at 6 months; p < 0.001), as well as improvements in other pain and HR-QoL outcomes. In contrast, the CMM group had no improvements in any outcomes. Significantly more patients in the low-frequency SCS plus CMM group than in the CMM group achieved ≥50% pain relief (60% vs 5%; p < 0.001). No patients required device removal due to adverse events.
Similar results were shown in the smaller (n = 36) of the two RCTs, in which trial stimulation was successful in 77% of patients.47 At 6 months, 59% of low-frequency SCS plus CMM versus 7% of CMM alone recipients achieved treatment success, which was defined as ≥50% pain relief during daytime or nighttime or “much improved” or “very much improved” on Patient Global Impression of Change (PGIC) pain and sleep scores. In terms of safety, one case of fatal subdural hematoma due to dural puncture during trial lead implantation, and one infection of the SCS system that required removal of the device 6 weeks after implantation occurred.
Patients with DPN have been shown to gain significant long-term pain relief with low-frequency SCS plus CMM. In a 5-year follow-up of 48 patients enrolled in two identically designed studies,47,52 86% of patients achieved treatment success at 1 year, a rate that slowly decreased each year to 55% at 5 years.53 Kaplan–Meier survival analysis indicated that 80% of the patients were still using their SCS device after 5 years. One patient required removal of the device 8 months after implantation due to a chronic infection of the SCS system.53 More recently, an 8- to 10-year follow-up study of 19 patients with painful DPN who continued to use SCS treatment after at least 8 years reported that pain intensity, day and night, was reduced significantly compared with baseline and, for >50% of patients, the pain reduction was >30% (considered to be clinically meaningful).54
High-Frequency SCS
Approval of the high-frequency Nevro 10-kHz SCS device to treat chronic retractable DPN was based on the results of an open-label 6-month RCT, with optional crossover at 6 months.48 Patients with refractory painful DPN were randomized to receive 10-kHz SCS plus CMM (n = 113) or CMM alone (n = 103). In the 10-kHz SCS plus CMM group, 104 patients underwent temporary trial stimulation. This was successful in 98 patients (94%), with 90 patients opting to undergo permanent device implantation.
The primary endpoint (≥50% improvement from baseline in VAS pain without worsening of baseline neurological deficits at 3 months) was achieved by significantly more 10-kHz SCS plus CMM than CMM alone recipients (79% vs 5%; between-group difference [BGD] 73.6%; 95% CI 64.2–83.0; p < 0.001). At 6 months, 10-kHz SCS plus CMM was associated with significantly (p < 0.001) higher rates of patients with a ≥50% improvement in pain response (85% vs 5%), sustained pain remission (60% vs 1%), neurological improvement (62% vs 3%), and patient satisfaction (92% vs 6%) than CMM alone.48 Substantial pain relief and other benefits were maintained over 12 months with 10-kHz SCS plus CMM.55
Over a 12-month period, procedure-related infections were reported in eight patients (5.2%), leading to surgical removal of the SCS device in five patients; infections in the remaining three patients were resolved with conservative treatment.55 Stimulation-related ADRs were not reported.
Capsaicin 8% Topical System
Capsaicin is a highly selective agonist for the transient receptor potential vanilloid-1 (TRPV1) receptor, which is an ion channel-receptor complex expressed on nociceptive nerve fibers in the skin.40 The 2021 Nobel prize in Physiology or Medicine was awarded jointly to Dr. David Julius and Dr. Ardem Patapoutian for their respective groundbreaking discoveries of receptors for temperature (TRPV1 receptors) and touch (Piezo2 ion channels).56 Discovery of the TRPV1 receptor led to an understanding of its importance in pain perception. In chronic pain states, TRPV1 receptors are up-regulated on neurons, have reduced stimulation thresholds, and increase pain perception. Activation of TRPV1 receptors results in pain, burning, itching, stinging, and other physiological responses.57,58
The capsaicin 8% (179 mg) topical system (Qutenza®)40 is the only topical treatment, and the only topical formulation of capsaicin, approved by the FDA to treat adults with painful DPN of the feet. Although multiple over-The-counter (OTC) products contain capsaicin, these relatively low-concentration (0.025–0.075%) formulations are not approved to treat painful DPN. Unlike the capsaicin 8% topical system, OTC topical capsaicin products require application several times each day, leading to poor compliance, and tend to have modest efficacy and generally poor tolerability.57,58 The capsaicin 8% topical system, in contrast, provides rapid and sustained benefits due to its engineered and patented matrix delivery system, which creates a forced diffusion of high concentration capsaicin into the skin during an application period of 30 min (for painful DPN of the feet) or 60 min (for post-herpetic neuralgia), with subsequent applications at ≥3-month intervals.40,59
The capsaicin 8% topical system consists of a silicone adhesive matrix that contains a microreservoir of high-concentration capsaicin solubilized in diethylene glycol monomethyl ether (DGME) with a polyester backing and removable liner.59 During application to the feet of patients with painful DPN, capsaicin is rapidly diffused into the epidermal layers of the skin via the influx of DGME and efflux of water. During the application period, and possibly for a few days afterward, the patient may feel a hot, burning sensation with hyperalgesia.57,58,60,61 This initial reaction is triggered by activation of TRPV1 receptors on the nociceptive nerve endings and is followed by desensitization,57,60,62,63 leading to defunctionalization and ablation of epidermal nerve fibers (ENF) via a chemoneurolytic process at the application site.64–67 This ablation and reduction of ENF density is temporary and reversible. Reinnervation of the TRPV1 nerve fibers occurs over the course of several months and pain may gradually reemerge due to the continuous consequences of diabetes.40 Of note, recent evidence suggests that treatment with capsaicin 8% topical systems may have an impact beyond pain relief, including the promotion of healthy nerve regeneration (see Unmet needs in the treatment of painful DPN: Disease prevention section for details).68–71 Systemic exposure to capsaicin following application of the topical system is very transient and low, since the high-concentration capsaicin does not penetrate deep into the dermal layers of the skin.58,72 As a result, the capsaicin 8% topical system is well tolerated, with a general lack of systemic ADRs, no potential DDIs or contraindications to its use, and no requirements for dose titration or adjustments in any patients (Table 2).40 This makes the capsaicin 8% topical system particularly favorable for use in complex patient populations, such as those taking multiple medications, those with co-morbid conditions, including hepatic or renal impairment, and those in whom treatment with oral medications that increase the risk of falls and fractures is considered unsuitable.
Evidence for the Efficacy of a Single Application
In the double-blind, placebo-controlled 12-week STEP trial, adult patients with painful DPN of the feet received a single 30-min application of the capsaicin 8% topical system (n = 186) or placebo (n = 183) and were followed for 12 weeks.73
The capsaicin 8% topical system provided rapid and sustained (≥3-month) improvement in pain-related outcomes that were significantly greater relative to placebo.73 The reduction from baseline in mean numeric pain rating scale (NPRS) scores for average daily pain during weeks 2–8 (primary endpoint) was significantly greater with the capsaicin 8% topical system than with placebo (BGD –6.6%; 95% CI –12.3 to –0.8; p = 0.025); and improvement was maintained during weeks 2–12 (BGD –7.1%; 95% CI –12.9 to –1.2; p = 0.02). Significantly more patients treated with the capsaicin 8% topical system than placebo achieved a clinically meaningful ≥30% reduction in pain during weeks 2–12 (40.9% vs 31.7%; p = 0.05). Compared with placebo, capsaicin 8% topical system recipients had a shorter median time to treatment response (defined as the first of three consecutive days on which the patient reported ≥30% decrease from baseline in average daily pain score; 19 vs 72 days), modest improvements from baseline in sleep interference scores during weeks 2–8 and weeks 2–12 (p ≤ 0.03 vs placebo), and no changes in sensory perception and reflex testing.73
In the capsaicin 8% topical system group, headache (in 2.2% of patients) was the only systemic ADR reported. Application-site reactions were reported by 33.9% of patients, and no patients discontinued treatment due to ADRs.73
Evidence for Safety and Efficacy After Repeated Applications
Due to the progressive nature of diabetes, patients with DPN have reduced ENF density,15 underscoring the need to investigate the potential consequences of repeated nerve fiber ablation on peripheral nerve sensory function. The open-label PACE RCT was designed primarily to evaluate the long-term (52-week) safety of repeated applications of the capsaicin 8% topical system plus standard of care (SoC) consisting of optimized treatment with antidepressants, anticonvulsants, and/or opioids.74,75 Adult patients with painful DPN of the feet were randomized to receive the capsaicin 8% topical system applied for 30 min plus SoC (n = 156), capsaicin 8% topical system applied for 60 min plus SoC (n = 157), or SoC alone (n = 155). Results are presented for the group treated with the capsaicin 8% topical system (30 min) plus SoC, as 30 min is the application duration approved for treatment of painful DPN of the feet.
The capsaicin 8% topical system was applied 1–7 times at intervals of ≥8 weeks. The mean between-treatment interval was 68.4 days, and 53.8% of patients in the capsaicin 8% topical system 30-min group received seven applications.74
The primary endpoint was the change from baseline in Norfolk Quality of Life-Diabetic Neuropathy (QoL-DN) scores. This validated patient-reported outcome measure captures the entire impact of nerve fiber dysfunction on QoL in DPN; score reductions correspond with functional improvement.74 Repeated treatment with the capsaicin 8% topical system was not associated with any deterioration of functional or neurological sensation. Improvements from baseline in Norfolk QoL-DN scores were −27.6% with capsaicin 8% topical system 30-min plus SoC in the total group, slightly higher (−31.2%) in the subgroup which received seven applications, and lower (−6.7%) in the SoC alone group. Norfolk subscale scores (small fiber, symptoms, autonomic, physical function, activities of daily living) and Utah Early Neuropathy Scale total and sharp sensation subscale scores also improved from baseline to a greater extent with the capsaicin 8% topical system plus SoC than SoC alone. The capsaicin 8% topical system had no negative effect on sharp, warm, cold, and vibration perception and reflex function relative to SoC alone.74
Compared with SoC alone, the capsaicin 8% topical system 30-min plus SoC led to numerically greater improvements in NPRS pain scores (average daily pain, pain intensity and pain interference) and EQ-5D utility index and VAS scores, higher rates of ≥30% and ≥50% pain responses (67.3% vs 40.6% and 44.8% vs 23.8%, respectively), higher rates of being “very much, much or minimally improved” on the PGIC scale (67.3% vs 38.5%), and lower rates of new prescriptions for concomitant opioids, antidepressants and anticonvulsants (increase from baseline of 0.1‒1.3% vs 3.2‒10.9%) at week 52.75 Formal statistical testing of these secondary efficacy endpoints was not performed, as PACE was primarily a safety study.
Repeated treatment with the capsaicin 8% topical system may result in progressive improvements in pain and other outcomes. A post-hoc analysis of PACE investigated the efficacy of repeated applications of the capsaicin 8% topical system in patients who failed to achieve a ≥30% pain response following the first application.76 Among 313 recipients of the capsaicin 8% topical system (pooled 30- and 60-min application times) plus SoC, 96 (30.7%) achieved a ≥30% response following the first application. Among non-responders at 3 months, 28.1% achieved a ≥30% reduction at 6 months, increasing to 42.5% and 45.7% at 9 and 12 months, respectively. By month 12, progressive improvements in pain, sleep, QoL, and patient satisfaction achieved by slower responders were similar to those in early responders.76 According to the investigators, a progressive pattern of response in some patients after repeated applications of the capsaicin 8% topical system may arise from a “pruning” effect on abnormal nerve fibers followed by regeneration of more normal fibers and/or a gradual effect of peripheral therapy on central sensitization leading to decreased pain perception over time.76
Efficacy and Tolerability Compared with Oral Medications
A network analysis has provided indirect evidence of the relative efficacy of the capsaicin 8% topical system versus placebo and oral pregabalin, gabapentin, and duloxetine in treating painful DPN,77 as no head-to-head studies have been conducted. Twenty-five RCTs were included in an analysis of the odds of achieving a ≥30% response at 12-weeks. STEP was the only RCT of the capsaicin 8% topical system to be included.
The likelihood of achieving a ≥30% response with the capsaicin 8% topical system was significantly greater relative to placebo (odds ratio 2.28; 95% CI 1.19‒4.03), and similar to that of pregabalin, gabapentin and duloxetine (odds ratio 0.99‒1.83, with non-significant 95% CIs). Importantly, the capsaicin 8% topical system offered tolerability benefits since, unlike oral medications, it was not associated with reports of systemic ADRs such as somnolence, dizziness, nausea, diarrhea, constipation, and fatigue, or with discontinuations due to ADRs.77 The only ADR of interest was the capsaicin 8% topical system had in common with oral pregabalin, gabapentin, and duloxetine was headache. The odds ratio for headache did not differ significantly between the capsaicin 8% topical system and placebo, and the mean probability of headache was lower with the capsaicin 8% topical system than with pregabalin, gabapentin, and duloxetine (10.6% vs 83.3%, 60.4%, and 28.8%, respectively).77
Tapentadol Extended-Release Tablets
Tapentadol ER (Nucynta® ER) is a dual µ-opioid receptor agonist and norepinephrine reuptake inhibitor (Table 2),41 which was approved to treat painful DPN based on its efficacy in two 12-week RCTs.78,79 Optimized dosages of tapentadol ER 100–250 mg twice daily significantly improved pain scores and other outcomes.78,79 In a pooled analysis of these key RCTs, the mean pain intensity score of 7.29 at the beginning of the initial open-label phase decreased to 4.15 following 3 weeks of treatment.80 In the double-blind phase limited to tapentadol responders, mean pain intensity scores at week 12 were lower with tapentadol ER than with placebo (3.77 vs 4.76), indicating that pain levels remained consistent with continued use of tapentadol ER, but worsened when placebo replaced tapentadol ER. Significantly more tapentadol ER than placebo recipients had a ≥50% reduction in pain intensity (38.9% vs 28.4%) and reported that their painful DPN was “very much improved” or “much improved” using the PGIC assessment (65.5% vs 41.7%).80
Despite regulatory approval of tapentadol ER to treat painful DPN, current AAN,18 ADA,20 and AACE21 guidelines do not recommend its use due to general concerns about opioid therapy (Table 1). In addition to more common ADRs (Table 2), tapentadol is associated with several potentially serious ADRs and DDIs. According to black-box warnings required by the FDA in the US prescribing information,41 tapentadol may cause serious, life-threatening or fatal respiratory depression; is associated with a risk of addiction, abuse, and misuse that can lead to overdose and death; and may result in profound sedation, respiratory depression, coma, and death if used concomitantly with benzodiazepines or other central nervous system depressants, including alcohol.
Duloxetine Capsules
Duloxetine (Cymbalta®, Drizalma Sprinkle™, Irenka®) acts as an SNRI (Table 2).42,43 Its analgesic effects in the treatment of DPN are thought to be associated with preferential blockade of late Nav 1.7 sodium ion channels,81 with increases in norepinephrine and, to a lesser extent, serotonin and dopamine in the CNS also appearing to play a role in the inhibition of neuropathic pain.82
Approval for the use of duloxetine 60 mg once daily to treat painful DPN was based on the results of two 12-week RCTs.83,84 Relative to placebo, duloxetine 60 mg once or twice daily significantly improved mean NPRS scores by an additional 1–1.7 points. Significantly more duloxetine than placebo recipients achieved a ≥50% pain response (40–45% vs 20–22%). There were no significant differences between duloxetine 60 mg once or twice daily. Pain relief was recorded as early as the first week in some patients and persisted throughout the study duration.83,84
In addition to common ADRs (Table 2), duloxetine has been associated with potentially fatal hepatotoxicity, serotonin syndrome (when taken alone or in combination with other serotonergic agents), severe skin reactions, increased risk of bleeding, increased blood pressure, sexual dysfunction, and other potentially serious ADRs and DDIs that require caution.42,43
Pregabalin Capsules and Solution
Pregabalin (Lyrica®)44 is a gabapentinoid with a complex mechanism of action (MoA) that involves inhibiting the calcium-mediated release of various neurotransmitters at neuronal synapses, as well as other activities, including influencing affective components of pain.85
In two RCTs pivotal to its approval for treating painful DPN, patients received pregabalin 100 mg three times daily (maximum dosage) for 5 weeks86 or 8 weeks.87 Pregabalin 300 mg/day significantly improved pain scores compared with placebo (mean change from baseline in VAS score 2.5 vs 0.8 cm) and increased the proportion of ≥50% pain responders (45% vs 18%). In both trials, pain decreased in some patients during the first week, with improvements persisting throughout the study period. A meta-analysis of 11 placebo-controlled RCTs found that pregabalin was effective in the treatment of both moderate and severe DPN-related pain, with greater improvement in those with severe than moderate pain.88
In addition to common ADRs (Table 2), pregabalin is associated with a risk of angioedema leading to life-threatening respiratory compromise, hypersensitivity reactions, and an increased risk of suicidal thoughts and behaviors, as well as other warnings and precautions.44 As the misuse and abuse of pregabalin appears to be growing, its use requires caution in high-risk patients, such as those with a history of opioid abuse.89
Other Guideline-Supported First-Line Oral Options
Guideline-supported first-line oral options for the treatment of painful DPN in clinical practice include TCAs, gabapentinoids, SNRIs, and sodium channel blockers,18–21 which are considered to modulate pain.90 Table 3 summarizes the MoA and clinical efficacy of these drug classes in treating painful DPN.18–21,77,82,85,91–114
 |
Table 3 Mechanism of Action and Efficacy of Oral Pharmacological Agents Recommended as First-Line treatment18–20 in Patients with Painful Diabetic Peripheral Neuropathy |
Tricyclic Antidepressants
TCAs (eg, amitriptyline (Elavil®, Vanatrip®),92–97 nortriptyline (Aventyl®, Pamelor®),98 desipramine (Norpramin®),99 and imipramine (Tofranil®)100 are frequently used to treat painful DPN and other types of neuropathic pain. Most evidence for the efficacy of TCAs in treating painful DPN relates to the use of amitriptyline, with little evidence for other TCAs (Table 3).18,19
The well-known ADRs of TCAs (eg, gastrointestinal issues, orthostatic hypotension, dry mouth, and urinary retention) are likely due to their activity on histaminic, adrenergic, and cholinergic receptors,10 and may be problematic in patients with pre-existing constipation, urinary retention, or orthostatic hypotension.18 Nortriptyline and desipramine98,99 are generally better tolerated than amitriptyline and imipramine and may be a safer option, especially in older patients.8
Serotonin/Norepinephrine Reuptake Inhibitors
In addition to FDA-approved duloxetine, ADA18 and AAN19 guidelines also recommend venlafaxine (Effexor®)102 and desvenlafaxine (Pristiq®),101 the only active metabolite of venlafaxine, as oral options for treating painful DPN (Table 3). These SNRIs have greater selectivity for inhibiting serotonin reuptake than norepinephrine reuptake, which occurs in a dose-related and sequential manner, and weakly inhibit dopamine reuptake.115
The tolerability profiles of desvenlafaxine and venlafaxine are comparable to that of duloxetine, with nausea and dizziness being the most common ADRs.101,102 The sequential effects of SNRIs on serotonin and norepinephrine results in an initial onset of serotonergic ADRs (eg, headaches, nausea, fatigue, sexual dysfunction) followed by ADRs at higher dosages that relate to both serotonin and norepinephrine (eg, activation effects, dry mouth, night sweats).115 Venlafaxine and duloxetine are metabolized by CYP isoenzymes leading to potential DDIs, whereas desvenlafaxine bypasses such metabolism, limiting the possibility of DDIs.115
Gabapentin
Gabapentin (Neurontin®, Gabarone®), the only gabapentinoid other than pregabalin currently available in the US, is FDA approved to treat post-herpetic neuralgia116 but not DPN. Two recent formulations of gabapentin, gabapentin gastro-retentive tablets (Gralise®) and gabapentin enacarbil ER (Horizant®), are also approved to treat post-herpetic neuralgia, but not painful DPN. Nevertheless, gabapentin has shown some efficacy in treating painful DPN (Table 3).103,104 In comparison to pregabalin, gabapentin has a much lower oral bioavailability (30–60% vs 90%) and is less rapidly absorbed (time to peak plasma concentrations 1 vs 3 hours).
As with pregabalin, gabapentin requires dose titration, tapered withdrawal, lower dosages in patients with renal impairment,116 and caution with use in patients at high-risk of misuse and abuse.89 The most common ADRs with gabapentin include CNS effects, weight gain, gastrointestinal effects, and peripheral edema. Due to risk of the latter, gabapentinoids should be used cautiously in patients with peripheral edema from comorbid cardiac, renal, liver, or other diseases.18
Sodium Channel Blockers
Sodium channel blockers (eg, carbamazepine [Tegretol®, Carbatrol®, Epitol®]), oxcarbazepine (Trileptal®), lamotrigine (Lamictal®), lacosamide (Vimpat®), and valproic acid (Depakote®, Depakene®) are also recommended for the treatment of painful DPN.8–10,18 As a class, sodium channel blockers appear to be more effective in reducing pain associated with DPN than placebo based on limited evidence from generally small RCTs (Table 3).107–114
Sodium channel blockers have wide structural diversity and may block other sodium channels, such as those in the CNS and skeletal muscle. As a result, they are associated with a variety of ADRs, which differ between individual drugs depending on their specificity for certain sodium channels.117
Future Research in Painful DPN
At the heart of research into painful DPN is the need for a better understanding of the correlation between diabetes severity and its impact on painful DPN; as well as cardiometabolic risk factors for painful DPN and their link to cardiovascular mortality. Genetic studies are needed to clarify disease mechanisms which differentiate painful and non-painful DPN.2,7 The increased focus on the patient has been paralleled by research into diagnostic tests using novel biomarkers, although more effort in this area is required, and assessment of more effective therapies for symptom management and ultimately disease modification.
Drugs in Phase 2 or 3 Clinical Trials
Many drugs with novel MoAs are being evaluated for the treatment of painful DPN.118 At the time of manuscript development, drugs that had successfully completed phase 2 or 3 RCTs were VM202, a gene therapy that provided pain relief in a patient subgroup and was well tolerated;119 and NRD135S.E1, a Lyn tyrosine kinase inhibitor that showed consistent pain relief benefits and was well tolerated.120 Details are in Table 4.118–122
 |
Table 4 Drugs in Development for Painful Diabetic Peripheral Neuropathy in Completed Phase 2 or 3 Randomized Controlled Trials as Reported in the Clinicaltrials.gov Database |
Numerous other drugs are in development to treat painful DPN and under evaluation in phase 2 or 3 RCTs (Table 5).118,123–134 AT-001, an aldose reductase inhibitor, targets the pathogenesis of neuropathic pain by inhibiting glucose metabolism by the polyol pathway.123 Other agents generally target the pathogenesis, transmission, activation, or expression of neuropathic pain by blocking or binding to a specific pain-related receptor (eg, bradykinin receptor B,124 TRPV1,125 μ-opioid receptor,126 transient receptor potential melastatin 8,127 adaptor associated kinase 1,128 transient receptor potential A1,129 transforming growth factor-α,131 or tumor necrosis factor receptor-2.132 The selective histone deacetylase 6 (HDAC6) inhibitor ricolinostat acts by stabilizing the nerve supply network.133 Low-dose naltrexone acts by suppressing microglial cell activation in the CNS,134 and was shown to have similar efficacy but better tolerability than amitriptyline in a 6-week crossover trial in 67 patients with painful DPN.135 A further study comparing low-dose naltrexone with placebo is underway.118
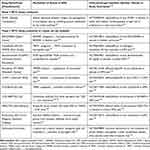 |
Table 5 Drugs in Development for Painful Diabetic Peripheral Neuropathy in Phase 2 or 3 Randomized Controlled Trials Currently Underway as Reported in the Clinicaltrials.gov Database |
Electrical Stimulation Devices
In addition to implantable SCS devices, several noninvasive electrical stimulation devices have been evaluated in RCTs in patients with painful DPN. Table 6 summarizes their effectiveness in treating painful DPN as reported in phase 3 or 4 RCTs and meta-analyses.136–139 Electrical stimulation devices are thought to produce analgesic effects in painful DPN by improving the microcirculation associated with neuropathy, thereby reducing symptoms and improving nerve function, stimulating cutaneous afferent fibers and limiting the central transmission of pain signals via nociceptive inhibition at the presynaptic level in the dorsal horn.136,140
 |
Table 6 Effectiveness of Electrical Stimulation Devices in the Treatment of Painful Diabetic Peripheral Neuropathy in Phase 3 or 4 Randomized Clinical Trials or Meta-Analyses |
To date, consistent, albeit generally small and transient, benefits have been shown only with transcutaneous electrical nerve stimulation (TENS). The use of electrical stimulation devices is generally well tolerated, without the DDIs and ADRs associated with the use of oral pharmacological treatments. Study results have been limited to small patient populations and significant effects in placebo groups.136,140
Unmet Needs in the Treatment of Painful DPN
Unmet needs with regard to the treatment of painful DPN can be categorized at three levels, which should form the basis for a personalized approach to the management of this frequently debilitating and progressive condition.10,20,141
- In the absence of any approved effective pharmacological disease-modifying therapy, preventative approaches that delay the development of nerve damage and slow disease progression would be highly beneficial. This should involve educating healthcare professionals and patients about diabetes and DPN, implementing effective targeted screening strategies as part of routine clinical practice, encouraging patients to undertake lifestyle modifications, and optimizing the use of medications. Early diagnosis and timely treatment of painful DPN is vital to prevent progression, avoid the development of advanced complications, and improve HR-QoL, economic and other outcomes.
- A vital goal should be to develop pathogenetically oriented disease-modifying treatments designed to prevent/reverse the nerve damage associated with painful DPN.
- Since approximately 30% of patients with DPN experience painful episodes, optimal approaches to minimize pain are an essential goal for a relevant proportion of patients.
Disease Prevention
To ensure that DPN is diagnosed and managed as early as possible, screening for DPN should be conducted regularly and routinely in all diabetic patients (Table 1).18–20 Healthcare professionals should be educated in patient assessment, which involves obtaining a careful clinical history and conducting a targeted physical exam. A patient-centered approach may require referral to specialists in other disciplines including but not limited to endocrinology, pain management, and podiatry. Patients should also be educated about the risk of DPN and its early signs and symptoms.
Management decisions pertaining to DPN prevention should be individualized to the patient’s needs. These include appropriate foot care and a range of initiatives to reduce DPN risk factors. To prevent the onset of DPN in patients with T1D, intensive glucose control should be implemented when possible.18–20 In patients with T2D, controlling features of the metabolic syndrome, such as hyperglycemia, hypertension and hyperlipidemia, together with educational strategies to improve lifestyle measures, including weight loss, increased physical activity, and smoking cessation, are recommended to prevent DPN. Education about lifestyle interventions is also important to prevent DPN in individuals with prediabetes/metabolic syndrome.18–20
Disease Modification
In the US, no pharmacological treatment is currently approved to modify the progression of DPN.
The loss of ENF density over time in patients with DPN is a natural consequence of disease progression and a major contributor to diabetic foot ulcers.142 Preliminary evidence suggests that the capsaicin 8% topical system may modify peripheral neuropathic pain, as it has been shown to regenerate and restore sensory nerve fibers.68–71 In a RCT assessing the mechanism of pain relief of the capsaicin 8% topical system, skin biopsies at 3 months in patients with painful DPN showed a significant increase in the density of intra-ENFs and sub-ENFs in those treated with the capsaicin 8% topical system plus SOC (n = 25) but not in those receiving SOC alone (n = 12).68 Patients with painful DPN who had pain reduction at 3 months with the capsaicin 8% topical system plus SoC (n = 18) had correlating increases in nerve fiber density, whereas non-responders without pain reduction (n = 7) did not. Importantly, the increase in ENF density did not correlate with an increase in pain, suggesting that nerve fibers were restored in a healthier state compared with baseline. Although the increases in vasodilation and improvements in warm perception sensory testing observed with the capsaicin 8% topical system require further investigation, they may signal restoration of sensory function which, in turn, can lead to improvement in the overall health of the diabetic foot.68 In similar exploratory studies, patients with peripheral neuropathic pain (n = 23),69 painful chemotherapy-induced peripheral neuropathy (CIPN; n = 16),70 or non-freezing cold injury (n = 16),71 were treated with a single application of the capsaicin 8% topical system. Heat-evoked neurogenic vasodilatation showed improvement in half of the patients with peripheral neuropathic pain 4 weeks after application, indicating that nerve fibers had regenerated.69 Intra- and sub-ENF regeneration and restoration were also shown when skin biopsies were performed 3 months post-application in patients with painful CIPN70 or non-freezing cold injury.71 These studies suggest that the benefits of high-concentration capsaicin may extend beyond pain relief for patients with painful DPN, although more research is needed to better understand the impact of capsaicin on the diabetic foot.
Epalrestat (an aldose reductase inhibitor which targets activation of the polyol pathway to reduce glucose metabolism) and actovegin (a poly adenosine diphosphate-ribose polymerase inhibitor with pleiotropic neuroprotective and metabolic effects) are licensed to treat DPN in various countries outside of the US based on limited evidence of their efficacy in modifying neurological signs and symptoms.143
Two nutraceuticals, α-lipoic acid and benfotiamine, are also licensed to treat DPN in various countries outside of the US143 and, according to the ADA, may be used as a pathogenetic adjunct to established pharmacological and non-pharmacological interventions for the management of persistent neuropathic symptoms.20 Of the nutraceuticals that have been evaluated in phase 3 RCTs (Table 7),144–150 α-lipoic acid and benfotiamine have the best evidence of neuropathic benefits. α-Lipoic acid, a naturally occurring fatty acid, provides neuroprotective effects by acting as an antioxidant.144,145 Benfotiamine, a fat-soluble derivative of thiamine, acts by inhibiting the formation of advanced glycation end products,146 thereby improving neuropathic symptoms in patients with DPN.147,151 These nutraceuticals are well tolerated, with adverse event profiles similar to those with placebo.
 |
Table 7 Mechanism of Action and Efficacy of Nutraceuticals in Treating Diabetic Peripheral Neuropathy in Phase 3 Randomized Controlled Trials |
Supplementation with vitamin B, vitamin D, and magnesium should currently be limited to patients with proven deficiencies to help prevent the worsening of DPN and other diabetes-related disorders.20 Additional evidence is needed before the use of other nutraceuticals (eg, vitamin E, acetyl-L-carnitine, polyunsaturated fatty acids) can be recommended to modify the pathogenesis of DPN.
Pain Management
Overall, it is estimated that more than half of patients with T2D develop signs and symptoms of peripheral neuropathy during their lifetime, with rates of 20–30% in newly diagnosed and early-stage (first few years) disease.20 Neuropathic pain is a cardinal symptom of DPN and is often severe, poorly diagnosed and difficult to treat.20,152 From the patient’s perspective, painful DPN has a marked negative impact on daily functioning (sleeping, walking, driving, exercising, working, and performing other daily activities) and HR-QoL which, in turn, increases the social and economic burden of the disease.20,152
Successful treatment of painful DPN requires a personalized approach balancing pain relief with improvements in daily functioning and HR-QoL. To achieve this, it is likely that more sophisticated tools beyond simple pain scores (eg, VAS or NPRS) will provide better feedback about neuropathic symptoms.20 The Neuropathy Total Symptom Score-6 evaluates the frequency and intensity of individual neuropathy sensory symptoms frequently identified by DPN patients (ie, numbness and/or insensitivity, prickling and/or tingling sensation, burning sensation, aching pain and/or tightness, sharp, shooting, lancinating pain, and allodynia and/or hyperalgesia).153 The modified Toronto Clinical Neuropathy Score evaluates the presence of symptoms (ie, foot pain, numbness, tingling, weakness, ataxia and upper limb symptoms) and clinical signs (ie sensory pinprick, temperature, light touch, vibration, and position sense) associated with DPN.154
At present, there is a significant need for more effective and better-tolerated treatment options for painful DPN, as many affected patients continue to experience pain despite treatment. While initial responses to current guideline-recommended oral treatments (eg, antiepileptics and antidepressants) may be good, pharmacological tolerance often occurs and higher dosages may be needed to achieve the same level of pain relief. This increases the likelihood of ADRs.20,141 Such patients may benefit from treatment choices that are better tolerated, such as lower-dose combination therapy (pharmacological and non-pharmacological), topical agents (eg, capsaicin 8% topical systems), nutraceuticals, and non-pharmacological approaches (eg, nerve stimulation).
Discussion
Despite multiple FDA-approved, guideline-recommended, and other available options to treat painful DPN, many patients continue to experience uncontrolled pain. An individualized and comprehensive approach, considering pharmacological, neuromodulatory, and non-pharmacological therapies, is often necessary to improve pain outcomes. Since complete resolution of symptoms is not always achievable, patients, caregivers and healthcare providers should have realistic expectations regarding the efficacy of available treatment options, understand that pain reduction (not necessarily pain elimination) and improved HR-QoL are the goals of therapy and that it may be necessary to try a series of treatments in order to identify the most beneficial option.18
Current US evidence-based guidelines on the treatment of painful DPN focus primarily on pharmacological treatments.18–20 Careful consideration is required when selecting pharmacological agents as affected patients are generally already receiving polypharmacy to treat diabetes and other health conditions, which increases the risk of DDIs and ADRs. Diabetic patients in the US take an average of 5.9 medications,155 with an even higher pill burden for those with painful DPN (83% take one or more pain medications solely to treat this condition).156 Treatment selection should consider the potential for systemic ADRs and DDIs, contraindications and precautions in special populations, the presence of comorbid mood and sleep disorders supporting the use of one option over another, costs, and individual patient preferences.157
Of the oral drug classes regarded as first-line therapy in US guidelines and recommendations,18–21 TCAs (eg, amitriptyline, nortriptyline, imipramine), SNRIs (eg, duloxetine, venlafaxine, desvenlafaxine), gabapentinoids (eg, pregabalin, gabapentin), and sodium channel blockers (eg, carbamazepine, oxcarbazepine, lamotrigine) are considered to have comparable efficacy with limited data to support one therapeutic intervention over another.18 Use of oral opioids, including those with a dual MoA such as tapentadol ER, is not recommended. Among topical pharmacological options (which include lignocaine and glyceryl trinitrate), the capsaicin 8% topical system has the most robust evidence and is the only topical agent currently approved by the FDA to treat painful DPN. The capsaicin 8% topical system can be used in combination with oral pharmacotherapy and is not associated with any contraindications, DDIs, systemic ADRs, or need for dose titration/adjustment.
In patients with painful DPN refractory to conventional treatment, neuromodulation with low- or high-frequency SCS is an FDA-approved option.20,21 Intrathecal drug delivery may also improve pain management.158,159 Although its FDA approval is not specific to painful DPN, intrathecal drug delivery using either ziconotide or morphine is recommended and is FDA-approved for chronic neuropathic pain. Use of these neuromodulating options requires careful consideration of individual patient characteristics (eg, pain location and intensity, stage of progression of DPN, response to previous pain therapies, comorbid medical conditions, and concomitant drug treatment), as well as their advantages and disadvantages from a patient-centric perspective.158,159
Future clinical studies in patients with painful DPN are needed to address gaps in current knowledge and provide guidance as to which patients will best respond to various interventions. A better understanding of the pathological mechanistic changes that occur in patients with painful DPN would not only lead to newer therapeutic targets but also would facilitate the discovery of biomarkers to identify responders versus non-responders. To support the use of one agent over another, comparative studies are needed to evaluate the efficacy of two or more active interventions (including oral medications, topical treatments, non-traditional therapies, non-pharmacologic interventions, and combination therapy). The long-term effectiveness of interventions on pain, as well as on other outcomes (eg, HR-QoL, patient functioning, mood, sleep) should be investigated.
Conclusion
Painful DPN, a highly prevalent and disabling complication of diabetes, impacts negatively on patient function and HR-QoL and is associated with significant morbidity, mortality, and healthcare costs. A variety of pharmacological and non-pharmacological options are available to treat painful DPN which may be combined as part of an individualized, comprehensive pain management plan. Healthcare providers are encouraged to increase their familiarity with the available options and to incorporate a comprehensive understanding of the clinical evidence substantiating their efficacy. In recognition of the needs of this fast-growing segment of the diabetic population, research into painful DPN has become increasingly active. Numerous studies are underway evaluating drugs with novel mechanisms of action and various noninvasive electrical stimulation devices. Beyond providing more effective pain relief, identifying disease-modifying interventions that can prevent or reverse the nerve damage associated with DPN should be a research priority. Pharmacoeconomic evaluations should be conducted to determine whether the enormous healthcare burden associated with painful DPN might be mitigated to some extent through the use of modern treatments with greater efficacy and improved tolerability relative to conventional oral agents, despite their higher acquisition costs.
Acknowledgments
The authors did not receive compensation or funding for the development and writing of the manuscript. Writing assistance was provided by Katherine Ann Lyseng-Williamson and Kerry Dechant, ISMPP CMPP™, on behalf of Content Ed Net and was funded by Averitas Pharma USA.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Funded by Averitas Pharma USA.
Disclosure
Jeremy A Adler and Theresa Mallick-Searle are members of the Speakers Bureau for Averitas Pharma USA. Dr Jeremy A Adler also reports personal fees from Collegium Pharma/BioDelivery Biosciences, Averitas Pharm, Neuromatrix, and Redhill Pharma, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Ang L, Mizokami-Stout K, Eid SA, et al. The conundrum of diabetic neuropathies-Past, present, and future. J Diabetes Complications. 2022;36(11):108334. doi:10.1016/j.jdiacomp.2022.108334
2. Jensen TS, Karlsson P, Gylfadottir SS, et al. Painful and non-painful diabetic neuropathy, diagnostic challenges and implications for future management. Brain. 2021;144(6):1632–1645. doi:10.1093/brain/awab079
3. Diabetes. Centers for Disease Control and Prevention; 2021. Available from: https://www.cdc.gov/diabetes/basics/diabetes.html.
4. Hicks CW, Selvin E. Epidemiology of peripheral neuropathy and lower extremity disease in diabetes. Curr Diab Rep. 2019;19(10):86. doi:10.1007/s11892-019-1212-8
5. Anastasi JK, Capili B. Detecting peripheral neuropathy in patients with diabetes, prediabetes and other high-risk conditions: an advanced practice nurse’s perspective. J Med Clin Nurs. 2022;3(2):143. doi:10.47363/jmcn/2022(3)143
6. Iqbal Z, Azmi S, Yadav R, et al. Diabetic peripheral neuropathy: epidemiology, diagnosis, and pharmacotherapy. Clin Ther. 2018;40(6):828–849. doi:10.1016/j.clinthera.2018.04.001
7. Sloan G, Selvarajah D, Tesfaye S. Pathogenesis, diagnosis and clinical management of diabetic sensorimotor peripheral neuropathy. Nat Rev Endocrinol. 2021;17(7):400–420. doi:10.1038/s41574-021-00496-z
8. Feldman EL, Callaghan BC, Pop-Busui R, et al. Diabetic neuropathy. Nat Rev Dis Primers. 2019;5(1):41. doi:10.1038/s41572-019-0092-1
9. Gupta M, Knezevic NN, Abd-Elsayed A, Ray M, Patel K, Chowdhury B. Treatment of painful diabetic neuropathy-A narrative review of pharmacological and interventional approaches. Biomedicines. 2021;9(5):573. doi:10.3390/biomedicines9050573
10. Staudt MD, Prabhala T, Sheldon BL, et al. Current strategies for the management of painful diabetic neuropathy. J Diabetes Sci Technol. 2022;16(2):341–352. doi:10.1177/1932296820951829
11. Naranjo C, Del Reguero L, Moratalla G, et al. Anxiety, depression and sleep disorders in patients with diabetic neuropathic pain: a systematic review. Expert Rev Neurother. 2019;19(12):1201–1209. doi:10.1080/14737175.2019.1653760
12. Elafros MA, Andersen H, Bennett DL, et al. Towards prevention of diabetic peripheral neuropathy: clinical presentation, pathogenesis, and new treatments. Lancet Neurol. 2022;21(10):922–936. doi:10.1016/S1474-4422(22)00188-0
13. Sloan G, Shillo P, Selvarajah D, et al. A new look at painful diabetic neuropathy. Diabet Res Clin Pract. 2018;144:177–191. doi:10.1016/j.diabres.2018.08.020
14. Javed S, Alam U, Malik RA. Treating diabetic neuropathy: present strategies and emerging solutions. Rev Diabet Stud. 2015;12(1–2):63–83. doi:10.1900/rds.2015.12.63
15. Tesfaye S, Boulton AJ, Dyck PJ, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33(10):2285–2293. doi:10.2337/dc10-1303
16. St Onge EL, Miller SA. Pain associated with diabetic peripheral neuropathy: a review of available treatments. P T. 2008;33(3):166–176.
17. Tesfaye S, Boulton AJM, Dickenson AH. Mechanisms and management of diabetic painful distal symmetrical polyneuropathy. Diabetes Care. 2013;36(9):2456–2465. doi:10.2337/dc12-1964
18. Price R, Smith D, Franklin G, et al. Oral and topical treatment of painful diabetic polyneuropathy: practice guideline update summary: report of the AAN Guideline Subcommittee. Neurology. 2022;98(1):31–43. doi:10.1212/wnl.0000000000013038
19. Pop-Busui R, Boulton AJM, Feldman EL, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(1):136–154. doi:10.2337/dc16-2042
20. Pop-Busui R, Ang L, Boulton AJM, et al. Diagnosis and Treatment of Painful Diabetic Peripheral Neuropathy. Arlington (VA): American Diabetes Association, Inc.; 2022.
21. Blonde L, Umpierrez GE, Reddy SS, et al. American Association of Clinical Endocrinology Clinical Practice Guideline: developing a Diabetes Mellitus Comprehensive Care Plan-2022 Update. Endocr Pract. 2022;28(10):923–1049. doi:10.1016/j.eprac.2022.08.002
22. Ziegler D, Keller J, Maier C, Pannek J. Diabetic neuropathy. Exp Clin Endocrinol Diabetes. 2021;129:S70–S81. doi:10.1055/a-1284-6245
23. James CF, Tripathi S, Karampatou K, Gladston DV, Pappachan JM. Pharmacotherapy of Painful Diabetic Neuropathy: a Clinical Update. Sisli Etfal Hastan Tip Bul. 2022;56(1):1–20. doi:10.14744/semb.2021.54670
24. Rafiullah M, Siddiqui K. Pharmacological Treatment of Diabetic Peripheral Neuropathy: an Update. CNS Neurol Disord Drug Targets. 2022;21(10):884–900. doi:10.2174/1871527320666210303111939
25. Mick G, Baron R, Correa-Illanes G, et al. Is an easy and reliable diagnosis of localized neuropathic pain (LNP) possible in general practice? Development of a screening tool based on IASP criteria. Curr Med Res Opin. 2014;30(7):1357–1366. doi:10.1185/03007995.2014.907562
26. American Diabetes Association. Introduction: standards of Medical Care in Diabetes—2022. Diabetes Care. 2022;45(Supplement_1):S1–S2. doi:10.2337/dc22-Sint
27. American Diabetes Association Professional Practice Committee. 12. Retinopathy, Neuropathy, and Foot Care: standards of Medical Care in Diabetes—2022. Diabetes Care. 2022;45(Supplement_1):S185–S194. doi:10.2337/dc22-S012
28. Khdour MR. Treatment of diabetic peripheral neuropathy: a review. J Pharm Pharmacol. 2020;72(7):863–872. doi:10.1111/jphp.13241
29. Ziegler D, Tesfaye S, Spallone V, et al. Screening, diagnosis and management of diabetic sensorimotor polyneuropathy in clinical practice: international expert consensus recommendations. Diabet Res Clin Pract. 2022;186:109063. doi:10.1016/j.diabres.2021.109063
30. Finnerup NB, Attal N, Haroutounian S, McNicol E. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–173. doi:10.1016/S1474-4422(14)70251-0
31. van Dam PS, Valk GD, Bakker K. [Diabetic peripheral neuropathy: international guidelines for prevention, diagnosis, and treatment]. Ned Tijdschr Geneeskd. 2000;144(9):418–421.
32. Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17(9):1113–e88. doi:10.1111/j.1468-1331.2010.02999.x
33. Boulton AJ. Guidelines for diagnosis and outpatient management of diabetic peripheral neuropathy. European Association for the Study of Diabetes. Neurodiab Diabetes Metab. 1998;24(Suppl 3):55–65.
34. Tan T, Barry P, Reken S, Baker M. Pharmacological management of neuropathic pain in non-specialist settings: summary of NICE guidance. BMJ. 2010;340:c1079. doi:10.1136/bmj.c1079
35. Moulin D, Boulanger A, Clark AJ, et al. Pharmacological management of chronic neuropathic pain: revised consensus statement from the Canadian Pain Society. Pain Res Manag. 2014;19(6):328–335. doi:10.1155/2014/754693
36. Schlereth T. Guideline “diagnosis and non interventional therapy of neuropathic pain” of the German Society of Neurology (deutsche Gesellschaft für Neurologie). Neurol Res Pract. 2020;2(1):16. doi:10.1186/s42466-020-00063-3
37. Haslbeck M, Neundörfer B, Wilm S. German national disease management guidelines ”diabetic neuropathy”. Important implications on clinical practice. MMW Fortschr Med. 2011;153(49–50):1.
38. Intellis™, Vanta™, Sequentia™ LT neurostimulation systems for pain therapy: information for prescribers. Minneapolis, MN: Medtronic, Inc.; 2021.
39. Senza®, Senza II™, Senza Omnia™ (spinal cord stimulation systems): US physician implant manual. Redwood City, CA: Nevro Corp.; 2020.
40. Qutenza® (Capsaicin) Topical System: US Prescribing Information. Morristown, NJ: Averitas Pharma, Inc; 2023.
41. Nucynta® ER (tapentadol) extended-release tablets, for oral use C-II: US prescribing information. Stoughton, MA: Collegium Pharmaceutical, Inc.; 2021.
42. Drizalma Sprinkle™ (Duloxetine Delayed-Release Capsules), for Oral Use: US Prescribing Information. Cranbury, NJ: Sun Pharmaceuticals Industries Limited; 2021.
43. Cymbalta® (Duloxetine Delayed-Release Capsules), for Oral Use: US Prescribing Information. Indianapolis, IN: Eli Lilly and Company; 2021.
44. Lyrica® (Pregabalin) Capsules and Solution, for Oral Use: US Prescribing Information. New York, NY: Pfizer Inc.; 2020.
45. Strand NH, Burkey AR. Neuromodulation in the treatment of painful diabetic neuropathy: a review of evidence for spinal cord stimulation. J Diabetes Sci Technol. 2022;16(2):332–340. doi:10.1177/19322968211060075
46. de Vos CC, Meier K, Zaalberg PB, et al. Spinal cord stimulation in patients with painful diabetic neuropathy: a multicentre randomized clinical trial. Pain. 2014;155(11):2426–2431. doi:10.1016/j.pain.2014.08.031
47. Slangen R, Schaper NC, Faber CG, et al. Spinal cord stimulation and pain relief in painful diabetic peripheral neuropathy: a prospective two-center randomized controlled trial. Diabetes Care. 2014;37(11):3016–3024. doi:10.2337/dc14-0684
48. Petersen EA, Stauss TG, Scowcroft JA, et al. Effect of high-frequency (10-kHz) spinal cord stimulation in patients with painful diabetic neuropathy: a randomized clinical trial. JAMA Neurol. 2021;78(6):687–698. doi:10.1001/jamaneurol.2021.0538
49. Clinical evidence on SCS for painful DPN. Minneapolis, MN: Medtronic; 2022. Available from https://www.medtronic.com/content/dam/medtronic-com/us-en/hcp/therapies-conditions/neurological/spinal-cord-stimulation/scs-pdn-clinical-evidence-compendium.pdf.
50. Duarte RV, Nevitt S, Copley S, et al. Systematic review and network meta-analysis of neurostimulation for painful diabetic neuropathy. Diabetes Care. 2022;45(10):2466–2475. doi:10.2337/dc22-0932
51. Duarte RV, Nevitt S, Maden M, et al. Spinal cord stimulation for the management of painful diabetic neuropathy: a systematic review and meta-analysis of individual patient and aggregate data. Pain. 2021;162(11):2635–2643. doi:10.1097/j.pain.0000000000002262
52. Pluijms WA, Slangen R, Bakkers M, et al. Pain relief and quality-of-life improvement after spinal cord stimulation in painful diabetic polyneuropathy: a pilot study. Br J Anaesth. 2012;109(4):623–629. doi:10.1093/bja/aes251
53. van Beek M, Geurts JW, Slangen R, et al. Severity of neuropathy is associated with long-term spinal cord stimulation outcome in painful diabetic peripheral neuropathy: five-year follow-up of a prospective two-center clinical trial. Diabetes Care. 2018;41(1):32–38. doi:10.2337/dc17-0983
54. Zuidema X, van Daal E, van Geel I, et al. Long-term evaluation of spinal cord stimulation in patients with painful diabetic polyneuropathy: an eight-to-ten-year prospective cohort study. Neuromodulation. 2023;26(5):1074–1080. doi:10.1016/j.neurom.2022.12.003
55. Petersen EA, Stauss TG, Scowcroft JA, et al. Durability of high-frequency 10-kHz spinal cord stimulation for patients with painful diabetic neuropathy refractory to conventional treatments: 12-month results from a randomized controlled trial. Diabetes Care. 2022;45(1):e3–e6. doi:10.2337/dc21-1813
56. The Nobel Prize. The Nobel Prize in Physiology or Medicine 2021 was awarded jointly to David Julius and Ardem Patapoutian “for their discoveries of receptors for temperature and touch”. Available from https://www.nobelprize.org/prizes/medicine/2021/summary/.
57. Anand P, Bley K. Topical capsaicin for pain management: therapeutic potential and mechanisms of action of the new high-concentration capsaicin 8% patch. Br J Anaesth. 2011;107(4):490–502. doi:10.1093/bja/aer260
58. Baranidharan G, Das S, Bhaskar A. A review of the high-concentration capsaicin patch and experience in its use in the management of neuropathic pain. Ther Adv Neurol Disord. 2013;6(5):287–297. doi:10.1177/1756285613496862
59. Wohlrab J, Neubert RH, Heskamp ML, Michael J. Cutaneous drug delivery of capsaicin after in vitro administration of the 8% capsaicin dermal patch system. Skin Pharmacol Physiol. 2015;28(2):65–74. doi:10.1159/000362740
60. Leppert W, Malec-Milewska M, Zajaczkowska R, Wordliseck Z. Transdermal and topical drug administration in the treatment of pain. Molecules. 2018;23(3):681. doi:10.3390/molecules23030681
61. Frias B, Merighi A. Capsaicin, nociception and pain. Molecules. 2016;21(6):797. doi:10.3390/molecules21060797
62. Noto C, Pappagallo M, Szallasi A. NGX-4010, a high-concentration capsaicin dermal patch for lasting relief of peripheral neuropathic pain. Curr Opin Invest Drugs. 2009;10(7):702–710.
63. Premkumar LS, Sikand P. TRPV1: a target for next generation analgesics. Curr Neuropharmacol. 2008;6(2):151–163. doi:10.2174/157015908784533888
64. Malmberg AB, Mizisin AP, Calcutt NA, von Stein T, Robbins WR, Bley KR. Reduced heat sensitivity and epidermal nerve fiber immunostaining following single applications of a high-concentration capsaicin patch. Pain. 2004;111(3):360–367. doi:10.1016/j.pain.2004.07.017
65. Lo Vecchio S, Andersen HH, Arendt-Nielsen L. The time course of brief and prolonged topical 8% capsaicin-induced desensitization in healthy volunteers evaluated by quantitative sensory testing and vasomotor imaging. Exp Brain Res. 2018;236(8):2231–2244. doi:10.1007/s00221-018-5299-y
66. Nolano M, Simone DA, Wendelschafer-Crabb G, Johnson T, Hazen E, Kennedy WR. Topical capsaicin in humans: parallel loss of epidermal nerve fibers and pain sensation. Pain. 1999;81(1–2):135–145. doi:10.1016/s0304-3959(99)00007-x
67. Kennedy WR, Vanhove GF, Lu SP, Tobias J. A randomized, controlled, open-label study of the long-term effects of NGX-4010, a high-concentration capsaicin patch, on epidermal nerve fiber density and sensory function in healthy volunteers. J Pain. 2010;11(6):579–587. doi:10.1016/j.jpain.2009.09.019
68. Anand P, Privitera R, Donatien P, et al. Reversing painful and non-painful diabetic neuropathy with the capsaicin 8% patch: clinical evidence for pain relief and restoration of function via nerve fiber regeneration. Front Neurol. 2022;13:998904. doi:10.3389/fneur.2022.998904
69. Sendel M, Dunst A, Forstenpointner J, Hüllemann P, Baron R. Capsaicin treatment in neuropathic pain: axon reflex vasodilatation after 4 weeks correlates with pain reduction. Pain. 2023;164(3):534–542. doi:10.1097/j.pain.0000000000002735
70. Anand P, Elsafa E, Privitera R, et al. Rational treatment of chemotherapy-induced peripheral neuropathy with capsaicin 8% patch: from pain relief towards disease modification. J Pain Res. 2019;12:2039–2052. doi:10.2147/jpr.S213912
71. Anand P, Privitera R, Donatien P, Misra VP, Woods DR. Capsaicin 8% patch treatment in non-freezing cold injury: evidence for pain relief and nerve regeneration. Front Neurol. 2021;12:722875. doi:10.3389/fneur.2021.722875
72. Babbar S, Marier JF, Mouksassi MS, et al. Pharmacokinetic analysis of capsaicin after topical administration of a high-concentration capsaicin patch to patients with peripheral neuropathic pain. Ther Drug Monit. 2009;31(4):502–510. doi:10.1097/FTD.0b013e3181a8b200
73. Simpson DM, Robinson-Papp J, Van J, et al. Capsaicin 8% patch in painful diabetic peripheral neuropathy: a randomized, double-blind, placebo-controlled study. J Pain. 2017;18(1):42–53. doi:10.1016/j.jpain.2016.09.008
74. Vinik AI, Perrot S, Vinik EJ, et al. Capsaicin 8% patch repeat treatment plus standard of care (SOC) versus SOC alone in painful diabetic peripheral neuropathy: a randomised, 52-week, open-label, safety study. BMC Neurol. 2016;16(1):251. doi:10.1186/s12883-016-0752-7
75. Vinik AI, Perrot S, Vinik EJ, et al. Repeat treatment with capsaicin 8% patch (179mg capsaicin cutaneous patch): effects on pain, quality of life, and patient satisfaction in painful diabetic peripheral neuropathy: an open-label, randomized controlled clinical trial. J Curr Med Res Opin. 2019;2(12):388–401. doi:10.15520/jcmro.v2i12.242
76. Freynhagen R, Argoff C, Eerdekens M, Engelen S, Perrot S. Progressive response to repeat application of capsaicin 179 mg (8% w/w) cutaneous patch in peripheral neuropathic pain: comprehensive new analysis and clinical implications. Pain Med. 2021;22(10):2324–2336. doi:10.1093/pm/pnab113
77. van Nooten F, Treur M, Pantiri K, Stoker M, Charokopou M. Capsaicin 8% patch versus oral neuropathic pain medications for the treatment of painful diabetic peripheral neuropathy: a systematic literature review and network meta-analysis. Clin Ther. 2017;39(4):787–803.e18. doi:10.1016/j.clinthera.2017.02.010
78. Schwartz S, Etropolski M, Shapiro DY, et al. Safety and efficacy of tapentadol ER in patients with painful diabetic peripheral neuropathy: results of a randomized-withdrawal, placebo-controlled trial. Curr Med Res Opin. 2011;27(1):151–162. doi:10.1185/03007995.2010.537589
79. Vinik AI, Shapiro DY, Rauschkolb C, et al. A randomized withdrawal, placebo-controlled study evaluating the efficacy and tolerability of tapentadol extended release in patients with chronic painful diabetic peripheral neuropathy. Diabetes Care. 2014;37(8):2302–2309. doi:10.2337/dc13-2291
80. Schwartz S, Etropolski MS, Shapiro DY, et al. A pooled analysis evaluating the efficacy and tolerability of tapentadol extended release for chronic, painful diabetic peripheral neuropathy. Clin Drug Investig. 2015;35(2):95–108. doi:10.1007/s40261-014-0249-3
81. Wang S-Y, Calderon J, Kuo Wang G. Block of neuronal Na+ channels by antidepressant duloxetine in a state-dependent manner. Anesthesiology. 2010;113(3):655–665. doi:10.1097/ALN.0b013e3181e89a93
82. Obata H. Analgesic mechanisms of antidepressants for neuropathic pain. Int J Mol Sci. 2017;18(11):2483. doi:10.3390/ijms18112483
83. Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain. 2005;116(1–2):109–118. doi:10.1016/j.pain.2005.03.029
84. Wernicke JF, Pritchett YL, D’Souza DN, et al. A randomized controlled trial of duloxetine in diabetic peripheral neuropathic pain. Neurology. 2006;67(8):1411–1420. doi:10.1212/01.wnl.0000240225.04000.1a
85. Chincholkar M. Gabapentinoids: pharmacokinetics, pharmacodynamics and considerations for clinical practice. Br J Pain. 2020;14(2):104–114. doi:10.1177/2049463720912496
86. Lesser H, Sharma U, LaMoreaux L, Poole RM. Pregabalin relieves symptoms of painful diabetic neuropathy: a randomized controlled trial. Neurology. 2004;63(11):2104–2110. doi:10.1212/01.Wnl.0000145767.36287.A1
87. Rosenstock J, Tuchman M, LaMoreaux L, Sharma U. Pregabalin for the treatment of painful diabetic peripheral neuropathy: a double-blind, placebo-controlled trial. Pain. 2004;110(3):628–638. doi:10.1016/j.pain.2004.05.001
88. Parsons B, Li C. The efficacy of pregabalin in patients with moderate and severe pain due to diabetic peripheral neuropathy. Curr Med Res Opin. 2016;32(5):929–937. doi:10.1185/03007995.2016.1151776
89. Evoy KE, Sadrameli S, Contreras J, Covvey JR, Peckham AM, Morrison MD. Abuse and misuse of pregabalin and gabapentin: a systematic review update. Drugs. 2021;81(1):125–156. doi:10.1007/s40265-020-01432-7
90. Fornasari D. Pharmacotherapy for neuropathic pain: a review. Pain Ther. 2017;6(Suppl 1):25–33. doi:10.1007/s40122-017-0091-4
91. Coluzzi F, Mattia C. Mechanism-based treatment in chronic neuropathic pain: the role of antidepressants. Curr Pharm Des. 2005;11(23):2945–2960. doi:10.2174/1381612054864993
92. Max MB, Culnane M, Schafer SC, et al. Amitriptyline relieves diabetic neuropathy pain in patients with normal or depressed mood. Neurology. 1987;37(4):589–596. doi:10.1212/wnl.37.4.589
93. Boyle J, Eriksson MEV, Gribble L, et al. Randomized, placebo-controlled comparison of amitriptyline, duloxetine, and pregabalin in patients with chronic diabetic peripheral neuropathic pain: impact on pain, polysomnographic sleep, daytime functioning, and quality of life. Diabetes Care. 2012;35(12):2451–2458. doi:10.2337/dc12-0656
94. Shabbir B, Shafi F, Mahboob F. Amitriptyline vs pregabalin in painful diabetic neuropathy; a randomised placebo-based study. P J M H S. 2011;5(4):745–747.
95. Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;2015(7):Cd008242. doi:10.1002/14651858.CD008242.pub3
96. Rudroju N, Bansal D, Talakokkula ST, et al. Comparative efficacy and safety of six antidepressants and anticonvulsants in painful diabetic neuropathy: a network meta-analysis. Pain Physician. 2013;16(6):E705–E714.
97. Asrar MM, Kumari S, Sekhar BC, Bhansali A, Bansal D. Relative efficacy and safety of pharmacotherapeutic interventions for diabetic peripheral neuropathy: a systematic review and Bayesian network meta-analysis. Pain Physician. 2021;24(1):E1–E14.
98. Derry S, Wiffen PJ, Aldington D, Moore RA. Nortriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;1(1):Cd011209. doi:10.1002/14651858.CD011209.pub2
99. Hearn L, Moore RA, Derry S, Wiffen PJ, Phillips T. Desipramine for neuropathic pain in adults. Cochrane Database Syst Rev. 2014;2014(9):Cd011003. doi:10.1002/14651858.CD011003.pub2
100. Hearn L, Derry S, Phillips T, Moore RA, Wiffen PJ. Imipramine for neuropathic pain in adults. Cochrane Database Syst Rev. 2014;2014(5):Cd010769. doi:10.1002/14651858.CD010769.pub2
101. Allen R, Sharma U, Barlas S. Clinical experience with desvenlafaxine in treatment of pain associated with diabetic peripheral neuropathy. J Pain Res. 2014;7:339–351. doi:10.2147/jpr.S55682
102. Rowbotham MC, Goli V, Kunz NR, Lei D. Venlafaxine extended release in the treatment of painful diabetic neuropathy: a double-blind, placebo-controlled study. Pain. 2004;110(3):697–706. doi:10.1016/j.pain.2004.05.010
103. Backonja M, Beydoun A, Edwards KR, et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA. 1998;280(21):1831–1836. doi:10.1001/jama.280.21.1831
104. Gorson KC, Schott C, Herman R, Ropper AH, Rand WM. Gabapentin in the treatment of painful diabetic neuropathy: a placebo controlled, double blind, crossover trial. J Neurol Neurosurg Psychiatry. 1999;66(2):251–252. doi:10.1136/jnnp.66.2.251
105. Meldrum BS, Rogawski MA. Molecular targets for antiepileptic drug development. Neurotherapeutics. 2007;4(1):18–61. doi:10.1016/j.nurt.2006.11.010
106. Zuliani V, Rivara M, Fantini M, Costantino G. Sodium channel blockers for neuropathic pain. Expert Opin Ther Pat. 2010;20(6):755–779. doi:10.1517/13543771003774118
107. Shaibani A, Fares S, Selam JL, et al. Lacosamide in painful diabetic neuropathy: an 18-week double-blind placebo-controlled trial. J Pain. 2009;10(8):818–828. doi:10.1016/j.jpain.2009.01.322
108. Wymer JP, Simpson J, Sen D, Bongardt S. Efficacy and safety of lacosamide in diabetic neuropathic pain: an 18-week double-blind placebo-controlled trial of fixed-dose regimens. Clin J Pain. 2009;25(5):376–385. doi:10.1097/AJP.0b013e318196d2b6
109. Eisenberg E, Lurie Y, Braker C, Daoud D, Ishay A. Lamotrigine reduces painful diabetic neuropathy: a randomized, controlled study. Neurology. 2001;57(3):505–509. doi:10.1212/wnl.57.3.505
110. Vinik AI, Tuchman M, Safirstein B, et al. Lamotrigine for treatment of pain associated with diabetic neuropathy: results of two randomized, double-blind, placebo-controlled studies. Pain. 2007;128(1):169–179. doi:10.1016/j.pain.2006.09.040
111. Dogra S, Beydoun S, Mazzola J, Hopwood M, Wan Y. Oxcarbazepine in painful diabetic neuropathy: a randomized, placebo-controlled study. Eur J Pain. 2005;9(5):543–554. doi:10.1016/j.ejpain.2004.11.006
112. Grosskopf J, Mazzola J, Wan Y, Hopwood M. A randomized, placebo-controlled study of oxcarbazepine in painful diabetic neuropathy. Acta Neurol Scand. 2006;114(3):177–180. doi:10.1111/j.1600-0404.2005.00559.x
113. Kochar DK, Jain N, Agarwal RP, Srivastava T, Agarwal P, Gupta S. Sodium valproate in the management of painful neuropathy in type 2 diabetes - A randomized placebo controlled study. Acta Neurol Scand. 2002;106(5):248–252. doi:10.1034/j.1600-0404.2002.01229.x
114. Kochar DK, Rawat N, Agrawal RP, et al. Sodium valproate for painful diabetic neuropathy: a randomized double-blind placebo-controlled study. Qjm. 2004;97(1):33–38. doi:10.1093/qjmed/hch007
115. Sansone RA, Sansone LA. Serotonin norepinephrine reuptake inhibitors: a pharmacological comparison. Innov Clin Neurosci. 2014;11(3–4):1.
116. Neurontin® (Gabapentin) Capsules, Tablets, Solution, for Oral Use: US Prescribing Information. New York, NY: Pfizer Inc; 2020.
117. Theile JW, Cummins TR. Recent developments regarding voltage-gated sodium channel blockers for the treatment of inherited and acquired neuropathic pain syndromes. Front Pharmacol. 2011;2:54. doi:10.3389/fphar.2011.00054
118. ClinicalTrials.gov. U.S. National Library of Medicine. Available from https://clinicaltrials.gov.
119. Kessler JA, Shaibani A, Sang CN, et al. Gene therapy for diabetic peripheral neuropathy: a randomized, placebo-controlled Phase III study of VM202, a plasmid DNA encoding human hepatocyte growth factor. Clin Transl Sci. 2021;14(3):1176–1184. doi:10.1111/cts.12977
120. Tiecke E, Rainisio M, Eisenberg E, et al. NRD.E1, an innovative non-opioid therapy for painful diabetic peripheral neuropathy-A randomized proof of concept study. Eur J Pain. 2022;26(8):1665–1678. doi:10.1002/ejp.1989
121. Anand U, Yiangou Y, Sinisi M, et al. Mechanisms underlying clinical efficacy of Angiotensin II type 2 receptor (AT2R) antagonist EMA401 in neuropathic pain: clinical tissue and in vitro studies. Mol Pain. 2015;11:38. doi:10.1186/s12990-015-0038-x
122. Rice ASC, Dworkin RH, Finnerup NB, et al. Efficacy and safety of EMA401 in peripheral neuropathic pain: results of 2 randomised, double-blind, phase 2 studies in patients with postherpetic neuralgia and painful diabetic neuropathy. Pain. 2021;162(10):2578–2589. doi:10.1097/j.pain.0000000000002252
123. Chalk C, Benstead TJ, Moore F. Aldose reductase inhibitors for the treatment of diabetic polyneuropathy. Cochrane Database Syst Rev. 2007;2007(4):Cd004572. doi:10.1002/14651858.CD004572.pub2
124. Talbot S, Couture R. Emerging role of microglial kinin B1 receptor in diabetic pain neuropathy. Exp Neurol. 2012;234(2):373–381. doi:10.1016/j.expneurol.2011.11.032
125. Rahn EJ, Hohmann AG. Cannabinoids as pharmacotherapies for neuropathic pain: from the bench to the bedside. Neurotherapeutics. 2009;6(4):713–737. doi:10.1016/j.nurt.2009.08.002
126. Zebala JA, Searle SL, Webster LR, et al. Desmetramadol has the safety and analgesic profile of tramadol without its metabolic liabilities: consecutive randomized, double-blind, placebo- and active comparator-controlled trials. J Pain. 2019;20(10):1218–1235. doi:10.1016/j.jpain.2019.04.005
127. Weyer AD, Lehto SG. Development of TRPM8 antagonists to treat chronic pain and migraine. Pharmaceuticals (Basel). 2017;10(2):37. doi:10.3390/ph10020037
128. Kostich W, Hamman BD, Li YW, et al. Inhibition of AAK1 kinase as a novel therapeutic approach to treat neuropathic pain. J Pharmacol Exp Ther. 2016;358(3):371–386. doi:10.1124/jpet.116.235333
129. Julius D. TRP channels and pain. Annu Rev Cell Dev Biol. 2013;29:355–384. doi:10.1146/annurev-cellbio-101011-155833
130. Verma V, Khoury S, Parisien M, et al. The dichotomous role of epiregulin in pain. Pain. 2020;161(5):1052–1064. doi:10.1097/j.pain.0000000000001792
131. Uchida K, Takano S, Matsumoto T, et al. Transforming growth factor activating kinase 1 regulates extracellular matrix degrading enzymes and pain-related molecule expression following tumor necrosis factor-α stimulation of synovial cells: an in vitro study. BMC Musculoskelet Disord. 2017;18(1):283. doi:10.1186/s12891-017-1648-4
132. Mizumura K, Murase S. Role of nerve growth factor in pain. Handb Exp Pharmacol. 2015;227:57–77. doi:10.1007/978-3-662-46450-2_4
133. Li J, Yu M, Fu S, Liu D, Tan Y. Role of selective histone deacetylase 6 inhibitor ACY-1215 in cancer and other human diseases. Front Pharmacol. 2022;13:907981. doi:10.3389/fphar.2022.907981
134. Rupp A, Young E, Chadwick AL. Low-dose naltrexone’s utility for non-cancer centralized pain conditions: a scoping review. Pain Med. 2023;24(11):1270–1281. doi:10.1093/pm/pnad074
135. Srinivasan A, Dutta P, Bansal D, et al. Efficacy and safety of low-dose naltrexone in painful diabetic neuropathy: a randomized, double-blind, active-control, crossover clinical trial. J Diabetes. 2021;13(10):770–778. doi:10.1111/1753-0407.13202
136. Stein C, Eibel B, Sbruzzi G, Lago PD, Plentz RD. Electrical stimulation and electromagnetic field use in patients with diabetic neuropathy: systematic review and meta-analysis. Braz J Phys Ther. 2013;17(2):93–104. doi:10.1590/s1413-35552012005000083
137. Bosi E, Bax G, Scionti L, et al. Frequency-modulated electromagnetic neural stimulation (FREMS) as a treatment for symptomatic diabetic neuropathy: results from a double-blind, randomised, multicentre, long-term, placebo-controlled clinical trial. Diabetologia. 2013;56(3):467–475. doi:10.1007/s00125-012-2795-7
138. Bosi E, Conti M, Vermigli C, et al. Effectiveness of frequency-modulated electromagnetic neural stimulation in the treatment of painful diabetic neuropathy. Diabetologia. 2005;48(5):817–823. doi:10.1007/s00125-005-1734-2
139. Lavery LA, Murdoch DP, Williams J, Lavery DC. Does anodyne light therapy improve peripheral neuropathy in diabetes? A double-blind, sham-controlled, randomized trial to evaluate monochromatic infrared photoenergy. Diabetes Care. 2008;31(2):316–321. doi:10.2337/dc07-1794
140. Thakral G, Kim PJ, LaFontaine J, Menzies R, Najafi B, Lavery LA. Electrical stimulation as an adjunctive treatment of painful and sensory diabetic neuropathy. J Diabetes Sci Technol. 2013;7(5):1202–1209. doi:10.1177/193229681300700510
141. Papanas N, Ziegler D. Emerging drugs for diabetic peripheral neuropathy and neuropathic pain. Expert Opin Emerg Drugs. 2016;21(4):393–407. doi:10.1080/14728214.2016.1257605
142. Narayanaswamy H, Facer P, Misra VP, et al. A longitudinal study of sensory biomarkers of progression in patients with diabetic peripheral neuropathy using skin biopsies. J Clin Neurosci. 2012;19(11):1490–1496. doi:10.1016/j.jocn.2011.12.026
143. Ziegler D, Papanas N, Schnell O, et al. Current concepts in the management of diabetic polyneuropathy. J Diabetes Investig. 2021;12(4):464–475. doi:10.1111/jdi.13401
144. Khan H, Singh TG, Dahiya RS, Abdel-Daim MM. α-Lipoic acid, an organosulfur biomolecule a novel therapeutic agent for neurodegenerative disorders: an mechanistic perspective. Neurochem Res. 2022;47(7):1853–1864. doi:10.1007/s11064-022-03598-w
145. Papanas N, Ziegler D. Efficacy of α-lipoic acid in diabetic neuropathy. Expert Opin Pharmacother. 2014;15(18):2721–2731. doi:10.1517/14656566.2014.972935
146. Pai ST. Chapter 13 - Peripheral Neuropathy. In: Rakel D, editor. Integrative Medicine.
147. Stracke H, Gaus W, Achenbach U, Federlin K, Bretzel RG. Benfotiamine in diabetic polyneuropathy (BENDIP): results of a randomised, double blind, placebo-controlled clinical study. Exp Clin Endocrinol Diabetes. 2008;116(10):600–605. doi:10.1055/s-2008-1065351
148. Shevalye H, Watcho P, Stavniichuk R, Dyukova E, Lupachyk S, Obrosova IG. Metanx alleviates multiple manifestations of peripheral neuropathy and increases intraepidermal nerve fiber density in Zucker diabetic fatty rats. Diabetes. 2012;61(8):2126–2133. doi:10.2337/db11-1524
149. Fonseca VA, Lavery LA, Thethi TK, et al. Metanx in type 2 diabetes with peripheral neuropathy: a randomized trial. Am J Med. 2013;126(2):141–149. doi:10.1016/j.amjmed.2012.06.022
150. Hor CP, Fung WY, Ang HA, et al. Efficacy of oral mixed tocotrienols in diabetic peripheral neuropathy: a randomized clinical trial. JAMA Neurol. 2018;75(4):444–452. doi:10.1001/jamaneurol.2017.4609
151. Ziegler D, Porta M, Papanas N, et al. The role of biofactors in diabetic microvascular complications. Curr Diabetes Rev. 2022;18(4):e250821195830. doi:10.2174/1871527320666210825112240
152. Sadosky A, Mardekian J, Parsons B, Hopps M, Bienen EJ, Markman J. Healthcare utilization and costs in diabetes relative to the clinical spectrum of painful diabetic peripheral neuropathy. J Diabetes Complications. 2015;29(2):212–217. doi:10.1016/j.jdiacomp.2014.10.013
153. Bastyr EJ 3rd, Price KL, Bril V. Development and validity testing of the neuropathy total symptom score-6: questionnaire for the study of sensory symptoms of diabetic peripheral neuropathy. Clin Ther. 2005;27(8):1278–1294. doi:10.1016/j.clinthera.2005.08.002
154. Bril V, Tomioka S, Buchanan RA, Perkins BA. Reliability and validity of the modified Toronto Clinical Neuropathy Score in diabetic sensorimotor polyneuropathy. Diabet Med. 2009;26(3):240–246. doi:10.1111/j.1464-5491.2009.02667.x
155. Saydah SH. Medication use and self-care practices in persons with diabetes. In: Cowie CC, Casagrande SS, Menke A, editors. Diabetes in America.
156. Gore M, Brandenburg NA, Hoffman DL, Tai K-S, Stacey B. Burden of illness in painful diabetic peripheral neuropathy: the patients’ perspectives. J Pain. 2006;7(12):892–900. doi:10.1016/j.jpain.2006.04.013
157. Stillman M. Clinical approach to patients with neuropathic pain. Cleve Clin J Med. 2006;73(8):726–736 passim. doi:10.3949/ccjm.73.8.726
158. Deer TR, Pope JE, Hanes MC, McDowell GC. Intrathecal therapy for chronic pain: a review of morphine and ziconotide as firstline options. Pain Med. 2019;20(4):784–798. doi:10.1093/pm/pny132
159. Deer TR, Hayek SM, Pope JE, et al. The Polyanalgesic Consensus Conference (PACC): recommendations for trialing of intrathecal drug delivery infusion therapy. Neuromodulation. 2017;20(2):133–154. doi:10.1111/ner.12543
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
