Back to Journals » Vascular Health and Risk Management » Volume 19
Using Coronary Artery Calcium Score as Diagnostic Tool in Symptomatic Chronic Coronary Syndrome Patients in a Real-Life Setting
Authors Witvliet MP , Arkenbout EK, Kamphuisen PW
Received 22 May 2023
Accepted for publication 4 August 2023
Published 5 September 2023 Volume 2023:19 Pages 571—582
DOI https://doi.org/10.2147/VHRM.S422458
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
M Patrick Witvliet,1,2 E Karin Arkenbout,3 Pieter W Kamphuisen1,4
1Department of Internal Medicine, Tergooi Medical Center, Hilversum, the Netherlands; 2Department of General Practice, Amsterdam UMC Location University of Amsterdam, Amsterdam, the Netherlands; 3Department of Cardiology, Tergooi Medical Center, Hilversum, the Netherlands; 4Department of Vascular Medicine, Amsterdam UMC location University of Amsterdam, Amsterdam, the Netherlands
Correspondence: M Patrick Witvliet, Department of Internal Medicine, Tergooi Medical Center, Laan van Tergooi 2, 1212 VG, Hilversum, the Netherlands, Tel +31 205664271, Email [email protected]
Background: The coronary artery calcium (CAC) score can be used to increase (CAC score > 0) or decrease (CAC score = 0) the likelihood of coronary artery disease (CAD). We compared the CAC score with the pre-test probability (PTP) for CAD (low, intermediate, and high). Furthermore, we compared the CAC score with exercise electrocardiography (ECG) and compared both tests with coronary angiography.
Methods and Results: We retrospectively identified patients with angina and/or dyspnea for whom CAC score was used to increase or decrease the likelihood of CAD. Of 882 patients, majority had low (45%) or intermediate (44%) PTP. Patients with higher PTP had significantly higher CAC scores (Cramer’s V = 0.29, p < 0.0001). Most patients (57%) had a CAC score of zero, especially those with low (73%) and intermediate (49%) PTP. However, 20% of patients with high PTP had CAC score of zero. Higher CAC scores were observed in patients with abnormal exercise ECG, but association was weak and not significant (Cramer’s V = 0.13, p = 0.08). Moreover, more than 40% of patients with an abnormal exercise ECG had CAC score of zero. Higher CAC scores were associated with more severe abnormalities on coronary angiography (Cramer’s V = 0.43, p < 0.0001), whereas there was no association between results of exercise ECG and coronary angiography (Cramer’s V = 0.11, p = 0.91).
Conclusion: CAC score can be used in addition to PTP to increase or decrease the likelihood of CAD, and it might be more useful than exercise ECG in the diagnostic work-up of chest pain.
Keywords: coronary artery disease, cardiovascular disease, CT, risk factors, angina, stable
Introduction
Patients with suspected coronary artery disease (CAD) in a non-acute setting often present with anginal symptoms and/or dyspnea.1–4 Patients presenting with typical angina have the highest pre-test probability (PTP) for CAD, but account for only 10–15% of patients suspected of having CAD in clinical practice.1,2,4–6 The majority presents with atypical angina or non-anginal chest pain, with a corresponding low PTP for obstructive CAD.1,2 To increase or decrease the clinical likelihood of CAD, additional tests can be performed.1 In the 2013 European Society of Cardiology (ESC) guidelines on the management of stable CAD, assessing electrocardiography (ECG) changes during exercise with exercise ECG was recommended for patients with an intermediate PTP for obstructive CAD.7 Unfortunately, studies have shown that it has limited power to rule in or rule out obstructive CAD with a sensitivity of 58%, specificity of 62%, and a high rate of inconclusive tests.8,9
Recent guidelines suggest using computed tomography coronary angiography (CTCA) or functional imaging to clarify the presence of CAD, as the diagnostic accuracy is superior to exercise ECG and other functional imaging techniques.1,8 However, there are major challenges in the widespread implementation of CTCA, as it requires substantial investment in computed tomography (CT) technology and personnel training.10,11 In the search for alternatives, the coronary artery calcium (CAC) score has been extensively studied as a predictor of major adverse cardiac events (MACE) in symptomatic patients. Several large observational studies have reported a strong positive association between CAC score and MACE in patients with anginal symptoms and/or dyspnea, with suspected CAD in a non-acute setting.12–14 Compared to patients with a CAC score of zero, patients with CAC score of 1–100, 100–400 and >400 had approximately 2, 3–6 and 5–8 fold increase in MACE, respectively.12–14 Similar associations have been reported in asymptomatic patients.15–19
Because the CAC score is widely available, rapid, and noninvasive with relatively low costs and low radiation doses, it is more accessible than CTCA or functional imaging.20,21 The 2019 ESC guidelines on chronic coronary syndromes state that the CAC score can be used in patients with angina and/or dyspnea in a non-acute setting to increase (CAC score > 0) or decrease (CAC score = 0) the clinical likelihood of CAD, although the optimal use of the CAC score to improve PTP assessment has not been established.1
In the present study, we compared the distribution of CAC scores with clinical symptoms and calculated PTP for obstructive CAD. We assessed the influence of risk factors on CAC scores and aimed to identify patients with the highest risk of elevated CAC scores. Furthermore, we assessed the association between results of CAC score and exercise ECG. Finally, in a subgroup of patients who underwent coronary angiography, we explored the association between results of both CAC score and exercise ECG, and results of coronary angiography.
Methods
Setting and Participants
This retrospective observational cohort study was conducted at Tergooi Medical Center, Hilversum, The Netherlands (Tergooi MC), a general teaching hospital in the Netherlands. We included patients with anginal symptoms and/or dyspnea with a documented CAC score between 1 January 2012 and 30 June 2021. We excluded two patients with a history of myocardial infarction, coronary intervention, or coronary bypass surgery. We excluded three patients in whom anginal symptoms were not specified. CAC scores were requested by a cardiologist at the outpatient clinic of the Tergooi MC in a non-acute setting. A cardiologist could request a CAC score at the outpatient clinic in two patient categories: 1) patients referred by a general practitioner for suspected angina pectoris, predominantly with atypical angina or non-anginal chest pain; and 2) patients at a follow-up visit after presentation to the emergency department for suspected acute coronary syndrome (ACS). In these patients, ACS was ruled-out, but CAD was still suspected. In all patients, CAC score was used as a diagnostic tool to increase or decrease the clinical likelihood of CAD. The decision to perform a CAC score was left at the discretion of the treating cardiologist.
We report the findings of our study according to the STROBE guidelines for observational studies.22 The local research committee of the Tergooi MC approved this study, conforming to the guidelines set out in the Declaration of Helsinki. As this study did not fall within the scope of the Dutch law on medical research involving humans, informed consent from individual participants was not required by the local research committee of the Tergooi MC. Patient data was anonymized and could not directly be traced back to individual participants.
Variables
According to the 2019 ESC guidelines on chronic coronary syndromes, dyslipidemia, diabetes mellitus, hypertension, smoking, and a family history of (premature) cardiovascular disease (CVD) are risk factors for CVD that increase the likelihood of CAD. Data on dyslipidemia, diabetes mellitus, and hypertension were obtained from the hospital medical records. Current smoking status and family history of (premature) CVD were obtained from outpatient clinic visits. Clinical symptoms were collected from hospital medical records. We collected results of the CAC scores. Lastly, we collected results of exercise ECG and coronary angiography that were performed in the six months prior to and following the CAC score.
Categorization of Clinical Symptoms
We categorized patients as typical angina, atypical angina, non-anginal chest pain, or dyspnea, based on symptoms mentioned in the hospital medical records. We used the traditional clinical classification of angina pectoris, which is mentioned in the 2019 ESC guideline for chronic coronary syndromes.1,23 Patients were categorized as typical angina if symptoms met all following three characteristics: 1) constricting discomfort in the front of the chest or in the neck, jaw, shoulder, or arm; 2) precipitated by physical exertion; and 3) relieved by rest or nitrates within 5 min. We categorized patients as atypical angina as the symptoms met two of these characteristics. We categorized patients as non-anginal chest pain as the symptoms met only one or none of these characteristics. If patients experienced dyspnea but their primary symptom was chest pain, we categorized these patients according to the clinical classification of angina pectoris. Patients were categorized as dyspnea if dyspnea was their only or primary symptom.
PTP for Obstructive CAD
For each patient, we calculated PTP for obstructive CAD, which was derived from a pooled analysis of three contemporary study cohorts, and is based on a patients age, sex and the nature of the clinical symptoms in Juarez-Orozco et al.2 We categorized patients into 3 PTP categories, based on the 2019 ESC guideline on chronic coronary syndromes.1 Patients with PTP ≤ 5% were categorized as low PTP, patients with PTP 6–14% were categorized as intermediate PTP and patients with PTP ≥ 15% were categorized as high PTP.
CAC Score
CAC scores were based on ECG-triggered CT scanning using the Agatston method.24 CT scans were performed on a Siemens Somatom AS64. We analysed the CAC score as a categorical variable. We divided patients into 4 categories: 1) CAC score = 0; 2) CAC score 1–99; 3) CAC score 100–399; and 4) CAC score ≥ 400. When multiple CAC scores were performed in the same patient, we only used the first CAC score for analyses.
Exercise ECG
Exercise ECG was performed in the presence of the treating physician, who reported result as abnormal, normal, or inconclusive. Target heart rate was set to 85% of the maximum age-predicted heart rate. Abnormal result was defined as ≥2 mm ST-segment depression in two contiguous leads during exercise. Normal result was defined as reaching the target heart rate without symptoms and without significant ST-segment depression. Exercise ECG was considered inconclusive if the target heart rate was not reached or if the ECG recording was uninterpretable due to artifacts or an abnormal resting ECG, for example, because of pre-existing conduction disorders.
Coronary Angiography
Coronary angiography results were categorized as significant stenosis, non-significant stenosis, wall irregularities, or normal. Significant stenosis was defined as >70% stenosis, or stenosis of 50–70% with either fractional flow reserve (FFR) ≤0.80, or instant flow reserve (IFR) ≤0.89.1,25 Non-significant stenosis was defined as stenosis of 30–50%, or stenosis of 50–70% with either FFR >0.80 or IFR >0.89. Wall irregularities was defined as stenosis of 0–30%. When coronary arteries were smooth and no stenoses were observed, coronary angiography was reported as normal. When abnormalities were observed in multiple arteries, result was reported according to the artery with the most severe abnormalities.
Outcomes
We assessed the distribution of CAC scores across all clinical symptom categories. We compared the result of CAC scores with PTP for obstructive CAD categories. We assessed the association between risk factors that increase the likelihood of CAD (hypertension, hypercholesterolemia, diabetes mellitus, smoking, and family history of (premature) CVD) and the CAC score. We assessed the association between CAC score and exercise ECG results. Finally, we compared the results of CAC scores and exercise ECG with results of coronary angiography.
Statistical methods
Discrete variables are presented as numbers and percentages, normally distributed continuous variables as mean ± standard deviation (SD), and non-normally distributed continuous variables as median and interquartile range (IQR). To test for differences between groups, we used the unpaired t-test for normally distributed variables and Mann–Whitney U-test for non-normally distributed variables. The chi-squared test was used to test for differences in proportions, and Cramer’s V correlation coefficient was used to determine the strength of the associations. When testing for associations between exercise ECG and other variables, we used only the positive and negative results of exercise ECG and excluded inconclusive test results.
To assess whether patients with risk factors had a higher risk of elevated CAC scores, we compared patients with a CAC score > 0 to those with a CAC score of 0. For these analyses, we only included patients with complete data on all risk factors that increase the likelihood of CAD (complete case sample, n = 787). These risk factors were hypertension, hypercholesterolemia, diabetes mellitus, current smoking, and a family history of (premature) CVD. Patient characteristics are shown in Table S1. To test whether patients with multiple risk factors had a higher risk of elevated CAC scores, we calculated odds ratios (OR) and corresponding 95% confidence intervals (95% CI) for patients with one, two or ≥ three risk factors and used patients without risk factors as the reference group. We further stratified the analyses according to PTP category. In a sensitivity analysis, we compared patients with a CAC score ≥ 100 to those with a CAC score of 0 and performed similar analyses.
Statistical significance was set at a 0.05 level. Statistical analyses were performed using R Studio (version 1.3.1093).
Results
In 882 patients with anginal symptoms or dyspnea, CAC score was calculated for assessment of CAD and were included in this study. The details of the inclusion of patients per year during the study period are shown in Figure S1. Mean age was 53.5 years (SD ± 10.2 years) and 28.1% were male. Other patient characteristics are shown in Table 1.
 |
Table 1 Patient Characteristics Study Population |
Main reasons for performing a CAC score were non-anginal chest pain (65.2%) and atypical angina (20.1%). Typical angina (3.5%) and dyspnea (11.2%) were less common indications. Of all patients, 501 (56.8%) had CAC score of 0, 265 (30.0%) had CAC score of 1–99, 82 (9.3%) had CAC score of 100–399 and 34 (3.9%) had CAC score ≥ 400.
Figure 1 shows the distribution of the CAC scores per clinical symptom category. CAC scores were equally distributed among patients with non-anginal chest pain, atypical angina, and dyspnea. The majority of these patients (50–59%) had a CAC score of zero. Only 8–9% had CAC score of 100–399 and a fraction (3–5%) had a CAC score ≥ 400. In patients with typical angina higher CAC scores were seen. Still, 29% of these patients had CAC score of zero.
 |
Figure 1 Distribution of CAC score per clinical symptom category based on the 2019 ESC guideline on chronic coronary syndromes: non-anginal chest pain, atypical angina, typical angina or dyspnea. |
PTP for Obstructive CAD
Of all patients, 400 (45.4%) had low, 391 (44.3%) had intermediate, and 91 (10.3%) had high PTP for obstructive CAD. The distribution of CAC scores across PTP categories is shown in Figure 2. There was a statistically significant positive association between CAC scores and PTP (Cramer’s V = 0.29, p < 0.0001). In patients with low PTP, the majority had a CAC score of zero (72.5%), and only a small proportion had a CAC score ≥ 100. In patients with intermediate PTP, half had a CAC score of zero and 15.6% had a CAC score ≥ 100. The highest CAC scores were observed in patients with high PTP. However, 19.8% of the patients with high PTP had a CAC score of zero.
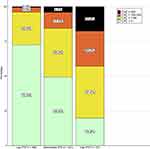 |
Figure 2 Distribution of CAC scores across PTP for CAD categories. |
Risk Factors and Risk of Elevated CAC Score
Patients with a CAC score > 0 were significantly more likely to be male, were older, and more often had hypertension, hypercholesterolemia, and diabetes mellitus than patients with a CAC score of 0 (Table 2). There were no significant differences in smoking status or family history of CVD. We stratified the results for each PTP category and observed similar results, particularly in patients with low and intermediate PTP (Table S2).
 |
Table 2 Characteristics of Patients with CAC Score of 0 and CAC Score > 0 |
Compared to patients without risk factors, OR for CAC score > 0 for patients with 1, 2 or ≥3 or more risk factors were 1.86 (95% CI 1.29–2.68), 2.67 (95% CI 1.79–4.01) and 4.34 (95% CI 2.55–7.51) respectively (Table 3). We stratified the results for each PTP category and observed similar results in the patients with low and intermediate PTP. In patients with high PTP, there was no clear interaction, probably because of the low number of patients and the high baseline risk for elevated CAC score in this group. Sensitivity analysis comparing patients with a CAC score ≥ 100 to patients with a CAC score = 0 showed similar results (Tables S3-S5).
 |
Table 3 Association Between Number of Risk Factors and Elevated CAC Score (CAC Score > 0) |
Comparing CAC Score with Exercise ECG
An exercise ECG was performed in 556 symptomatic patients (63%) with reported CAC scores. Almost all exercise ECGs were performed prior to the CAC score (546/556, 98.2%). Differences in characteristics between patients with and without exercise ECG are shown in Tables S6 and S7.
Of all exercise ECG tests, 381 (68.5%) were normal, 29 (5.2%) were abnormal, and 141 exercise ECG tests (25.4%) were inconclusive. In five patients (0.9%), result of exercise ECG was not reported, and were therefore excluded from further analyses. Of the patients with normal exercise ECG, 11.0% had a CAC score of 100–399, and 2.6% had a CAC score ≥ 400 (Figure 3). Higher CAC scores were observed in patients with abnormal exercise ECG test, but association was weak and statistically not significant (Cramer’s V = 0.13, p = 0.08). Moreover, 41.4% of patients with an abnormal exercise ECG had CAC score of zero.
 |
Figure 3 Results of CAC scores compared to results of exercise ECG. For each exercise ECG result (normal, abnormal, inconclusive) we showed the distribution of CAC scores. |
Comparing CAC Score and Exercise ECG with Results of Coronary Angiography
In total, 381 (43.2%) patients had a CAC score > 0. Coronary angiography was performed in 92 of these patients (24.1%). There was a moderate positive association between CAC score and abnormalities on coronary angiography (Cramer’s V = 0.43, p < 0.0001). In patients with CAC score of 1–99, majority (56%) had normal coronary angiography and only one patient (4%) had a significant stenosis, while in patients with CAC score ≥ 400, 38.5% had a significant stenosis and none of the patients had a normal coronary angiography (Figure 4).
In 62/92 patients (67.4%) with coronary angiography, exercise ECG was performed (all prior to coronary angiography). We compared the results of the coronary angiography and exercise ECG (Figure 5). There was no association between results of exercise ECG and coronary angiography (Cramer’s V = 0.11, p = 0.91).
Discussion
In this observational clinical practice-based study on the use of the CAC score in patients with angina and/or dyspnea, who are suspected of having CAD in a non-acute setting, we showed that the majority of patients had a CAC score of zero, especially those with low and intermediate PTP for obstructive CAD. However, 20% of the patients with high PTP had a CAC score of zero. Patients with multiple risk factors had a higher risk of elevated CAC score, especially those with low and intermediate PTP. Furthermore, we showed a significant association between CAC score and coronary angiography results, whereas no association was found between exercise ECG and coronary angiography. These results can help optimize the use of the CAC score in clinical practice. Moreover, these results can be used to identify patients who are most likely to have (highly) elevated CAC scores.
In patients with low PTP, almost three-quarters had a CAC score of zero and only a fraction (4%) had a CAC score ≥ 100. In these patients, diagnostic testing may be deferred, especially when there are no risk factors that increase the likelihood of CAD. However, in clinical practice a patient or clinician might still want more assurance in excluding CAD when there are risk factors that increase the likelihood of CAD. In these cases, CAC score is a simple and effective tool, and obstructive CAD can be excluded in the majority of patients. Among patients with low PTP and zero or one risk factor(s), only a few patients had a CAC score ≥ 100, whereas patients with multiple risk factors were more likely to have a CAC score ≥ 100. This might indicate that the CAC score should be used in patients with low PTP only when multiple risk factors are present.
Among the patients with intermediate PTP, half had a CAC score of zero. In this group, a higher proportion (16%) of patients had a CAC score ≥ 100. Similar to patients with low PTP, those with multiple risk factors had the highest risk of elevated CAC score.
Highest CAC scores were observed in patients with high PTP. Nevertheless, 20% had a CAC score of zero. As this involved almost exclusively patients with zero or one risk factor(s), the CAC score could be used to lower the likelihood of CAD in these patients. In patients with multiple risk factors, few had a CAC score of zero, and the CAC score could only be used to determine the extent of CAC.
As over 70% of our study population were females, this shows that in clinical practice, clinicians are most likely to perform CAC scores in females. A possible explanation would be the growing attention to sex differences in cardiovascular disease.26 Women often present with other symptoms than men, with (typical) angina being less frequently reported, and these symptoms can also be caused by other conditions.26 Therefore, it can be difficult to distinguish whether these symptoms originate from CAD. In such cases, a clinician may use the CAC score to increase or decrease the clinical likelihood of obstructive CAD.
In further analyses, we compared the CAC score with results of exercise ECG, and compared both to results of coronary angiography. First, we observed a high rate of inconclusive exercise ECG results (25%). Second, patients with an abnormal exercise ECG had somewhat higher CAC scores, although the association was weak and not statistically significant. Moreover, more than 40% of patients with abnormal exercise ECG had CAC score of zero. Third, there was no association between exercise ECG and coronary angiography. In contrast, higher CAC scores were significantly associated with more severe abnormalities on coronary angiography. Previous studies have also reported a low diagnostic accuracy of exercise ECG for detecting CAD and a high rate of inconclusive tests.8,9 Therefore, we suggest using the CAC score in the diagnostic work-up of chest pain rather than exercise ECG to increase or decrease the likelihood of CAD.
Previous studies have incorporated the CAC score, in addition to PTP and risk factors, into a single risk model to predict cardiovascular events and mortality.27,28 In these studies, adding the CAC score improved risk stratification, mostly by identifying individuals at low risk for events. Furthermore, we observed a clear association between CAC score and coronary angiography results. This is consistent with findings from previous studies on symptomatic patients in a non-acute setting, where higher CAC scores were found to be strongly and independently associated with an increased risk for MACE.12–14 It should be noted that a CAC score of zero does not fully exclude significant coronary stenosis from a non-calcified lesion, although the prevalence of obstructive stenosis ≥70% on CTCA was only 1.4% when the CAC score was zero.29
Strengths and Limitations
The results of our study were based on real-life data, which improves the generalizability of our results. However, this study had several limitations. First, as this was a retrospective study, clinical symptoms were based on hospital medical records. Although symptoms were generally well documented, it is possible that not all symptom characteristics were provided in all cases, with consequently an underrepresentation of patients with typical angina. Second, due to the retrospective study design, we could not assess reasons for performing or not performing CAC score and exercise ECG. Third, coronary angiography was performed in one-quarter of all patients with a CAC score > 0. Unfortunately, we could not assess the extent to which the (combination of) results of CAC score and exercise ECG played a role in the decision to perform coronary angiography. Information on other influencing factors was also not available. For example, a clinician might proceed to additional diagnostics faster when a patient has continuous symptoms during follow-up. Fourth, no data were available on patients with exercise ECG in whom CAC score was not performed. Therefore, we were unable to validate whether association between exercise ECG and coronary angiography was absent in patients without CAC scores. Fifth, most patients in the hospital catchment area are Caucasians. People of Caucasian descent generally have a higher CAC score than people of other ethnicities.30 Therefore, our results might be different in populations of other ethnicities.
Conclusion
In this clinical practice study, we showed that CAC score can be used in addition to PTP for obstructive CAD to increase or decrease the clinical likelihood of CAD. Furthermore, CAC score might be more useful in the diagnostic work-up of chest pain than exercise ECG.
Data Sharing Statement
The data underlying this article will be shared upon reasonable request by the corresponding author.
Funding
The manuscript was funded by an unrestricted grant provided by the Tergooi Academy, Tergooi Medical Center, the Netherlands, for the PhD project of the main author, M. Patrick Witvliet.
Disclosure
The authors report no relationships that could be construed as a conflict of interest.
References
1. Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes: the task force for the diagnosis and management of chronic coronary syndromes of the European society of cardiology (ESC). Eur Heart J. 2019;41:407–477. doi:10.1093/eurheartj/ehz425
2. Juarez-Orozco LE, Saraste A, Capodanno D, et al. Impact of a decreasing pre-test probability on the performance of diagnostic tests for coronary artery disease. Europ Heart J. 2019;20:1198–1207. doi:10.1093/ehjci/jez054
3. Abidov A, Rozanski A, Hachamovitch R, et al. Prognostic significance of dyspnea in patients referred for cardiac stress testing. New Engl J Med. 2005;353:1889–1898. doi:10.1056/NEJMoa042741
4. Cheng VY, Berman DS, Rozanski A, et al. Performance of the traditional age, sex, and angina typicality-based approach for estimating pretest probability of angiographically significant coronary artery disease in patients undergoing coronary computed tomographic angiography: results from the multinational coronary CT angiography evaluation for clinical outcomes: an international multicenter registry (CONFIRM). Circulation. 2011;124:2423–2432, 2421–2428. doi:10.1161/circulationaha.111.039255
5. Genders TS, Steyerberg EW, Hunink MG, et al. Prediction model to estimate presence of coronary artery disease: retrospective pooled analysis of existing cohorts. BMJ. 2012;344:e3485. doi:10.1136/bmj.e3485
6. Reeh J, Therming CB, Heitmann M, et al. Prediction of obstructive coronary artery disease and prognosis in patients with suspected stable angina. Eur Heart J. 2018;40:1426–1435. doi:10.1093/eurheartj/ehy806
7. Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European society of cardiology. Eur Heart J. 2013;34:2949–3003. doi:10.1093/eurheartj/eht296
8. Knuuti J, Ballo H, Juarez-Orozco LE, et al. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis in patients with stable angina: a meta-analysis focused on post-test disease probability. Eur Heart J. 2018;39:3322–3330. doi:10.1093/eurheartj/ehy267
9. Singh T, Bing R, Dweck MR, et al. Exercise electrocardiography and computed tomography coronary angiography for patients with suspected stable angina pectoris: a post hoc analysis of the randomized scot-HEART trial. JAMA Cardiol. 2020;5:920–928. doi:10.1001/jamacardio.2020.1567
10. Moss AJ, Williams MC, Newby DE, Nicol ED. The updated NICE guidelines: cardiac CT as the first-line test for coronary artery disease. Curr Cardiovasc Imaging Rep. 2017;10:15. doi:10.1007/s12410-017-9412-6
11. Nicol EPS, Roditi G, Roobottom C; On behalf of the British Society of Cardiovascular Imaging / British Society of Cardiovascular Computed Tomography. The challenge of national CT coronary angiography (CTCA) provision in response to NICE CG95 update; 2016. Available from: https://bsci.org.uk/standards-and-guidelines/nice-cg95-update-2016/.
12. Al-Mallah MH, Qureshi W, Lin FY, et al. Does coronary CT angiography improve risk stratification over coronary calcium scoring in symptomatic patients with suspected coronary artery disease? Results from the prospective multicenter international CONFIRM registry. Europ Heart J. 2013;15:267–274. doi:10.1093/ehjci/jet148
13. Bom MJ, Van der Zee PM, Van der Zant FM, Knol RJJ, Cornel JH. Independent prognostic value of coronary artery calcium score and coronary computed tomography angiography in an outpatient cohort of low to intermediate risk chest pain patients. Netherlands Heart J. 2016;24:332–342. doi:10.1007/s12471-016-0819-5
14. Engbers EM, Timmer JR, Ottervanger JP, Mouden M, Knollema S, Jager PL. Prognostic value of coronary artery calcium scoring in addition to single-photon emission computed tomographic myocardial perfusion imaging in symptomatic patients. Circ Cardiovasc Imaging. 2016;9:e003966. doi:10.1161/CIRCIMAGING.115.003966
15. Budoff MJ, Young R, Burke G, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (Mesa). Eur Heart J. 2018;39:2401–2408. doi:10.1093/eurheartj/ehy217
16. Carr JJ, Jacobs DR Jr, Terry JG, et al. Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol. 2017;2:391–399. doi:10.1001/jamacardio.2016.5493
17. Paixao ARM, Ayers CR, El Sabbagh A, et al. Coronary artery calcium improves risk classification in younger populations. JACC Cardiovasc Imaging. 2015;8:1285–1293. doi:10.1016/j.jcmg.2015.06.015
18. Tota-Maharaj R, Blaha MJ, McEvoy JW, et al. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J. 2012;33:2955–2962. doi:10.1093/eurheartj/ehs230
19. Yano Y, O’Donnell CJ, Kuller L, et al. Association of coronary artery calcium score vs age with cardiovascular risk in older adults: an analysis of pooled population-based studies. JAMA Cardiol. 2017;2:986–994. doi:10.1001/jamacardio.2017.2498
20. Lo-Kioeng-Shioe MS, Rijlaarsdam-Hermsen D, van Domburg RT, et al. Prognostic value of coronary artery calcium score in symptomatic individuals: a meta-analysis of 34,000 subjects. Int J Cardiol. 2020;299:56–62. doi:10.1016/j.ijcard.2019.06.003
21. Halliburton SS, Abbara S, Chen MY, et al. SCCT guidelines on radiation dose and dose-optimization strategies in cardiovascular CT. J Cardiovasc Comput Tomogr. 2011;5:198–224. doi:10.1016/j.jcct.2011.06.001
22. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi:10.1016/j.jclinepi.2007.11.008
23. Diamond GA. A clinically relevant classification of chest discomfort. J Am Coll Cardiol. 1983;1:574–575. doi:10.1016/S0735-1097(83)80093-X
24. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi:10.1016/0735-1097(90)90282-T
25. Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2010;31:2501–2555. doi:10.1093/eurheartj/ehq277
26. Meyer MR. Chronic coronary syndromes in women: challenges in diagnosis and management. Mayo Clinic Proceed. 2021;96:1058–1070. doi:10.1016/j.mayocp.2020.09.023
27. Meng J, Jiang H, Ren K, Zhou J. Comparison of risk assessment strategies incorporating coronary artery calcium score with estimation of pretest probability to defer cardiovascular testing in patients with stable chest pain. BMC Cardiovasc Disord. 2023;23:53. doi:10.1186/s12872-023-03076-3
28. Winther S, Schmidt SE, Foldyna B, et al. Coronary calcium scoring improves risk prediction in patients with suspected obstructive coronary artery disease. J Am Coll Cardiol. 2022;80:1965–1977. doi:10.1016/j.jacc.2022.08.805
29. Villines TC, Hulten EA, Shaw LJ, et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT angiography evaluation for clinical outcomes: an international Multicenter) registry. J Am Coll Cardiol. 2011;58:2533–2540. doi:10.1016/j.jacc.2011.10.851
30. McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: results from the multi-ethnic study of atherosclerosis (Mesa). Circulation. 2006;113:30–37. doi:10.1161/circulationaha.105.580696
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.