Back to Journals » Research and Reports in Neonatology » Volume 14
Vitamin D Status of Preterm Newborns at Approximately 4 Weeks of Age in Shenzhen, China: A Retrospective Observational Cohort Study Conducted Across Two Centers
Authors Guo Y , Yu Z, Tu H, Zheng B, Li J, Liu Y
Received 17 November 2023
Accepted for publication 27 February 2024
Published 6 March 2024 Volume 2024:14 Pages 59—66
DOI https://doi.org/10.2147/RRN.S450403
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Schelonka
Yanping Guo,1 Zhangbin Yu,2 Huiying Tu,2 Biying Zheng,1 Jiamin Li,1 Ying Liu1
1Department of Pediatrics, Peking University Shenzhen Hospital, Shenzhen, Guangdong, People’s Republic of China; 2Department of Neonatology, Shenzhen People’s Hospital (The Second Clinical Medical College, Jinan University, the First Affiliated Hospital, Southern University of Science and Technology), Shenzhen, Guangdong, People’s Republic of China
Correspondence: Yanping Guo; Ying Liu, Tel +86-15919990131 ; +86-13902992158, Email [email protected]; [email protected]
Background and Objectives: To examine the correlation between the concentration of vitamin D (VD) in venous blood at approximately 4 weeks of age (± 4 weeks of age) and neonatal outcomes in preterm infants (birth weight < 1500 g or gestational age < 32 weeks) in two neonatal intensive care units (NICUs) located in Shenzhen, China.
Methods and Study Design: Preterm infants were split into two groups based on their VD concentration at ± 4 weeks of age: VD insufficiency (VDI) group (≤ 20 ng/mL) and VD sufficient (VDS) group (> 20 ng/mL). Binary logistic regression analysis was used to examine relationships between outcomes and VDI.
Results: Of 230 infants in total, 119 (51.7%) were assigned to the VDI group and 111 to the VDS group (48.3%). No correlation was found between serum VD at ± 4 weeks of age and gestational age (p> 0.05). The starting point of the two groups for oral VD intake did not differ significantly (p> 0.05). At ± 4 weeks of age, oral VD dose (P< 0.05) was greater in the VDS group. Gestational diabetes mellitus was associated with VDI (OR=1.94, 95% CI 1.01– 3.75, p=0.047) after controlling for this risk. Following correction for gestational age and oral VD dosage at ± 4 weeks old, VDI was also linked to a significant risk of retinopathy of prematurity (OR=2.00, 95% CI 1.08– 3.68, p< 0.027).
Conclusion: Preterm newborns (gestational age < 32 weeks or birth age < 1500 g) in NICUs in Shenzhen, China continue to have significantly high VDI. Higher VDI is associated with gestational diabetes mellitus and retinopathy of prematurity.
Keywords: very preterm birth, very low birth weight infant, vitamin D, 4 weeks of age, outcome
Introduction
Vitamin D insufficiency (VDI) is prevalent in premature babies. In very preterm newborns, the incidence of VDI at birth can reach around 70%, due to early pregnancy termination and lack of a source of VD.1,2 VD is crucial to calcium homeostasis, bone health, and overall health.3–6 The most accurate indicator of VD deficiency is 25-hydroxyvitamin D (25-OH-D), which is the predominant and more stable form of VD circulating in the blood.7 Research has established a link between VD deficit and preterm birth, and VDI also has a negative impact on pregnancy outcomes.8 Therefore, it is essential to regularly monitor the VD status of preterm newborns and to supplement VD in a timely and acceptable manner. Serum 25-OH-D concentration have been measured approximately 4 weeks after birth in clinical studies conducted both domestically and in other countries to determine the VD status of preterm infants.9,10 The aim of this study was to retrospectively examine the VD status at about 4 weeks postpartum [gestational age (GA) <32 weeks or birth weight (BW) <1500 g] in preterm newborns, assess its risk factors, and assess its influence on the major problems of preterm children.
Methods
Participants
This study was an observational cohort, retrospective, two-center investigation. The study included all newborns admitted to the neonatology departments of Peking University Shenzhen Hospital and Shenzhen People’s Hospital between January 1, 2020 and December 31, 2022. All newborns with a GA of less than 32 weeks or a BW of less than 1500 g who were hospitalized for more than or equal to 28 days and who survived at 36 weeks’ postmenstrual age were included in the research cohort. Exclusion criteria included missing clinical data, congenital anomalies, congenital chromosomal or genetic metabolic illnesses, and failure to test 25-OH-D concentration in venous blood at about 4 weeks of age. Additionally, infants who died during the trial were not included. The hospital’s academic ethics committee accepted this study without the need to obtain informed consent {Peking University Shenzhen Hospital Ethics Review (Research) [2019] No. (019-Revision 2)}.
Data Collection
Maternal age, method of conception, pregnancy-induced hypertension (PIH), and gestational diabetes mellitus (GDM) were among the maternal data gathered. Data about newborns, such as sex, BW, GA, delivery method, and multiple births (twins or more), were gathered. Records were kept on the usage of pulmonary surfactant (PS), length of stay, oral VD intake time, oral VD intake dose, and serum 25-OH-D concentration at approximately 4 weeks (±4 weeks) postpartum. A number of conditions potentially lead to poor outcomes in neonates, including periventricular leukomalacia in preterm infants (PVL), neonatal respiratory distress syndrome (NRDS), intraventricular hemorrhage (IVH), necrotizing enterocolitis (NEC), respiratory distress syndrome (RDS), early onset sepsis (EOS), late onset sepsis (LOS), and bronchopulmonary dysplasia (BPD), and these were all considered in this study.
Measurements
On the day of blood collection, the hospital laboratory used an Access 25(OH) Vitamin D Total test to measure the concentration of serum 25-OH-D (Roche Cobas e601 automatic electrochemiluminescence immunoanalyzer and LIAISON® XL automatic immunochemiluminescence immunoanalyzer). The Access 25(OH) Vitamin D Total assay, which integrates 25-OH-D2 and 25-OH-D3 to determine total 25-OH-D concentrations directly, is a paramagnetic particle chemiluminescent immunoassay that serves as the best analyte for assessing VD status overall.
Standards and Definitions
Serum concentration of less than 20 ng/mL indicated VDI, with serum concentration of more than 20 ng/mL indicating VD adequacy.
The Expert Consensus on Diagnosis and Treatment of Neonatal Sepsis (version 2019)11 was used for diagnostic standards for EOS and LOS. The Practice of Neonatology (5th Edition)12 provided the diagnostic standards for RDS, IVH, NEC, retinopathy of prematurity (ROP), and PVL. Various definitions of BPD were used in our study. BPD (2001) was classed as mild, moderate, or severe and was defined as the need for supplemental oxygen for 28 days or longer.13 BPD (2018) was defined as the need for respiratory support for at least 3 days, according to the revised GA of 36 weeks.14 To determine the most appropriate diagnostic standards for BPD, Jensen et al carried out a comprehensive multicenter clinical analysis in 2019.15,16 In our study, only oxygen flow was taken into account for grading BPD (2019), not oxygen concentration. Survival without major morbidity was defined as survival in the absence of any the serious morbidities indicated in the Data collection section.17
Statistical Analysis
Medians [M (Q1, Q3)] or percentages were used to express demographic information. Spearman correlation was employed for analysis. We used the chi-square test or the Kruskal–Wallis test in the univariate analysis. After adjusting for variables in the univariate analysis, we performed a logistic regression analysis to determine the odds ratios (OR) based on the presence of VD. P<0.05 was deemed statistically significant. SPSS v.18.0 was used to perform the statistical analyses (SPSS Inc., Chicago, Illinois).
Results
Participant Attributes
A total of 454 in-born with a GA <32 weeks or BW <1500 g were included. Of these, 137 with missing serum 25-OH-D data at ±4 weeks of age and 87 babies who were hospitalized for fewer than 28 days were excluded. This left the data of 230 newborns for analysis (Figure 1).
 |
Figure 1 Flow chart for the population under study. |
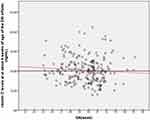
Vitamin D Concentrations at Approximately 4 Weeks of Age
Figure 2 displays the distribution of serum VD levels in the 230 newborns at ±4 weeks of age. At this age, the mean serum 25-OH-D level was 19.8 (15.9, 23.8) ng/mL (Table 1). Table 1 shows that 119 newborns (51.7%) were in the VDI group and 111 infants (48.3%) were in the vitamin D sufficient (VDS) group. At ±4 weeks of age, there was no correlation between GA and 25-OH-D level (Rs=–0.1, p=0.131) (Figure 2).
 |
Table 1 Traits of Premature Babies and Levels of Vitamin D at Approximately 4 Weeks of Life |
Relationship Between Risk Factors and VDI
Lower VD levels were associated with a higher probability of GDM (p=0.018) and with a lower oral dosage of VD (p=0.012) at ±4 weeks of age (Tables 1 and 2). Nevertheless, following multivariable linear regression and correction for the oral intake dose of VD at ±4 weeks of age, only GDM was found to be significant (OR 1.94, 95% CI 1.01–3.75, p<0.05) (Table 3).
 |
Table 2 Risk Variables and VD Levels at ±4 Weeks of Age Analyzed Using Univariate Binary Regression |
 |
Table 3 Multivariate Binary Regression Analysis of Risk Variables and VD Levels After Controlling for Oral VD Intake Dose at ±4 Weeks of Age |
Relationship Between Significant Morbidity and VDI in Premature Newborns
Following multivariable linear regression, with correction for GA and the oral intake dose of VD at ±4 weeks of age, VDI was also linked to a high risk of ROP (OR=2.00, 95% CI 1.08–3.68, p<0.05) (Table 4).
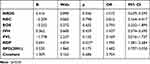 |
Table 4 Results of Multivariate Binary Regression Analysis Performed to Determine Primary Complications and VD Levels After Adjusting for GA and Oral Dosage of VD at ±4 Weeks of Age |
Discussion
This was a retrospective, two-center, observational cohort study exploring VD status ±4 weeks postpartum (BW <1500 g or GA <32 weeks), assessing its risk factors, and assessing its influence on the major complications of preterm infants at Shenzhen People’s Hospital and Peking University Shenzhen Hospital in China. According to our research, 51.7% of preterm infants who consistently received the recommended dose of VD after delivery were still VD deficient at the age of 4 weeks. The results of other studies have varied, owing to inconsistent detection techniques and VDI cut-off values; however, the prevalence of VD deficiency has been found to be more than half of infants, reaching as high as 80%.18–20
According to our univariate analysis, there was a higher intake of VD in the VDS group at ±4 weeks of age, which was also consistent with clinical practice and related to the dose dependence of VD. The oral intake dose of VD at 4 weeks of age was also closely related to the level of VD at 4 weeks of age (p<0.05). We discovered no correlation between GA and VD content in venous blood at ±4 weeks of age (Figure 2).This could be connected to the lengthier intravenous feeding of multivitamins in preterm children with lower GAs, as well as the increased oral VD consumption in infants with an increase in alkaline phosphatase concentration 2 weeks after delivery.21–23 Furthermore, the univariate analysis indicated a strong correlation between VDI and PIH (P<0.05). However, the multivariable analysis revealed that the association between the two variables was not statistically significant (P>0.05), potentially attributable to the presence of multiple confounding factors.
The multivariate analysis revealed a relationship between VDI and GDM after correcting for the oral intake dose of VD at ±4 weeks of age. Many studies have demonstrated that low levels of VD during pregnancy can result in low levels of VD in premature infants after they are born.24–26 According to Milan et al,27 GDM patients had lower serum VD levels and serum VD was negatively correlated with their fasting blood glucose levels. Additionally, higher expression of genes linked to VD resistance was seen in GDM patients, and this expression was inversely correlated with serum VD levels. Ali Khan et al28 discovered that pregnant women with GDM had low serum VD levels, which may be directly linked to the functional genetic variation of the VD receptor gene. Owing to the retrospective nature of our research, data on the status and degree of VD supplementation during pregnancy could not be gathered. Therefore, to better understand VDI in premature infants in Shenzhen, we are developing a prospective large-sample multicenter cohort study.
After controlling for the interaction of gestational age at birth and total vitamin D dose, multivariable regression revealed a strong correlation between VDI and risk for ROP. This finding aligns with prior studies. Kabataş et al29 determined that there is an inverse correlation between 25-OH-D levels and risk of ROP development and treatment requirement. Low vitamin D levels might have a role in the aetiopathogenesis of ROP in premature infants. Boskabadi et al30 found that Low serum levels of vitamin D in premature infants and their mothers were associated with incidence of ROP. The higher the stage of ROP, the greater was the severity of vitamin D deficiency. As vitamin D directly affects the vascular endothelial stability, its deficiency will most likely affect the incidence of ROP in premature infants who are at risk of vitamin D deficiency. The inflammatory and angiogenic effects of vitamin D deficiency can cause early damage to the retinal blood vessels. Greater risk for ROP in VDI infants, could be related to the antioxidant effects and improved micronutrient and mineral absorption.31 The incidence of additional unfavorable outcomes, including as RDS, NEC, EOS, IVH, PVL, and BPD (2001, 2018, 2019), did not differ statistically significantly between the two groups (Tables 1 and 4). There was no correlation between these outcomes and VD levels. This aligns with the findings of earlier research.32 Additionally, research has demonstrated a strong correlation between preterm outcomes and low VD levels.33,34 However, the results of studies vary greatly from one another, which may be directly related to research techniques, sample size, and GA in the studies.
Our study had some limitations. First, it was a two-center, retrospective study. Second, the sample size was small due to the large number of cases for which venous blood 25-OH-D concentration was not recorded at ±4 weeks after birth. Many clinical data cannot be collected prospectively. Our next research project will be to conduct a prospective multicenter homogenization study to assess VD status in preterm infants in Shenzhen and determine the effects of VD supplementation in preterm infants of different gestational ages.
Conclusion
In neonatal intensive care units in Shenzhen, China, preterm newborns (BW <1500 g or GA <32 weeks) still have a very high rate of VDI. An increased risk of VDI was associated with GDM and ROP.
Data Sharing Statement
The corresponding author may obtain any data from the study upon reasonable request, [email protected] (Yanping Guo).
Acknowledgments
We are grateful to all the children and their families for participating in this research.
Funding
This work was supported by the General Program for Clinical Research at Peking University Shenzhen Hospital [grant number LCYJ2020013]. Clinical trial registration number: ChiCTR2100048293.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Kiely ME, Wagner CL, Roth DE. Vitamin D in pregnancy: where we are and where we should go. J Steroid Biochem Mol Biol. 2020;201:105669. doi:10.1016/j.jsbmb.2020.105669
2. Abrams SA. Vitamin D in preterm and full-term infants. Ann Nutr Metab. 2020;76(Suppl 2):6–14. doi:10.1159/000508421
3. Bhattoa HP, Konstantynowicz J, Laszcz N, et al. Vitamin D: musculoskeletal health. Rev Endocr Metab Disord. 2017;18(3):363–371. doi:10.1007/s11154-016-9404-x
4. Yuan C, Qu C, Ji W. Vitamin D supplementation for improving children with bone mineral density: a protocol for systematic review and meta-analysis. Medicine. 2020;99(52):e23475. doi:10.1097/MD.0000000000023475
5. Sassi F, Tamone C, D’Amelio P. Vitamin D: nutrient, hormone, and immunomodulator. Nutrients. 2018;10(11):1656. doi:10.3390/nu10111656
6. Bikle DD. Vitamin D Regulation of Immune Function. Curr Osteoporos Rep. 2022;20(3):186–193. doi:10.1007/s11914-022-00732-z
7. Tripathi A, Ansari M, Dandekar P, Jain R. Analytical methods for 25-hydroxyvitamin D: advantages and limitations of the existing assays. J Nutr Biochem. 2022;109:109123. doi:10.1016/j.jnutbio.2022.109123
8. Woo J, Giurgescu C, Wagner CL. Evidence of an Association Between Vitamin D Deficiency and Preterm Birth and Preeclampsia: a Critical Review. J Midwifery Women's Health. 2019;64(5):613–629. doi:10.1111/jmwh.13014
9. Yanmei C, Xin-Zhu L, Rong Z, et al. Expert consensus on Clinical management of metabolic bone disease in preterm infants (2021). Chin J Contemp Pediatr. 2021;23(8):761–772. doi:10.7499/j.issn.1008-8830.2105152
10. Faienza MF, D’Amato E, Natale MP, et al. Metabolic Bone Disease of Prematurity: diagnosis and Management. Front Pediatr. 2019;7:143. doi:10.3389/fped.2019.00143
11. Neonatology Group, Pediatrics Branch of Chinese Medical Association, Infection Professional Committee of Neonatology Branch of Chinese Medical Doctor Association. Expert Consensus on diagnosis and Treatment of neonatal sepsis (2019 edition). Chin J Pediatr. 2019;57(4):252–257. doi:10.3760/cma.j.issn.0578-1310.2019.04.005
12. Shao X-M, H-m Y, X-s Q. Practice of Neonatology.
13. Jobe AH, Bancalari E. Bronchopulmonary dysplasia[J]. Am J Respir Crit Care Med. 2001;163(7):1723–1729. doi:10.1164/ajrccm.163.7.2011060
14. Higgins RD, Jobe AH, Koso-Thomas M, et al. Bronchopulmonary Dysplasia: executive Summary of a Workshop. J Pediatr. 2018;197:300–308. doi:10.1016/j.jpeds.2018.01.043
15. Jensen EA. Prevention of Bronchopulmonary Dysplasia: a Summary of Evidence-Based Strategies. Neoreviews. 2019;20(4):e189–e201. doi:10.1542/neo.20-4-e189
16. Jensen EA, Dysart K, Gantz MG, et al. The Diagnosis of Bronchopulmonary Dysplasia in Very Preterm Infants. An Evidence-based Approach. Am J Respir Crit Care Med. 2019;200(6):751–759. doi:10.1164/rccm.201812-2348OC
17. Poryo M, Maas S, Gortner L, et al. Effects of small for gestational age status on mortality and major morbidities in ≤750 g neonates. Early Hum Dev. 2020;144:105040. doi:10.1016/j.earlhumdev.2020.105040
18. Munshi UK, Graziano PD, Meunier K, Ludke J, Rios A. Serum 25 Hydroxy Vitamin D Levels in Very Low Birth Weight Infants Receiving Oral Vitamin D Supplementation. J Pediatr Gastroenterol Nutr. 2018;66(4):676–679. doi:10.1097/MPG.0000000000001831
19. Tofe-Valera I, Pérez-Navero JL, Caballero-Villarraso J, Cañete MD, Villa-Jiménez R, De la Torre-Aguilar MJ. Vitamin d deficiency with high parathyroid hormone levels is related to late onset SEPSIS among preterm infants. BMC Pregnancy Childbirth. 2023;23(1):23. doi:10.1186/s12884-022-05334-2
20. Chebet M, Piloya T, Ameda F, Mukunya D, Kiguli S. Vitamin D deficiency in low-birth-weight infants in Uganda; a cross sectional study. PLoS One. 2022;17(11):e0276182. doi:10.1371/journal.pone.0276182
21. Hsu PC, Tsao PN, Chou HC, Huang HC, Yen TA, Chen CY. Sodium Glycerophosphate Use in Parenteral Nutrition Improves Mineral Metabolism in Extremely Low Birth Weight Infants. J Pediatr. 2023;253:63–71.e2. doi:10.1016/j.jpeds.2022.09.017
22. Perrone M, Casirati A, Stagi S, et al. Don’t Forget the Bones: incidence and Risk Factors of Metabolic Bone Disease in a Cohort of Preterm Infants. Int J Mol Sci. 2022;23(18):10666. doi:10.3390/ijms231810666
23. Adnan M, Wu SY, Khilfeh M, Davis V. Vitamin D status in very low birth weight infants and response to vitamin D intake during their NICU stays: a prospective cohort study. J Perinatol. 2022;42(2):209–216. doi:10.1038/s41372-021-01238-9
24. Motlagh AJ, Davoodvandi A, Saeieh SE. Association between vitamin D level in mother’s serum and the level of vitamin D in the serum of pre-term infants. BMC Pediatr. 2023;23(1):97. doi:10.1186/s12887-023-03854-0
25. Kwon KW, Lee YH, Yeo MH, et al. Maternal and Fetal Effects of Gestational Vitamin D Concentration. Healthcare. 2023;11(16):2325. doi:10.3390/healthcare11162325
26. Dorreh F, Ahmadi R, Absalan A, et al. High prevalence of hypovitaminosis D3 among pregnant women in central Iran: correlation with newborn vitamin D3 levels and negative association with gestational age. Obstet Gynecol Sci. 2023;66(5):395–406. doi:10.5468/ogs.22251
27. Milan KL, Jayasuriya R, Harithpriya K, et al. Impact of vitamin D resistance genes on vitamin D deficiency during pregnancy among the South Indian population. J Reprod Immunol. 2023;160:104143. doi:10.1016/j.jri.2023.104143
28. Ali Khan I, Alhaizan MA, Neyazi SM, et al. Relevance of Serum Levels and Functional Genetic Variants in Vitamin D Receptor Gene among Saudi Women with Gestational Diabetes Mellitus. Nutrients. 2023;15(19):4288. doi:10.3390/nu15194288
29. Kabataş EU, Dinlen NF, Zenciroğlu A, et al. Relationship between serum 25-hydroxy vitamin D levels and retinopathy of prematurity. Scott Med J. 2017;62(4):129–135. doi:10.1177/0036933017701867
30. Boskabadi H, Abrishami M, Shoeibi N, et al. Comparison of Vitamin D Levels in Premature Infants with and without Retinopathy of Prematurity. Arch Iran Med. 2022;25(4):209–213. doi:10.34172/aim.2022.36
31. Agrawal G, Dutta S, Prasad R, et al. Fetal oxidative stress, micronutrient deficiency and risk of retinopathy of prematurity: a nested case-control study. Eur J Pediatr. 2021;180(5):1487–1496. doi:10.1007/s00431-020-03896-x
32. Matejek T, Zemankova J, Malakova J, et al. Severe vitamin D deficiency in preterm infants: possibly no association with clinical outcomes? J Matern Fetal Neonatal Med. 2022;35(8):1562–1570. doi:10.1080/14767058.2020.1762560
33. Papalia H, Samonini A, Buffat C, et al. Low Vitamin D Levels at Birth and Early Respiratory Outcome in Infants With Gestational Age Less Than 29 Weeks. Front Pediatr. 2022;9:790839. doi:10.3389/fped.2021.790839
34. Liu W, Xu P. The association of serum vitamin D level and neonatal respiratory distress syndrome. Ital J Pediatr. 2023;49(1):16. doi:10.1186/s13052-023-01415-w
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.