Back to Journals » Infection and Drug Resistance » Volume 17
A Cutaneous Phaeohyphomycosis Case Caused by Paraconiothyrium cyclothyrioides in Southern China
Authors Li J, Yaqoob MD , Liu K, Sun H, Qiu Q, Ke X, Hu Y
Received 21 March 2024
Accepted for publication 3 June 2024
Published 14 June 2024 Volume 2024:17 Pages 2401—2404
DOI https://doi.org/10.2147/IDR.S470026
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Junlan Li,1,* Muhammad Danish Yaqoob,2,* Kangxing Liu,2 Hengbiao Sun,3 Qinghua Qiu,4 Xiuling Ke,2 Yongxuan Hu2
1Department of Dermatology and Venereology, Meizhou People’s Hospital, Meizhou, People’s Republic of China; 2Department of Dermatology and Venereology, The Third Affiliated Hospital of Southern Medical University, Guangzhou, People’s Republic of China; 3Department of Clinical Laboratory, The Third Affiliated Hospital of Southern Medical University, Guangzhou, Guangdong, People’s Republic of China; 4Department of Clinical Laboratory, Meizhou People’s Hospital, Meizhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Junlan Li, Department of Dermatology and Venereology, Meizhou People’s Hospital, Huangtang Road, Meizhou, 514031, People’s Republic of China, Tel/Fax + 86 753 2202723, Email [email protected] Yongxuan Hu, Department of Dermatology and Venerology, the 3rd Affiliated Hospital of Southern Medical University, 183 West Zhongshan Road, Guangzhou, 510630, People’s Republic of China, Tel/Fax + 86 20 62784560, Email [email protected]
Abstract: Paraconiothyrium cyclothyrioides is a coelomycetous fungus species that was recently identified. We present a case of an elderly farmer with chronic skin lesions of the opisthenar caused by P. cyclothyrioides.
Keywords: phaeohyphomycosis, cutaneous, paraconiothyrium cyclothyrioides
Introduction
Paraconiothyrium cyclothyrioides, a fungus of the Coelomycetes genus, was found ubiquitously in the environment such as plants, wood, soil, etc. It was an emerging pathogen although rarely described in human infections.1,2 It belongs to a diverse group of fungi that cause phaeohyphomycosis, a large group of diseases brought on by fungi that grow septate hyphae in tissue that contain melanin.3 This bacterium causes disseminated illnesses such as fungemia and endocarditis in addition to subcutaneous infections, eumycetomas, osteomyelitis, arthritis, and myositis.4 We herein report a typical case of cutaneous phaeohyphomycosis lesions due to Paraconiothyrium cyclothyrioides in an elderly woman.
Case Report
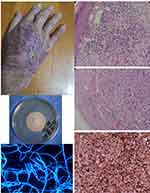
A 74-year-old woman, farmer by profession, residing in the countryside of Meizhou, southern China, presented to our outpatient clinic on November 20, 2023. She complained of an itchy and painful erythematous plaque on the right opisthenar. The lesion started 2 years ago. The woman had visited another hospital, and a clinical diagnosis of chronic eczema was made. Before he visited our hospital, topical application of mometasone furoate cream and oral antihistamines had been used for more than 2 weeks, but the lesion did not improve. On physical examination, she had a crusted, ulcerated plaque on the right opisthenar (measuring 2×4 cm) and several macular papules and nodules on erythematous plaque (Figure 1A).
Her family history is unremarkable. Diabetes mellitus, hypertension, HIV infection, HBV and syphilis are all negative in the patient. She has a history of asthma for many years and was treated with long-term 5mg of prednisone orally daily and budesonide spray.
At our hospital, biopsy specimens revealed pseudoepitheliomatous hyperplasia and suppurative granulomas, and fungal elements were seen invading the dermis by PAS and GMS (Figure 1B–1D), but acid-fast staining was negative. And immunohistochemistry of biopsy specimens showed that CD3, CD5, CD20 and Ki67 are all negative.
The fungus culture of the tissue specimens yielded a one colony-type mold (Figure 1E).
Extensive morphological and molecular characterization of the isolate was required to obtain a definitive identification. The isolates were cultured on SDA plates at 28°C for 7 days, microscopic morphology showed septate, bamboo-like hyphae, and no spores were found (Figure 1F).
The total DNA was extracted using 6% InStaGeneTM Matrix (BioRad, Hercules, CA, USA). Ribosomal DNA ITS regions of the isolation were amplified using a Biometra T-Gradient Thermoblock (Whatman Biometra, Goettingen, Germany) with primers ITS-5 (5’-GGAAGTAAAAGTCGTAACAAGG-3’) and ITS-4 (5’-TCCTCCGCTTATTGATATGC-3’). PCR was carried out at 94°C for 5 min, followed by 30 cycles at 94°C for 60s, annealing at 55°C for 90s, and an extension at 72°C for 90s; the reaction continued at 72°C for 10 min. The DNA fragments were sequenced using an ABI PRISM 3100 sequencer (Applied Biosystems, Foster City, CA, USA). Subsequently, the PCR and sequencing data went through Blast analysis and homology comparison in GenBank. The result of this isolate was 100% homology with Paraconiothyriumcy clothyrioides (accession no. PP449044).
For treatment, she received oral itraconazole 200 mg/day. After six weeks of treatment, the lesions clearly showed clinical improvement with less ulceration. The patient remains under follow-up.
Discussion
The fungi of Coelomycetes were initially classified into three subclasses, and the genus Paraconiothyrium was proposed in 2004.5 Human infections with these molds are typically superficial and are difficult to make a microbiological diagnosis. However, these fungi can cause severe deep, disseminated infections in immunocompromised patients. There are no treatment recommendations, with few antifungal therapy data available.1,2,6
In the reported cases, the clinical manifestations are difficult to distinguish phaeohyphomycosis, chromoblastomycosis, mycobacteria, actinomycosis, nocardiosis, cutaneous squamous cell carcinoma, and Kaposi’s sarcoma, therefore making a clinical diagnosis of the phaeohyphomycosis is much more difficult than other differential diagnoses.1,2,6–8
We described a typical case of cutaneous phaeohyphomycosis lesions due to Paraconiothyrium cyclothyrioides in an elderly woman. She has a history of long-term 5mg of prednisone orally daily and budesonide spray, this may lead to immunocompromised. She is still engaged in agricultural labor, and there is a risk and possibility of external injuries. Clinical suspicion of this rare infection, together with biopsy and fungal culture findings, is crucial for early diagnosis, particularly as the complete resolution can be achieved with itraconazole alone.
In summary, it should be considered in the differential diagnosis of invasive fungal infections in immunocompromised patients. The rare soil fungus P. cyclothyrioides has pathogenic potential in chronic, crusted, and ulcerated skin lesions.
Ethical Approval Statement and Informed Consent
The study was approved by the Ethics Committee of the Meizhou People’s Hospital. Written informed consent was provided by the patient to have the case details and accompanying images published.
Acknowledgments
We thank the Meizhou People’s Hospital and the 3rd Affiliated Hospital of Southern Medical University for their effort in medical records management. We thank Wiley Science Editing for editing this manuscript.
Disclosure
The authors declare no potential conflicts of interest in this work.
References
1. Gordon RA, Sutton DA, Thompson EH, et al. Cutaneous phaeohyphomycosis caused by Paraconiothyrium cyclothyrioides. J Clin Microbiol. 2012;50(11):3795–3798. doi:10.1128/JCM.01943-12
2. Malaure C, Hoang S, Bagny K, et al. Multifocal cutaneous phaeohyphomycosis caused by Paraconiothyrium cyclothyrioides in an immunocompromised patient: a case report. J Dermatol. 2023;50(6):e179–e180. doi:10.1111/1346-8138.16706
3. Marques SA, Camargo RMP, Summerbell RC, et al. Subcutaneous phaeohyphomycosis caused by Phaeoacremonium parasiticum in a renal transplant patient. Med Mycol. 2006;44(7):671–676. doi:10.1080/13693780600895181
4. Baradkar VP, Mathur M, Kumar S. Phaeohyphomycosis of subcutaneous tissue caused by Phaeoacremonium parasiticum. Indian J Med Microbiol. 2009;27(1):66–69. doi:10.1016/S0255-0857(21)01760-6
5. Verkley GJM, da Silva M, Wicklow DT, Crous PW. Paraconiothyrium, a new genus to accommodate the mycoparasite Coniothyrium minitans, anamorphs of Paraphaeosphaeria, and four new species. Stud Mycol. 2004;50:323–335.
6. Colombier MA, Alanio A, Denis B, et al. Dual invasive infection with phaeoacremonium parasiticum and paraconiothyrium cyclothyrioides in a renal transplant recipient: case report and comprehensive review of the literature of phaeoacremonium phaeohyphomycosis. J Clin Microbiol. 2015;53(7):2084–2094. doi:10.1128/JCM.00295-15
7. Hamed A, Bosshardt Hughes O, Palavecino EL, Jakharia N. Cutaneous infection caused by paraconiothyrium cyclothyrioides in a renal transplant recipient. Transpl Infect Dis. 2021;23(4):e13624. doi:10.1111/tid.13624
8. Mori H, Hayashi S, Okamoto M, et al. Paraconiothyrium cyclothyrioides infected on the sole of a healthy person: a case report. J Dermatol. 2022;49(8):e278–e279. doi:10.1111/1346-8138.16403
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.