Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
Associations Between Serum Vitamin A Levels in Early Pregnancy and the Risk of Gestational Diabetes Mellitus
Received 25 January 2024
Accepted for publication 6 July 2024
Published 31 July 2024 Volume 2024:17 Pages 2895—2901
DOI https://doi.org/10.2147/DMSO.S460796
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Jie Yu,1 Yanping Liu,2 Lingling Xu1
1Department of Endocrinology, Key Laboratory of Endocrinology of National Health Commission, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People’s Republic of China; 2Department of Clinical Nutrition, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People’s Republic of China
Correspondence: Yanping Liu; Lingling Xu, Email [email protected]; [email protected]
Background: The relationship between vitamin A levels and gestational diabetes mellitus (GDM) is not well understood, and prospective studies are lacking.
Methods: This was a prospective, longitudinal study. A total of 391 women in early pregnancy were recruited between October and December 2018 at Shunyi District Maternal and Child Health Hospital (Beijing, China). Serum vitamin A concentration was measured at enrollment. GDM was diagnosed on the basis of a 75 g oral glucose-tolerance test at 24– 28 weeks of follow-up. Logistic regression was used for the analysis.
Results: None of the subjects in the cohort had vitamin A deficiency or excess. At the follow-up, 76 participants had developed GDM. Participants who developed GDM were older and had higher body mass index, fasting insulin, HbA1c, fasting glucose, homeostasis model assessment for insulin resistance, triglyceride, low-density lipoprotein cholesterol, and high-sensitivity CRP levels, as well as higher serum vitamin A levels at baseline. On logistic multivariate analysis, higher vitamin A was positively associated with higher risk of GDM. The adjusted OR was 2.85 (95% CI 1.04– 7.80, P=0.042) for Q4 versus Q1 and 1.59 (95% CI 1.11– 2.28, P=0.011) for every 1 SD increase in serum vitamin A levels. In participants within the vitamin A reference range (0.33– 0.78 mg/L), the positive association also maintained significance.
Conclusion: Higher serum vitamin A levels were associated with higher GDM risks, even within the reference range. The results and possible mechanisms need to be further verified and clarified.
Keywords: gestational diabetes mellitus, vitamin A, insulin resistance, inflammation
Introduction
Vitamin A is a fat-soluble essential nutrient that can be obtained from plant and animal food and affects numerous basic physiological functions, including growth, vision, and metabolism.1 Vitamin A circulates mainly in the form of RBP4, which is transported to tissue and converted into retinoic acid. In past years, vitamin A deficiency was a significant public health concern, especially in developing countries, and vitamin A supplementation during pregnancy is suggested.2 However, in recent years, serum concentrations of vitamin A in pregnant women in China, especially in Beijing, have gradually increased.3
Gestational diabetes mellitus (GDM) is one of the most common complications during pregnancy and is also globally increasing in prevalence.4 GDM is associated with adverse obstetric and neonatal outcomes, and also increases the risk of future type 2 DM, obesity, and cardiovascular disease in mother and child.5,6 Several risk factors for GDM have been identified, such as previous GDM, obesity, and polycystic ovary syndrome.5 Although maternal nutritional status has also been linked to GDM,7 the relationship between vitamin A and GDM is not well understood.
Research in this area has mainly focused on RBP4, and most studies have found that RBP4 concentrations were significantly positively associated with a higher risk of GDM.8 However, retinol, the main circulating form of vitamin A, has been far less studied. A retrospective study found that vitamin A levels in early pregnancy had a nonsignificantly positive association with GDM.9 Another retrospective case–control study found that lower first-trimester concentrations of retinol were associated with a risk of insulin-treated GDM.10 So far, no prospective studies have investigated the relationship between serum vitamin A levels in early pregnancy and the incidence of GDM. In the present study, we examined maternal vitamin A concentrations in the first trimester and risk of GDM during follow-up.
Methods
The study protocol was approved by the Ethics Committee of Peking Union Medical College Hospital (approval document hs-1646). This study also followed the Declaration of Helsinki, and all participants signed a written informed consent form before recruitment.
Study Population
The analysis of this study was based on a prospective longitudinal cohort study aiming to identify risk factors for adverse pregnant and perinatal outcomes in pregnant women, and more details can be found in our previous published work.11 In short, 432 women in early pregnancy were recruited between October and December 2018 at the Shunyi District Maternal and Child Health Hospital (Beijing, China) as the baseline. Women were disqualified from participation if they 1) had not experienced a singleton pregnancy, 2) had laboratory-confirmed fasting glucose ≥6.1 mmol/L, HbA1c >6.5%, or a prior diagnosis of DM before conception, 3) had a record of autoimmune diseases, including systemic lupus erythematosus, or were currently on corticosteroids, 4) had a confirmed diagnosis of hyperthyroidism or hypothyroidism, 5) had a miscarriage or induced delivery before undergoing a 75 g oral glucose tolerance test during the 24- to 28-week gestation period, 6) had a history of liver or kidney malfunction or suspected acute inflammation indicated by CRP >10 mg/L, or 7) lacked complete records of vitamin A measurements.
A standard questionnaire was used to collect demographics, lifestyle, medical and family history, parity status, and use of multinutrient supplements at baseline. All participants were regularly followed up during the entire pregnancy in the same hospital, and at 24–28 weeks of gestation, a 75 g oral glucose-tolerance test was administered to all participants. GDM was diagnosed based on the IADPSG criteria:12 fasting plasma glucose (FPG) ≥5.1 mmol/L, 1 h PG ≥10 mmol/L, and 2 h PG ≥8.5 mmol/L. A total of 391 women with complete data were eligible for analysis. A participant inclusion and exclusion flowchart is presented in Figure 1.
 |
Figure 1 Flowchart of participant inclusion and exclusion. |
Anthropometric Measurements
A portable stadiometer was used to measure height to the nearest 0.1 cm. A calibrated scale was used to measure weight vertically to the nearest 0.1 kg. Body mass index (BMI) was calculated as weight (kg)/height (m2).
Biochemical Measurements
Blood samples were collected from all participants during the first visit (before 12 weeks of pregnancy) after overnight fasting (≥8 h). PG, insulin, hemoglobin, high-sensitivity CRP (hs-CRP), triglyceride (TG), total cholesterol (TC), high–density lipoprotein cholesterol (HDL-C), and low–density lipoprotein cholesterol (LDL-C) levels were measured as per previous publications.11,13 The homeostasis model assessment for insulin resistance (HOMA-IR) was calculated as (FPG [mmol/L] × fasting serum insulin [mIU/mL])/22.5.
Serum vitamin A concentrations were measured using rapid liquid chromatography–tandem mass spectrometry (LC-MS/MS) on an Acquity UPLC system (Waters, Milford, MA, USA) in tandem with an AB Sciex 4000 QTrap system (Applied Biosystems, Foster City, CA, USA). The normal reference range for vitamin A is 0.33–0.78 mg/L. Levels of vitamin A <0.2 mg/L indicates a deficiency, whereas a level over 1.2 mg/L indicates an excess of vitamin A, according to the Mayo Medical Laboratory.
Statistical Analysis
Continuous data with normal distribution are expressed as means ± SD, while those with abnormal distribution are expressed as medians (interquartile range). Categorical variables are expressed as percentages or proportions. Student’s t-test, Mann–Whitney U test, or χ2 test was used for comparison between groups. Associations between serum vitamin A levels at baseline and GDM incidence during follow-up were assessed using logistic regression analyses adjusted for confounding factors. ORs and 95% CI were computed for every 1 SD increase in and quartiles of vitamin A levels. A total of three models were constructed: Model 1 (not adjusted), Model 2 (adjusted for age, BMI, and parity), and Model 3 (Model 2 + hs-CRP, HOMA-IR, TG, HDL-C, physical activity, family history of DM, and vitamin A supplementation).
Associations between levels of vitamin A and GDM were evaluated on a continuous scale with restricted cubic spline curves with four knots, and the model was adjusted for confounding factors as per Model 3. On sensitivity analyses, we tested the association between vitamin A levels and GDM using logistic regression analyses of participants with normal vitamin A levels. All statistical analyses were performed using SPSS 25.0 (IBM, Armonk, NY, USA), R 3.6.3, and Python 3.7. All P values were two-tailed and considered statistically significant at P<0.05.
Results
Baseline Characteristics
Table 1 shows the baseline characteristics of the study population according to GDM status. Participants who developed GDM during the follow-up period were older and had higher BMI, fasting insulin, HbA1c, FPG, HOMA-IR, TG, LDL-C, and hs-CRP. Participants who developed GDM had less exercise and a higher proportion of family history of DM. None of the subjects had a vitamin A deficiency or excess. Although most participants had serum vitamin A levels within the normal range, those with GDM had higher levels.
 |
Table 1 Baseline characteristics of participants by GDM status |
Baseline Vitamin A and Risk of GDM During Follow-Up
On logistic regression analyses, 1 SD increase and the highest quartile of baseline vitamin A were significantly and positively associated with increased risk of GDM during follow-up after adjusting confounding factors: adjusted ORs were 2.85 (95% CI 1.04–7.80, P=0.042) for Q4 versus Q1 and 1.59 (95% CI 1.11–2.28, P=0.011) for every 1 SD increase (Table 2). On sensitivity analyses of participants with vitamin A levels in the normal range, a similar association was found between higher vitamin A levels and an increased risk of GDM (Table 3). The associations between vitamin A levels on a continuous scale and GDM risks were linear in all subjects (overall P=0.011, nonlinear P=0.378) and participants with vitamin A levels in the normal range (overall P=0.012, nonlinear P=0.807; Figure 2).
 |
Table 2 Serum vitamin A at baseline and GDM risk during follow-up |
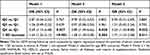 |
Table 3 Serum vitamin A in normal range at baseline and GDM risk during follow-up |
Discussion
This prospective study aimed to look at how vitamin A levels in blood related to GDM risk. We found that higher vitamin A in early pregnancy (and even normal vitamin A levels) was positively associated with GDM risks and not due to other known risk factors. Prior research has primarily concentrated on vitamin A deficiency, emphasizing its detrimental impact on both maternal and infant health during pregnancy and postpartum.2 Vitamin A deficiency impairs insulin secretion.1 Certain investigations have revealed that individuals with GDM tend to have lower serum retinol levels, indicating that GDM serves as an additional risk factor for vitamin A deficiency,14 which has been attributed to hindrance in the transportation and release of vitamin A from hepatic stores stemming from hyperglycemia.15
As economic prosperity has grown, vitamin A levels have risen accordingly. A recent study revealed that vitamin A deficiency among pregnant women in China is now considered a minor public health concern,16 which is consistent with the present study, where no subjects were found to have vitamin A deficiency. Given the current situation, it is essential to direct attention towards determining the suitable upper limit for serum vitamin A levels during pregnancy.
A recent study encompassing 119,286 participants from western China proposed a reference range of 0.26–0.63 mg/L for vitamin A levels in pregnant women during their first trimester,16 but it did not consider adverse maternal or fetal outcomes. A retrospective study found vitamin A in early pregnancy had a nonsignificantly positive association with GDM,9 which supports our results to some extent. The other retrospective case–control study found lower first-trimester concentrations of retinol were associated with risk of insulin-treated GDM,10 which seems contradictory to our results. However, the average retinol level in the insulin-treated GDM group was comparatively low, suggesting that there could be individuals with vitamin A deficiency among them, potentially introducing bias to the results.
However, the underlying mechanisms that explain the relationship between vitamin A levels and GDM are still unclear. The primary source of vitamin A intake is diet, where animal products contribute significantly, while plant-based sources serve as alternative options.17,18 In our study, individuals with elevated serum vitamin A levels also exhibited higher BMI and TG levels, suggesting a state of excessive nutrition. Given that vitamin A is fat-soluble and GDM is related to adiposity, we speculated that the relationship between vitamin A and GDM was more likely related to excess adiposity than vitamin A per se. However, additional research is crucial to validate these observations and provide deeper insights into the specific mechanisms involved.
Our study had some strengths: first, this was the first prospective longitudinal cohort study to evaluate the association between vitamin A and GDM; and second, the study collected detailed demographic, clinical, and biological information. There are also limitations to our study: the sample was relatively smal; we did not measure other indicators related to vitamin A metabolism; and some data, e.g., for diet, sleep, stress, polycystic ovary syndrome, and cigarette smoking, were lacking, which might cause some bias in the results.
Conclusion
In conclusion, we found a positive association between vitamin A and risk of GDM, even in the current normal reference range. Further research is required to elucidate this relationship and the underlying mechanisms.
Abbreviations
GDM, gestational diabetes mellitus; BMI, body mass index; Hs-CRP, high-sensitivity CRP; TG, triglyceride; TC, total cholesterol; HDL-C, high–density lipoprotein cholesterol; LDL-C, low–density lipoprotein cholesterol; HOMA-IR, insulin resistance.
Data Sharing
All data generated or analyzed during this study are included in the article.
Ethics
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Ethics Committee of Peking Union Medical College Hospital (approval document hs-1646). Written informed consent was obtained from all subjects.
Consent for Publication
All patients signed a written informed consent form to publish their research data.
Acknowledgments
The authors would like to thank the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (CIFMS; 2021-I2M-C&T-B-003), the National Natural Science Foundation of China (82100947), and all participants in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, interpretation, or all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval to the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
This research was supported by the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (CIFMS; 2021-I2M-C&T-B-003) and the National Natural Science Foundation of China (82100947).
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Bastos Maia S, Rolland Souza A, Costa Caminha M, et al. Vitamin A and pregnancy: a narrative review. Nutrients. 2019;11(3):681. doi:10.3390/nu11030681
2. McGuire S. WHO guideline: vitamin a supplementation in pregnant women. Geneva: WHO 2011; WHO guidelines: vitamin A supplementation in postpartum women. Geneva: WHO, 2011. Adv Nutr. 2012;3(2):215–216. doi:10.3945/an.111.001701
3. Li J, Zheng C, Ni J, et al. 2013—2016年北京地区孕妇维生素A、维生素E营养水平 [Trend of vitamin A and vitamin E among pregnancy in Beijing in 2013–2016]. Wei Sheng Yan Jiu. 2019;48(1):56–60. Chinese.
4. Zhou T, Du S, Sun D, et al. Prevalence and trends in gestational diabetes mellitus among women in the United States, 2006–2017: a population-based study. Front Endocrinol. 2022;13:868094.
5. Sweeting A, Wong J, Murphy HR, et al. Clinical updates for gestational diabetes mellitus. Endocr Rev. 2022;43(5):763–793. doi:10.1210/endrev/bnac003
6. Ye W, Luo C, Huang J, et al. Gestational diabetes mellitus and adverse pregnancy outcomes: a systematic review and meta-analysis. BMJ;2022:e067946. doi:10.1136/bmj-2021-067946
7. Ibrahim I, Bashir M, Singh P, Al Khodor S, Abdullahi H. Effect of nutritional supplementation during pregnancy on the incidence of gestational diabetes and glycemic control. Front Nutr. 2022;9. doi:10.3389/fnut.2022.867099
8. Lu J, Wang D, Ma B, et al. Blood retinol and retinol-binding protein concentrations are associated with diabetes: a systematic review and meta-analysis of observational studies. Eur J Nutr. 2022;61(7):3315–3326. doi:10.1007/s00394-022-02859-2
9. Liang JW, Chen MX, Hu XA, et al. Potential biomarkers for predicting gestational diabetes mellitus and adverse pregnancy outcomes during early pregnancy. Clin Lab. 2021;67(8). doi:10.7754/Clin.Lab.2021.201022
10. Fruscalzo A, Londero AP, Driul L, et al. First-trimester concentrations of TTR-RBP4-retinol complex components as early markers of insulin-treated gestational diabetes mellitus. Clin Chem Lab Med. 2015;53(10):1643–1651. doi:10.1515/cclm-2014-0929
11. Liu PJ, Liu Y, Ma L, et al. Associations between gestational diabetes mellitus risk and folate status in early pregnancy and the MTHFR C677T polymorphism in Chinese women. Diabetes Metab Syndr Obes. 2020;13:1499–1507. doi:10.2147/DMSO.S250279
12. Metzger BE, Gabbe SG, Persson B, et al. The international association of diabetes and pregnancy study groups recommends the diagnosis and classification of hyperglycemia during pregnancy. Diabetes Care. 2010;33(3):676–682. doi:10.2337/dc10-0719
13. Heslehurst N, Ngongalah L, Bigirumurame T, et al. Association between maternal adiposity measures and adverse maternal outcomes in pregnancy: a systematic review and meta-analysis. Obes Rev. 2022;23(7). doi:10.1111/obr.13449
14. Lira LQ, Dimenstein R. Vitamin A and gestational diabetes. Rev Assoc Med Bras. 2010;56(3):355–359. doi:10.1590/S0104-42302010000300023
15. Yang C, Chen J, Liu Z, et al. Prevalence and factors influencing vitamin A deficiency in pregnant Chinese women. Nutr J. 2016;15(1):12. doi:10.1186/s12937-016-0131-7
16. Gao F, Guo F, Zhang Y, et al. Vitamin A, D, and E levels and reference ranges for pregnant women: a cross-sectional study, 2017–2019. Front Nutr. 2021;8. doi:10.3389/fnut.2021.628902
17. Olza J, Aranceta-Bartrina J, González-Gross M, et al. Dietary intake and food sources of zinc, selenium, and Vitamins A, E and C in the Spanish Population: findings from the ANIBES Study. Nutrients. 2017;9(7):697.
18. Weber D, Grune T. Contribution of β-carotene to vitamin A supply to humans. Mol Nutr Food Res. 2012;56(2):251–258. doi:10.1002/mnfr.201100230
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

