Back to Journals » International Journal of General Medicine » Volume 17
Autonomic Nervous System and Sarcopenia in Elderly Patients: Insights from Long-Term Heart Rate Variability Monitoring in a Hospital Setting
Received 9 April 2024
Accepted for publication 7 August 2024
Published 12 August 2024 Volume 2024:17 Pages 3467—3477
DOI https://doi.org/10.2147/IJGM.S472913
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Vinay Kumar
Jia Liu, Fan Zhang
Department of Geriatrics, Peking University Third Hospital, Beijing, People’s Republic of China
Correspondence: Fan Zhang, Department of Geriatrics, Peking University Third Hospital, 49 North Garden Road, Beijing, 100191, People’s Republic of China, Email [email protected]
Background: Emerging evidence suggests a link between muscle health and the autonomic nervous system, but research is scarce. This study examines the connection between long-term heart rate variability (HRV) measured autonomic function and sarcopenia in the elderly, focusing on muscle mass and strength.
Patients and Methods: This retrospective cross-sectional study comprised 132 elderly hospitalized patients. Sarcopenia was defined according to the European Working Group on Sarcopenia in Older People (EWGSOP2) criteria, involving reduced muscle mass and strength. HRV was assessed using standard deviation of NN intervals (SDNN), with values below 100 milliseconds indicating reduced HRV. Multivariate logistic regression and Pearson’s correlation analyses were conducted to explore the associations between sarcopenia, muscle metrics, and HRV parameters.
Results: Among elderly hospitalized patients, 45.45% had reduced HRV, with sarcopenia patients showing a fivefold higher risk (OR: 5.042; p = 0.034). Grip strength and SARC-CalF scores were independent factors associated with reduced HRV. Moderate correlations were noted between grip strength and HRV indices, particularly with SDNN (r = 0.393, p = 0.001) and the triangular index (r = 0.385, p < 0.001), while a weaker correlation was found with very low frequency power (VLF) (r = 0.283, p = 0.006). No significant correlations were identified between HRV and muscle mass. Regression analyses revealed significant independent associations between HRV parameters and the decline in muscle strength and the onset of sarcopenia.
Conclusion: Reduced HRV is closely linked to sarcopenia and diminished muscle strength in the elderly, with the triangular index and SDNN as key indicators, highlighting HRV’s potential in muscle health assessment.
Keywords: muscle strength, SDNN, triangular index, muscle mass
Introduction
Sarcopenia is a geriatric syndrome characterized by age-related loss of muscle mass, decreased muscle strength, and declined physical function. The prevalence of sarcopenia increases significantly among older adults, and it can lead to functional decline, falls, frailty, increased healthcare expenditures, decreased quality of life, and even mortality.1,2 Early research on sarcopenia focused primarily on assessing muscle quantity, but as studies progressed, it became evident that muscle function had a stronger correlation with adverse outcomes. Consequently, there has been a greater emphasis on evaluating both muscle quantity and function in the diagnosis of sarcopenia, as outlined by the latest European consensus on sarcopenia.2 Sarcopenia’s etiology is complex, encompassing factors such as inflammation, malnutrition, reduced physical activity, and oxidative stress. Additionally, the sympathetic nervous system exerts regulatory control over skeletal muscle. Dysfunction in the sympathetic nervous system can undermine muscle performance, as documented in conditions like Alzheimer’s disease,3 Parkinson’s disease,4 and multiple system atrophy.5 Fundamental research has demonstrated that the sympathetic denervation can impair axonal function of motor neurons, potentially leading to reduced neurotransmitter release and diminished muscle contraction strength.6 The sympathetic nervous system regulates the structure and function of the neuromuscular junction, with norepinephrine being the main neurotransmitter of sympathetic ganglion neurons that modulates neuromuscular transmission. β2-adrenergic receptor agonists can inhibit protein degradation in denervated muscles.7 Studies have shown that maintaining sympathetic neurons can alleviate motor neuron denervation and delay sarcopenia. Continuous expression of Hand2 in sympathetic neurons in middle-aged mice enhances neuromuscular junction transmission, muscle fiber movement, and prevents sympathetic denervation.6 In summary, basic research indicates that the sympathetic nervous system plays a crucial role in regulating the structure and function of skeletal muscle. However, clinical studies are needed to confirm these findings and to explore potential therapeutic strategies targeting the sympathetic nervous system for the prevention and treatment of sarcopenia.
The autonomic nervous system (ANS) comprises the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), which often function in a complementary yet nuanced manner, sometimes acting in opposition but also synergistically depending on the physiological context. Microneurography, an effective method for measuring Muscle Sympathetic Nerve Activity (MSNA), plays a crucial role in studying human sympathetic nervous system activities. Previous research utilizing microneurography as a measure of sympathetic activity has identified that a sympatho-vagal imbalance appears to be associated with sarcopenia in male patients with heart failure.8 However, the complexity of the procedure and its minimally invasive nature pose challenges for its widespread implementation in clinical settings. Heart rate variability (HRV) refers to the temporal variation between successive heartbeats, with both SNS and PNS exerting regulatory effects on HRV.9 Therefore, HRV is commonly utilized as an indicator of ANS activity and is a widely applied non-invasive biomarker associated with health. HRV can predict the risk of onset and mortality associated with cardiovascular diseases,10 although it is typically considered alongside other clinical factors. Typically, a lower HRV indicates compromised autonomic function and a reduced capacity to cope with various stressors.11 Long-term (24-hour) and short-term (5-minute) analyses are two principal methods for HRV assessment. Long-term HRV analysis is superior in reflecting daily activities, circadian rhythms, and responses to environmental stimuli, in comparison with short-term analysis. The most frequently employed HRV indices include standard deviation of NN intervals (SDNN), root mean square of differences between successive NN intervals (rMSSD), percent NN intervals >50 ms different from the prior interval (pNN50), triangular index, as well as low-frequency power (LF) and high-frequency power (HF), and very low frequency power (VLF). A higher SDNN generally indicates healthier autonomic function, elevated rMSSD suggests increased parasympathetic activity and better stress recovery, while the LF/HF ratio serves as an index of sympathetic-vagal balance.9
Preliminary evidence from basic science research suggests that muscle health is influenced by the sympathetic nervous system. However, current studies are limited by small sample sizes, short-term HRV analysis, or cross-sectional designs, and there is a lack of research applying long-term HRV monitoring to explore the potential relationship between sympathetic nervous system function and sarcopenia over extended periods. We hypothesize that patients with sarcopenia will exhibit alterations, particularly a reduction, in HRV during long-term monitoring. The aim of this study is to investigate whether there is a correlation between autonomic nervous function, as measured by HRV, and sarcopenia in terms of muscle mass and strength in an elderly population. Additionally, we aim to identify which HRV parameters show the strongest correlation with muscle status.
Material and Methods
Setting and Participants
This is a retrospective cross-sectional study conducted at Peking University Third Hospital. Patient data was derived from the electronic medical records system of the hospital. The study analyzed data from elderly patients aged ≥65 years who were admitted to the geriatric department from March 2023 to December 2023. A total of 132 patients who met the following criteria were included in the study: 1. Completion of a standard HRV examination within 48 hours of admission; 2. Holter monitoring indicating sinus rhythm; 3. Completion of muscle assessment within 48 hours of admission.
The research protocol has been approved by the Peking University Third Hospital Medical Science Research Ethics Committee (M2023831) and adheres to the principles of the Helsinki Declaration and its amendments.
Data Collection
The study gathered baseline data on the participants, including demographics and medical history including age, gender, height, weight, and detailed past medical history, encompassing both chronic conditions and recent acute episodes. Body Mass Index (BMI) is calculated by dividing an individual’s weight (in kilograms) by their height (in meters) squared (BMI = kg/m2). The age-adjusted Charlson Comorbidity Index (aCCI) has been used to quantify the overall burden of comorbidities in patients, with an adjustment made for age to provide a precise evaluation of risk, particularly in elderly populations. This index assigns weights to 19 different comorbid conditions, each based on its potential to impact mortality. Age is adjusted to accurately reflect the increased mortality risk associated with aging, thereby offering a refined understanding of comorbidity burden in older adults.
Laboratory findings from peripheral blood samples, representing a routine comprehensive metabolic panel, were analyzed within 24 hours of admission were also collected, including white blood cell count, hemoglobin level, platelet count, transaminase level, total protein level, albumin level, blood urea nitrogen level, creatinine level, estimated glomerular filtration rate, and dimerized plasmin fragment D (D-dimer) level.
Nutritional status was assessed using the Mini Nutritional Assessment–Short Form (MNA-SF), a crucial tool for identifying nutritional risk in the elderly, evaluated by trained nursing staff within 24 hours of admission, with a total score ranging from 0 to 14 and scores ≤11 indicating nutritional risk. The Barthel Index (BI) was used to assess activities of daily living (ADL) scores, a key metric in evaluating the functional independence of elderly patients, covering 10 categories (feeding, transferring, grooming, toilet use, bathing, mobility, stairs, dressing, bowel, and bladder control), with scores ranging from 0 to 100, where lower scores indicate higher dependency.
Muscle Assessment
In the context of clinical work, geriatricians within the Department of Geriatric Medicine typically evaluate the muscular health of their patients shortly after admission, using a range of assessment tools and documenting their findings. For this particular study, the following muscle assessment data were collected:
1. SARC-CalF Questionnaire: The SARC- CalF questionnaire is a screening tool for sarcopenia and assesses six components: strength, assistance with walking, rising from a chair, climbing stairs, falls, and calf circumference (measured with a non-elastic measuring tape). A score of 11 points or higher suggests a potential presence of sarcopenia.
2. Handgrip strength measurement: This is conducted using an electronic hand dynamometer (EH101; CAMRY, Guangdong, China). Each side is measured twice, and if the difference between the two measurements exceeds 3 kilograms, a third measurement is taken. The highest value of grip strength is recorded. According to the European consensus on sarcopenia developed by the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), a handgrip strength of less than 27 kilograms in men and less than 16 kilograms in women is considered indicative of reduced muscle strength.2
3. Body composition analysis: Segmental multi-frequency bioelectrical impedance analysis (BIA) (InBody720; BiSpace Co., Ltd, Korea) is used to determine the body composition. It measures skeletal muscle mass and appendicular skeletal muscle mass (ASM). The Skeletal Muscle Mass Index (SMI) is then calculated using the formula ASM divided by height squared (ASM/Height2). According to the European consensus on sarcopenia developed by the EWGSOP2, an SMI of less than 7.0 kg/m2 in men and less than 5.5 kg/m2 in women is considered indicative of low muscle quantity.2
The diagnosis of sarcopenia is established in patients who exhibit both a decrease in muscle mass (an SMI of less than 7.0 kg/m² in men and less than 5.5 kg/m² in women) and a decrease in muscle strength (a handgrip strength of less than 27 kilograms in men and less than 16 kilograms in women) according to the European consensus developed by EWGSOP2.2 Functional impairment is a critical metric for assessing sarcopenia severity. However, due to the high prevalence of disability and partial disability among our study’s elderly inpatient population, administering physical function tests posed significant challenges. Consequently, these assessments were not included in our study.
HRV Assessment
HRV was assessed using a 12-lead dynamic electrocardiograph (model MGY-H12; DM Software Inc., USA) over a 24-hour period starting at 9 a.m. HRV parameters were analyzed using the Holter System software (version 12.net, DM Software, USA). In our study, the average duration between HRV assessment and body composition analysis was approximately 2 days. This study evaluated seven HRV indices, including four time-domain measures—SDNN, rMSSD, pNN50, and the Triangular Index. The latter quantifies the density of all NN intervals on a histogram through triangular interpolation, providing a nuanced measure of interval distribution. Additional, three frequency-domain were examined—HF (0.15–0.40 Hz), LF (0.04–0.15 Hz), and VLF (0.003–0.04 Hz). These measures analyze the power spectral density of heart rate oscillations across distinct frequency bands, offering a comprehensive perspective on the autonomic regulation of the heart. An SDNN value below 100 ms is considered indicative of reduced HRV.12,13
Statistical Analysis
Statistical analyses were conducted using SPSS version 27.0 and GraphPad Prism 9. Continuous variables were expressed as mean ± standard deviation for data following a normal distribution or as median with interquartile range (25th - 75th percentiles) for data not normally distributed. The determination of data distribution normality was assessed using the Shapiro–Wilk test. Categorical data were presented as counts and percentages. The study population was categorized into groups exhibiting reduced HRV and those with normal HRV. The t-test or Mann–Whitney U-test was applied to compare continuous variables, depending on the distribution normality, while the chi-square test was used for categorical variables, aiming to identify differences in characteristics and muscle assessment indices between the groups. Multivariate logistic regression analysis was employed to investigate the association between sarcopenia, muscle assessment indices, and reduced HRV. Pearson’s correlation analysis was used to examine the correlations between HRV indices parameters and muscle metrics (muscle mass, muscle strength, Calf Circumference, SARC-CalF score). Univariate and multivariate logistic regression analyses were utilized to assess the independent associations between various HRV parameters and sarcopenia, declined muscle strength, declined muscle mass. A p-value of < 0.05 was considered significant for all statistical tests.
Results
Table 1 outlines the characteristics of the study population among 132 elderly hospitalized individuals, with 45.45% displaying reduced HRV. The mean ages for the control group and the reduced HRV group were 77.60 ± 6.75 years and 79.35 ± 8.83 years, respectively, demonstrating no significant statistical difference (p = 0.200). Both groups were comparable in gender distribution, BMI, aCCI, and liver and kidney function tests. A notable distinction was observed in the MNA-SF scores, with the reduced HRV group having a median score of 12 (IQR: 10–14), lower than the control group’s median of 13 (IQR: 12–14). This suggests a greater proportion of individuals at nutritional risk in the reduced HRV group (39.4%) compared to 16.7% in the control group. Furthermore, the Barthel Index, evaluating functional independence, revealed significantly lower median values in the reduced HRV group (75, IQR: 60–95) than in the control group (95, IQR: 81.25–100), highlighting decreased independence in daily activities among these individuals. Laboratory assessments showed slightly higher counts of white blood cells and platelets in the reduced HRV group compared to controls, though both groups’ values remained within normal clinical limits. All HRV parameters were significantly lower in the reduced HRV group compared to the control group.
 |
Table 1 Characteristics of the Study Population |
Table 2 presents a comparative analysis of muscular metrics between the control group and the cohort with reduced heart rate variability (HRV). Muscle Strength: There was a marked difference in muscle strength, with the reduced HRV group demonstrating significantly lower average strength (19.05 ± 6.99 kg) compared to the control group (26.29 ± 9.95 kg), a disparity that is statistically significant (p < 0.001). Additionally, a high percentage (73.1%) of participants in the reduced HRV group exhibited reduced muscle strength. Muscle Mass: Skeletal muscle mass assessments conducted via BIA indicated that individuals in the reduced HRV group had significantly lower muscle mass, with an average of 23.50 kg (IQR: 21.25–27.50). Despite this, the skeletal muscle mass index (SMI) and the proportion of patients with decreased muscle mass based on SMI did not show a significant difference between the two groups. Sarcopenia Diagnosis: While the calf circumference measurements were comparable between groups, the scores from the SARC-CalF questionnaire—which assesses risk factors for sarcopenia—were significantly higher in the reduced HRV group (11.0, IQR: 5.0–14.0) compared to the control group (3.5, IQR: 0–11.5). This finding suggests a higher risk or presence of sarcopenia in the reduced HRV cohort. Moreover, a larger proportion of patients in the reduced HRV group (23.3%) were diagnosed with sarcopenia based on their muscle mass and strength, differing significantly from the 7% observed in the control group (p = 0.035).
 |
Table 2 Comparison of Muscle Metrics Between the Reduced HRV Group and the Control Group |
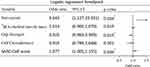
Multivariate logistic regression analysis was utilized in Figure 1 to investigate the correlation between sarcopenia, muscular assessment indicators and decreased HRV. The study analyzed decreased HRV as the outcome variable, considering the presence of sarcopenia and muscular assessment indicators as distinct independent variables. It controlled for variables such as gender, age, and baseline differences among groups, including the Barthel Index, MNA-SF score, white blood cell count, and platelet count. The study revealed that sarcopenia (OR: 5.042; 95% CI [1.127, 22.551]; p = 0.034), grip strength (OR: 0.925; 95% CI [0.869, 0.985]; p = 0.015) and SARC-CalF scores (OR: 1.077; 95% CI [1.005, 1.155]; p = 0.036) are independently associated with a reduction in HRV. However, the skeletal muscle mass assessed using BIA and calf circumference does not show an independent correlation with reduced HRV.
Table 3 shows the correlation between HRV indices parameters and muscle metrics (grip strength, skeletal muscle mass, SMI, calf circumference, SARC-CalF score). Grip Strength exhibited significant correlations with SNDD (logarithmic transformation), Triangular Index (logarithmic transformation), and VLF (logarithmic transformation). Specifically, Grip Strength correlated moderately with SNDD (r = 0.393), the Triangular Index (r = 0.385), and weakly with VLF (r = 0.283). Calf Circumference exhibited significant correlations with Triangular Index (logarithmic transformation) and VLF (logarithmic transformation) with low correlation coefficients (r = 0.228 and r = 0.246, separately). SARC-CalF score exhibited significant negative correlations with SNDD (logarithmic transformation) and Triangular Index (logarithmic transformation) with low correlation coefficients (r = −0.241 and r = −0.223, separately). There were no statistically significant correlations between HRV indicators and skeletal muscle mass, SMI.
 |
Table 3 Correlation Analysis of Muscle Metrics and HRV Parameters |
Utilizing univariate and multivariate logistic regression analyses, we explored the relationships between HRV parameters and three key outcomes: the decline in muscle strength, the decrease in muscle mass, and the onset of sarcopenia. In our analysis, HRV parameters functioned as independent variables, with adjustments made for potential confounders such as age, gender, BMI, Barthel Index, MNA-SF score, and aCCI. Our findings revealed significant independent associations between a lower SDNN (OR: 0.976; 95% CI: [0.960, 0.993]; p = 0.006) and a reduced triangular index (OR: 0.809; 95% CI: [0.709, 0.924]; p = 0.002) with the decline in muscle strength. Additionally, a decreased triangular index (OR: 0.767; 95% CI: [0.625, 0.945]; p = 0.012) was found to be independently associated with sarcopenia. Conversely, our analysis did not reveal any statistically significant associations between the decline in muscle mass and the HRV parameters (as detailed in Table 4).
 |
Table 4 Logistic Regression Analysis of Correlation Between HRV Parameters and Markers of Sarcopenia |
Discussion
Our study utilized long-term HRV analysis to establish a significant correlation between sarcopenia and decreased HRV in elderly hospitalized individuals. Individuals with sarcopenia demonstrated a fivefold increased risk of decreased HRV compared to those without sarcopenia. Biologically, lower HRV is indicative of relative sympathetic overactivity and insufficient parasympathetic activity at the sinoatrial node. This suggests that patients with sarcopenia exhibit poor autonomic function and reduced responsiveness to various stressors.9,11 Previous studies in the elderly community using short-term HRV analysis have also observed decreased HRV and an imbalance in autonomic regulation among individuals with sarcopenia.14,15 Sarcopenia and autonomic impairment may be reciprocally influential. On one hand, research in basic science has demonstrated the regulatory role of the autonomic nervous system, specifically the sympathetic system, in motor innervation, neuromuscular junction structure, and skeletal muscle function. The sympathetic system influences muscle protein synthesis, inhibits protein breakdown, and mitigates skeletal muscle loss by maintaining sympathetic neurons.6 Impairment in the sympathetic nervous system can undermine muscle performance, as documented in conditions like Alzheimer’s disease, Parkinson’s disease, and multiple system atrophy. On the other hand, individuals with sarcopenia may experience impaired autonomic function due to decreased physical activity. Previous studies have shown that physical activity and exercise are associated with increased HRV.16,17 Reduced physical activity and exercise in sarcopenia patients could lead to decreased HRV. Additionally, research has shown a correlation between sarcopenia and chronic inflammation,18–20 which may in turn affect autonomic cardiac regulation.21 HRV is also associated with chronic stress and inflammation.22 The correlation between platelet levels and decreased HRV in our study may reflect the role of inflammation. Consequently, exploring the reciprocal influence between sarcopenia and HRV provides valuable insights into the mechanisms and effects of sarcopenia, thereby opening new avenues for its prevention and treatment. Clinically, we can utilize this phenomenon to identify high-risk patients early and develop personalized intervention strategies. Therapeutic interventions could include tailored exercise programs aimed at increasing physical activity and improving HRV, and autonomic function support through medications or lifestyle changes. These interventions may help mitigate the adverse effects of sarcopenia and improve overall patient outcomes.
In our study, we discovered that muscle strength exhibited a stronger correlation with long-term HRV in elderly hospitalized patients compared to muscle mass. This finding differs from previous studies that primarily focused on short-term HRV and sarcopenia. Recent research conducted in community populations has identified a relationship between HRV and muscle mass, but no association with muscle strength or physical activity.15 Although both studies employed BIA to assess body composition and calculate SMI, the variations in study populations should be noted, with the community study encompassing younger individuals with higher levels of physical activity. Furthermore, discrepancies in HRV monitoring durations might have contributed to the inconsistent outcomes. Long-term HRV analysis provides a more comprehensive understanding of daily activities, circadian rhythms, and responses to environmental stimuli, which may exert a greater influence on muscle strength and function. Previous investigations have also indicated a correlation between grip strength and HRV,23 although without evaluating muscle mass. Generally, older adults with greater muscle strength tend to have higher levels of physical activity, and physical activity is more conducive to increasing HRV, which may result in a more direct correlation between muscle strength and HRV than between muscle mass and HRV. Unlike early research on sarcopenia, current diagnosis of sarcopenia necessitates considering both muscle strength and muscle mass. This is essential because these two factors reflect muscle status from different perspectives. Based on our study, a stronger correlation may exist between the sympathetic nervous system and muscle strength.
Within the parameters of HRV, it was observed that the triangular index is independently associated with both sarcopenia and muscle strength, whereas SDNN exclusively shows an independent relationship with muscle strength. No significant correlations were observed among rMSSD, pNN50, HF, LF, VLF, and muscle metrics. The triangular index and SDNN are non-linear time-domain metrics within HRV parameters. SDNN calculates the standard deviation of NN intervals (intervals between successive normal heartbeats). The HRV triangular index is the total number of all NN intervals divided by the height of the histogram of all NN intervals measured at a discrete scale of 1/128 seconds, reflecting the overall variability of NN (normal-to-normal) intervals for a comprehensive evaluation of heart rate variability.24 Therefore, both metrics can provide an overall insight into the autonomic regulation of cardiac function. While rMSSD and pNN50, also time-domain parameters within HRV, predominantly reflect parasympathetic activity. The link between sarcopenia and muscle strength changes with overall autonomic nervous system alterations, rather than distinct effects from the sympathetic or parasympathetic systems, is noteworthy. HF, LF, and VLF represent frequency-domain indicators in HRV analysis. Time-domain HRV metrics demonstrate a more robust correlation with muscle status compared to these frequency-domain indicators, a finding supported by short-term HRV monitoring studies in small, community-based cohorts.14 The study further endorses the judicious monitoring of long-term HRV—focusing on the triangular index and SDNN—as a strategic measure in the management of elderly patients predisposed to sarcopenia or those experiencing a decline in muscle strength.
As a predictive marker of cardiovascular health, numerous studies have identified a correlation between reduced HRV and increased mortality rates, as well as elevated risks of cardiac events.25 HRV has been utilized for risk stratification concerning all-cause mortality, cardiac death, and arrhythmic death post-myocardial infarction. Our study suggests that in the elderly hospitalized population, particularly among those with sarcopenia or decreased muscle strength, monitoring HRV and evaluating cardiac function should be emphasized.
The study faces several constraints: 1. The single-center cross-sectional design limits causal inference, making it impossible to ascertain the causal link between sarcopenia and decreased HRV. 2. Being carried out within a tertiary hospital’s elderly inpatient demographic, the subjects likely present with advanced disease states and poorer overall health, leading to possible selection bias. This highlights the necessity for further investigation via larger, prospective clinical trials. 3. Assessment of physical function was limited by the compromised daily living abilities of the elderly inpatients, constraining the evaluation of physical capabilities.
Conclusion
This investigation illuminates the significant relationship between compromised autonomic nerve function, as manifested through long-term HRV measurements, and the presence of sarcopenia and attenuated muscle strength in elder inpatient populations. The study elucidates that muscle strength bears a more substantial association with HRV parameters than muscle mass. Significantly, the triangular index and SDNN stand out as principal HRV indicators connected to these health concerns. This research highlights HRV’s potential in muscle health assessment.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The Peking University Third Hospital Medical Science Research Ethics Committee approved the study (M2023831). The procedures used in this study adhere to the tenets of the Declaration of Helsinki. Given the observational and retrospective nature of the study, the Ethics Committee waived the requirement for obtaining informed consent. All participant data were anonymized by removing any identifiable information, ensuring confidentiality. Data access was restricted to the research team and secured through measures such as encrypted storage.
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was not funded.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chen L, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J Am Med Dir Assoc. 2020;21(3):300–307. doi:10.1016/j.jamda.2019.12.012
2. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi:10.1093/ageing/afy169
3. Nair SS, Govindankutty MM, Balakrishnan M, Prasad K, Sathyaprabha TN, Udupa K. Investigation of Autonomic Dysfunction in Alzheimer’s Disease-A Computational Model-Based Approach. Brain Scien. 2023;13(9):1322. doi:10.3390/brainsci13091322
4. Fujita H, Ogaki K, Shiina T, Sakuramoto H, Nozawa N, Suzuki K. Impact of autonomic symptoms on the clinical course of Parkinson’s disease. Neurol Sci. 2024;45(8):3799–3807. doi:10.1007/s10072-024-07422-x
5. Malkiewicz JJ, Siuda J. Comparison of autonomic dysfunction in patients with Parkinson’s Disease, progressive supranuclear palsy, and multiple system atrophy. Neurol Neurochir Pol. 2024;58(2):193–202. doi:10.5603/pjnns.96939
6. Delbono O, Rodrigues A, Bonilla HJ, Messi ML. The emerging role of the sympathetic nervous system in skeletal muscle motor innervation and sarcopenia. Ageing Res Rev. 2021;67:101305. doi:10.1016/j.arr.2021.101305
7. Navegantes LC, Baviera AM, Kettelhut IC. The inhibitory role of sympathetic nervous system in the Ca2+-dependent proteolysis of skeletal muscle. Braz J Med Biol Res. 2009;42(1):21–28. doi:10.1590/S0100-879X2009000100005
8. Fonseca G, Santos M, Souza FR, et al. Sympatho-Vagal Imbalance is Associated with Sarcopenia in Male Patients with Heart Failure. Arq Bras Cardiol. 2019;112(6):739–746. doi:10.5935/abc.20190061
9. Shaffer F, Ginsberg JP. An Overview of Heart Rate Variability Metrics and Norms. Front Public Health. 2017;5:258. doi:10.3389/fpubh.2017.00258
10. Sessa F, Anna V, Messina G, et al. Heart rate variability as predictive factor for sudden cardiac death. Aging. 2018;10(2):166–177. doi:10.18632/aging.101386
11. Kim HG, Cheon EJ, Bai DS, Lee YH, Koo BH. Stress and Heart Rate Variability: a Meta-Analysis and Review of the Literature. Psychiatry Invest. 2018;15(3):235–245. doi:10.30773/pi.2017.08.17
12. Electrophysiology TFOT, Bigger JT, Camm AJ. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17(3):354–381. doi:10.1093/oxfordjournals.eurheartj.a014868
13. Wang J, Xu Z, Lv K, et al. The Predictive Value of Serum Calcium on Heart Rate Variability and Cardiac Function in Type 2 Diabetes Patients. Front Endocrinol. 2022;13:864008. doi:10.3389/fendo.2022.864008
14. Freitas VPD, Passos RDS, Oliveira AA, et al. Sarcopenia is associated to an impaired autonomic heart rate modulation in community-dwelling old adults. Arch Gerontol Geriat. 2018;76:120–124. doi:10.1016/j.archger.2018.01.006
15. Zheng K, Wang Z, Han P, et al. Lower heart rate variability is associated with loss of muscle mass and sarcopenia in community-dwelling older Chinese adults. J Formos Med Assoc. 2024;123(5):571–577. doi:10.1016/j.jfma.2023.10.010
16. Daniela M, Catalina L, Ilie O, Paula M, Daniel-Andrei I, Ioana B. Effects of Exercise Training on the Autonomic Nervous System with a Focus on Anti-Inflammatory and Antioxidants Effects.. Antioxidants (Basel). 2022;11(2). doi:10.3390/antiox11020350
17. Besnier F, Labrunee M, Pathak A, et al. Exercise training-induced modification in autonomic nervous system: an update for cardiac patients. Ann Phys Rehabil Med. 2017;60(1):27–35. doi:10.1016/j.rehab.2016.07.002
18. Livshits G, Kalinkovich A. Restoration of epigenetic impairment in the skeletal muscle and chronic inflammation resolution as a therapeutic approach in sarcopenia. Ageing Res Rev. 2024;96:102267. doi:10.1016/j.arr.2024.102267
19. Xu X, Wen Z. The mediating role of inflammaging between mitochondrial dysfunction and sarcopenia in aging: a review. American j Clin Experi Immu. 2023;12(6):109–126.
20. Zhang H, Qi G, Wang K, et al. Oxidative stress: roles in skeletal muscle atrophy. Biochem Pharmacol. 2023;214:115664. doi:10.1016/j.bcp.2023.115664
21. Li G, Zhang L, Liu M. Meta-analysis on inflammation and autonomic nervous system of coronary heart disease combined with depression. BMJ Open. 2024;14(3):e079980. doi:10.1136/bmjopen-2023-079980
22. Chrousos GP, Papadopoulou-Marketou N, Bacopoulou F, Lucafò M, Gallotta A, Boschiero D. Photoplethysmography (PPG)-determined heart rate variability (HRV) and extracellular water (ECW) in the evaluation of chronic stress and inflammation. Hormones. 2022;21(3):383–390. doi:10.1007/s42000-021-00341-y
23. Koopman JJ, van Bodegom D, Maan AC, et al. Heart rate variability, but not heart rate, is associated with handgrip strength and mortality in older Africans at very low cardiovascular risk: a population-based study. Int J Cardiol. 2015;187:559–561. doi:10.1016/j.ijcard.2015.03.383
24. Sassi R, Cerutti S, Lombardi F, et al. Advances in heart rate variability signal analysis: joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace. 2015;17(9):1341–1353. doi:10.1093/europace/euv015
25. Hillebrand S, Gast KB, de Mutsert R, et al. Heart rate variability and first cardiovascular event in populations without known cardiovascular disease: meta-analysis and dose-response meta-regression. Europace. 2013;15(5):742–749. doi:10.1093/europace/eus341
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Effectiveness of Home-Based Exercise and Nutrition Programs for Senior Adults on Muscle Outcomes: A Scoping Review
Salas-Groves E, Childress A, Albracht-Schulte K, Alcorn M, Galyean S
Clinical Interventions in Aging 2023, 18:1067-1091
Published Date: 11 July 2023