Back to Journals » Journal of Asthma and Allergy » Volume 17
Changes in Skin Test Aeroallergen Sensitization in Mexico Over the Past 14 Years and According to Climate
Authors Larenas-Linnemann D , Morfín-Maciel BM , Gonzalez-Uribe V , Gallego-Corella CI, Rico-Solís GA, Hernández-Velázquez L, García-Imperial D , Caballero-Lopez CG, Garibay-Vargas OM, Gálvez-Romero JL, García Fajardo D, Barroso-Santos J, Pérez-Áviles HDJ, Luna-Pech JA, García-Cobas CY, Coronado-Hernández KG, Ortega-Cisneros M, González-Gutiérrez CH, Rivero-Yeverino D, Navarrete-Rodríguez EM, Lezama-Vázquez L, Rivera-Alvarado KL, Ochoa-López GG, Covarrubias-Ramírez SE, Reyes-Galindo CP, Bayardo-Gutiérrez B, Calderón-Ezquerro MDC
Received 18 March 2024
Accepted for publication 14 June 2024
Published 6 August 2024 Volume 2024:17 Pages 733—742
DOI https://doi.org/10.2147/JAA.S462694
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Luis Garcia-Marcos
Skin Test Aeroallergen Sensitization in Mexico – Video abstract [462694]
Views: 45
Désirée Larenas-Linnemann,1 Blanca María Morfín-Maciel,2 Victor Gonzalez-Uribe,3 Claudia Ivonne Gallego-Corella,4 Germán Agustín Rico-Solís,5 Luiana Hernández-Velázquez,6 Daniel García-Imperial,7 Chrystopherson Gengyny Caballero-Lopez,8 Ondina Marlene Garibay-Vargas,9 José Luis Gálvez-Romero,10 Daniela García Fajardo,11 Joel Barroso-Santos,12 Herberth de Jesús Pérez-Áviles,13 Jorge Agustín Luna-Pech,14 Cecilia Yvonne García-Cobas,15 Kareli Guadalupe Coronado-Hernández,16 Margarita Ortega-Cisneros,17 Carlos Humberto González-Gutiérrez,18 Daniela Rivero-Yeverino,8 Elsy Maureen Navarrete-Rodríguez,19 Leticia Lezama-Vázquez,20 Karen Lilian Rivera-Alvarado,21 Georgina Guadalupe Ochoa-López,22 Sara Elizabeth Covarrubias-Ramírez,23 Claudia Patricia Reyes-Galindo,24 Beatriz Bayardo-Gutiérrez,25 María del Carmen Calderón-Ezquerro26
1Centro de Excelencia en Asma y Alergia Larenas, Hospital Médica Sur, Mexico City, DF, Mexico; 2Private practice, Mexico City, DF, Mexico; 3AlergiaMx, Mexico City, DF, Mexico; 4Centro de Alergia y Asma de Tijuana, Tijuana, BCN, Mexico; 5Hospital Regional Valentín Gómez Farías, Department of Allergy and Clinical Immunology, Colima, COL, Mexico; 6IMSS Hospital General de Zona Número 8, Ensenada, BCN, Mexico; 7Private Practice, Querétaro, QRO, Mexico; 8Hospital Universitario de Puebla, Benemérita Universidad Autónoma de Puebla, Puebla, PUE, Mexico; 9Private practice, Uruapan, MICH, Mexico; 10Jefatura de investigación, Hospital Regional ISSSTE, Puebla, PUE, Mexico; 11Private Practice, San Luis Potosí, SLP, Mexico; 12Private practice, Pachuca, HGO, Mexico; 13Private Practice, Mérida, YUC, Mexico; 14Departamento de Disciplinas Filosófico, Metodológico e Instrumentales, CUCS, Universidad de Guadalajara, JAL, Mexico; 15Alergia e Inmunología, HGR 46, Instituto Mexicano del Seguro Social, Guadalajara, JAL, Mexico; 16Centro Médico Nacional del Occidente Pediatrics, Guadalajara, JAL, Mexico; 17Centro Médico Nacional de Occidente UMAE Hospital de Especialidades, Department of clinical immunology and allergy, Guadalajara, JAL, Mexico; 18HGZ # 1 IMSS, Zacatecas, ZAC, Mexico; 19Hospital Infantil de México ‘Federico Gómez’, Mexico City, DF, Mexico; 20Private practice, Tuxtla-Gutiérrez, CHIS, Mexico; 21IMSS UMAE 14, Veracruz, VER, Mexico; 22Private practice, Ciudad Juárez, CHIH, Mexico; 23Plebitos, Especialidades Pediátricas, Mazatlán, SIN, Mexico; 24ISSSTE, Ciudad Victoria, TAMPS, Mexico; 25Centro Médico Nacional de Occidente UMAE Hospital de Especialidades, Departamento de Inmunología Clínica y Alergia, Hospital Regional ISSSTE, Puebla, PUE, Mexico; 26Instituto de Ciencias de la Atmósfera y Cambio Climático, Universidad Autónoma de México, Mexico City, DF, Mexico
Correspondence: Désirée Larenas-Linnemann, Centro de Excelencia en Asma y Alergia Larenas, Hospital Médica Sur, Torre 2 cons. 602, Puente de Piedra 150, Col. Toriello Guerra, Del. Tlalpan, Ciudad de México, 14050, Mexico, Tel +52-55-5171-2248 ; +5606-6222 Ext.4372 ; +52-55-8509-5950, Email [email protected]
Introduction: Aeroallergen exposure has an intra- and extra-domiciliary component and varies according to climatological zones. Mexico is a large country with a great variety of climates. A previous study (2009) evaluated skin prick test results (SPT) in different regions. In this study, we compare previous sensitization patterns from 14y ago with current ones and compare them between different climatological zones.
Methods: Mexican allergists were asked to share their last 100 SPT results in patients with respiratory allergy. Clinics were grouped in (semi)humid vs (semi)dry zones. Results were analyzed nationwide and compared to the 2009 results, calculating odds ratio (OR) and 95% confidence intervals (95% CIs), with p < 0.05 as cut-off. Similarly, we compared (semi)humid versus dry zones.
Results: We collected 2915 SPT results from 28 clinics (19 cities). Dermatophagoides was the most frequently sensitizing allergen. There was a significant increase in SPT positivity from 2009 to 2023 in both in- and outdoor aeroallergens (OR 1.26– 2.65, 95% CI from 1.06– 1.50 to 1.99– 3.52). Comparing dry-humid zones, sensitization to pollen from Oleaceae, Fagaceae (p < 0.0001 all) and most weeds is more frequent in humid zones, as are Dermatophagoides and cockroach (both p < 0.0001). Eucalyptus, mesquite, and all grass pollen sensitizations predominate in dry zones (p < 0.05– 0.0001). There are no differences in sensitization to cat or dog between zones.
Conclusion: We found a general increase in SPT sensitization over the past fourteen years, suggesting that this is probably not only due to climate change. The different sensitization profile throughout the country was mainly related to humidity. Repeating epidemiologic SPT studies over the years could help tracking changes in allergen sensitization over time.
Keywords: allergy, diagnosis, skin prick testing, aeroallergen, climate change, pollen allergy, allergic rhinitis, allergic asthma
Introduction
The allergenic content of the atmosphere varies according to plant phenology, linked to meteorological conditions, geography, and degree of urbanization.1 Mexico is a large country with a surface area of 1,935,162 km,2 consisting of 32 states. The north of the country has a dry climate, with desert areas in four states. The central zone is considered temperate and semi-humid, while in the southwest, the warm, semi-humid climate predominates, and in the southeast, the climate ranges from temperate humid to a frankly tropical one.2 In the northwest and northeast, scrublands prevail, with large areas of coniferous forests, oaks, grasslands, and saline soil vegetation. Mountainous forest areas can be found in the center and coniferous and oak forests in the center and northwest of the country. There is a predominance of dry forest in the southwest, while the vegetation is aquatic (mangroves) and humid jungle in the southeast.2 As a result of this diversity, variation in allergen sensitization profiles can be expected.
In the context of climate change in Mexico, Cuervo-Robayo et al published data for the last hundred years, showing mean temperature has increased by nearly 0.2°C on average, but this has been more pronounced in the Northern Nearctic provinces. The southern tropical provinces cooled at the beginning of the 20th century and then warmed consistently since the 1970s. Precipitation increased in the middle of the past century but has been decreasing since.3 More recently, a rise in the temperature of +0.71°C was documented between 1951 and 2017 and no change in overall precipitation. However, when the full water balance was seasonally accounted for (precipitation minus potential evapotranspiration), the trend resulted in more extreme climates with a wetter wet season and a much drier dry season across the country,4 in agreement with data from the World Bank 1901–2020.5
In 2009, we conducted a structured, retrospective chart-review of skin prick test (SPT) results, with the participation of eleven allergy clinics throughout the country plus ten that submitted joint results of 1500 patients in the North. Each of the former clinics uploaded the results of at least a hundred patients, giving a total of 4169 SPT-result charts. Dermatophagoides pteronyssinus was the most frequently sensitizing allergen (51%) followed by pollens from various trees (Ash 27%, Alder 22%, Oak 19%), and Bermuda grass (26%). In the hot zones (humid and dry) Aspergillus sensitization was more frequent than in the more temperate zones, while cockroaches thrive in big cities and humid zones; contrarily, Mesquite and Poplar sensitize more in dry zones. Generally, weed pollens were less important.6
Reports of aeroallergen sensitization profiles in Latin America are not abundant but have been conducted in some other countries, such as Colombia,7 Venezuela,8 Brazil,9 and Argentina.10 However, to our knowledge, no reports exist related to changes in aeroallergen sensitization over time nor comparing different climatological zones in one country.
Thus, we decided to repeat the retrospective chart review focusing on SPT aeroallergen positivity in different regions of Mexico and compare the results with the 2009 Mexican SPT data.6
Materials and Methods
Allergists throughout the country were invited to download the results of their most recent SPT (at least 100), conducted in patients 3–80 years-old with respiratory allergy onto a standardized Excel file. Centers indicated which allergens were tested, and which of them presented a positive SPT. According to the Mexican Guidelines on allergen immunotherapy, a mean wheal diameter 3 mm larger than the mean wheal size of the negative control, is considered a positive test.11 Participating centers were grouped according to the National Institute of Statistics and Geography (Instituto Nacional de Estadística, Geografía e Informática (INEGI)) climatological classification,2 in (semi)humid and (semi)dry zones and per average temperature. The dry zones correspond to the Köppen-Geiger climate classification of B, for desert and semi-arid regions in temperature ranging from cold (Bwk) to hot (Bwh). The (semi)humid INEGI regions correspond to Köppen-Geiger classifications A (tropical) to C (temperate), with summer temperatures from warm to hot (see Köppen-Geiger climate classifications).
Many centers test with Dermatophagoides spp. as cross-reactivity between Dermatophagoides pteronyssinus and Dermatophagoides farinae is very high.12,13 Other centers, however, do test for the separate species. For data analysis, outcomes of all three groups were presented separately. Results were analyzed nationwide and compared to the data from a very similar study in Mexico in 2009. For the comparison of the ratios of SPT positivity between old and the new data and humid versus dry regions, only allergens with >500 SPT were considered. Comparisons were conducted with chi-square test, with Yate’s correction for continuity applied to calculate odds ratios (OR) and 95% confidence intervals (95% CIs), with p <0.05 as cut-off to detect statistically significant differences.
In Mexico, in accordance with the General Health Law and its regulations, clinical research studies that are exempt from requiring approval by an ethics committee are those that involve the use of medical records, as long as the confidentiality of patient’s personal data is ensured, and legal provisions regarding the protection of personal and health data are complied. Our retrospective, anonymized chart review falls under this category. This is also in accordance with the guidelines outlined in the Declaration of Helsinki.
Results
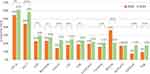
In the 2022–2023 study allergists from 28 different clinics from 19 different cities, distributed throughout Mexico, participated (Table 1 and Figure 1), with a total of 2915 skin prick test results collected. As this was a retrospective collection of real-world data, each center reported the findings of their routine testing. Thus, not all allergens were tested in all centers. Figure 2 depicts aeroallergens with at least 500 conducted SPTs and at least a 10% SPT positivity. Nationwide, house dust mite (HDM) is by far the most frequently sensitizing allergen. For a report on all tested allergens and their frequency of positivity, see Supplementary Table 1.
 |
Table 1 Participating Centers, Their Distribution Over the Humid and Dry Regions and Number of SPTs Reviewed per Center |
 |
Figure 1 Geographic distribution of the participating centers and climatological zones in Mexico. Mexican Republic with climatological zones according to INEGI and participating centers. INEGI climatological zones are based on average temperature and rainfall and closely related to the Köppen-Geiger climate classification. All Köppen-Geiger B-classified cities are in our dry group. A more precise description can be found on the INEGI website.2 |
As Dermatophagoides pteronyssinus and Dermatophagoides farinae cross react almost completely,13,14 many allergists opt for skin testing with a mixture of Dermatophagoides spp. The next most frequently aeroallergen sensitization is directed against ash tree pollen, the tropical grass Bermuda grass and cat. In Figure 3 we compare the positive ratio of aeroallergens in SPTs conducted recently, against those reported in the 2009 SPT study. All aeroallergens, except for Blomia tropicalis, showed a rise in SPT positivity, almost all of these increases in SPT positivity being of statistical significance (for detailed comparisons see Supplementary Table 2). The most remarkable increases in SPT sensitization (≥10%) were documented for Dermatophagoides farinae, perennial ryegrass (Lolium) and saltbush.
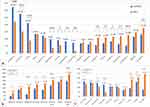
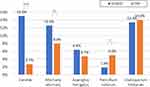
In the Figures 4–6, we present the frequency of SPT positivity to aeroallergens in the humid versus the dry regions, again only considering those aeroallergens with at least 500 SPTs. SPT sensitization to pollens from the Oleaceae family (ash, olive and privet) and the Fagaceae family (oak, Casuarina), among others (Figure 4a), is more frequent in humid regions; for the most frequently tested tree pollens the odds ratio for SPT positivity for patients living in humid regions compared to patients living in dry regions varied from 1.66 (95% CI 1.09–2.55) for acacia to 2.78 (95% CI, 2.06–3.75) for olive (Supplementary Table 3). Meanwhile, SPT sensitization to pollens from walnut tree, white pine, juniper, eucalyptus, and mesquite and others (Figure 4a) is more frequently seen in regions with a drier climate. For these trees, the odds ratios for SPT sensitization for patients living in humid versus patients living in drier regions varied from 0.70 (95% CI, 0.56–0.87) for mesquite to 0.38 (95% CI, 0.27–0.54) for eucalyptus.
All grass pollen sensitizations were more abundant among patients from drier regions, with the pollen of Bermuda grass, a tropical grass, being the most frequently sensitizing grass in the drier regions (Figure 4b). Most of these differences reached statistical significance, as shown in Supplementary Table 4.
As for sensitization to weed pollens, some are more frequent in humid zones (ragweed (Ambrosia), Lamb’s quarters (Chenopodium) and sunflower (Helianthus)), while others are more common in drier zones, such as Russian thistle (Salsola kali), saltbush (Atriplex) and plantain (Plantago lanceolata), reaching the highest SPT sensitization for weed pollens of 24.4% in dry regions (Figure 4c and Supplementary Table 5).
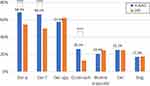
Figure 5 and Supplementary Table 6 depict the SPT sensitization in humid versus dry regions for perennial allergens. There was a higher SPT positivity among patients living in humid regions for HDM and cockroach, while there was no difference in sensitization to cat and dog.
Finally, Figure 6 and Supplementary Table 7, show the frequency of SPT sensitivity to molds. Generally, SPT sensitization to molds is not very common nationwide. Although three centers detected positivity in almost a third of their patients, these are isolated reports that need to be confirmed with larger sample sizes. Candida and Alternaria sensitization is much more abundant in patients from humid regions, rising to a 15% SPT positivity. The second most often SPT sensitizer from among the molds is Cladosporium, being equally frequent in humid and dry regions.
We could not find any significant difference in sensitization patterns related to temperature in our study sample.
Discussion
In this paper, we show the outcomes of skin-prick tests in patients with respiratory allergies throughout Mexico and compare results against a similar study conducted in 2009. We demonstrate that there was an increase in SPT positivity for almost all the most frequent allergens from all reported sources, both in- and outdoors. The only two exceptions were cockroach, for which SPT sensitization was maintained around 20%, and Blomia tropicalis, for which the sensitization frequency was reduced. When comparing the humid against the drier regions of Mexico in 2022–2023 the profile of the SPT sensitizations showed several clear differences: there are trees whose pollens sensitize more in the humid climates and others that sensitize more often in drier climates. For grasses, sensitization is more common in drier regions and for weeds it depends on the weed. As expected, HDM sensitization is more frequent in humid climates as is SPT positivity for cockroach and some molds, while there is no difference in pet allergen sensitization between humid and dry zones.
Interpreting these data in the context of local pollen exposure is not easy as registration of pollen counts is only done persistently in Mexico City and from time to time in Hermosillo, Los Mochis, San Luis Potosí, Toluca and Monterrey. Moreover, pollen counting was practically stopped 2020–2022 during the Pandemics. Of the pollens counted, the yearly pollen load in 2009–2013 was 30–50% higher than the yearly count of 2017 onward (unpublished data). Also, in Mexico, there is no clear pollen season, as polinization practically continues year-round. Thus, apart from the number of pollens in the air, the observed increase in sensitization frequency for pollens here reported should probably – at least in part – be accounted for by other mechanisms, which we shall briefly review.
Vegetation in polluted areas could produce more allergenic pollen, as the interaction between air pollutants and pollen grains might damage the pollen cell wall, increasing the quantity of allergenic molecules released into the environment;15 also, particulate matter could serve as pro-allergic adjuvants.
A rise in sensitization to tree pollens related to climate change in children and adolescents with respiratory allergy was documented in a very comprehensive study in Seoul, Korea. Lee et al analyzed SPT sensitization and meteorological data over two decades (from 1998 till 2019). Among the major tree pollens, the largest increases in allergic sensitization were noted for oak, hazel, and alder pollens, with an annual increase of 0.28%, the major increases being detected within the younger age groups. Meanwhile, the meteorological data in Seoul showed a parallel increase in the duration of the pollen season from 98 days to 140 days and a rise in temperature, both factors correlating positively with the rise in SPT positivity to tree pollens.16
Since the 2009 analysis, it became clear that the most frequently sensitizing pollens in Mexico are not olive, birch and timothy grass as in Europe, but their family members or related pollens: ash, oak and Bermuda grass. In our population sensitization to some pollens was more frequent in the dry regions, such as grasses, several weeds (plantain, Russian thistle, saltbush and dandelion) and mesquite. Data reported in Qatar, with a hot and dry climate, are partly in agreement with our findings. The highest frequency of SPT positivity was reported for pollen from Amaranthaceae (66.2%), followed by Poaceae (55.8%), mesquite (18.1%) and dandelion.17 In Kuwait, sensitization to Russian thistle was the most frequently reported sensitization, followed by Lamb’s quarters and Bermuda grass; indoor allergens were less important in this cohort.18
Since several years back, it became clear how climate change is increasing not only the peak pollen season and thus the pollen load in the environment but also the duration of the pollen seasons and even the allergenicity of pollens.19–21 At the start of this, millennium aerobiologists already had observed a trend toward an earlier start of the birch pollen season in many European countries, related to increasing temperatures over the past 30 years.22 Apart from temperature, Rogers et al also demonstrated how environmental carbon dioxide (CO2) can increase plant biomass and photosynthesis. CO2 level is higher in urban areas, and some investigators have demonstrated an increase in inner-city ragweed allergenic potential: the plants grew faster, flowered earlier, and produced significantly greater aboveground biomass and pollen.23 More recently, colleagues from Mexico City also reported on the association among allergenic sensitivity, pollination, and pollution.24
Although one would not expect to find a rise in pet allergen sensitization due to climate change, the rise in pet ownership25,26 could be an explanation for the augmented sensitization frequency we found for cat (18–25%) and dogs (9–17%) from 2009 to today. Globally, pet ownership has been on the rise, and a survey showed Mexico is among the countries with the highest dog ownership.27
Finally, another explanation could be that recently exposed individuals are more susceptible to develop specific-IgE to any (aero)allergen, as predicted by the “broken barrier” theory. This could also be a factor in the simultaneous increase we observed in the sensitization frequency of indoor allergens.28
Our study is based on retrospective chart reviews of the 100+ most recent SPT results in various allergy clinics in 19 cities throughout Mexico. In our country, there are several providers of allergen extracts, what can result in differences in quality and potency of the SPT material. Moreover, each SPT technician (physician or nurse) has his own technique of conducting and reading an SPT. Due to the retrospective methodology of this trial, these issues were not standardized among the different participating centers, which could be a factor of bias. However, in this sense, it is reassuring that the 2023 SPT positivity for cat and dog is practically the same in humid and dry regions, indicating that it is very probable that SPT techniques do not vary too much between centers.
When comparing 2009 with 2022–2023 data, other factors of bias could be present. Thus, the rise in allergen sensitization documented here could have several causes, apart from climate change and augmented exposure to allergens of higher allergenicity. The number of centers that participated in our recent chart review was much larger than the number of centers participating in 2009, and only partly overlapped. Moreover, some of the allergen extract providers have changed during these past fourteen years. Probably, this did not impact too much, as many different centers participated and thus, we might expect a regression to the mean due to some centers using more potent and others less potent allergen extracts. However, the only allergen extract with remarkably lower potency currently is Blomia tropicalis that, in 2009, was almost exclusively sold by a Cuban company preparing a high quality, highly concentrated allergen extract, meeting European standards. This facility is no longer providing extracts for export. This could explain why Blomia tropicalis is the only allergen with a reduced current sensitization frequency.
The retrospective SPT chart-review from 2009 was followed two years later by a prospective study, with the same set of blinded allergen extracts used in all participating centers, standardizing SPT technique with proficiency testing before recruiting patients.29 Thus, we are now in the planning phase of a prospective study of similar design as the prospective one from more than a decade ago, to produce more robust data. Even so, the experience showed that the results from the prospective study in 2012 did not show major differences from those of the retrospective chart review from 2009. Moreover, sensitization data can now also be collected from molecular allergy diagnostics, but costs are still prohibitive for large samples. Finally, simultaneous collection of precise aerobiology data on pollens in the atmosphere, as was done in Korea, would be very enriching. In Mexico, we do not yet have these high-tech methodologies for aerobiology detection available.
Conclusions
Our results suggest a remarkable increase in SPT sensitivity across the whole range of allergens, seasonal and perennial as well as in-door and out-door ones, over the past 14 years. Conclusions should be drawn with care as some confounding factors and possible points of bias could not be ruled out. Public health suggestions based on our findings are a stricter anti-pollution policy and for patients to wear a KN-95 face mask out-doors during the pollen season of their particular sensitizer and during days of high pollution. Economically supporting the online pollen reporting website to augment the detection stations within Mexico City and in other cities and to give continuity to this endeavor could help with that.
We also demonstrated a different sensitization profile throughout the country, related to humidity. Allergists should assemble their SPT panel with the most frequently sensitizing allergens nationwide but also be acquainted with the local flora and partly adapt their SPT panel accordingly.11,30 Moreover, running retrospective chart reviews of SPT results is of ongoing value, as changing sensitization profiles, as well as local differences can be picked up by this simple, low-cost method, as long as the sample size is large enough. These data should be confirmed in a prospective study with the same blinded extracts being tested with a standardized SPT technique. Data should ideally be complemented by molecular allergen sensitization profiles.
Abbreviations
CI, confidence interval; HDM, House dust mite; INEGI, Instituto Nacional de Estadística, Geografía e Informática; OR, Odds ratio; SPT, skin prick test.
Acknowledgments
We would like to acknowledge the study-group members from Centro Médico Nacional del Occidente Pediatric ward, Guadalajara (GUAD), Mexico: Héctor Hugo Campos-Téllez, Britza Barrios-Díaz and Lourdes Iveth Salazar-Lizárraga. The Center of Excellence in Asthma and Allergy, Mexico City, Mexico, supported with their staff time spent on statistical calculations. All participating centers dedicated their spare time to submit the data.
Disclosure
Dr. Larenas Linnemann reports personal fees from ALK, AstraZeneca national and global, Bayer, Chiesi, Grunenthal, Grin, GSK national and global, Viatris, Menarini, MSD, Novartis, Pfizer, Sanofi, Siegfried, UCB, Carnot; grants from AbbVie, Bayer, Lilly, Sanofi, AstraZeneca, Pfizer, Novartis, Circassia, UCB, GSK, Chiesi, outside the submitted work. In addition, she is the Chair of immunotherapy committee, Colegio mexicano de inmunología clínica y alergia. Dr Gallego-Corella reports personal fees from Takeda, outside the submitted work. Dr García-Imperial reports grants from Chiesi, Astra-Zeneca and Alk-Abello, outside the submitted work. Dr Ortega-Cisneros reports grants and personal fees from Sanofi and Chiesi, outside the submitted work. Dr Navarrete-Rodríguez reports personal fees from Astra Zeneca, AbbVie, Pfizer, Sanofi, and Eli Lilly, outside the submitted work. Dr Covarrubias-Ramírez received an educational grant from Sandoz Laboratory. None of the other authors declare any conflicts of interest for this work.
References
1. Galan C, Alcazar P, Oteros J, et al. Airborne pollen trends in the Iberian Peninsula. Sci Total Environ. 2016;550:53–59. doi:10.1016/j.scitotenv.2016.01.069
2. Instituto Nacional de Estadística GeII. Geography and Environment. Climatology; 2023. Available from: https://www.inegi.org.mx/temas/climatologia/. Accessed
3. Cuervo-Robayo AP, Ureta C, Gomez-Albores MA, Meneses-Mosquera AK, Tellez-Valdes O, Martinez-Meyer E. One hundred years of climate change in Mexico. PLoS One. 2020;15(7):e0209808. doi:10.1371/journal.pone.0209808
4. Murray-Tortarolo G. Seven decades of climate change across Mexico. Atmósfera. 2021;34(2): 217–226.
5. World Bank Group. Climate change knowledge portal. 2021; Available from: https://climateknowledgeportal.worldbank.org/country/mexico/climate-data-historical. Accessed
6. Larenas-Linnemann DE, Fogelbach GA, Alatorre AM, et al. Patterns of skin prick test positivity in allergic patients: usefulness of a nationwide SPT chart review. Allergol Immunopathol. 2011;39(6):330–336. doi:10.1016/j.aller.2010.09.006
7. Sanchez-Caraballo J, Diez-Zuluaga S, Cardona-Villa R. Sensitization to aeroallergens in allergic patients from Medellin, Colombia. Rev Alerg Mex. 2012;59(3):139–147.
8. Sanchez-Borges M, Capriles-Hulett A, Torres J, et al. Diagnosis of allergic sensitization in patients with allergic rhinitis and asthma in a tropical environment. Rev Alerg Mex. 2019;66(1):44–54. doi:10.29262/ram.v66i1.570
9. Pastorino AC, Kuschnir FC, Arruda LK, et al. Sensitisation to aeroallergens in Brazilian adolescents living at the periphery of large subtropical urban centres. Allergol Immunopathol. 2008;36(1):9–16. doi:10.1157/13115665
10. Pendino P, Aguero C, Cavagnero P, Lopez K, Kriunis I, Molinas J. Aeroallergen sensitization in wheezing children from rosario, Argentina. World Allergy Organ J. 2011;4(10):159–163. doi:10.1097/WOX.0b013e318232df96
11. Larenas-Linnemann D, Luna-Pech JA, Rodriguez-Perez N, et al. GUIMIT 2019, Mexican guideline on immunotherapy. guideline on the diagnosis of IgE-mediated allergic disease and immunotherapy following the ADAPTE approach. Rev Alerg Mex. 2019;66(Suppl 1):1–105. doi:10.29262/ram.v66i5.631
12. Weghofer M, Thomas WR, Kronqvist M, et al. Variability of IgE reactivity profiles among European mite allergic patients. Eur J Clin Invest. 2008;38(12):959–965. doi:10.1111/j.1365-2362.2008.02048.x
13. Arlian LG, Bernstein IL, Vyszenski-Moher DL, Gallagher JS. Investigations of culture medium-free house dust mites. IV. Cross antigenicity and allergenicity between the house dust mites, Dermatophagoides farinae and D. pteronyssinus. J Allergy Clin Immunol. 1987;79(3):467–476. doi:10.1016/0091-6749(87)90364-2
14. Platts-Mills TA, Chapman MD. Dust mites: immunology, allergic disease, and environmental control. J Allergy Clin Immunol. 1987;80(6):755–775. doi:10.1016/S0091-6749(87)80261-0
15. Sedghy F, Varasteh AR, Sankian M, Moghadam M. Interaction between air pollutants and pollen grains: the role on the rising trend in allergy. Rep Biochem Mol Biol. 2018;6(2):219–224.
16. Lee KS, Kim K, Choi YJ, et al. Increased sensitization rates to tree pollens in allergic children and adolescents and a change in the pollen season in the metropolitan area of Seoul, Korea. Pediatr Allergy Immunol. 2021;32(5):872–879. doi:10.1111/pai.13472
17. Al-Nesf MA, Gharbi D, Mobayed HM, et al. The association between airborne pollen monitoring and sensitization in the hot desert climate. Clin Transl Allergy. 2020;10(1):35. doi:10.1186/s13601-020-00339-6
18. Al-Dowaisan A, Fakim N, Khan MR, et al. Salsola pollen as a predominant cause of respiratory allergies in Kuwait. Ann Allergy Asthma Immunol. 2004;92(2):262–267. doi:10.1016/S1081-1206(10)61558-X
19. D’Amato G, Cecchi L, D’Amato M, Annesi-Maesano I. Climate change and respiratory diseases. Eur Respir Rev. 2014;23(132):161–169. doi:10.1183/09059180.00001714
20. Choi YJ, Lee KS, Oh JW. The impact of climate change on pollen season and allergic sensitization to pollens. Immunol Allergy Clin North Am. 2021;41(1):97–109. doi:10.1016/j.iac.2020.09.004
21. Barnes CS. Impact of climate change on pollen and respiratory disease. Curr Allergy Asthma Rep. 2018;18(11):59. doi:10.1007/s11882-018-0813-7
22. Emberlin J, Detandt M, Gehrig R, Jaeger S, Nolard N, Rantio-Lehtimaki A. Responses in the start of Betula (birch) pollen seasons to recent changes in spring temperatures across Europe. Int J Biometeorol. 2002;46(4):159–170. doi:10.1007/s00484-002-0139-x
23. Rogers CA, Wayne PM, Macklin EA, et al. Interaction of the onset of spring and elevated atmospheric CO2 on ragweed (Ambrosia artemisiifolia L.) pollen production. Environ Health Perspect. 2006;114(6):865–869. doi:10.1289/ehp.8549
24. Pavon-Romero GF, Larenas-Linnemann DE, Xochipa Ruiz KE, Ramirez-Jimenez F, Teran LM. Subcutaneous allergen-specific immunotherapy is safe in pediatric patients with allergic rhinitis. Int Arch Allergy Immunol. 2021;182(6):553–561. doi:10.1159/000513158
25. Christopoulos K, Benetou V, Riza E, Pantazis N. Pet ownership and survival of European older adults. Eur J Ageing. 2022;19(4):1549–1560. doi:10.1007/s10433-022-00739-6
26. Colella V, Wongnak P, Tsai YL, et al. Human social conditions predict the risk of exposure to zoonotic parasites in companion animals in East and Southeast Asia. Commun Med. 2022;2(1):144. doi:10.1038/s43856-022-00210-8
27. GfK. Pet ownership, global GfK survey. 2016. Available from: https://cdn2.hubspot.net/hubfs/2405078/cms-pdfs/fileadmin/user_upload/country_one_pager/nl/documents/global-gfk-survey_pet-ownership_2016.pdf. Accessed
28. Akdis CA. The epithelial barrier hypothesis proposes a comprehensive understanding of the origins of allergic and other chronic noncommunicable diseases. J Allergy Clin Immunol. 2022;149(1):41–44. doi:10.1016/j.jaci.2021.11.010
29. Larenas-Linnemann D, Michels A, Dinger H, et al. Allergen sensitization linked to climate and age, not to intermittent-persistent rhinitis in a cross-sectional cohort study in the (sub)tropics. Clin Transl Allergy. 2014;4(1):20. doi:10.1186/2045-7022-4-20
30. Larenas-Linnemann D, Ortega-Martell JA, Del Rio-Navarro B, et al. Mexican clinical practice guidelines of immunotherapy 2011. Rev Alerg Mex. 2011;58(1):3–75.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.